Abstract
Background The choice and use of unicondylar knee arthroplasty (UKA) has gone through a nation wide resurgence at the start of the 21st century in Finland. We evaluated the population-based survival of UKA in patients with primary osteoarthritis (OA) in Finland, and the factors affecting their survival.
Method The Finnish Arthroplasty Register was established in 1980. During the years 1985–2003, 1,928 primary UKAs were recorded in the register; 1,819 of these were performed for primary OA. Of these 1,819 UKAs, we selected for further analysis implants that had been used in more than 100 operations during the study period. The survival rates of UKAs were analyzed using Kaplan-Meier analysis and the Cox regression model.
Results Analysis of the whole study period showed that UKAs had a 73% (95% CI: 70–76) survival rate at 10 years, with revision for any reason as the end point. Those patients who received the Oxford menisceal bearing unicondylar (n = 1145) had a survival rate of 81% (95% CI: 72–89) at 10 years. The group that received the Miller-Galante II unicondylar (n = 330) had a 79% survival rate (95% CI: 71–87) at 10 years, whereas the Duracon (n = 196) had a survival rate of 78% (95% CI: 72–84) and the PCA (n = 146) had a survival rate of 53% (95% CI: 45–60) at 10 years. The number of UKA operations in Finland has increased markedly in recent years. At the time of operation, the mean age of the patients was 65 (38–91) years. Younger patients (≤ 65 years of age) were found to have a 1.5-fold (95% CI: 1.1–2.0; p = 0.04) increased risk of revision compared to older patients (< 65 years).
Interpretation UKA is a viable option for the treatment of unicompartmental osteoarthritis of the knee. However, patients should be made aware of the lower survival of the UKAs compared with total knee arthroplasties.
Unicondylar knee arthroplasty (UKA) has been performed for more than three decades. Initial results with the very first designs were not promising, although the basic idea was appropriate. If only one compartment of the knee is affected, is there really a need to replace the whole knee joint? Skolnick et al. (Citation1975) published results of a series of 14 knees with a UKA. Other early reports also included papers by Marmor (Citation1976) and by Scott and Santore (Citation1981) with series of 124 and 100 knees, respectively. Prerequisites for a UKA such as unicompartmental disease, functioning anterior cruciate ligament, tibiofemoral angles between physiological valgus and 10° varus and no subluxation are largely accepted in retrospective studies (Deschamps et al. Citation1987, Goodfellow et al. Citation1994).
There has only been one randomized, prospective study comparing 5-year results of UKA and total knee arthroplasty (TKA) in osteoarthritic knees (Newman et al. Citation1998). The authors concluded that it seems reasonable to offer suitable patients the benefits of a more normal knee by preserving the cruciate ligaments and intact articular cartilage whenever possible. Retrospective direct comparison studies comparing UKA with TKA (Cobb et al. Citation1990, Rougraff et al. Citation1991) have shown the superiority of UKA. These studies may be criticized for their lack of randomization. In addition, we were able to find one systematic review comparing bi- and unicompartmental prostheses (Callahan et al. Citation1995). The review found both procedures to be effective—based on pain, function, and range of movement on a global rating scale (Drake et al. Citation1994). Since 1987, however, UKA operations have been reported to be more effective due to improved patient selection procedures and advanced implant design. In their study comparing UKA and TKA, Bengtson and Knutson (Citation1991) stated that the risk of serious complications—such as infection of prostheses—is lower for UKAs. Register-based results of UKA have only been reported previously from Sweden (Robertsson et al. Citation1999, Citation2000) and from USA (Gioe et al. Citation2003).
We evaluated the survival of UKAs in patients with primary osteoarthritis (OA) and the factors affecting survival of the implants by means of a prospective population-based study based on data obtained from the Finnish Arthroplasty Register.
Patients and methods
Our study was based on information recorded in the Finnish Arthroplasty Register (Paavolainen et al. Citation1991, Puolakka et al. Citation2001) relating to patients who underwent UKA between January 1, 1985 and December 31, 2003 inclusive. Information on 1,928 UKAs had been recorded individually for all such operations since the beginning of the Register. An English translation of the form used for this purpose has been discussed previously (Puolakka et al. Citation2001). Revisions were linked to the primary operation using the unique personal ID number assigned to each resident of Finland. Information on dead or emigrated patients was provided by the Population Register Center, which has data on all citizens of Finland. Of the 1,928 UKAs in the register, 1,819 (94%) were performed on patients with primary OA. These 1,819 UKAs were included in our analysis.
Time-dependent trends
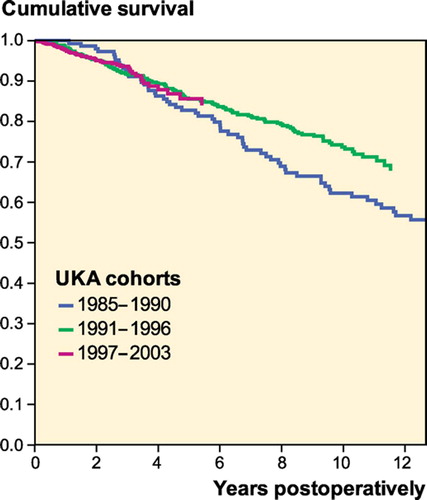
The number of hospitals performing UKAs was analyzed for three time periods: 1985–1986, 1992–1993, and 2002–2003. Survival of UKAs was analyzed separately for the whole study period and for 3 consecutive time periods (1985–1990, 1991–1996, and 1997–2003). The results of the first time period are based almost exclusively on the PCA prosthesis.
Inclusion criteria for design analysis
We selected UKA designs that had been used in more than 100 operations during the study period (Espehaug et al. Citation1995, Havelin et al. Citation1995, Eskelinen et al. Citation2006). In addition, only implants with more than 20 patients at risk at 10 years (Dorey Citation2004) were included.
According to our inclusion criteria, 4 implant designs were included: the Oxford menisceal bearing (Biomet, Warsaw, IN), the Miller-Galante unicondylar (Zimmer, Warsaw, IN), the PCA unicondylar (Howmedica, Rutherford, NJ) and the Duracon unicondylar (Howmedica). These 4 designs covered 92% of all UKAs implanted in Finland in patients with primary OA (). Thus, 1,736 UKAs were included in the design analysis.
Table 1. Bearing types of the four most commonly used unicompartmental knee prostheses (n = 1,817)
Statistics
In all analyses, the endpoint for survival was defined as revision for any reason. The Kaplan-Meier survival data were used to construct the survival probabilities of implants at 5, 7 and 10 years of follow-up. Survival data obtained in the Kaplan-Meier analysis were compared by the log-rank test. The Cox multiple-regression model was applied to study differences between groups and to adjust for potential confounding factors. The factors studied with the Cox model were as follows: implant designs, hospital UKA volume (≤ 10 or < 10 UKAs annually), time periods (1985–1990, 1991–1996, and 1997–2003), age group (≤ 65 and < 65 years) and sex. All models included adjustment for differences in age (≤ 65 and < 65 years) and sex. When UKA designs were analyzed in the Cox model, the most commonly implanted UKA (Oxford menisceal bearing) served as the reference design. Dead or emigrated patients were censored at the time point at which they had emigrated or died. For further analysis, the Cox regression analyses provided estimates of survival probabilities and revision risk ratios (RR) for different factors. Estimates from Cox analyses were used to construct adjusted survival curves at mean values of the risk factors. The Wald test was used to calculate p-values for data obtained from the Cox multiple regression analysis. Differences between groups were considered statistically significant if the p-values were less than 0.05 in a two-tailed test.
We used SPSS software version 12.0 for the statistical analyses.
Results
Primary operation
Patient characteristics
Of the 1,819 UKA operations, 1,244 (68%) were performed on female patients and 575 (32%) on male patients. At the time of operation, the mean age of the patients was 65 (38–91) years (). Of all UKAs, 913 (50%) were performed on the left knee. The number of UKA operations has increased markedly over the last years in Finland ().
Table 2. Age distribution of UKAs (n = 1,819)
Table 3. The number of UKA for primary osteoarthritis have increased from 1985 to 2003 in Finland (n = 1,819)
The number of hospitals performing UKAs for primary OA increased from 2 over the first period (1985–1986) to 19 in the early years of the next decade (1992–1993), and to 40 at the end of the study period (2002–2003). During the last time period analyzed (2002–2003), 28 of the 40 hospitals included in the study performed less than 10 UKAs annually.
Implants
Over the whole study period 9 UKA designs were used, 5 of them in fewer than 100 operations. All implants were cemented. At the end of the study period (2002–2003), only 2 UKA designs were being used in Finland: the Oxford menisceal bearing (Biomet) and the Miller Galante II unicondylar (Zimmer).
Revision operations
During 1985–2003, 234 revisions were performed. The most common reason for revision was aseptic loosening (n = 104, 44%). Progression of the OA in other compartments of the knee accounted for 33% of the revisions (n = 77). Breakage of the polyethylene matrix accounted for 9% of the revisions (n = 22), malalignment of the prosthesis for 6% (n = 14), and fracture of the bone for 3% (n = 8). 49% (n = 114) of the revisions were performed on the right knee, and 51% (n = 120) on the left knee.
When a reoperation was performed, conversion to bi- or tricompartmental arthroplasty (TKA) was the most common procedure, totaling 197 (84%) re-operations. TC-3 or hinged implant was used in 20 cases (9%) and uni- to uni-revision was performed in 17 cases (17%).
Follow-up results for all primary operations
In the Kaplan-Meier analysis, UKAs showed a 73% (95% CI: 70–76) survival rate at 10 years.
Survival of UKA cohorts
At 10 years, UKAs implanted during the first period (1985–1990) showed a survival rate of 63% (95% CI: 55– 71), and UKAs implanted during the second period (1991–1996) showed a survival rate of 74% (95% CI: 70–79). Long-term follow-up data were not available for UKAs implanted during the last period (1997–2003); at 6-year follow-up, however, they had an 84% (95% CI: 78–89) survival rate. Kaplan-Meier analysis of UKAs indicated that the 1991–1996 cohort had better overall survival than the 1985–1990 cohort (p = 0.02). There were no differences in survival between the other cohorts. The Cox regression analysis (with or without adjustment for age and sex) gave similar results ().
Survival of UKA designs ()
At 7 years, only the Oxford menisceal bearing and the Miller-Galante unicondylar had survival rates over 85%. However, at 10 years survival rates for all UKA designs had declined to < 85%. In the Cox regression model (with or without adjustment for age and sex), both the Duracon and the PCA unicondylar implants were found to have an increased risk of revision as compared to the Oxford (; ).
Figure 2. Cox-adjusted survival curves of 1,736 UKAs in patients with primary osteoarthritis. UKA design served as the strata factor. The endpoint was defined as revision for any reason. Adjustment has been made for age and sex.
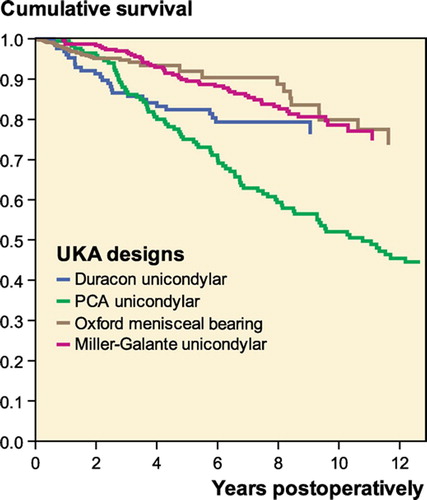
Table 4. Survival of UKA designs. The endpoint was defined as revision for any reason. 5-, 7-, and 10-year survival rates were obtained from the Kaplan-Meier analysis (n = 1,736)
Effect of gender and age on risk of revision
Cox regression analysis of all data showed that there was no significant difference in revision risk between males and females (with adjustment for age and type of UKA). Younger patients (≤ 65 years of age) were found to have a 1.5-fold (95% CI: 1.1–2.0) increased risk of revision as compared to patients of < 65 years (p = 0.04) (with adjustment for sex and brand of UKA).
The effect of hospital volume on survival of implants
Neither the Kaplan-Meier analysis nor the Cox multiple-regression analysis model revealed any significant difference in revision risk between hospitals performing ≤ 10 UKAs annually and hospitals performing < 10 UKAs annually (with adjustment for age, sex, and UKA design).
Discussion
The Finnish Arthroplasty Register was established in 1980 with the intent of tracking the use and failure rates of different implants. This populationbased study was designed to review outcomes of primary UKA implantation and evaluate the longterm durability of UKAs.
Nationwide studies enable trends in the use of UKAs to be shown more accurately and on a larger scale than studies from specialized centers. The limitations of register-based studies have been well defined (Paavolainen et al. Citation1991, Kim et al. Citation2002, Eskelinen et al. Citation2005). For example, we cannot report any subjective outcome measurements such as the Knee Society score or WOMAC; nor did we include quality of life evaluations such as the SF 36.
The choice and use of UKA has gone through a second peak at the start of the 21st century (). This is partly because of new prosthesis designs, a less invasive operation technique, and a good patient response with good long-term results compared to TKA or high tibial osteotomy (HTO) (Jenny et al. Citation1998, Argenson et al. Citation2002, Naudie et al. Citation2004, Price Citation2005). There was, however, a decrease in the number of UKAs over the period 1994–1999, due to poor outcomes of earlier designs (PCA unicondylar) and less rigorous selection of patients. When the modified Oxford menisceal bearing UKA (phase 3) was introduced in Finland in 1999, enthusiasm for its use began to rise and since the turn of the century, the number of UKAs implanted has progressively increased.
As much as 25% of all the UKAs were implanted in patients aged between 50 and 59 years. Being a younger group, they are more active, which places more demands on their prostheses. There is variation among hospitals performing UKAs in Finland. One reason for this may be that in some hospitals, UKAs have replaced HTOs in younger patients with medial compartment osteoarthritis. On the other hand, some hospitals seem to prefer the TKA over the UKA type due to poorer survival of the latter. In this study, most of the patients were females, but this should not have any clinical significance for the survival of UKAs (Kurtz et al. Citation2005).
Several studies have emphasized the importance of patient selection when performing either a UKA or an HTO (Scott and Santore Citation1981, Thornhill Citation1986, Iorio et al. Citation2003, Naudie et al. Citation2004). Gill and co-workers made the controversial statement that HTO should be superior to UKA. Moreover, if arthroplasty is required, one should favor the use of TKA implants (Gill et al. Citation1995). Similarly, in our hospital HTO is chosen for younger, active patients with unicompartmental medial osteoarthritis (Gill et al. Citation1995, Price et al. Citation2001) combined with a limb deformity, and who have a projected life expectancy of 20 years or more (Iorio et al. Citation2003). For other patients, we favor UKA or TKA.
There is also a group of older patients, with isolated medial compartment disease. Some orthopedic surgeons recommend that these patients should be treated with a UKA implant because of better rehabilitation (Price et al. Citation2001). The other point of view is to make a permanent solution for the elderly on the basis of their projected life expectancy and choose a TKA because of the better long-term implant survival rates.
Aseptic loosening has been one of the most common reasons for a revision (Robertsson et al. Citation1999, Robertsson Citation2000, Gioe et al. Citation2003). One cause of aseptic loosening is abrasion of the polyethylene matrix of the implant (Wright Citation2005). The Finnish Arthroplasty Register reports these phenomena separately, even though they are causally related. On the other hand, there have been reports concerning polyethylene wear in a menisceal bearing component, which was found to be minimal even in vivo (Argenson et al. Citation1992, Psychoyios et al. Citation1998, Robertsson Citation2001). A study showing abrasion of polyethylene over a range of 0.026–0.043 mm a year has been published (Argenson and O'Connor Citation1992). The Oxford menisceal bearing is the only knee prosthesis design among total and unicondylar prostheses providing identically compatible sliding surfaces. Thus, in theory this factor should be greatly beneficial to patients in terms of minimal polyethylene abrasion (Wright Citation2005). However, in a comparative nationwide register study in Sweden (Robertsson Citation2000), contrary to expectations, such a benefit was not reflected by any reduction in the cumulative revision rate (CRR) for the Oxford knee compared to others.
The Oxford unicondylar arthroplasty had the best survival rate in this study, but a word of caution is in order. In the Swedish arthroplasty register study (Robertsson et al. Citation2001), results from 1987–1998 showed that the Oxford mobile bearing had a significantly higher CRR than fixed-bearing models. Moreover, the higher CRR for the Oxford UKA was associated with hospitals with low surgical volume of prostheses replacement (Robertsson et al. Citation2001). In our study, the number of hospitals performing less than 10 operations a year has begun to increase during the past years. This may have a detrimental effect on survival rates in the years to follow. On the other hand, better survival rates have been obtained with fixed-plateau type UKAs (Rougraff et al. Citation1991, Argenson et al. Citation2002, Naudie et al. Citation2004). In a study of 160 Miller-Galante II unicondylar prostheses with a 3–10-year follow-up (Argenson et al. Citation2002), there was only one revision due to polyethylene wear at 9 years.
Clinical studies (Capra and Fehring Citation1992, Murray et al. Citation1998, Berger et al. Citation1999, Squire et al. Citation1999) on unicondylar arthroplasties with as much as a 20-year follow-up have achieved 98% survival rates at 10 years. There has only been one prospective, randomized comparison study between UKAs and TKAs, with the mid-term results published (Newman et al. Citation1998). In other studies, it is questionable whether patient selection and primary diagnoses are truly comparable—or whether the groups studied are equally paired. In an earlier study using a community-based implant register, Gioe et al. (Citation2003) obtained a 89% survival rate for a UKA at 10-year follow-up. In their study, revision for any reason was used as the endpoint. Similarly, using a population based-register Robertsson and co-workers (Citation1999) found an 85% survival rate for a UKA at 10-year follow-up. In the past decade, long-term survival rates for UKAs have been approaching the survival rates of TKAs (Deshmukh and Scott Citation2001).
In our study, when revision of the UKA was performed only 7% of the revised knees were actually replaced with a new UKA. Generally speaking, this is the correct approach because a significantly higher revision rate was reported after a UKA to a UKA revision, as compared to replacement of a UKA by a TKA (Robertsson Citation2000). Moreover, Lewold et al. (Citation1998) found that 4 years after a UKA to a UKA revision, one quarter of the patients required another revision operation. The same authors suggested that once it has failed, a UKA should be revised with a TKA. In our study, the most common cause of revision was aseptic loosening. Aseptic loosening and progression of knee osteoarthritis have also been the two most common reasons for a revision in previous registry-based studies (Robertsson et al. Citation1999, Robertsson Citation2000, Gioe et al Citation2003).
The survival rate of UKAs has improved in Finland. However, it seems that our results are not similar to those reported by surgeons designing UKAs, or to results from specialized centers (Price Citation2005). Based on the Swedish Arthroplasty Register, Robertsson et al (Citation2001) showed that the long-term results of UKA are related to the number of UKAs performed by a hospital. In particular, the survival rate of a technically demanding implant (Oxford) was most affected by volume in that hospital. Consequently, the risk of revision for the Oxford UKA was 3 times higher when surgery was performed in a low-volume unit. Although we measured no difference in revision risk between hospitals performing more than 10 UKAs and those performing less than 10 UKAs annually, it is reasonable to assume that the fact that the 400 UKAs implanted annually were decentralized over 40 different arthroplasty centers in Finland cannot lead to optimum longterm results. Thus, in order to increase the survival of UKAs in Finland, we do need centralization of arthroplasty surgery.
No competing interests declared.
Contributions of authors
EK: study design and writing. Ppa: study design and writing. AE: study design, data analysis and writing. Ppu: statistical supervision of the Arthroplasty Register, data analysis and writing. VR: study design and writing.
- Argenson J N, O'Connor J J. Polyethylene wear in meniscal knee replacement. A one to nine-year retrieval analysis of the Oxford knee. J Bone Joint Surg (Br) 1992; 74: 228–32
- Argenson J-N A., Chevrol-Benkeddache Y., Aubaniac J-M. Modern unicompartmental knee arthroplasty with cement. J Bone Joint Surg (Am) 2002; 84: 2235–9
- Bengtson S., Knutson K. The infected knee arthroplasty. A six-year follow-up of 357 cases. Acta Orthop Scand 1991; 62: 301–11
- Berger R A, Nedeff D D, Barden R M, Sheinkop M M, Jacobs J J, Rosenberg A G, Galante J O. Unicompartmental knee arthroplasty. Clinical experience at 6- to 10-year followup. Clin Orthop 1999, 367: 50–60
- Callahan C M, Drake B G, Heck D A, Dittus R S. Patients outcomes following unicompartmental or bicompartmental knee arthroplasty. J Arthroplasty 1995; 10: 141–50
- Capra S W, Fehring T K. Unicondylar arthroplasty. A survivorship analysis. J Arthroplasty 1992; 7: 247–51
- Cobb G A, Kozinn S C, Scott R D. Unicondylar or total knee replacement: the patient's preference. J Bone Joint Surg (Br) 1990; 72: 166–72
- Deschamps G., Lapeyre B. Rupture of anterior cruciate ligament: a frequently unrecognized cause of failure of unicompartmemntal knee prosthesis. Rev Chir Orthop Reparatrice Appar Mot 1987; 73: 544–51
- Deshmukh R V, Scott R D. Unicompartmental knee arthroplasty. Long-term results. Clin Orthop 2001, 392: 272–8
- Dorey F J. Survivorship analysis of surgical treatment of the hip in young patients. Clin Orthop 2004, 418: 23–8
- Drake B G, Callahan C M, Dittus R S, Wright J G. Global rating systems used in assessing knee replacement outcomes. J Arthroplasty 1994; 9: 409–17
- Eskelinen A., Remes V., Helenius I., Pulkkinen P., Nevalainen J., Paavolainen P. Total hip arthroplasty for primary osteoarthrosis in younger patients in the Finnish arthroplasty register. 4,661 primary replacements followed for 0-22 years. Acta Orthop 2005; 76: 28–41
- Eskelinen A., Remes V., Helenius I., Pulkkinen P., Nevalainen J., Paavolainen P. Uncemented total hip arthroplasty in young patients –a mid-to long-term follow-up study from the Finnish Arthroplasty Register. Acta Orthop 2006; 77: 57–70
- Espehaug B., Havelin L I, Engesaeter L B, Vollset S E, Langeland N. Early revision among 12,179 hip prostheses. A comparison of 10 different brands reported to the Norwegian Arthroplasty Register, 1987–1993. Acta Orthop Scand 1995; 66: 487–93
- Gill T., Schemitsch E H, Brick G W, Thornhill T S. Revision total knee arthroplasty after failed unicompartmental knee arthroplasty or high tibial osteotomy. Clin Orthop 1995, 321: 10–8
- Gioe T J, Killeen K K, Hoeffel D P, Bert J M, Comfort T K, Scheltema K., Mehle S., Grimm K. Analysis of unicompartmental knee arthroplasty in a communitybased implant registry. Clin Orthop 2003, 416: 111–9
- Goodfellow J W, Kershaw C J, D'A Benson M K, O'Connor J J. The Oxford knee for unicompartmental osteoarthritis. The first 103 cases. J Bone Joint Surg (Am) 1994; 76: 801–6
- Havelin L I, Vollset S E, Engesaeter L. B. Revision for aseptic loosening of uncemented cups in 4,352 primary total hip prostheses. A report from the Norwegian Arthroplasty Register. Acta Orthop Scand 1995; 66: 494–500
- Iorio R., Healy W L. Current concepts review. Unicompartmental arthritis of the knee. J Bone Joint Surg (Am) 2003; 7: 1351–64
- Jenny J Y, Tavan A., Jenny G., Kehr P. Long-term survival rate of tibial osteotomies for valgus gonarthrosis. Rev Chir Orthop Reparatrice Appar Mot 1998; 84: 350–7
- Kim Y H, Kook H K, Kim J S. Total hip replacement with a cementless acetabular component and a cemented femoral component in patients younger than fifty years of age. J Bone Joint Surg (Am) 2002; 84: 770–4
- Kurtz S., Mowat F., Ong K., Chan N., Lau E., Halpern M. Prevalence of primary and revision total hip and knee arthroplasty in the United States from 1990 through 2002. J Bone Joint Surg (Am) 2005; 87: 1487–97
- Lewold S., Robertsson O., Knutson K., Lidgren L. Revision of unicompartmental knee arthroplasty. Outcome in 1135 cases from the Swedish knee arthroplasty study. Acta Orthop Scand 1998; 69: 469–74
- Marmor L. The modular (Marmor) knee. Case report with a minimum follow-up of 2 years. Clin Orthop 1976, 120: 86–94
- Murray D W, Goodfellow J W, O'Connor J J. The Oxford medial unicompartmental arthroplasty: A ten-year survival study. J Bone Joint Surg (Br) 1998; 80: 983–9
- Naudie D., Guerin J., Parker D A, Bourne R B, Rorabeck C H. Medial unicompartmental knee arthroplasty with the Miller-Galante prosthesis. J Bone Joint Surgery (Am) 2004; 86: 1931–5
- Newman J H, Ackroyd C E, Shah N A. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg (Br) 1998; 80: 862–5
- Paavolainen P., Hamalainen M., Mustonen H., Slatis P. Registration of arthroplasties in Finland. A nationwide prospective project. Acta Orthop Scand (Suppl 241) 1991; 27–30
- Price A J. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop 2005, 435: 171–80
- Price A J, Webb J., Topf H., Dodd C A F., Goodfellow J W, Murray D W. Rapid recovery after Oxford Unicompartmental arthroplasty though a short incision. J Arthroplasty 2001; 16: 970–6
- Psychoyios V., Crawford R W, O'Connor J J., Murray D W. Wear of congruent meniscal bearings in unicompartmental knee arthroplasty. A retrieval study of 16 specimens. J Bone Joint Surgery (Br) 1998; 80: 976–82
- Puolakka T J, Pajamaki K J, Halonen P J, Pulkkinen P O, Paavolainen P., Nevalainen J K. The Finnish Arthroplasty Register: report of the hip register. Acta Orthop Scand 2001; 72: 433–41
- Robertsson O. Unicompartmental arthroplasty. Results in Sweden 1986–1995. Orthopade 2000; 29: S6–S8
- Robertsson O. Fixed bearing vs mobile bearing. J Bone J Joint (Br) (Suppl II) 2001; 109–10
- Robertsson O., Borgquist L., Knutson K., Lewold S., Lidgren L. Use of unicompartmental instead of tricompartmental prosthesis for unicompartmental arthrosis in the knee is a cost-effective alternative. Acta Orthop Scand 1999; 70: 170–5
- Robertsson O., Knutson K., Lewold S., Lidgren L. The routine of surgical management reduces failure after unicompartmental knee arthroplasty. J Bone J Surg (Br) 2001; 83: 45–9
- Rougraff B T, Heck D A, Gibson A E. A comparison of tricompartmental and unicompartmental arthroplasty for the treatment of gonarthrosis. Clin Orthop 1991, 273: 157–64
- Scott R D, Santore R F. Unicondylar unicompartmental knee replacement for osteoarthritis of knee. J Bone Joint Surg (Am) 1981; 63: 536–44
- Skolnick M D, Bryan R S, Peterson L F A. Uniconpartmental polycentric knee arthroplasty. Description and preliminary results. Clin Orthop 1975, 112: 208–14
- Squire M W, Callaghan J J, Goetz D D, Sullivan P M, Johnston R C. Unicompartmental knee replacement. A minimum 15 year follow-up study. Clin Orthop 1999, 367: 61–72
- Thornhill T S. Unicompartmental knee arthroplasty. Clin Orthop 1986, 205: 121–31
- Wright T M. Polyethylene in knee arthroplasty: what is the future?. Clin Orthop 2005, 440: 141–8