Abstract
The standard treatment for late infections of knee prostheses is a two-stage reimplantation with a temporary articulating spacer between operations, but there is no universal agreement as to the best type of spacer to be used and surgeons have created modifications according to their technical and economic resources. We describe our modified technique for custom-made articulating spacers.
Spacers have evolved from simple monoblock designs made of acrylic cement alone to articulated, modular, complex and expensive designs with different grades of constriction. Many surgeons are reluctant to use these devices because of the costs and the potential risks of inserting metallic or plastic elements into a septic joint. Further refinements for customization of articulating spacers have been attempted (Rand Citation, Goldman et al. Citation). We have found no reports describing a technique for making custom hand-made articulating spacers.
A 68-year-old woman with rheumatoid arthritis for more than 20 years, and treated with immunosuppressive agents, had had a knee prosthesis for 16 years and walked with an orthosis because of instability. After the initial knee arthroplasty, she had an early infection with wound dehiscence that was successfully treated with surgical debridment and prolonged antibiotic therapy. She came to us with fever, tenderness, pain and swelling of the knee since 3 days previously, and a meticilin-sensitive S. aureus strain was grown in cultures from the knee exudate. We performed a two-stage revision arthroplasty with an articulating spacer built intraoperatively using cement loaded with antibiotic. A specific course of intravenous antibiotics was given, followed by oral therapy.
The patient was weight bearing on the articulating cement spacer for most of the time because of a contralateral femoral fracture with a delayed union. 11 weeks later, with no clinical signs or symptoms of infection of the knee, a constrained prosthesis was inserted. Cultures taken during the operation were negative. 3 months after surgery, knee motion was 0–135° and the patient had no pain. After 5 years, there has been no recurrence.
Surgical technique and postoperative protocol
During the first operation, the prosthesis components and cement are removed and an extensive debridement is performed (synovial membrane, devitalized bone and periarticular tissues). Biopsies are taken for culture and histology.
The distal femoral and proximal tibial components of the spacer are formed manually. The cement is modeled in its doughy phase to avoid excessive interdigitation in the remaining bone—in order to facilitate its removal at reimplantation of the prosthesis. Extra antibiotic is added to each pack of cement, based on the previous cultures and antibiogram results and without exceeding 10% of the total weight of the composite cement-antibiotic. The spacer component for the bone with a smaller defect is prepared first to limit displacement of the original joint line. In this way it is easier to restore the original joint line of the knee giving each spacer its proper thickness. No pre-manufactured spacer molds are used.
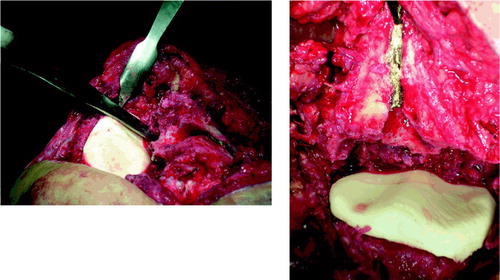
The tibial component is created over a flat mass of cement, to which a stem is added or crafted to minimize mobilization and secondary bone loss. With a curved osteotome, the spacer is contoured around the remaining tibia and excess cement is removed. 2 smooth grooves are crafted on the tibial cement spacer using finger pressure or a Hohmann retractor. This also creates a central crest, in an attempt to increase conformity with the femoral condyles and reduce instability between components. Marking the anterior femoral cortex with a line perpendicular to the transepicondylar axis can help to establish the proper rotation of the tibial component, so that both the grooves and rim will be congruent with the femoral component. A curved osteotome helps to craft the rim of the tibial component ().
Figure 1. Modeling of the tibial component. Note the grooves on the tibial side and the line marked over the femur to help in proper rotation of the component. A curved Hohmann retractor and also finger pressure can be used to create two smooth grooves on the tibial component.
The femoral component is constructed using 1 or 2 packs of antibiotic-loaded cement. A rudimentary “C-shape” mold is created on the edge of the surgeon’s hand and placed over the remaining femur, with the knee in a fiexed position. The posterior femoral condyles are modeled using a broad, curved osteotome (). Anterior and posterior areas can be smoothed using a sterile polyethylene (Goldstein et al. Citation2001) tibial trial component, but this requires the opening and re-sterilization of a prosthesis trial kit. We try to avoid this and use a curved osteotome instead. Excess cement on the posterior and lateral sides of the distal femur is removed or cut out with the osteotome or a surgical knife. In cases of segmentary defects, we prefer to add the cement directly over the bone and mold it with the osteotome.
Figure 2. Troclear groove is contoured with a curved Hohmann retractor, posterior condyles and anterior femoral shield extended with a curved osteotome. Final remodeling is done with a tip burr.
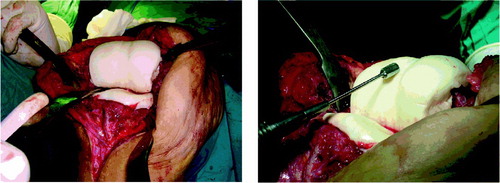
The femoral shield is extended proximally to shape a patellofemoral surface and a shallow femoral trochlear groove is created with finger pressure—or a curved Hohmann retractor—to obtain adequate patellofemoral gliding and congruence with the tibial central crest. It is also important to release and expose the posterior condyles and to extend the femoral spacer through the posterior condyles in order to re-create a C-shape that prevents displacement. A final remodeling of the grooves (carving of prominent zones or badly shaped spikes) can be done with a set of tip burr instruments ( and ). Leaving the knee slightly lax is preferable to excessive tension.
Figure 3. An articulating spacer reconstructs a femoral segmentary defect (b) after removal of an infected total knee (a).

A continuous passive program is started within 24 h postoperatively, progressing slowly in flexion and never surpassing 90° (Duncan et al. Citation1992, McPherson et al. Citation1995). Range of motion is limited to avoid subluxation and locking of the articulating cement spacer. Isometric exercises with and without bracing are encouraged, and assisted active flexion and extension exercises are allowed. Total weight bearing with the aid of crutches or a cane starts on the fourth or fifth postoperative day. An extension orthosis of the knee is worn during ambulation.
Discussion
While the advantages of articulating spacers in the treatment of infected total-knee artroplasty have been widely described, there is no universal agreement about the best type of spacer to be used (Booth and Lotke Citation1989, McPherson et al. Citation1995, Carlton et al. Citation1997, Fehring et al. Citation2000, Haddad et al. Citation2000, Siebel et al. 2000, Bloom et al. Citation2004, Haleem et al. Citation2004). Hand-made spacers are still the most commonly used alternative. These retain most of the advantages of articulating spacers, but the low cost and the possibility of adding high doses of antibiotic can be considered to be particular advantages of hand-made spacers (Alt et al. Citation2004). They can be made in any surgical theater without specific tools. The main disadvantage of this system resides in its potential instability, where the patient is obliged to walk with an extension or a hinged orthosis.
Author contributions
All the authors started to work in this project several years ago in the first institution. We started developing some protocols, performing first cases in cadavers and are now preparing a review of our first 30 patients with this method. All authors contributed to the writing and revision of this report.
- Alt V., Bechert T., Steinrücke P., Wagener M., Seidel P., Dingeldein E., Domann E., Schettler R. In vitro testing of antimicrobial activity of bone cement. Antimicror. Agents Chemother 2004; 48(11)4084–8
- Bloom A. V., Brown J., Taylor A. H., Pattison G., Whitehouse S., Bannister G. C. Infected total knee arthroplasty. J Bone Joint Surg (Br) 2004; 86: 688–91
- Booth R. E., Jr., Lotke P. A. The results of spacer block technique in revision of infected total knee arthroplasty. Clin Orthop 1989, 248: 57–60
- Calton T. F., Fehring T. K., Griffin W. L. Bone loss associated with the use of spacer blocks in infected TKA. Clin Orthop 1997, 345: 148–54
- Duncan C. P., Beauchamp C. P., Masri B. The antibiotic loaded joint replacement system: A novel approach to the management of the infected knee replacement. J Bone Joint Surg (Br) 1992; 74: 296, (suppl III)
- Fehring T. K., Odum S., Calton T. F., Mason J. B. Articulating versus static spacers in Revision Total Knee Arthroplasty for sepsis. Clin Orthop 2000, 380: 9–16
- Goldman R. T., Scuderi G. R., Insall J. N. Two-stage reimplantation for infected TKA. Clin Orthop 1996, 331: 118–24
- Goldstein W., Kopplin M., Wall R., Berland K. Temporary articulating methylmethacrylate antibiotic spacer. A new method of intraoperative manufacturing of a custom articulating spacer. J Bone Joint Surg (Am) 2001; 83(2)92–7
- Haddad F. S., Masri B. A., Campbell D., McGraw R. W., Beauchamp C. P., Duncan C. The PROSTALAC functional spacer in two-stage revision for infected knee replacements. J Bone Joint Surg (Br) 2000; 82: 807–12
- Haleem A., Berry D. J., Hansen A. Mid-term to long-term follow up of two stage reimplantation for infected total knee arthroplasty. Clin Orthop 2004, 428: 35–9
- McPherson E. J., Lewonowsky K., Dorr L. D. Use of an articulated PMMA spacer in the infected TKA. J Arthroplasty 1995; 10: 87–9
- Rand J. A. Alternatives to reimplantation for salvage of the total knee arthroplasty complicated by infection. J Bone Joint Surg (Am) 1993; 75: 282–9
- Siebel T., Kelm J., Porsch M., Regitz T., Neumann W. H. Two-stage exchange of infected knee arthroplasty with an prosthesis like interim cement spacer. Acta Orthop Belg 2002; 68(2)150–6