Abstract
Background The lateral collateral ligament complex is the key structure involved in recurrent elbow instability. Treatment is surgical, by repair or reconstruction of the lateral collateral ligament complex. We evaluated the effect of arthroscopic electrothermal shrinkage for treatment of chronic posterolateral rotator elbow instability.
Methods 21 patients, median age 32 (24–50) years, suffering from chronic lateral elbow instability underwent arthroscopic electrothermal ligament shrinkage with a bipolar shrinkage probe. All patients were available for follow-up after median 30 (8–48) months.
Results No complications were seen. The Morrey score increased from 40 to 77 points. The result was moderate (50–80 points) in 10 patients, and in the other patients a good result was achieved (80–95 points). The manual stress radiography showed a mean lateral joint opening of 13 (8–18) mm preoperatively. During follow-up, it decreased to 2 (1–4) mm.
Interpretation Our findings suggest that arthroscopic bipolar ligament shrinkage is sufficient for the treatment of chronic posterolateral rotator elbow instability.
The elbow is the second most common joint to become dislocated in adults. Dislocations represent 11–28% of total elbow injuries, with an annual incidence of 6–8 cases per 100,000 people (Hildebrand et al. Citation1999). Most of them occur from a fall onto an outstretched hand, especially during sports activities.
Simple dislocations are treated with closed reduction and a short period of immobilization (Lansinger et al. Citation1984, Josefsson et al. Citation1987, Schippinger et al. Citation1999). In only 2%, chronic instability develops (Rieunau et al. Citation1972). Chronic elbow instability without fractures in adults can be of 3 types: (1) valgus instability, (2) posterolateral rotator instability, and (3) isolated radial head instability (Lee and Rosenwasser Citation1999). The valgus instability is usually the result of over-use in throwing athletes. Isolated radial head instability is rare.
Posterolateral rotator instability is usually the result of a complete or incomplete elbow dislocation (O'Driscoll et al. Citation1991). The lateral collateral ligament complex is the key structure involved in recurrent elbow instability. Treatment is surgical, by repair or reconstruction of the lateral collateral ligament complex—specifically the ulnar part (O'Driscoll Citation1999, McKee et al. Citation2003).
Thermal shrinkage of the glenohumeral joint capsule is an established arthroscopic method for treatment of recurrent shoulder dislocation (Jackson Citation1999, Lyons et al. Citation2001). It is also possible to shrink elongated cruciate ligaments (Carter et al. Citation2002, Wienecke and Lobenhoffer Citation2003, Dodds et al. Citation2004) or elongated grafts (Spahn and Schindler Citation2002). The application of thermal energy can be performed with laser energy or using monopolar or bipolar electromagnetic energy. In this prospective study, we evaluated the outcome of thermal shrinkage for the treatment of chronic posterolateral elbow instability.
Patients and methods
Patients
In a prospective study, 21 patients (mean age 34 (24–50) years, 12 males) who had been suffering from chronic lateral elbow instability for more than 6 months—mean 13(6–24) months—underwent arthroscopic electrothermal shrinkage and were followed for mean 30 (8–48) months. 10 patients had suffered from an elbow dislocation, all treated by closed reduction and short immobilization. The other patients had suffered a severe elbow sprain. The diagnosis of instability was based on history (dislocation or substantial injury), complaints (a feeling of radial instability), positive clinical tests, and stress radiography. In all patients, the lateral pivot shift test (according to O'Driscoll et al. (Citation1991)) was positive and the lateral joint opening was 6 mm or more at manual varus stress radiography (Hempfling Citation1995).
The preoperative findings and outcome were rated using the Morrey score (Morrey Citation1985). This score covers 5 items: pain (30 points), strength (15 points), motion (37 points), instability (6 points), and function (12 points). Manual stress radiography was performed in sitting position and flexion of 25°. All manual stress radiography was performed by the senior author, and analyzed according to Eygendaal at al. (Citation2000), who described this technique for evaluation of ulnar instability. In our modification, we measured the distance in mm between the most distal point of the curved contour of the capitulum and the radial head by radioscopic view. A distance of more than 6 mm was defined as lateral instability, as suggested by Morrey (Citation1985). The stress radiography was always performed before anesthesia.
Standard radiographs and MRI were performed in all cases, but these evaluations gave no additional information.
Operation technique
All operations were performed under general anesthesia in the prone position (the patient is positioned face down with the shoulder abducted 90°). The prone position allows unlimited pronation and supination during the shrinkage procedure. A pneumatic tourniquet (250 mm Hg) was applied.
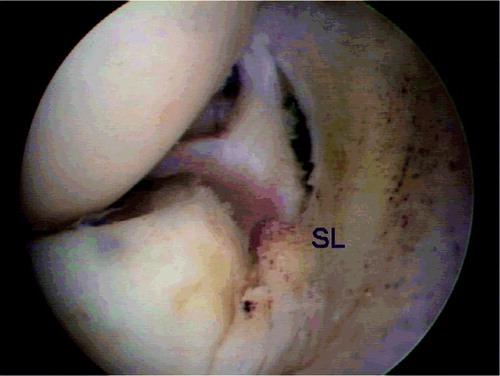
We used the anteromedial and the anterolateral standard portal for arthroscopic ligament shrinkage. A high anteromedial portal is not necessary. The dorsal joint space was inspected through a low posterolateral portal. For resection of an olecranon osteophyte, an additional posterocentral portal was used in 1 patient. The fluid inflow was limited by using a pump (80 mm Hg) to reduce fluid irrigation into the soft tissues and to avoid edema. After diagnostic inspection and optional arthroscopic surgery (Table), the elongated lateral ligamentous-capsular complex was inspected (). In the case of lateral instability, the joint space is abnormally wide.
Figure 1. Arthroscopic view of the lateral joint space. The elongation of the lateral ligamentous complex is quite obvious. RH: radial head; C: capitulum.
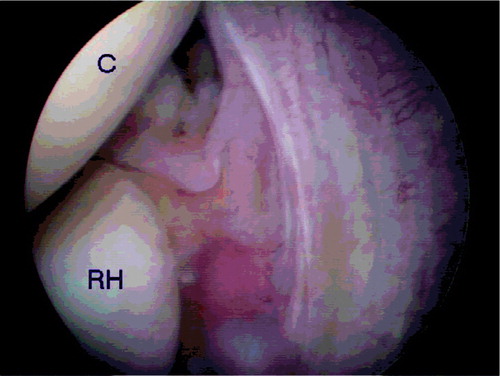
The thermal shrinkage was carried out using a bipolar application probe (Arthrocare system; Arthrocare Europe AB, Stockholm, Sweden) with an output of 284 W (). The procedure started in the ventral part of the ligamentous complex. The probe was moved across the lateral capsuloligamentous complex. The temperature is continually monitored by the apparatus. The tissue is examined visually and by probing during the shrinkage procedure. Response is confirmed visually through alteration in color of the tissue (this appears yellower and flatter) and by visible shrinkage of the capsule. Finally, the joint space is tight and the ligamentous complex is tight during hook palpation (), and the clinical evaluation demonstrates a negative pivot shift test. During the shrinkage procedure, the surgeon applies a mild manual varus stress to approximate the lateral ligamentous complex.
Rehabilitation protocol
An elbow brace protecting against varus and valgus stress was used in all cases for 8 weeks (Epimax; Ormed GmbH, Freiburg Germany). The brace allowed an unlimited training of extension and flexion. Unlimited training of pronation/supination was allowed after 4 weeks. Sports activites were possible after 3 months.
Statistics
All data are presented as means. Student's t-test (paired test) was used to compare the means. The level of significance was set at p < 0.05.
Results (Table)
During the follow-up time, no patient had a recurrent elbow dislocation. No complications were seen. The lateral pivot shift test became negative in all patients. The additional intraarticular pathologies which required additional arthroscopic therapy did not influence the result.
Morrey score increased from 40 (30–51) to 77 (62–90) points (p < 0.001). The outcome was moderate (50–80 points) in 10 cases. A good result was achieved in the other patients (80–95 points). At stress radiography, the distance between capitellum and radial head decreased from 13 (8–18) mm preoperatively to 2 (1–4) mm at follow-up(p < 0.001).
Discussion
Short-term outcome after open ligament reconstruction for chronic elbow instability is acceptable (Osborne and Cotterill Citation1966, Lee and Rosenwasser Citation1999, O'Driscoll Citation1999, McKee et al. Citation2003, Olsen and Sojbjerg Citation2003) but complications such as infection, scarring, joint stiffness, arthrofibrosis and atrophy are not uncommon (Marti et al. Citation2002). Arthroscopic elbow surgery is not problem-free, but severe complications are rare and it may therefore have a place in the treatment of lateral elbow instability (Kelly et al. Citation2001).
We found that a tight lateral ligamentous complex produced by thermal shrinkage was already detectable during the operation. The lateral instability had disappeared at the end of the operation in all patients, and stress radiographies became normal. These objective findings correlated with a good or moderate clinical outcome. The main benefit of this technique is the possibility of early rehabilitation, which may be the best prophylaxis against arthrofibrosis and muscular atrophy.
We did not observe any complications in our patients. This does not exclude the possibility that complications specific for elbow arthroscopy may occur (Kelly et al. Citation2001). Thermal shrinkage has its own complications. Ligament shrinkage results from thermal affection alteration of collagen. One side effect is the loss of cellular and intracellular structures in the ligaments, associated with loss of mechanical stress resistance. The biological reorganization of the ligaments begins some weeks after surgery (Hecht et al. Citation1999). In the postoperative phase (3 months after surgery), the ligaments may rupture—which one should be aware of in the postoperative treatment. Perry and Higgins (Citation2000) described a total rupture of the anterior cruciate ligament after thermal shrinkage. Our recommendations for rehabilitation are empirical. Caution should be exercised by patients who participate in contact or collision sports. Further studies may demonstrate whether thermal shrinkage is the most appropriate treatment for microinstability or if it is best used as an adjunct to other stabilization procedures. In addition, long-term follow-up will be required to demonstrate the benefit of thermal shrinkage over the established procedure of open operations.
Patients, arthroscopic findings and results of stress radiography
Author contributions
GS performed all operations and wrote the manuscript. SK and RW performed the patients' evaluations. HMK was involved in creating the discussion and performed the statistical analysis.
- Carter T. R., Balilie D., Edinger S. Radiofrequency electrothermal shrinkage of the anterior cruciate ligament. Am J Sports Med 2002; 30: 221–6
- Dodds S. D., Panjabi M. M., Daigneault J. P. Radiofrequency probe treatment for subfailure ligament injury: na biomechanical study of rabbit ACL. Clin Biomech 2004; 19: 175–83
- Eygendaal D., Heijboer M. P., Obermann W. R., Rozing P. M. Medial instability of the elbow. Acta Orthop Scand 2000; 71: 480–3, Findings on valgus load radiography and MRI in 16 athletes
- Hecht P., Hayasashi K., Lu Y., Fanton G. S., Thabit G., Vanderby R., Markel M. Monopolar radiofrequency energy effects on joint capsular tissue: Potential treatment for joint instability. Am J Sports Med 1999; 27: 761–71
- Hempfling H. Farbatlas der Arthroskopie groβer Gelenke. Fischer, Stuttgart, Jena, New York 1995
- Hildebrand K. A., Patterson S. D., King G. J. W. Acute elbow dislocations Simple and complex. Orthop Clin North Am 1999; 30: 63–79
- Jackson R. W. Energy from the electromagnetic spectrum. Am J Knee Surg 1999; 12: 181–5, The future in orthopaedic surgery
- Josefsson P. O., Gentz C. F., Johnell B., Wendeberg B. Surgical versus nonsurgical treatment of ligamentous injuries following dislocations of the elbow joint. Clin Orthop 1987; 214: 165–9
- Kelly E. W., Morrey B. F., O'Driscoll S. W. Complications of elbow arthroscopy. J Bone Joint Surg (Am) 2001; 83: 25–34
- Lansinger O., Karlsson J., Korner L., Mare K. Dislocation of the elbow joint. Arch Orthop Trauma Surg 1984; 102: 183–6
- Lee M. L., Rosenwasser M. P. Chronic elbow instability. Orthop Clin North Am 1999; 30: 81–9
- Lyons T. R., Griffith P. L., Savoie F. H., Field L. D. Laserassisted capsulorrhaphy for multidirectional instability of the shoulder. Arthroscopy 2001; 17: 25–30
- Marti R. K., Kerkhoffs G. M. M. J., Maas M., Blankevoort L. Progressive surgical release of posttraumatic stiff elbow. Acta Orthop Scand 2002; 73: 144–50, Technique and outcome after 2–18 years in 46 patients
- McKee M. D., Schemitz E. H., Sala M. J., O'Driscoll S. W. The pathoanatomy of lateral ligamentous disruption in complex elbow instability. J Shoulder Elbow Surg 2003; 12: 391–6
- Morrey B. F. The elbow and ist disorders. WB Saunders Company, Philadelphia London Toronto 1985; 73–91
- O'Driscoll S. W. Elbow instablity. Acta Orthop Belg 1999; 65: 404–15
- O'Driscoll S. W., Bell D. F., Morrey B. F. Posterolateral rotatory instability of the elbow. J Bone Joint Surg (Am) 1991; 73: 440–6
- Olsen B. S., Sojbjerg J. O. The treatment of reccurent posterolateral instability of the elbow. J Bone Joint Surg (Br) 2003; 85: 342–6
- Osborne G., Cotterill P. Recurrent dislocation of the elbow. J Bone Joint Surg (Br) 1966; 48: 340–6
- Outerbridge R. E. The etiology of chondromalacia patellae. J Bone Joint Surg (Am) 1961; 43: 752–7
- Perry J. J., Higgins L. D. Anterior and posterior cruciate ligament rupture after thermal treatment. Arthroscopy 2000; 16: 732–6
- Rieunau G., Gay R., Martinez C., Mansat C., Mansat M. Luxation récidivante du coude. Rev Chir Orthop 1972; 58: 257–64
- Schippinger G., Seibert F. J., Steinbock J., Kurcharczyk M. Management of simple elbow dislocations. Langenbecks Arch Surg 1999; 384: 294–7, Does the period of immobilization affect the eventual results?
- Spahn G., Schindler S. Tightening elongated ACL-grafts by application of bipolar electromagnetic energy (ligamentshrinkage). Knee Surg Sports Traumatol Arthrosc 2002; 10: 66–72
- Wienecke H., Lobenhoffer P. Grundlagen radiochirurgischer Systeme und ihre Anwendungen in der Arthroskopie (Basic principles of radiosurgical sytems and their applications in arthroscopy). Unfallchirurg 2003; 106: 2–12