Abstract
Introduction The cementation of a total hip prosthesis may cause bone necrosis, either by direct toxicity or by generation of heat during the polymerization process. This necrotic bone may create conditions that encourage the growth of bacteria. We compared the revision rates due to infection in primary uncemented total hip arthroplasties (THAs) with those of cemented THAs with antibiotic-loaded cement and to those of cemented THAs without antibiotic cement.
Methods Data from the Norwegian Arthroplasty Register for the period 1987–2003 were used. To have comparable groups, we analyzed only primary THAs performed because of primary osteoarthrosis, and where both the acetabular and the femoral component of the prosthesis were either uncemented or cemented (n = 56,275).
Results In total, 252 revisions due to infection were reported. Compared to the uncemented THAs (n = 5,259), the risk of revision due to infection for THAs without antibiotic cement (n = 15,802) was increased 1.8 times (CI 1.0–3.1; p = 0.04). No differences could be detected when compared to THAs with antibiotic-loaded cement (n = 35,214) (RR 1.2, CI 0.7–2.0; p = 0.5). The average operating time for uncemented THAs was 15 min less than for cemented THAs.
Interpretation The risk of revision due to infection was the same for uncemented and for cemented arthroplasties with antibiotic-loaded cement, but higher for cemented arthroplasties without antibiotic cement. Our findings can be explained by reduced resistance to infection caused by the cement, which appears to be neutralized by adding antibiotic to the cement.
Peroperative wound contamination during implantation of primary total hip arthroplasties (THAs) occurs in more than 30% of all operations in standard and in ultra-clean operating theaters (Davis et al. Citation1999, Clarke et al. Citation2004a, Citationb, Maathuis et al. Citation2005). Many THAs are considered to fail due to the presence of clinically unrecognized low-grade infection. In accordance with this, we have previously shown that in primary THAs antibiotic prophylaxis given systemically and in bone cement not only reduces the risk of revision due to infection, but also reduces the risk of aseptic loosening (Espehaug et al. Citation1997, Engesæter et al. Citation2003).
Cement per se may create conditions for growth of the omnipresent bacteria, for example by causing bone necrosis, by toxicity or by generation of heat during polymerization (Mjöberg Citation1997, Jonbergen et al. Citation2004). However, some authors doubt that the curing process of the cement causes thermal injury (Toksvig-Larsen et al. Citation1991). If, however, the cementation in some way results in tissue necrosis, such damage should be less in uncemented prostheses, and these implants should accordingly be less disposed to infection. We have explored this hypothesis by using data on primary THAs in the Norwegian Arthroplasty Register. The revision rates due to infection for uncemented hip arthroplasty were compared with those for cemented arthroplasty with antibiotic-loaded cement, and for cemented arthroplasty without antibiotic cement.
Patients and methods
The Norwegian Arthroplasty Register was established in September 1987. Each THA performed in Norway is reported individually by the surgeon by filling out a standard form (Havelin et al. Citation2000). The information given in the form includes the identity of the patient, the date of operation, indication for surgery, type of prosthesis, type of cement, duration of the operation, type of operating room (“greenhouse”, laminar air ventilation, ordinary ventilation), and type of systemic antibiotic prophylaxis. From the start of the Register in September 1987 to the end of December 2003, 85,120 primary THAs were reported. Included in the present study were primary THAs performed because of idiopathic osteoarthritis of the hip, and prostheses where both the acetabular and the femoral component were either uncemented or cemented. Furthermore, only operations in which systemic antibiotic—penicillin (cloxacillin or dicloxacillin) or cephalosporin (cephalotin or cefuroxime)—had been given were selected. We compared 3 groups of THAs: uncemented hip arthroplasty, cemented arthroplasty with antibiotic-loaded cement, and cemented arthroplasty without antibiotic cement. Failure (revision) of the implant was defined as surgical removal or exchange of the whole or part of the implant. Using the unique ID number assigned to every inhabitant of Norway, the information on each primary THA was linked to an eventual revision. Separate analyses were performed on homogenous subgroups of implants consisting of (1) the most common cemented prosthesis in Norway, the Charnley (Thackray, Leeds, UK) with the high-viscosity cement Palacos with or without gentamicin (0.5 g gentamicin per 40 g of bone cement) (Shering-Plough, Kenilworth, NJ) and (2) the most common uncemented prosthesis, the Corail stem (hydroxyapatite-coated) in combination with Atoll or Tropic cups (also hydroxyapatite-coated) (DepPuy, Leeds, UK).
Statistics
Survival analyses were performed with the Kaplan-Meier method and Cox regression. Patients who died or emigrated during follow-up were identified from files provided by Statistics Norway, and the follow-up time for prostheses in these patients were censored at the date of death or emigration. We used a Cox multiple regression model to study relative revision risks (failure-rate ratios) among the 3 groups of THAs with adjustments for the possible influences of sex, age (<51, 51–60, 61–70, 71–80, or <80 years), type of systemic antibiotic prophylaxis—penicillin (cloxacillin or dicloxacillin) or cephalosporin (cephalotin or cefuroxime)— and duration of systemic prophylaxis, type of operating room, and the duration of the operation as a continuous variable. Estimates from Cox analyses with the 3 THA groups as strata factor were used to construct adjusted survival curves. For revisions, the surgeon had recorded one or more reasons for failure, but when in combination with infection, infection was considered to be the primary cause of revision. Otherwise, aseptic loosening was counted as the principal cause of revision when given in combination with other causes.
We used the statistical package SPSS version 13.0 (SPSS Inc. Citation2004).
Results
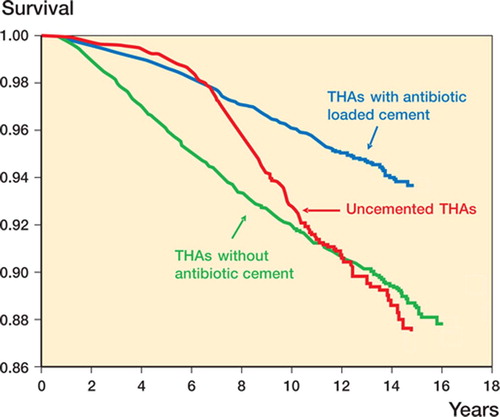
56,275 primary THAs performed because of primary coxarthrosis and with both components cemented or uncemented, fulfilled the inclusion criteria. The patients with uncemented prostheses were younger and the duration of the operation was shorter for uncemented THA than for the other 2 groups (). There was an increasing use of cement with antibiotic after 1993 and a corresponding reduction in the use of cement without antibiotic, while the use of uncemented THAs was almost unchanged ().
Figure 1. Number of THAs performed annually from 1987 to 2003 for uncemented arthroplasties, for cemented hip arthroplasties with antibiotic-loaded cement, and for cemented hip arthroplasties without antibiotic cement.
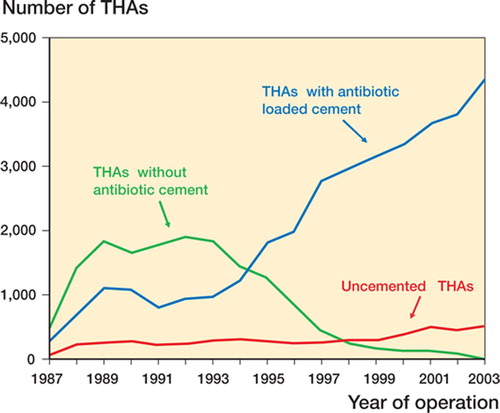
Table 1. Data on uncemented THAs, on THAs with antibiotic-loaded cement, and on THAs without antibiotic cement
Infection as endpoint in the analyses
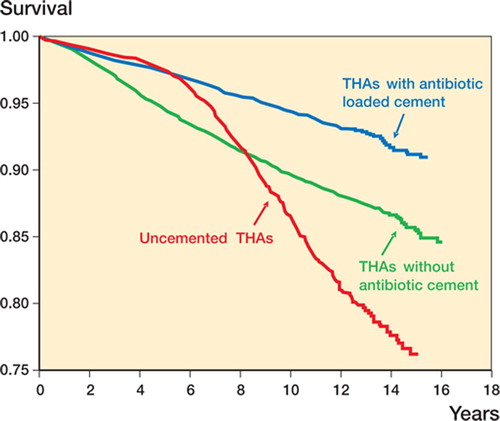
Compared to uncemented THAs, the cemented prostheses without antibiotic cement had 1.8-times increased risk of revision due to infection (CI 1.0–3.1; p = 0.04), but we found no difference for the cemented arthroplasties with antibiotic-loaded cement (RR = 1.2, CI 0.7–2.0; p = 0.5) (, ). For cemented arthroplasties without antibiotic cement, the risk of revision due to infection was increased 1.5 times compared to cemented arthroplasties with antibiotic-loaded cement (CI 1.1–2.0; p = 0.004).
Figure 2. Cox-adjusted survival curves with infection as endpoint for uncemented arthroplasties, for cemented hip arthroplasties with antibiotic-loaded cement, and for cemented hip arthroplasties without antibiotic cement.
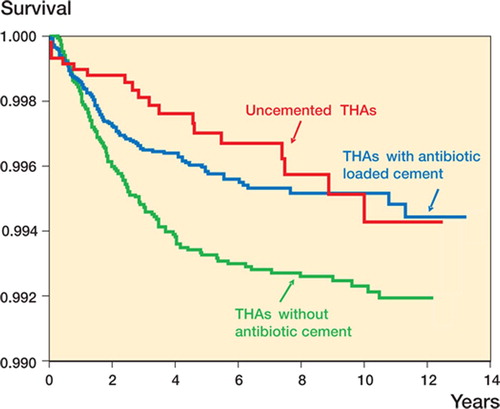
Table 2. Results of primary uncemented THAs, THAs with antibiotic-loaded cement, and of THAs without antibiotic cement in patients with primary coxarthrosis. Number of THAs, number of THA revisions, Kaplan-Meier 12-year revision percentages, Cox relative revision risk (RR) (with uncemented THAs as reference value), 95% confidence interval for RR, and P-value estimated with infection, with aseptic loosening, and with all reasons for revision as endpoint in the analyses
Of the 252 revisions performed because of infection, 224 (89%) were carried out during the first 5 years postoperatively (92% for cemented arthroplasties with antibiotic-loaded cement, 89% for cemented arthroplasties without antibiotic cement, and 67% for uncemented arthroplasties). In the analyses for infections occurring during the first 5 years postoperatively, the infections occurring later were censored. The revision risks for infections among the 3 groups were then similar to that for the whole material, but some more marked. With uncemented arthroplasties as reference, we found a 2.5-times increased risk of revision for cemented arthroplasties without antibiotic cement (CI 1.3–4.7; p = 0.005) and no increase compared to cemented arthroplasties with antibiotic-loaded cement (RR = 1.5, CI 0.8–2.9; p = 0.2).
Infections in arthroplasties with operative time 51–110 min (n = 40,823)
To avoid the influence of operations of extremely short or long duration, we performed separate analyses for THAs with the most common operation time, i.e. between 51 and 110 min (representing 73% of all THAs). Compared to uncemented THAs, the risk of revision due to infection for THAs without antibiotic cement was 1.4 (CI 0.7–2.5; p = 0.3) and for THAs with antibiotic-loaded cement it was 0.8 (CI 0.5–1.5; p = 0.5). For the operations with a duration of 51–110 min, the risk of revision due to infection increased with the length of the procedure (p = 0.001).
Compared to the category 71–90 min (n = 19,295), the group with operating time of 51–70 min (n = 8,541) had a reduced risk of revision due to infection (RR = 0.5; p = 0.04), but when compared to the 91–110 min group (n = 12,987) there was no significant difference in the risk of revision (RR = 1.4; p = 0.3).
Infections in arthroplasties performed before and after 1995
Due to the skew in time of observations for the 3 groups of arthroplasties, with relatively more THAs without antibiotic cement early in the period and relatively more THAs with antibiotic loaded-cement at the end of the studied period, we performed separate analyses for operations before 1995 (n = 21,498) and after January 1, 1995 (n = 34,777) (). Again, the results were similar to those of the whole material, but more pronounced in the first period and less pronounced in the last period. In the first period (before 1995), compared to uncemented arthroplasties (n = 1,957), 2.3 times increased risk of revision due to infection was found for cemented arthroplasties without antibiotic cement (n = 12,421) (CI 1.0–5.2; p = 0.05). For cemented arthroplasties with antibiotic-loaded cement (n = 7,120), no increased risk was found (RR = 1.0, CI 0.4–2.4; p = 1.0). In the last period, we found no statistically significant differences between the 3 groups. Compared to uncemented THAs (n = 3,302), the risk ratio for cemented THAs without antibiotic cement (n = 3,381) was 1.4 (p = 0.4), and for THAs with antibiotic-loaded cement (n = 28,094) risk ratio was 1.1 (p = 0.8).
Aseptic loosening as endpoint in the analyses
With aseptic loosening as endpoint and with uncemented arthroplasties as reference, the risk of revision was higher (RR = 1.3) for cemented arthroplasties without antibiotic cement (p < 0.001), but lower (RR = 0.6) for cemented hip arthroplasties with antibiotic-loaded cement (p < 0.001) (, ).
All reasons for revision as endpoint in the analyses
With all reasons for revision as endpoint, and again with uncemented THAs as reference, the revision rate for cemented arthroplasties without antibiotic was reduced to 0.9 times (p = 0.01), and for arthroplasties with antibiotic-loaded cement it was reduced to 0.5 times (p < 0.001) (, ).
Adjustments for systemic antibiotic prophylaxis
Only operations performed with systemic antibiotic prophylaxis—either cephalosporin (the first-generation cephalotin or the second-generation cefuroxime) or penicillinase-resistant penicillin (cloxacillin or dicloxacillin)—were included, irrespective of the duration of the systemic prophylaxis. If operations with systemic antibiotic prophylaxis given only on the day of surgery were selected, the results were similar. If only THAs with no systemic antibiotic prophylaxis were selected (n = 1,225), the numbers in the different groups were too small for further analysis.
Analyses in a subgroup of Charnley prostheses with Palacos cement and uncemented Corail stems with either Atoll or Tropic cup (n = 19,007)
To have an even more homogenous subgroup of hip arthroplasties, we selected Charnley prostheses with high-viscosity cement (Palacos) with gentamicin (n = 14,973) or without gentamicin (n = 2,336) and the uncemented hydroxyapatite-coated Corail femur stems with either Atoll or Tropic cups (n = 1,698). The results were the same as for the whole material, except that no increased rate of aseptic loosening was found for the uncemented prostheses compared to cemented arthroplasties with antibiotic cement ().
Table 3. Results of primary uncemented Corail stem with Atoll or Tropic cup, and of primary Charnley THAs with and without gentamicin in Palacos cement, in patients with primary coxarthrosis. Number of THAs, number of THA revisions, Kaplan-Meier 12-year revision percentages, Cox relative revision risk (RR) (with uncemented THAs as reference value), 95% confidence interval for RR, and p-value estimated with infection, with aseptic loosening, and with all reasons for revision as endpoint in the analyses
Discussion
We found that uncemented hip arthroplasties had the same the risk of revision due to infection as cemented arthroplasties with antibiotic-loaded cement, but reduced risk compared to cemented arthroplasties without antibiotic cement. One possible explanation could be that the cementation per se in some way creates conditions that are conducive to the growth of bacteria following the apparently unavoidable contamination peroperatively (Davis et al. Citation1999, Clarke et al. Citation2004a, Maathuis et al. Citation2005). Necrotic bone tissue around the cement, caused by cement toxicity or heat generation during curing of the cement, could be the potential growth medium. Antibiotic in the cement could partly protect against growth of bacteria in this area of low resistance to infection. The insertion of an uncemented hip arthroplasty might cause less tissue necrosis and the antibiotic may therefore not be needed to the same extent.
89% of the revisions due to infection were performed during the first 5 years postoperatively. If necrotic tissue plays any role in the risk of infection with THAs, it could be expected that the increased risk of infection should decrease with time i.e. after the necrotic tissue close to the cement has been resorbed and substituted by normal vascular tissue with normal resistance to infection. In accordance with this, the differences among the three groups studied were most evident during the first few years postoperatively ().
Differences in duration of the operation should be considered in explaining the differences among the groups. The operating time for the uncemented prostheses was on average 15 min shorter than that for the cemented THAs, and accordingly these operations were probably less exposed to perioperative contamination. This difference in operating time in the 3 groups was adjusted for in the Cox model in all the results presented. Accordingly, the reduced operating time is not the only explanation for the low risk of infection in the uncemented THAs. Moreover, we studied the subgroup of THAs with the most common operating time (duration 51–110 min) separately, covering 73% of all operations. In this subgroup stratified for operating time, the differences among the three groups of THAs were also the same as for the whole material. On the other hand, for the operations lasting 51–110 min, an increased risk of revision due to infection with increasing duration of the operation was found for both cemented and uncemented THAs. This seems plausible, since increased contamination might be expected from longer duration of the surgery. Similar results have been reported previously from the Norwegian Arthroplasty Register (Småbrekke et al. Citation2004).
In the present and previous studies, we have demonstrated reduced revision due to aseptic loosening with antibiotic in the cement (Espehaug et al. Citation1997, Engesæter et al. Citation2003). Low-grade infections can be expected to be one of many different reasons for aseptic loosening (Maathuis et al. Citation2005). Aseptic loosening is a diagnosis of exclusion, depending on the number of methods available and on the intensity of the search for infection (Neut et al. Citation2003). The surgeon probably, but wrongly, reports some low-grade infections to the registry as aseptic loosening. This seems to be the most plausible explanation for the reduced aseptic loosening in cemented THAs performed with systemic antibiotic prophylaxis and antibiotic-loaded bone cement in the present study and in earlier papers from the registry (Espehaug et al. Citation1997, Engesæter et al. Citation2003).
In the current study, we included some cements (e.g. Boneloc, CMW1, and CMW3) and some brands of cemented and uncemented prostheses with documented inferior results (Havelin et al. Citation1995, Citation2002, Espehaug et al. Citation2002, Furnes et al. Citation2005). To circumvent the influence of these inferior implants, we carried out a separate analysis of a subgroup of THAs consisting of the Charnley prostheses with high-viscosity cement (Palacos), and of the uncemented hydroxyapatite-coated Corail femur stems with either Atoll or Tropic uncemented cups. The results for these more homogenous subsets of THAs were the same as for the whole material, which strengthens our overall findings.
The percentage of revisions due to infection in our series was 0.45% (252 of 56,275 primary THAs), the same as the reported 0.45% revision percentage for infection in a multi-surgeon audit of infection after total hip replacement in the UK (7 of 1,567 primary THAs) (Blom et al. Citation2003). These authors found, however, a total of 1% postoperative infection and, accordingly, only half of the infections were revised. In the Norwegian Arthroplasty Register only infections treated with revision are reported, as infected THAs treated with antibiotics only (or antibiotics combined with debridement and washout) are not reported. If non-revision treatments for infection were used differently in the 3 groups we studied, this could have influenced our results. We have, however, no reason to believe that is the case.
The presented risks of revision due to infection in the uncemented prostheses in the Norwegian Arthroplasty Register are acceptable. The overall revision rate and the rate of revision because of aseptic loosening for uncemented prostheses were, however, too high and have been mainly due to failure of the uncemented cups (Havelin et al. Citation1995, Citation2000, Citation2002, Furnes et al. Citation2005). Also, our overall revision rates for cemented arthroplasties without antibiotic cement are rather high, but this partly reflects the results of the inferior cements in use in the early 1990s (Havelin et al. Citation2000).
We acknowledged the skew in time of observation of the patients in the 3 different groups of arthroplasties () and we therefore performed separate analyses for the first and last part of the period studied. For the first period, our findings were the same as for the whole material, but more evident. In the last period, similar differences were found, but they were not statistically significant.
No competing interests declared.
Contributions of authors
This paper is a close teamwork by the orthopedic surgeons (LBE, OF and LIH) and the statisticians (BE and SAL). All have participated in the design of the study, interpretation of the results, and in elaboration of the manuscript. LBE is, however, main responsible for designing the study, for performing the statistical analyses, and for writing of the manuscript.
- Blom A W, Taylor A H, Pattison G, Whitehouse S, Bannister G C. Infection after total hip arthroplasty. The Avon experience. J Bone Joint Surg (Br) 2003; 85: 956–9
- Clarke M T, Lee P T H, Roberts C P, Gray J, Keene G S, Rusthon N. Contamination of primary total hip replacements in standard and ultra-clean operating theaters detected by the polymerase chain reaction. Acta Orthop Scand 2004a; 75: 544–8
- Clarke M T, Roberts C P, Lee P T H, Gray J, Keene GS, Rusthon N. Polymerase chain reaction can detect bacterial DNA in aseptically loose total hip arthroplasties. Clin Orthop 2004b, 427: 132–7
- Davis N, Curry A, Gambhir A K, Panigrahi H, Walker C R C, Wilkins E G L, Worsley M A, Kay P R. Intraoperative bacterial contamination in operations for joint replacement. J Bone Joint Surg (Br) 1999; 81: 886–9
- Engesæter L B, Lie S A, Espehaug B, Furnes O, Vollset S E, Havelin L I. Antibiotic prophylaxis in total hip arthroplasty. Effects of antibiotic prophylaxis systemically and in bone cement on the revision rate of 22,170 primary hip replacements followed 0–14 years in the Norwegian Arthroplasty Register. Acta Orthop Scand 2003; 74: 644–51
- Espehaug B, Engesæter L B, Vollset S E, Havelin L I, Langeland N. Antibiotic prophylaxis in total hip arthroplasty. Review of 10,905 primary cemented total hip replacements reported to the Norwegian Arthroplasty Register, 1987–1995. J Bone Joint Surg (Br) 1997; 79: 590–5
- Espehaug B, Furnes O, Havelin L I, Engesæter L B, Vollset S E. The type of cement and failure of total hip replacements. J Bone Joint Surg (Br) 2002; 84: 832–8
- Furnes O, Espehaug B, Lie S A, Engesæter L B, Vollset S E, Hallan G, Fenstad A M, Havelin L I. Prospective studies of hip and knee prostheses. The Norwegian Arthroplasty Register 1987–2004. Scientific exhibition presented at the 72nd Annual Meeting of the American Academy of Orthopaedic Surgeons, Washington DCUSA, February, 23–272005
- Havelin L I, Espehaug B, Vollset S E, Engesæter L B. Early aseptic loosening of uncemented femoral components in primary total hip replacement. A review based on the Norwegian Arthroplasty Register. J Bone Joint Surg (Br) 1995; 77: 11–7
- Havelin L I, Espehaug B, Lie S A, Engesæter L B, Furnes O, Vollset S E. The Norwegian Arthroplasty Register. 11 years and 73,000 arthroplasties. Acta Orthop Scand 2000; 71: 337–53
- Havelin L I, Espehaug B, Engesæter L B. The performance of two hydroxyapatite- coated acetabular cups compared with Charnley cups. From the Norwegian Arthroplasty Register. J Bone Joint Surg (Br) 2002; 84: 839–45
- Jonbergen J P W van, Anderson P G, Faber F W M. Total hip arthroplasty with Boneloc cement: Unsatisfactory results in 163 hips after 9 to 11 years. Hip International 2004; 14: 229–32
- Maathuis P G M, Neut D, Busscher H J, van der Mei H C, van Horn J R. Perioperative contamination in primary total hip arthroplasty. Clin Orthop 2005, 433: 136–9
- Mjöberg B. The theory of early loosening of hip prostheses. Orthopedics 1997; 20: 1169–75
- Neut D, van Horn J R, van Kooten T G, van der Mei H C, Busscher H J. Detection of biomaterial-associated infections in orthopaedic joint implants. Clin Orthop 2003, 413: 261–8
- Småbrekke A, Espehaug B, Havelin L I, Furnes O. Operating time and survival of primary total hip replacements. An analysis of 31 745 primary cemented and uncemented total hip replacements from local hospitals reported to the Norwegian Arthroplasty Register 1987–2001. Acta Orthop Scand 2004; 75: 524–32
- SPSS Inc. SPSS Advanced Models 13.0. SPSS Inc, Chicago 2004
- Toksvig-Larsen S, Franzen H, Ryd L. Cement interface temperature in hip arthroplasty. Acta Orthop Scand 1991; 62: 102–5