Abstract
Background Studies have shown that the degree of initial displacement and also comminution of the femoral calcar, size of the head and varus angulation are prognostic of failure in displaced femoral neck fracture. We have applied these radiographic criteria in order to select patients who would benefit from internal fixation as opposed to primary hemiarthroplasty, and this prospective study was conducted in order to monitor the results of this strategy.
Methods 683 displaced fractures of the femoral neck were treated with internal fixation or primary hemiarthroplasty based on the proposed radiographic criteria in a prospective consecutive study, and the patients were followed for 1–6 years. We treated 228 fractures with internal fixation and 455 by bipolar hemiprosthesis. The choice of operation was based on clinical evaluation of the patient and assessment of the assumed healing potential of the fracture, as determined by radiographic evaluation. Revision and mortality were primary endpoints.
Results 54 (24%) of the patients originally treated by osteosynthesis were revised, whereas 9 (2%) of the patients treated with hemiarthroplasty had revision surgery. There were no significant differences in mortality between the groups at 30, 120 or 365 days.
Interpretation Even when treating only the fractures with the assumed best healing potential with internal fixation, the results are inferior to hemiarthroplasty.
The best treatment for displaced fracture of the femoral neck is still to be determined (Masson et al. Citation2004). Several studies have shown a 30–40% rate of reoperation after internal fixation and superior function after primary hemi-or total arthroplasty (Johansson et al. Citation2000, Rogmark et al. Citation2002 a, Citationb, Roden et al. Citation2003). Cost has been shown to be greater after internal fixation due to the high rate of reoperation, as have morbidity and mortality due to complications (Palmer et al. Citation2000, Rog-mark et al. Citation2003). Nevertheless, arthroplasty might be an unnecessary procedure for the 60–70% of the patients who would have an uncomplicated osteosynthesis (Lykke et al. Citation2003).
There is clearly a need for ways of determining which patients would benefit from internal fixation rather than a primary hip replacement. Preoperative selection criteria might be clinical or radiographic. The scientific evidence is, however, conflicting. In studies of older age groups, no ill effects of either age or sex were found (Nilsson et al. Citation1988, Alberts and JervaeusCitation1990, Strömqvist et al. Citation1992, Alho et al. Citation1999). Osteoporosis is more prevalent in older age groups and appears to be related to an increased risk of nonunion after internal fixation (Hedstrom Citation2004). On the other hand, some authors have recommended internal fixation for younger patients (Parker and Tagg Citation2002). Several studies have shown that the degree of initial displacement prognosticates failure, and others have found that comminution of the femoral calcar, size of the head and varus angulation affect healing (Alho et al. Citation1991, Citation1992, Nilsson et al. Citation1993).
At our institution, we have applied radiographic criteria in order to select patients who would benefit from internal fixation rather than primary hemiarthroplasty. We assumed that the rate of reoperation would be reduced after internal fixation. This prospective study was conducted to monitor the results of this strategy, and to investigate the usefulness of the proposed radiographic criteria in a clinical environment.
Patients and methods
All patients treated for hip fracture at the Department of Orthopedic Surgery of Østfold Hospital between September 1, 1998 and August 31, 2003 were included in a prospective hip fracture audit. For the present report, we have included patients with a displaced fracture of the femoral neck who were treated with internal fixation with Olmed screws or Exeter cemented hemiarthroplasty. Patients with a pathological fracture (9 patients) and undisplaced femoral neck fractures (20 patients) during the study period, and also those aged below 65 years (49 patients) were excluded. This left 683 patients in the study, who were followed for 1–6 years. Most patients were seen at the outpatient clinic 4 months and 1 year after the fracture, and all reoperations were recorded. In accordance with other studies, for this report we only included reoperations that were considered to be revisions of the index operation. This included dislocation of the prosthesis, even if it occurred only once. The hospital records of all patients were checked in order to make sure that no reoperation occurred unreported. We also recorded the date of death.
At the time of admission the choice of operation was made based on an evaluation of the patient's age, sex and physical and mental condition, as well as an evaluation of the radiographs of the fracture. The fracture was examined for the degree of angulation of the femoral head, the presence of comminution of the femoral calcar, and the size of the femoral head. Angulation of the head in excess of 30 degrees, presence of comminution of the femoral calcar, and a small head fragment were each considered to be predictive of reduced healing potential (Alho et al. Citation1992). Such fractures were treated by hemiarthroplasty. The findings in the radiographs were decisive in most cases, but in some instances very frail patients were treated with internal fixation.
The characteristics of the patients are shown in . There was no difference in mean age between the two groups, but significantly more men were treated with internal fixation.
Table 1. Background information on patients included in the study (683)
There was a non-significant trend toward treating patients in ASA groups 3 and 4 with internal fixation. There were variations in the choice of treatment of subgroups of patients admitted from different habitats, but walking ability did not have any bearing on the choice of treatment.
The majority of internal fixations were performed by residents (). There were 41 different residents, and each performed from 1 to 22 operations. 23 residents performed less than 5 internal fixations during the study period. Hemiarthroplasties were performed by an orthopedic surgeon or a resident assisted by an orthopedic surgeon.
Table 2. Time of day at start of surgery and status of performing surgeon. Values are number (%)
All patients were scheduled for a follow-up visit at 120 days. 111 patients died before the follow-up. 94 patients died after 120 days without having attended a follow-up, and 7 patients were lost to follow-up.
Statistics
The chi-squared test was used to compare proportions. For evaluation of risk factors and construction of survival curves, we used a Cox regression model and Kaplan-Meyer survival curves. Data are given with mean and 95% confidence interval. P-values below 0.05 were considered significant.
Results
We performed 9 revisions after hemiarthroplasty (2%; CI 0.7–3.3%) and 54 revisions after internal fixation (24%; CI 18–29%) (, ). Data were entered into a Cox regression model to investigate risk factors for revision. The initial analysis showed significant influence of primary operation (p < 0.001). The analysis was then redone separately for internal fixation and hemiarthroplasty. Hemiarthroplasty reduced the risk of revision by a factor of 0.08 (0.4–0.16). There was a significantly increased risk of revision for men treated with hemiarthroplasty compared to women, as well as for hemiarthroplasty performed in the evening ( and ). We were unable to identify any risk factors for revision in the case of internal fixation. There was a non-significant trend toward worse results when surgery was performed in the evening and at night compared to during the day ().
Figure 1. Survival of implant. Kaplan-Meyer curve of 455 hemiarthroplasties and 223 internal fixations.
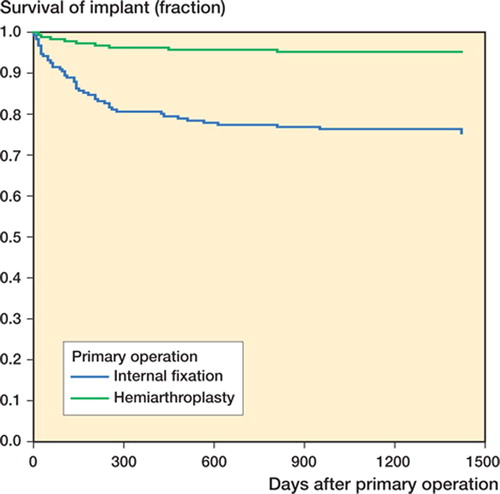
Table 3. Reason for revision and type of revision performed after internal fixation (228) and hemiarthroplasty (455)
Table 4. Risk of revision. Logistic regression analysis showing p-values, odds ratio (OR) with 95% confidence intervals (CI) of 683 fractures treated with internal fixation (228) or hemiarthroplasty (455)
Table 5. Significantly a better results when hemiarthroplasty is performed during daytime. Values are number (%)
Table 6. Non-significant a trend toward better results when internal fixation is performed during daytime. Values are number (%)
Mortality at 30 days was lower for internal fixation, but the difference was not statistically significant. Moreover, the difference decreased with time (). The survival curves are shown in . By using a Cox regression model, adjusting for patient-related factors as well as type of operation, time of day of operation and level of surgeon, we did not find any difference in mortality between internal fixation and hemiarthroplasty. The strongest predictors of increased mortality were sex, age, ASA groups 3–4, and not living in one's own home ().
Figure 2. Survival of patients. Kaplan-Meyer curve of 455 patients treated with hemiarthroplasty and 223 patients treated with internal fixation.
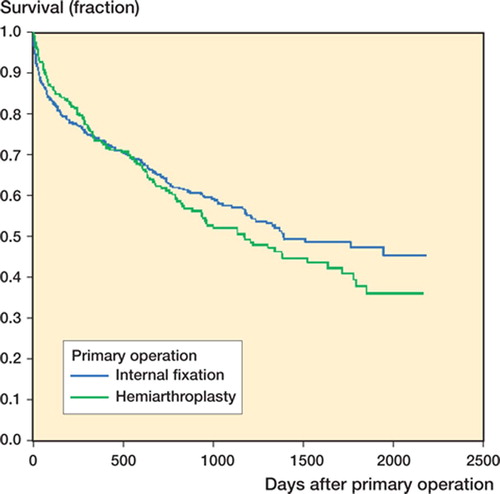
Table 7. Number of patients who had died by 30, 120 and 365 days. Values are number (%)
Table 8. Estimating risk of death after treatment of displaced fracture of the femoral neck in a Cox regression model showing odds ratio (OR), and 95% confidence interval (CI)
Discussion
In this prospective study, we selected patients with a displaced femoral neck fracture for internal fixation on the basis of radiographic criteria as described by Alho et al. (Citation1992). Our hypothesis was that selecting the patients with the best healing potential would reduce the number of unnecessary arthroplasties. Compared to other studies, our revision rate seems acceptable. However, the fractures with the assumed better healing potential that were treated with internal fixation had a significantly higher revision rate than the fractures treated with arthroplasty.
We have previously investigated the reliability of the criteria in a clinical setting (Bjorgul and Reikeras Citation2002) and we found that the interobserver reliability was low. There are many uncertainties in the clinical decision-making process, and several factors other than radiographic criteria might influence the choice of treatment. It is well documented that the quality of the surgery influences outcome when performing closed reduction and percutaneous osteosynthesis of a hip fracture (Garden Citation1961, Johansson et al. Citation2000). In this study, we did not collect data pertaining to the position of screws and perfection of reduction. It might be argued that performing a large number of hemiarthroplasties would reduce the level of competence in performing osteosynthesis. However, the level of competence of the surgeon did not influence our results. The 24% revision rate for internal fixation is similar to that in other reports from hospitals performing osteosynthesis almost exclusively (Lykke et al. Citation2003). One study has reported a 36% failure rate despite optimal screw placement and reduction in most patients (Tidermark et al. Citation2003). The revision rate in several randomized studies has ranged from 33% (Ravikumar and Marsh Citation2000) to 58% (Roden et al. Citation2003), so in that regard our results seem acceptable.
Although we recorded several parameters pertaining to the preoperative health status of the patient, we did not specifically record the patient's mental status. This might be a weakness of the study.
We found a non-significant trend toward worse results when the surgery was performed in the evening and at night. In this material, a relatively small proportion of operations were performed at night. The reason for this trend is not obvious. The level of expertise of the operating team might be different at night, and the patient may have had to wait longer. Furthermore, it is interesting that hemiarthroplasties performed between 4:00 p.m. and 12:00 midnight have significantly higher revision rates than hemiarthroplasties performed during daytime. These aspects of hip fracture treatment will be the subject of closer scrutiny.
Although several authors have claimed that arthroplasty should be the treatment of choice for displaced intracapsular fracture of the femur, others have maintained that selecting patients with reduced healing potential would reduce the number of unnecessary arthroplasties.
In 7 randomized controlled comparisons between internal fixation and prosthetic joint replacement, only 1 (Davison et al. Citation2001) found a significant difference in mortality. This report showed significantly better survival among patients treated with internal fixation than with hemiarthroplasty, measuring length of survival. 6 reports found no difference (Johansson et al. Citation2000, Ravikumar and Marsh Citation2000, Parker et al. Citation2002, Rogmark et al. Citation2002a, Roden et al. Citation2003, Tidermark et al. Citation2003), and this is reflected in the findings of a recent meta-analysis (Bhandari et al. Citation2003) incorporating most of these studies. In our study, we found no significant difference among the treatment groups—although there was a tendency for higher mortality within 30 days in patients treated with hemiprosthesis. Analysis in a Cox regression model revealed no difference in mortality between the groups.
We conclude that in our hospital, using radiographic criteria for determining choice of treatment for displaced femoral neck fractures has kept the revision rate low after internal fixation. However, even when we selected the patients with the assumed best healing potential, we did not even achieve the results of arthroplasty obtained with those patients who had the assumed worst healing potential. We recommend hemiarthroplasty as a safe method of treatment, and we recommend that it should be performed by trained operating teams during daytime.
This work was supported by grants from Stiftelsen Sofies Minde, The Norwegian Medical Association, The Norwegian Orthopaedic Association and Gjensidige Nor.
Contributions of authors
KB has been involved in all aspects of the investigation and completion of the paper. OR has participated in the conception and writing of the article.
- Alberts K A, Jervaeus J. Factors predisposing to healing complications after internal fixation of femoral neck fracture. A stepwise logistic regression analysis. Clin Orthop 1990, 257: 129–33
- Alho A, Benterud J G, Ronningen H, Hoiseth A. Radiographic prediction of early failure in femoral neck fracture. Acta Orthop Scand 1991; 62: 422–6
- Alho A, Benterud J G, Ronningen H, Hoiseth A. Prediction of disturbed healing in femoral neck fracture. Radiographic analysis of 149 cases. Acta Orthop Scand 1992; 63: 639–44
- Alho A, Benterud J G, Solovieva S. Internally fixed femoral neck fractures. Early prediction of failure in 203 elderly patients with displaced fractures. Acta Orthop Scand 1999; 70: 141–4
- Bhandari M, Devereaux P J, Swiontkowski M F, Tornetta P, III, Obremskey W, Koval K J, Nork S, Sprague S, Schemitsch E H, Guyatt G H. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg (Am) 2003; 85A: 1673–81
- Bjorgul K, Reikeras O. Low interobserver reliability of radiographic signs predicting healing disturbance in displaced intracapsular fracture of the femoral neck. Acta Orthop Scand 2002; 73: 307–10
- Davison J N, Calder S J, Anderson G H, Ward G, Jagger C, Harper W M, Gregg P J. Treatment for displaced intra-capsular fracture of the proximal femur. A prospective, randomised trial in patients aged 65 to 79 years. J Bone Joint Surg (Br) 2001; 83: 206–12
- Garden R S. Low-angle fixation in fractures of the femoral neck. J Bone Joint Surg (Br) 1961; 43: 647–63
- Hedstrom M. Are patients with a nonunion after a femoral neck fracture more osteoporotic than others? BMD measurement before the choice of treatment? A pilot study of hip BMD and biochemical bone markers in patients with femoral neck fractures. Acta Orthop Scand 2004; 75: 50–2
- Johansson T, Jacobsson S A, Ivarsson I, Knutsson A, Wahlstrom O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand 2000; 71: 597–602
- Lykke N, Lerud P J, Stromsoe K, Thorngren K G. Fixation of fractures of the femoral neck. A prospective, randomised trial of three Ullevaal hip screws versus two Hansson hook-pins. J Bone Joint Surg (Br) 2003; 85: 426–30
- Masson M, Parker M J, Fleischer S. Cochrane Database of Systematic Reviews. 2004
- Nilsson L T, Strömqvist B, Thorngren K G. Nailing of femoral neck fracture. Clinical and sociologic 5-year follow-up of 510 consecutive hips. Acta Orthop Scand 1988; 59: 365–71
- Nilsson L T, Johansson A, Strömqvist B. Factors predicting healing complications in femoral neck fractures. 138 patients followed for 2 years. Acta Orthop Scand 1993; 64: 175–7
- Palmer S J, Parker M J, Hollingworth W. The cost and implications of reoperation after surgery for fracture of the hip. J Bone Joint Surg (Br) 2000; 82: 864–6
- Parker M J, Tagg C E. Internal fixation of intracapsular fractures. J R Coll Surg Edinb 2002; 47: 541–7
- Parker M J, Khan R J, Crawford J, Pryor G A. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures in the elderly. A randomised trial of 455 patients. J Bone Joint Surg (Br) 2002; 84: 1150–5
- Ravikumar K J, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced sub-capital fractures of femur--13 year results of a prospective randomised study. Injury 2000; 31: 793–7
- Roden M, Schon M, Fredin H. Treatment of displaced femoral neck fractures: a randomized minimum 5-year follow-up study of screws and bipolar hemiprostheses in 100 patients. Acta Orthop Scand 2003; 74: 42–4
- Rogmark C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg (Br) 2002a; 84: 183–8
- Rogmark C, Carlsson A, Johnell O, Sernbo I. Primary hemiarthroplasty in old patients with displaced femoral neck fracture: a 1-year follow-up of 103 patients aged 80 years or more. Acta Orthop Scand 2002b; 73: 605–10
- Rogmark C, Carlsson A, Johnell O, Sembo I. Costs of internal fixation and arthroplasty for displaced femoral neck fractures: a randomized study of 68 patients. Acta Orthop Scand 2003; 74: 293–8
- Strömqvist B, Nilsson L T, Thorngren K G. Femoral neck fracture fixation with hook-pins. 2-year results and learning curve in 626 prospective cases. Acta Orthop Scand 1992; 63: 282–7
- Tidermark J, Ponzer S, Svensson O, Soderqvist A, Tornkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg (Br) 2003; 85: 380–8