Abstract
Background The aims of this study were to quantify the risk and identify the causes of early postoperative mortality after total hip arthroplasty. This would help clinicians address preventable causes of death and help in accurate counseling and consenting of patients.
Methods We determined the death rate at 90 days in an unselected consecutive series of 1,727 primary total hip arthroplasties where patients had not routinely received chemothromboprophylaxis.
Results The mortality at 90 days was 17/1,727 (1%). The 90-day mortality was 0.2% in patients under 70 years of age, 1.3% in patients between 70 and 80, and 2.5% in those over 80. 7 patients died from ischemic heart disease, 4 died following cerebrovascular events, and 2 from pulmonary embolism. 4 patients died from non-vascular causes. Of the vascular deaths, ischemic heart disease outnumbered cerebrovascular events which, in turn, outnumbered pulmonary embolism (7 vs. 4 vs. 2).
Interpretation Strategies aimed at reducing deaths should address all vascular causes, not just pulmonary embolism. Our findings can be used to inform patients as to the risk of early death after total hip arthroplasty.
Primary total hip arthroplasty (THA) carries a risk of early postoperative death. In early series, the death rate was 3–6% from pulmonary embolus alone (Coventry et al. Citation1974), a figure that is not acceptable for an operation designed to improve quality of life. Although previous studies have quantified the risk of death, to our knowledge, only one other study has stratified the risk of death in relation to age (Lie et al. Citation2002).
The aims of this study were to determine the timing and cause of death following primary THA in current practice, to identify preventable deaths, to stratify the risk of death in relation to age, and to improve the quality of informed consent given to patients about to undergo THA.
Patients and methods
Over a 3-year period (1993–1996), 1,727 consecutive patients underwent primary THA at the Avon Orthopaedic Centre. The outcome was audited and patients who died within 90 days had their medical case notes, death certificates and post mortem reports examined. Retrieval at 90 days, with regards to death, was 100%.
Results
7 patients (0.41%) died within 30 days of their procedure and a further 10 (0.58%) died between day 30 and day 90, giving a total mortality rate at 90 days of 0.98% (17/1,727). 7 patients (0.41%) died from ischemic heart disease (IHD), 4 (0.23%) died following cerebrovascular events (CVE) and 2 (0.12%) died from pulmonary embolism (PE). 4 patients (0.23%) died from non-vascular causes ().
Table 1. Timing and causes of death in 17/1,727 patients within 90 days of primary THA
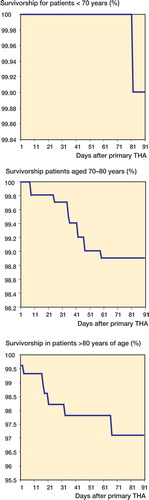
The 90-day mortality was 2/822 (0.2%) in patients under 70 years of age, 8/626 (1.3%) in patients between 70 and 80, and 7/279 (2.5%) in those over 80 ().
Table 2. Death rates at 30 and 90 days after primary THA according to age at procedure
Discussion
In this study the death rate at 30 days was 0.41%. This compares with 0.91% in the Trent Arthroplasty Survey (Fender et al. Citation1997), 0.35% in the National Confidential Enquiry into Perioperative Deaths (NCEPOD) report (Campling Citation1993), an estimated 60-day mortality of 0.8% seen in the Norwegian Hip Registry (Lie et al. Citation2000), 0.69% in the UK National Total Hip Replacement Outcome survey (Williams et al. Citation2002), and 0.48% in the Pulmonary Embolism Prevention (PEP) trial (Citation2000). The PEP trial, however, includes both hip and knee replacements and is not strictly comparable.
Our fatality rate from PE was 0.12%. This was without routine chemothromboprophylaxis. Mechanical thromboprophylaxis was employed. All patients wore thromboembolic deterrent (TED) stockings and a small proportion had AV impulse foot pumps. A trochanteric detachment approach to the hip was not used and a standard combined general and spinal anesthetic technique was employed. Without exception, this allowed mobilization of the patient within 48 h.
The fatality rate from PE of 0.12% is average in contemporary studies. The highest rate reported (0.19%) was from the Trent Arthroplasty survey (Fender et al. Citation1997) and the lowest (0.04%) was from the Oxford Record Linkage study (Seagroatt et al. Citation1991). The latter only recorded readmissions and may thus have missed deaths in the community.
Informed consent can be obtained from patients before THA and the risk of death quantified, by using the age-stratified data given in and the .
Vascular deaths (from CVE, IHD and PE) outnumbered non-vascular causes (13 vs. 4). Of the vascular deaths, ischemic heart disease outnumbered cerebrovascular events which, in turn, outnumbered pulmonary embolism (7 vs. 4 vs. 2). Strategies aimed at reducing deaths should thus address all vascular causes, and not just PE.
In a meta-analysis (1994), the antiplatelet trialists collaboration showed that using aspirin prophylaxis versus placebo caused a reduction in vascular deaths by one-sixth following non-cardiac surgery. The results of the PEP trial (Citation2000) were comparable with this reduction, but unfortunately lacked the power to show this conclusively. In a different setting, using beta-blockers, deaths following noncardiac surgery were reduced from 14% to 3% in high-risk patients (Mangano et al. Citation1996).
A power calculation based on the data from our study, with mortality from PE of 0.12%, shows that a randomized controlled trial of chemoprophylaxis versus no chemoprophylaxis, using death as an outcome measure, would require approximately 24,000 patients in each group to show a 10% reduction in mortality (Maxwell Citation1990). Death following total hip arthroplasty is rare, and pulmonary embolus accounted for only 12% of deaths in this study. Further effort should be directed towards reducing the rate of death from preventable vascular causes.
The risk of death after total hip arthroplasty increases dramatically with age. Patients and their families should be counselled accordingly.
No competing interests declared.
Contributions of authors
AB, GP data collection and manuscript preparation. AT data collection. SW statistics and data processing. GB senior author.
- Campling E A. The report of the National Confidential Enquiry into Perioperative Deaths. Royal Colleges of Physicians of the United Kingdom. 1993, Faculty of Public Health Medicine
- Coventry M B, Beckenbaugh R D, Nolan D R, Ilstrup D M. 2,012 total hip arthroplasties. A study of postoperative course and early complications. J Bone Joint Surg (Am) 1974; 56(2)273–84
- Fender D, Harper W M, Thompson J R, Gregg P J. Mortality and fatal pulmonary embolism after primary total hip replacement. Results from a regional hip register. J Bone Joint Surg (Br) 1997; 79(6)896–9
- Lie S A, Havelin L I, Engesaeter L B, Gjessing H K, Vollset S. Mortality after total hip replacement, 0–10 years follow up of 39,505 patients in the Norwegian Arthroplasty Register. Acta Orthop Scand 2000; 71(1)19–27
- Lie S A, Havelin L I, Engesaeter L B, Furnes O, Vollset S. Early postoperative mortality after 67,548 total hip replacements. Causes of death and thrombosis prophylaxis in 68 Norwegian hospitals from 1987 to 1999. Acta Orthop Scand 2002; 73(4)392–9
- Mangano D T, Layug E L, Wallace A, Tateo I. Effect of atenolol on mortality and cardiovascular morbidity after noncardiac surgery. Multicenter Study of Perioperative Ischemia Research Group. N Engl J Med 1996; 335(23)1713–20
- Maxwell S E. Designing experiments and analyzing data: a model comparison perspective. Wadsworth Pub. Co, Belmont, Calif 1990
- Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention (PEP) trial. Lancet 2000; 355: 1295–302
- Seagroatt V, Tan H S, Goldacre M, Bulstrode C, Nugent I, Gill L. Elective total hip replacement: incidence, emergency readmission rate, and postoperative mortality. BMJ (Clinical research ed.) 1991; 303: 1431–5
- Williams O, Fitzpatrick R, Hajat S, Reeves B C, Stimpson A, Morris R W, [all names]. Mortality, morbidity, and 1-year outcomes of primary elective total hip arthroplasty. J Arthroplasty 2002; 17(2)165–71