Abstract
Background Bone morphogenetic proteins (BMPs) have the potential to improve incorporation of allograft bone in revision surgery. This could result in improved fixation and graft incorporation.
Patients and methods We evaluated the effect of mixing OP-1 (BMP-7) with morselized allograft in hip revisions. In a case-control study, 20 acetabular revisions (10 in the study group, 10 controls) and 41 femoral revisions (11 in study group, 30 controls) were done using impaction allografting. The migration of the cups and stems was studied with radiostereometric analysis (RSA) for up to 5 years. Changes of bone mineral density around the femoral component were measured with dual energy X-ray adsorptiometry for 2 years. Bone remodeling and the extent of radiolucent lines were evaluated on conventional radiographs after 5 years. The clinical results were documented using Harris hip score.
Results In the cup study, there was no significant difference in implant migration between the study and control groups. 4 sockets in the study group were classified as radiographically loose after 5 years and 2 of them were revised after 5 years. After 2 years, the stems in the study group showed slightly increased posterior tilt (0.3°, p = 0.03). 1 stem in the study group loosened and was revised during the third year of observation.
Interpretation The sample size and study design in our evaluation did not allow any firm conclusions. Absence of any trend to improved fixation and early revisions in the study group prompted us to stop recruitment to this study. ▪
Implant loosening is associated with loss of bone mass and the remaining surrounding bone is often osteoporotic. During surgery, poor bone stock may be addressed by the use of bigger or longer implants, transplantation of bone tissue or bone substitutes, or various combinations of these methods. To facilitate healing of the graft and additional regeneration of host bone, local use of hormones, osteoclast inhibitors or growth factors may be attractive options (Bolder et al. Citation2003, Cook et al. Citation2003, Åstrand and Aspenberg Citation2004). Mixing of such substances with bone chips may be one way of facilitating postoperative rehabilitation and long-term results after revision surgery. BMP-7 is one of several growth factors with the potential to improve incorporation of allograft bone; it became available for clinical trials during the late 1990s.
BMP-7 or Osteopontin (OP, Stryker Biotech, Montreux, Switzerland) belongs to the transforming growth factor family. It stimulates recruitment of stem cells and vascular ingrowth, resulting in bone formation. It has proved to be effective in animal models, and as effective as autograft in the treatment of tibial nonunions and posterolateral fusions of the spine (Friedlaender et al. Citation2001, Blattert et al. Citation2002, Johnsson et al. Citation2002, Cook et al. Citation2003, Einhorn Citation2003). Case reports have indicated that the use of BMPs may also be beneficial in conjunction with use of allograft bone in revision surgery (Cook et al. Citation2001), and that this substance may possibly improve the results of impaction allografting of the femur. In a pilot study, we evaluated the effects of BMP on component fixation and bone remodeling after mixing OP-1 (Stryker Biotech) with morselized allograft bone during impaction grafting in hip revision surgery. We hypothesized that addition of this growth factor would facilitate implant fixation and improve mineralization of the transplanted graft.
Patients and methods
During a period of 1 year, 14 consecutive patients (10 acetabular and 11 femoral revisions) were treated with impaction allografting (study group S, and ). After each procedure, the surgeon filled in a form concerning the amount of allograft used and estimated the implant/living bone contact for the acetabular component. From a database including 160 revisions followed with radiostereometry, 1 control case for each acetabular revision and 2–3 control cases for each femoral revision were chosen. The control cases (C) were matched for sex, age, type of defect, type of implant (cemented/uncemented) and volume of allograft used, as measured or estimated by the surgeon during the operation.
Table 1. Cup study. 10 hips with OP–1 mixed into the allograft (study group) and 10 controls. Median (range)
Table 2. Stem study. 11 hips with OP-1 mixed into the allograft (study group) and 30 controls. Median (range)
On the acetabular side, the percentage contact between implant and living host bone was also considered when looking for suitable control cases. Because of the high number of variables used at this procedure, only 1 control case with revised socket was found for each study case. On the femoral side, control cases were selected from the same database based on use of the same implant design (Spectron EF; Smith & Nephew, Memphis,TN, USA), use of impaction grafting and at least 55 mL bone graft (the minimum for the study group) and presence of postoperative DEXA and radiostereometric examinations. 30 femoral revisions fulfilled these criteria ().
On the acetabular side, a plate was used in one patient (control group, cemented fixation) with a rim defect. Central defects were covered with a metallic net (1 study, 1 control case) or a bone bloc (5 S, 3 C) from the donated femoral head, which was shaped using chisels and an air-powered saw. The bone blocs were used to cover defects in the medial wall of the acetabulum and were not meant to carry any substantial amount of load.
The femoral heads were milled using a Tracer mill (maximum aperture barrel, Ossano, 9 S, 9 C) or an air-powered mill (Synthes-Stratec, Switzerland; 1 S, 1 C). 1 unit of BMP-7 (3.5 mg) was added to each femoral head used. Impaction grafting was done using a combination of impactors, punches and the reversed reaming technique. Cemented Reflection (Smith & Nephew) and Palacos with gentamicin (Schering Plough, Belgium) or uncemented and hydroxyapatite/tricalcium phosphatecoated Harris-Galante II/Trilogy cups (Zimmer, Warsaw, IN, USA) with additional screw fixation were used (). In 1 case, the pubic bone fractured during removal of an uncemented cup with pelvic osteolysis. The fracture healed without any signs of instability (proximal migration according to RSA of 0.1 mm at 5 years).
On the femoral side, defects were covered with metallic net in 9 cases (3 S, 6 C). Our impaction technique corresponded to the one described by Gie et al. (Citation1993), except for the use of polished rotating reamers during the initial phase of impaction in 24 cases (11 S, 13 C) (Höstner et al. Citation2001). In 2 cases (control group), whether this technique or the conventional technique was used had not been recorded. The air-powered bone mill was used in 2 cases in each group, and the Tracer mill in the remaining cases. The patients were mobilized the day after the operation. They were instructed to bear partial weight using two crutches for 3 months.
During the operation, tantalum markers were inserted into the acetabulum, the polyethylene cup or liner, and the proximal femur. 37 of the stems were supplied with titanium towers inserted into the prosthetic shoulder, tip and collar. In these stems, both proximal/distal migration and stem rotations could be studied. Premarked stems were not available to us for a short period. In four stems operated during this period (4 C), we could only study the migration of the center of the femoral head. Radiostereometric examinations were done postoperatively (median 8 days, range 3–10 days) after 3 and 6 months, and 1, 2 and 3 years after the operation.
During the initial part of this study, we measured analog radiographs manually. Later on, a new technique based on measurements of digital radiographs was used. This technique is more precise than manual measurements (Börlin et al. Citation2002). Computation of the three-dimensional marker positions and implant motions between examinations was done using UMRSA (RSA Biomedical, Umeä, Sweden).
The precision of our radiostereometric measurements of the acetabular component was studied in 60 examinations repeated at an interval of about 15 min. 30 measurements were manual and 30 were digital. The error was expressed as 99% confidence interval. The data obtained—medial/lateral, proximal/distal, anterior/posterior translations and rotations around the corresponding axes—were 0.29, 0.17 and 0.47 mm and 0.92, 1.21 and 0.35°, respectively, using the manual technique. The corresponding data for the digital measurements were 0.15, 0.15, 0.28 mm and 0.70, 0.27 and 0.41°, respectively. The precision of manual measurements on the stem side has been studied previously (Kärrholm et al. Citation1999). On the femoral side, measurements of bone mineral density (Lunar DPX-IQ, GE Healthcare, Diegem, Belgium) were done postoperatively after 6 months, 1 year and 2 years. The precision of these studies has been reported (Kärrholm et al. Citation1999).
Conventional radiographic examinations (AP, lateral and pelvic views) were done postoperatively and at 1, 2, 3 and 5 years. In this paper, only the results of comparison between the postoperative examination and the 5-year follow-up are described. We evaluated the presence of radiolucent lines and graft remodeling in the 6 cup and 14 stem regions according to Hultmark et al. (Citation2003) and Gruen et al. (Citation1979). To reduce the amount of data presented, the results for each implant were simplified to represent the entire interface on the AP and lateral view of the corresponding periprosthetic regions. The implants were classified as “definitely loose” if there was complete radiolucency on one or both projections, obvious displacement and/or visible fracture of the cement. Clinical evaluation was done preoperatively after 1, 2, 3 and 5 years. The preoperative results and those obtained after 2 and 5 years are presented. On the acetabular side, statistical evaluation of results obtained at 5 years and on the femoral side at 2 years (before any revision) and 5 years was done. Non-parametric tests were used.
Results
Cup study
During the study period there were no cup revisions. In both groups, there was an early proximal migration (median values of 0.4 and 0.2 in study and control groups, respectively, at 3 months) followed by stabilization of most implants. At 5 years, the median migration had increased to 0.7 and 0.3 mm in the two groups, without any statistically significant difference (p = 0.4). There were no statistically significant differences between the other migration parameters either (medial/lateral, anterior/posterior translations and rotations) (p < 0.6, ).
Table 3. Cup study. Migration data in OP-1 treated hips (study group, n=10) and controls (n=10) at 5-year follow-up. Median (range)
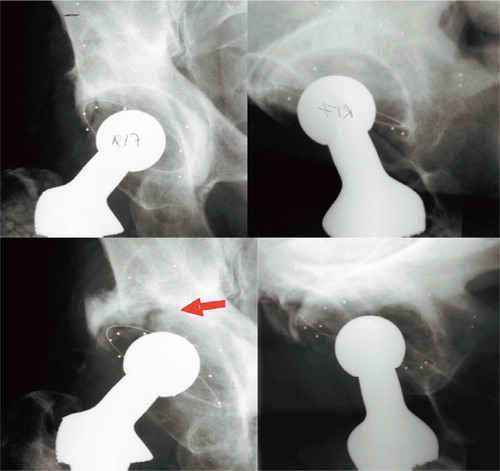
At 2 years, 5 cups in the study group and 3 in the control group had migrated 0.5 mm or more proximally (). 2 of these, both cemented cups in the study group, were subsequently revised—1 after 5 years and 3 months and the second after 6 years—because of loosening. At 5 years, these 2 cups had migrated 5.5 and 4.2 mm proximally. Both patients developed moderate pain during activity. 1 of them showed progressive tilting (26 degrees increased inclination according to RSA) and also had a feeling of instability. Conventional radiographs showed graft resorption and displacement, but the radiolucent lines only embraced about 50% of the interface. In the second loose cemented socket the cement had fractured at the pool of the cup, which, with the proximal-lateral part of the cement mantle, dislodged proximally and somewhat laterally (). The proximal part of the graft had resorbed, whereas the medial and distal parts of the graft bed seemed to be inte-At 2 years, the Harris hip score was higher in the grated with no radiolucency between the remaining study group (p = 0.02), but the gain value (differpart of the cement mantle and/or the host bone and ence preoperatively – 2 years) and the pain score the graft. Both of these revised cups were found to were similar (). be extremely loose at the revision.
Figure 1. Proximal migration of cemented (Ce) and uncemented (UCe) revision sockets used with impacted allograft mix with OP-1 (black) and without OP-1 (green).8 cases with at least 0.5 mm of migration at 3 years are illustrated.
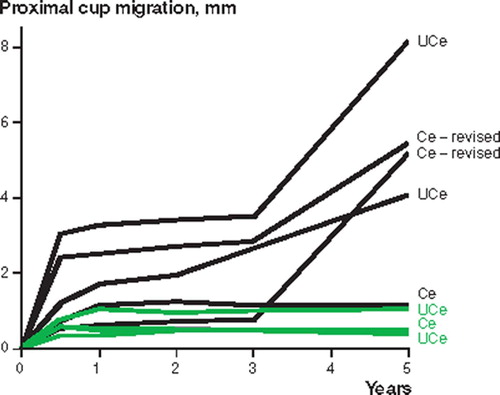
Figure 2. Acetabular revision in a 78-year-old man operated with impaction grafting mixed with OP-1, and a cemented Reflection cup.Upper left and right: postoperative AP and lateral views.After 5 years (lower left and right) the graft had disappeared proximally and medially (see lateral view), the cement mantle had fractured (arrow), and the metallic indicator had loosened and become deformed.The center of the socket migrated 4.8 mm laterally and 4.2 mm proximally.At revision, the cup was found to be loose and the proximal graft bed had resorbed. Distal to the cement fracture, the cement mantle was fixed to the graft bed, which seemed to have integrated into the underlying host bone.
The patient with the most pronounced proximal migration at 5 years (8.2 mm) had a loose uncemented cup radiographically and moderate hip symptoms, but no revision has been planned to date. In addition, 1 uncemented cup in the study group was classified as loose from conventional radiographs (). These 2 press-fit cups had complete or almost complete radiolucent lines on the AP or lateral view.
Table 4. Cup study. Radiographic results at 5 years. The 4 cups classified as loose, including the 2 subsequently revised cases, had radiolucent lines to various extents with or without pronounced migration or cement fracture (1 case, see ). Values are number of hips
At 2 years, the Harris hip score was higher in the study group (p = 0.02), but the gain value (difference preoperatively – 2 years) and the pain score were similar ().
Stem study
In both groups, the mean and median subsidence increased up to 2 years after the operation (, ). Between the 2-year and 3-year follow-up, 2 stems were revised in the study group. Between 3 and 5 years, the remaining 9 cases displayed proximal-distal migration of less than ± 0.1 mm. In the control group, 9 of 30 stems subsided above our detection limit for RSA measurements (observed range: −0.2 to −6.1). In both groups, the stem showed small median rotations posteriorly (around the transverse axis) and into retroversion (around the longitudinal axis). In both groups, the varus/valgus rotations were close to or zero. Increased retroversion was observed in the study group, both before (at 2 years) and after (at 5 years) exclusion of the 2 revised cases (p = 0.03).
Figure 3. Proximal/distal migration of the stem (mean, SE). Because of massive subsidence, the 2 loosenings have a considerable influence on the mean values before revision (arrows). Black: study group; green: controls.
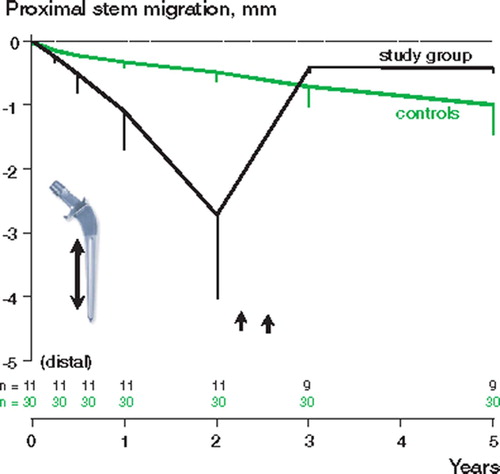
Table 5. Stem study. Migration data in OP-1 treated hips (study group) and controls before any revision (2 years) and after 5 years. Median (range)
Both patients who were subsequently revised had experienced sudden pain during the postoperative year. RSA revealed continuous subsidence, which increased from 0.8 and 3.2 mm at 6 months to 10.9 and 16.1 mm at 2 years. At this follow-up, both stems showed posterior tilt (−0.65°, −4.5°) and retroversion (23.7°, 29.5°), whereas one had tilted into varus (−5.1°) and the other into valgus (3.8°). Both were revised before the 3-year follow-up. Radiographs at 2 years showed allograft resorption and fracture of the cement combined with a medial or lateral dislocation of the stem tip.
At the revision the stems were easily removed. There were small traces of loose particles in the canal, and the inside of the femur was rougher than during the first revision because parts of the bone graft seemed to have healed to the endocortex. 1 stem was revised using a longer cemented stem and impaction grafting. The other patient received a longer cemented stem without any grafting.
2 patients in the control group suffered femoral fractures distal to the tip of the stem after a fall on plain ground. Both fractures occurred between 3 and 6 months after the index operation. They were treated with open reduction and plates. RSA up to 5 years revealed proximal (+)/distal (−) migration of 0.5 and −0.4 mm.
At 5 years, none of the 9 remaining stems in the study group were classified as loose. In the control group, 2 of the stems in the 29 patients who attended were classified as loose. According to RSA, these stems showed the most pronounced distal migration of the 38 remaining cases (13.5 and 6.6 mm). The first case showed proximal cementstem separation, cement mantle fracture and progressive osteolysis. Despite having symptoms, the patient was not interested in revision but changed his mind 2 years later. The second patient had complete lines in 5 of 7 Gruen regions on AP view and a complete line on the lateral view, but no symptoms ().
Table 6. Stem study. Radiographic results at 5 years. Values are number of hips
After 6 months the median bone mineral density had decreased proximally (Gruen regions 1–4) in the controls, whereas the study group showed a more variable pattern (). In region 6, the study group showed a minimum median increase (study vs. control group: p = 0.04) and less bone loss in region 7 (p = 0.03) than seen in the controls. Distally, there were no differences. After 2 years and before any revision, the divergent pattern of bone mineral changes in regions 6 and 7 had disappeared. In the study population the density did, however, continue to decrease distal to the tip of the stem (region 4), whereas it increased in the controls (study vs. control group: p = 0.04).
Table 7. Stem study. Change of bone mineral density (%) in 11 OP-1 treated hips (study group) and 27 controls. Three hips in the control group could not be analyzed because of plates and screws (n=2) or technical failures. Median (range)
The Harris hip and pain scores and the gain values 0–2 years were similar ( and ).
Discussion
Graft remodeling after the impaction procedure involves a complicated sequence of biological events which have only been partly characterized to date. According to biopsy and retrieval studies (Ullmark and Obrant Citation2002), minimum bone formation may be initiated 1 month after implantation. After 8–11 months, the osteoid/bone layer might have a thickness of 3–5 mm. After 2 years, there is mainly bone with hematopoietic marrow (Ullmark and Linder Citation1998, Linder Citation2000). The grafted bone will thus be slowly replaced with living bone. At some locations—and probably those that do not carry load—the graft will be resorbed and may not be replaced with living bone. Sörensen et al. (Citation2003) used PET to study bone metabolism and blood flow in the impacted area around cemented femoral stems up to 1 year after the operation. As early as 8 days after the operation, blood flow and bone formation were demonstrated adjacent to the allograft. After 1 year, bone formation was found close to the cement mantle.
The key to success with the impaction grafting technique is to obtain sufficient primary stability, and to make sure that this stability is maintained during the phase of revitalization of the graft. According to the studies that have been published, this remodeling phase takes at least 1 year, and probably longer depending on the thickness of the graft bed. If there is rapid revascularization, resorption that is too fast might jeopardize the stability. According to Jensen et al. (Citation2002), OP-1 may enhance bone formation in dogs, but also accelerates bone resorption in the early phase after grafting.
Jeppson et al. (2003) studied bone formation in rats using a conduction chamber. They observed reduced ingrowth into graft mixed with OP-1 if the bone graft had also been treated with clodronate, and they concluded that resorption of the graft is necessary before any substantial new bone formation can take place. Søballe et al. (Citation2004) studied the effects of mixing allograft with OP-1 in a canine revision model. Interestingly, they found improved implant fixation without any addition of OP-1 on the side simulating a primary arthroplasty, but they found the opposite on the other side where they had created a situation that was meant to simulate a revision. They speculated that the impaired bone bed changed the balance between resorption and formation in favor of more rapid bone formation and mineralization.
Our study was not quite conclusive concerning the effect of OP-1, but our data do not indicate any positive effect of clinical relevance. When performing impaction grafting in a clinical revision situation, more micromotions of the stem were found with use of OP-1, resulting in 2 early re-revisions. On the acetabular side, there was no significant difference. At 5 years, the magnitude of median proximal migration was nonetheless more than twice as high mainly due to outliers, which sub-sequently loosened. To date, 2 of these cups have been revised because of clinical symptoms.
Changes of bone mineral density (BMD) in the graft bed could be an effect of revascularization, resulting in either resorption or increased mineralization of the graft—or a combination of these two events. Theoretically, resorption may also be caused by dissolution in an acid environment, but any substantial dissolution of the graft in the proximal femur during the postoperative year for this reason is probably rare. In a previous study, we observed that revision stems operated with impacted bone graft and cement lose BMD in the proximal regions up to 6 months. Thereafter, the BMD increases up to roughly postoperative values between 6 months and 1 year, suggesting revitalization of the graft by a process of resorption followed by formation of new bone.
Measurements of bone mineral density in our study group indicated increased density in Gruen regions 6 and 7 after 6 months, but this effect disappeared with longer follow-up, making the relevance of its clinical importance uncertain. Interestingly, the part of the graft bed that might be supposed to carry least load (Gruen region 4) had lost more density at the last follow-up.
The comparatively small effect of OP-1 when used in our clinical application can probably be explained by a more rapid revascularization and faster graft resorption. The graft remodeling and new bone formation that follows may not be fast enough to secure implant stability in some patients.
We used one package (device) of OP-1 for each femoral head, according to the instructions of the manufacturer. During the first operation, a representative of the company was also present to make sure that the mixing procedure was done according to the instructions. The size and bone quality of femoral heads may, however, vary as well as the impaction technique. It may be that choice of another dosage would have yielded a different result, but as far as we know, the effect of dose variations in humans has not been studied.
Other variables such as type of stem or socket implanted, graft size and treatment, and (not least) impaction technique may have more or less of an influence on the results (Höstner et al. Citation2001, van Doorn et al. Citation2002, Bolder et al. Citation2003, Cornu et al. Citation2003a, Citationb, Jeffery et al. Citation2003). In this study we tried to reduce the effect of these confounders by use of a control group. Even if the matching was not perfect, we believe that it was acceptable—not least because of the complexity and high numbers of variables to consider in these cases.
Even so, some influence of bias cannot be completely ruled out. From a theoretical standpoint, our study could be influenced by selection, surgical bias and evaluation bias. More difficult cases could have been selected to one of the groups and surgeons with less experience could have been over- or under-represented in the study and control groups, respectively. We tried to address these possible problems by performing the study cases consecutively and by other measures such as classification of bone defects and measurements of graft volume described above. Another—and perhaps more important—confounder in our study is that the observations on the acetabular and femoral sides were not independent, since many hips were operated on both sides. Thus, if the patients in the study group were more or less susceptible to loosening for any reason, this patient-related effect could influence the observations positively or negatively on both sides. This problem can only be properly addressed using two completely different study populations, which are evaluated in a randomized comparison.
The background variables in our study were strictly related to the patient demographics and surgical technique used at our hospital. It may be that the results could have been different if we had used harder impaction or—as suggest by Bolder et al. (Citation2003)—bigger bone chips in the acetabulum. Use of harder impaction may increase the risk of fracture, however (Ornstein et al. Citation2002). In our first 100 cases with impaction grafting of the femur, and with at least 5 years of follow-up, the overall re-revision rate due to loosening was 3%, suggesting acceptable surgical technique (unpublished observation). On the acetabular side it is higher, which has made us change to the use of larger handmade chips.
Mixing of OP-1 with morselized allograft did not improve the early fixation of either the acetabular or the femoral component. The dosage of OP-1 used was as recommended by the manufacturer, but even so, could not have been optimal. Despite the fact that more cases, longer follow-up and a randomized study design are desirable in order to be able to reach definite conclusions, the early clinical failures prompted us to stop this study.
Financial support was obtained from the Swedish Research Council, the Neubergh Research Foundation, the IngaBritt and Arne Lundberg Foundation, and also from Smith & Nephew Inc., USA, and Stryker Biotech Inc., USA.
Author contributions
JK operated half of the patients, collected all data and wrote the manuscript. PH, JT, RR performed the radiologic evaluation.
- Blattert T R, Delling G, Dalal P S, Toth C A, Balling H, Weckbach A. Successful transpedicular lumbar interbody fusion by means of a composite of osteogenic protein-1 (rhBMP-7) and hydroxyapatite carrier: a comparison with autograft and hydroxyapatite in the sheep spine. Spine 2002; 27(23)2697–705
- Bolder S B, Verdonschot N, Schreurs B W, Buma P. The initial stability of cemented acetabular cups can be augmented by mixing morsellized bone grafts with tricalciumphosphate/hydroxyapatite particles inbone impaction grafting. J Arthroplasty 2003; 18(8)1056–63
- Börlin N, Thien T, Kärrholm J. The precision of radiostereometric measurements. Manual vs. digital measurements. J Biomech 2002; 35(1)69–79
- Cook S D, Barrack R L, Shimmin A, Morgan D, Carvajal J P. The use of osteogenic protein-1 in reconstructive surgery of the hip. J Arthroplasty 2001; 16(8)88–94, (Suppl 1)
- Cook S D, Barrack R L, Patron L P, Salkeld S L. Osteoinductive agents in reconstructive hip surgery: a look forward. Clin Orthop 2003, 417: 195–202
- Cornu O, Bavadekar A, Godts B, Van Tomme J, Delloye C, Banse X. Impaction bone grafting with freezedried irradiated bone. Part I. Femoral implant stability: cadaver experiments in a hip simulator. Acta Orthop Scand 2003a; 74(5)547–52
- Cornu O, Bavadekar A, Godts B, Van Tomme J, Delloye C, Banse X. Impaction bone grafting with freezedried irradiated bone. Part II. Changes in stiffness and compactness of morselized grafts: experiments in cadavers. Acta Orthop Scand 2003b; 74(5)553–8
- Einhorn T A. Clinical applications of recombinant human BMPs: early experience and future development. J Bone Joint Surg (Am) 2003; 85(3)82–8, (Suppl)
- Friedlaender G E, Perry C R, Cole J D, Cook S D, Cieruy G, Muscklen G F, Zyck G A, Calham J H, La Forte A J, Yiu S. J Bone Joint Surg (Am) 2001; 83: S151–8, (Suppl 1 (Pt 2))
- Gie G A, Linder L, Ling R S, Simon J P, Slooff T J, Timperley A J. Contained morselized allograft in revision total hip arthroplasty. Surgical technique. Orthop Clin North Am 1993; 24(4)717–25
- Gruen T A, McNeice G M, Amstutz H C. ”Modes of failure” of cemented stemtype femoral components: a radiographic analysis of loosening. Clin Orthop 1979, 141: 17–27
- Gustilo R B, Pasternak H S. Revision total hip arthroplasty with titanium ingrowth prosthesis and bone grafting for failed cemented femoral component loosening. Clin Orthop 1988, 235: 111–9
- Hultmark P, Höstner J, Herberts P, Kärrholm J. Radiographic evaluation of Charnley cups used in first-time revision: repeated observations for 7–15 years. J Arthroplasty 2003; 18(8)1005–15
- Höstner J, Hultmark P, Kärrholm J, Malchau H, Tveit M. Impaction technique and graft treatment in revisions of the femoral component: laboratory studies and clinical validation. J Arthroplasty 2001; 16(1)76–82
- Jeffery M, Scott G, Freeman M. Failure of an uncemented non-porous metal-backed prosthesis with augmentation using impacted allograft for acetabular revision 12- to 17-year results. J Bone Joint Surg (Br) 2003; 85(2)182–6
- Jensen T B, Overgaard S, Lind M, Rahbek O, Bunger C, Søballe K. Osteogenic protein 1 device increases bone formation and bone graft resorption around cementless implants. Acta Orthop Scand 2002; 73(1)31–9
- Jeppsson C, Åstrand J, Tägil M, Aspenberg P. A combination of bisphosphonate and BMP additives in impacted bone allografts. Acta Orthop Scand 2003; 74(4)483–9
- Johnsson R, Strömqvist B, Aspenberg P. Randomized radiostereometric study comparing osteogenic protein-1 (BMP-7) and autograft bone in human noninstrumented posterolateral lumbar fusion: 2002 Volvo Award in clinical studies. Spine 2002; 27(23)2654–61
- Kärrholm J, Hultmark P, Carlsson L, Malchau H. Subsidence of a non-polished stem in revisions of the hip using impaction allograft. Evaluation with radiostereometry and dual-energy X-ray absorptiometry. J Bone Joint Surg (Br) 1999; 81(1)135–42
- Linder L. Cancellous impaction grafting in the human femur: histological and radiographic observations in 6 autopsy femurs and 8 biopsies. Acta Orthop Scand 2000; 71(6)543–52
- Ornstein E, Atroshi I, Franzen H, Johnsson R, Sandquist P, Sundberg M. Early complications after one hundred and forty-four consecutive hip revisions with impacted morselized allograft bone and cement. J Bone Joint Surg (Am) 2002; 84(8)1323–8
- Søballe K, Jensen T B, Mouzin O, Kidder L, Bechtold J E. Differential effect if a bone morphogenetic protein-7 (OP-1) on primary and revision loaded, stable implants with allograft. J Biomed Mater Res 2004; 71 A(4)569–76
- Sörensen J, Ullmark G, Långstrom B, Nilsson O. Rapid bone and blood flow formation in impacted morselized allografts: positron emission tomography (PET) studies on allografts in 5 femoral component revisions of total hip arthroplasty. Acta Orthop Scand 2003; 74(6)633–43
- Ullmark G, Linder L. Histology of the femur after cancellous impaction grafting using a Charnleyprosthesis. Arch Orthop Trauma Surg 1998; 117(3)170–2
- Ullmark G, Obrant K J. Histology of impacted bonegraft incorporation. J Arthroplasty 2002; 17(2)150–7
- van Doorn W J, ten Have B L, van Biezen F C, Hop W C, Ginai A Z, Verhaar J A. Migration of the femoral stem after impaction bone grafting. First results of an ongoing, randomised study of the exeter and elite plus femoral stems using radiostereometric analysis. J Bone Joint Surg (Br) 2002; 84(6)825–31
- Åstrand J, Aspenberg P. Topical, single dose bisphosphonate treatment reduced bone resorption in a rat model for prosthetic loosening. J Orthop Res 2004; 22(2)244–9