Abstract
Background After total hip replacement, increased bone metabolism is seen. A local periprosthetic osteopenia can be measured by dual-energy X-ray absorptiometry (DXA), but it is still unkown whether biochemical markers can be used to monitor the local remodeling at an earlier stage.
Patients and methods In this prospective study we compared the biochemical markers tartrate-resistant acid phosphatase 5b (TRAP 5b), bone ALP, osteocalcin and CrossLaps with periprosthetic DXA in 17 consecutive patients after uncemented total hip replacement.
Results We found a highly significant early increase in TRAP 5b after 2 weeks and 6 weeks, which was followed by a densitometrically detectable decrease in bone mineral density after 26 weeks, especially in periprosthetic section Gruen zone 7. Bone ALP and osteocalcin levels as markers of osteoblast activity, and also Cross-Laps as a further marker of osteoclast activity, did not appear to allow any significant prediction of local bone remodeling.
Discussion Our findings show that TRAP 5b is a sensitive parameter for monitoring of osteoclast activity after cementless total hip replacement, and may predict local osteopenia.
Directly after total hip replacement, there are numerous changes in bone metabolism. The osteointegration of the protheses is a result of degradation and setting up of new bone, which can be described as bone remodeling. The main lines of cells responsible are osteoclasts and osteoblasts.
Whereas bone-specific alkaline phosphatase, osteocalcin and procollagen-1 propeptides are markers of osteoblast activity, hydroxyproline, crosslinked telopeptides, and pyridinoline are markers of bone resorption and are used to diagnose diseases of bone metabolism, osteoporosis, Paget’s disease, and bone metastases (Pagani et al. Citation2005).
TRAP 5b is a specific and sensitive marker enzyme of osteoclasts. The osteoclast-specific isoform 5b is detectable in serum, and its concentration is seen as a specific index of bone resorption. Even so, the use of TRAP 5b after endoprosthetic surgery and for monitoring of periprosthetic bone metabolism has not been established. TRAP 5b is produced by osteoclasts that endocytose products of bone matrix degeneration after secretion of acids and lysosomal proteases into the gap between cell membrane and bone matrix. Within the cell, trans-cytotic vesicles containing the products of bone matrix degeneration become fused to vesicles containing TRAP. The degradation products are then destroyed further by reactive oxygen species produced by TRAP (Halleen et al. Citation1996, 1999). Afterwards, the degradation products and the TRAP molecules are secreted through the basolateral membrane. Thus, there is a correlation between the amount of TRAP circulating and the amount of bone resorbed, which reflects the rate of bone resorption (Halleen et al. Citation2000, 2001). There is an immunoassay to specifically detect levels of the isoform TRAP 5b, which correlates with the activity of osteoclasts. Earlier studies have shown that TRAP 5b levels do not show cyclical variation and are not regulated by kidney or liver function (Halleen et al. Citation1996).
Osteocalcin is synthesized by osteoclasts and embedded in bone matrix, and is also secreted in the bloodstream. Alkaline phosphatase is not a unique enzyme but consists of genetically determined isoenzymes in the liver, bone, small intestine, placenta, bile duct, and in tumors. Elevation of liver or bone alkaline phosphatases is mostly responsible for an increase in total alkaline phophatase.
CrossLaps are products of degradation of type I collagen, which is the major component of organic bone matrix, and they are regarded as markers of bone resorption.
Due to the lack of a suitable research model for aseptic loosening, we looked into a clinical situation in which bone loss after joint replacement is known. In total hip replacement, changes in periprosthetic bone metabolism and bone mineral density around the implant are well described in the literature (Brown et al. 2003). These changes can be reliably measured and quantified by dualenergy X-ray absorbtiometry (DXA), which is a well-established and validated method of bone densitometry (Venesma et al. 2000, 2003, Wilkinson et al. Citation2001, 2003, Aldinger et al. Citation2003, Rahmy et al. Citation2003).
In this study we wanted to trace the course of markers of osteoblast and osteoclast activity and to compare these data with the radiographic findings of DXA. After hip replacement, there is an increase in bone remodeling and thus an increase in osteoblast and osteoclast activity also. We hoped to determine whether it would be possible to detect increased activity in bone metabolism through monitoring of biochemical markers, and whether it would be possible to detect the development of periprosthetic osteopenia earlier than can be shown radiographically.
Patients and methods
In this prospective study, 17 consecutive patients (9 women, mean age 64 (52–73), and 8 men, mean age 62 (39–75)) were examined over 6 months after uncemented total hip replacement due to primary arthrosis. Exclusion criteria were fractures, diseases of bone metabolism, Paget’s disease, endocrinological, nephrological or gastrointestinal disorders, therapy for osteoporosis, or tumor. All surgeries were elective without preceding trauma. An anterolateral approach was used. In all 17 patients, a proximal press-fit (PPF) stem was used. The PPF stem is non-coated, and made of Ti-Al6-V4 with a 12/14 taper. The proximal press fit allows proximal anchorage without transmission of distal load. The rectangular profile prevents rotation of the stem. Earlier studies have shown a low sintering of the stem. Body mass index was 26 (24–31) in women and 26 (19–30) in men.
Measurements of periprosthetic bone mineral density (BMD) were carried out 1, 2, 8, 16, and 26 weeks postoperatively using DXA (Hologic QDR 4500 Plus). A metal-removal algorithm allowed the measurement of BMD close to the implant. In addition to the complete periprosthetic BMD, a sub-analysis of the 7 zones of Gruen was made. In addition, the BMD of the lumbar spine was measured preoperatively and 26 weeks after operation in order to look for general osteoporosis. Blood testing was done on the day before surgery and 2, 3, 6, 8, 12, 16, and 26 weeks postoperatively. The parameters of interest were TRAP 5b, bone ALP, osteocalcin and CrossLaps. TRAP 5b was measured by using the test kit of Medac (Wedel, Germany). To measure osteocalcin and CrossLinks, we used the test kits of OsteoPark (Herlev, Denmark). For measurement of bone alkaline phosphatase, we used the test kit from Quidel Corporation (San Diego, CA).
Statistics
We used the Wilcoxon-Mann-Whitney U-test and the Spearman rank correlation. A p-value of < 0.01 was considered significant, and p < 0.001 to be highly significant.
Results
DEXA
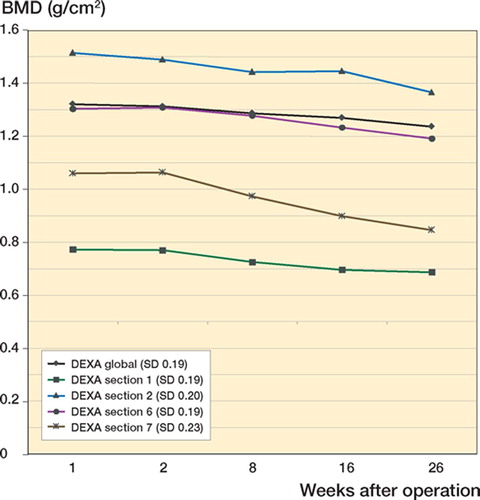
Periprosthetic BMD was initially measured for the total area around the prosthesis, and was considered a global value of all Gruen zones (1–7). The mean value (SD) of the BMD 1 week postoperatively was 1.32 (0.18) g/cm2. It showed a decrease after 26 weeks. In women, the decrease was from 1.25 g/cm2 to 1.2 g/cm2, and in men it was from 1.39 g/cm2 to 1.3 g/cm2. The time dependence of the periprosthetic BMD was in both sexes parallel. Separate evaluation of each section showed a clear alteration, especially in zone 7. The initial value was 1.06 (0.22) g/cm2 and showed a decrease of 20% after 26 weeks. The BMD of the lumbar spine (vertebrae 1–3) was mean 1.00 g/cm2 preoperatively and the same at 26 weeks postoperatively ().
TRAP 5b
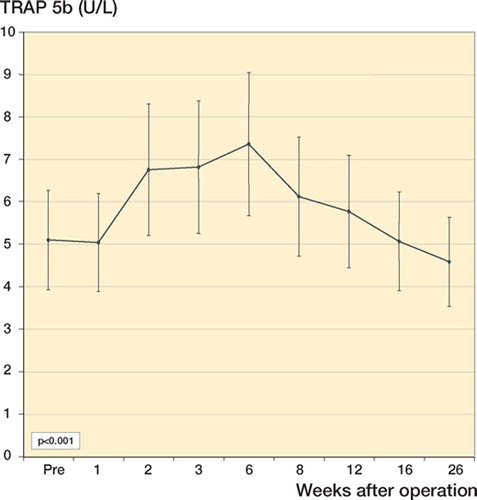
The mean value (SD) of TRAP 5b was 5.09 (1.38) U/L preoperatively, and it was the same 1 week after surgery. The first highly significant increase was seen 2 weeks after surgery. The peak was reached after 6 weeks (7.35 (1.90) U/L) (highly significant) and a decline after 26 weeks was measured. The percentage deviation in mean values was 33% after 2 weeks, 44% after 6 weeks, and –10% after 26 weeks ().
Bone ALP
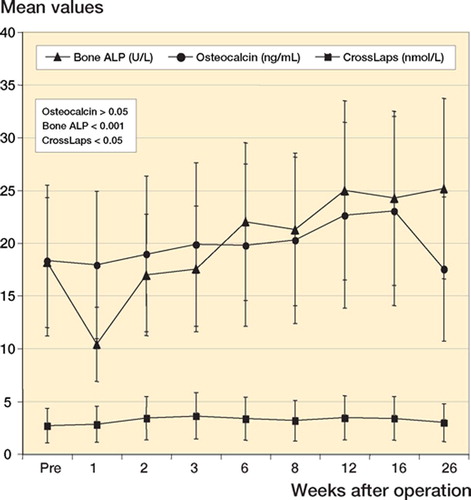
Preoperatively, the mean value (SD) of bone ALP was 18.1 (7.25) U/L. Whereas the first testing after 1 week showed a significant decrease, an increase was seen over the following weeks until the end of the measuring period (26 weeks) ().
Osteocalcin
The preoperative mean value (SD) was 18.3 (8.25) ng/mL. It showed a decrease after 1 week (not statistically significant) and a significant increase after 16 weeks. 26 weeks after surgery, it had declined to 17.5 (7.39) ng/mL ().
CrossLaps
The preoperative mean value (SD) was 2.70 (1.47) nmol/L. A significant peak was seen 3 weeks after surgery ().
Discussion
There is no method for early detection of aseptic loosening that is simple and cost-effective with a high degree of sensitivity and specificity. Some biochemical parameters might enable detection of early changes around the implant due to loosening. We thus set out to find a method of monitoring bone remodeling and osteoclast activity.
The implantation of prostheses leads to a remodeling of the interface. The initial primary stability of the prosthesis after implantation will give way to secondary stability through an osteointegrative process. The rebuilding of bone can be measured by DXA.
It is well known that there can be local osteopenia after implantation of a prosthesis, over the first 6–12 months. Brodner et al. (Citation2004) showed a significant decline in BMD in Gruen zones 1, 6, and 7 in 100 patients over a period of 5 years (Brodner et al. Citation2004). Also, Venesmaa et al. (Citation2003) found a total decline in periprosthetic BMD after uncemented hip replacement, with a maximum decline at distal zones 6 and 7. The effect was seen over a period of 3–5 years. Nishii et al. (Citation1997) also found a decrease in periprosthetic BMD around 32 cementless hip prostheses after 2 years (Nishii et al. Citation1997, Venesma et al. 2000, 2003, Wilkinson et al. Citation2001, 2003, Brodner et al. Citation2004). Aldinger et al. (Citation2003) confirmed the assumption that the main loss of BMD occurs during the first postoperative year (Aldinger et al. Citation2003).
Our findings correspond well with the results in the literature. Since a relationship between general osteoporosis and periprosthetic BMD was seen, we excluded patients with general osteoporosis by measuring BMD in the lumbar spine preoperatively and at the end of the study (Rahmy et al. Citation2003). We found a significant decline in total periprosthetic BMD after 8 weeks. Compared to all zones, the decline in zone 7 was highly significant and showed a further decline at the end of our study. A total decline in BMD of the overall area was seen but the findings did not approach statistical significance until the end of the sampling period. This typical loss of BMD after implantation of total hip prostheses can be explained by remodeling of the periprosthetic bone. A similar progression was also seen by other authors, with a peak after 1 year and measurable values after 5 years (Wilkinson et al. Citation2001, 2003, Venesma et al. 2003). Our findings correspond well with the data we found in the literature. We could not find a correlation between periprosthetic BMD and age, BMI, or sex. Thus, the parameters of bone metabolism measured should probably be ascribed to local rebuilding of the bone.
Parameters such as osteocalcin or bone ALP reflect osteoblast activity. The most sensitive parameter for measurement of bone resorption is CrossLaps in serum. However, published studies have only described the course of such parameters in patients with evident loosening of the prosthesis (Nishii et al. Citation1997, Pellengahr et al. Citation2001, Pagani et al. Citation2005).
There has been some controversy surrounding claims about parameters of bone resorption. Although some authors have found a significant increase in secretion of such parameters in urine (Witzleb and Menschikowski Citation2001), this has not been confirmed by others (Nishli et al. 1997, Pagani et al. Citation2005).
Our results regarding osteocalcin are in accordance with the findings published in the literature, that a significant increase can be seen only after 12–16 weeks (Pagani et al. Citation2005). The parameters of osteoblast activity do not show a consistent development over the follow-up period. They do not give any clear prediction of early remodeling in the early postoperative period. Bone ALP showed a significant increase at the end of our study.
We concentrated on the time-course of TRAP 5b—which reflects osteoclast activity specifi-cally—since aseptic loosening is always associated with activation of osteoclasts. Numerous studies have shown the sensitivity and specificity of TRAP 5b in reflecting osteoclast activity (Halleen et al. Citation2000, 2001), but there have been few studies on the application of TRAP 5b in monitoring of early prosthetic loosening. We found a significant percentage increase in TRAP 5b levels of 33% after 2 weeks and 44% after 6 weeks. The increase precedes the measurable decrease in periprosthetic bone mineral density seen by DXA. The peak in TRAP 5b was found after 6 weeks, with a subsequent decline. Bone loss is multifactorial and may be partly be related to weight bearing, trauma, stress shielding, or heparin. This effect is not dependent on the age, BMI, or sex of the patient. Measurement of TRAP 5b in serum is easy, and its value is independent of external influences.
Based on our results, we conclude that TRAP 5b is a useful biochemical parameter to monitor osteoclast activity in the initial phase of bone remodeling after total hip replacement. The changes in TRAP 5b levels precede radiographic changes, which are somewhat delayed after osteoclast activity has started. Further studies should be conducted to determine whether TRAP 5b monitoring is effective after total joint replacement. The benefit to patients would be enormous if early diagnosis of aseptic loosening were possible without the need for radiographic methods. Replacement surgery might be prevented by direct pharmaceutical intervention.
Contributions of authors
BH: patient treatment, statistical analysis, and writing of the paper. CE: surgeon. MF: patient treatment, DEXA measurement, and statistical analysis. LZ: surgeon, head of the department. AAK: surgeon, idea, study design and supervisor.
- Aldinger P. R, Sabo D., Pritsch M., Thomasen M., Mau H., Ewerbeck V., Breusch S. J. Pattern of periprosthetic bone remodelling around stable uncemented tapered hip stems: a prospective 84-month follow up study and a median 156-month cross-sectional study with DXA. Calcif Tissue Int 2003; 73: 115–21
- Brodner W., Bitzan P., Lomoschitz F., Krepler P., Jankovsky R., Lehr S., Kainberger F., Gottsauner. Changes in bone mineral density in the proximal femur after cementless total hip arthroplasty. A five-year longitudinal study. J Bone Joint Surg (Br) 2004; 86: 20, Brown A., Papp, J., Reiter, A. The periprosthetic bone remodelling process –signs of vital bone reaction. Int Orthop 2004: 27: S7-10
- Halleen J., Hentunen T. A., Hellmann J., Väänänen H. K. Tar-trate-resistant acid phosphatase from human bone: purification and development of an immunoassay. J Bone Min Res 1996; 11: 1444–52
- Halleen J., Räisänen S., Salo J. J., Hentunen T. A., Reddy S. V., Roodman D. G., Lehenkari P. P., Kaija H., Vihko P., Väänänen H. K. Intracelluar fragmentation of bone resorption products by reactive oxygene species generated by osteoclastic tartrate-resistant acid phosphatase. J Biol Chem 1999; 274: 22907–10
- Halleen J. M., Alatalo S. L., Suominen H., Cheng S., Janckila A. J., Väänänen H. K. Tartrate-resistant acid phosphatase 5b: a novel serum marker of bone resorption. J Bone Miner Res 2000; 15: 1337–445
- Halleen J. M., Alatalo S. L., Janckila A. J., Woitge H. W., Sebel M. J., Väänänen H. K. Tartrate-resistant acid phosphatase 5b is a specific and sensitive marker of bone resorption. Clin Chem 2001; 47: 597–600
- Nishii T., Sugano N., Masuhara K., Shibuya T., Ochi T., Tamura S. Longitudinal evaluation of time ralated bone remodelling after cementless total hip arthroplasty. Clin Orthop 1997; 339: 121–31
- Pagani F., Francucci C. M., Moro L. Markers of bone turnover: biochemical and clinicla perspectives. J Endorcinol Invest 2005; 28(10S)8–13
- Pellengahr C., Mayer W., Durr H. R., Maier M., Muller P., Veihelmann A., Zysk S., Jansson V., Refior H. J. The value of desoxypyridinoline in the diagnostic of loosened arthroplasty. Arch Orthop Trauma Surg 2001; 121(4)205–6
- Rahmy A. I., Gonsens T., Blake G. M, Tonino A., Fogelman I. Periprosthetic bone remodelling of two types of uncemented femoral implant with proximal hydroxyapatite coating: a 3-year follow-up study addressing the influence of prosthesis design and preoperative bone density on periprosthtic bone loss. Osteoporos Int 2003; 6, Epub
- Venesmaa P. K., Kroger H. P., Miettinen H. J., Jurvelin J. S., Suomalainen O. T., Alhava E. M. Bone loss around failed femoral implant measured by dual-energy-x-ray absorptiometry. J Orthop Sci 2000; 5: 380–4
- Venesmaa P. K., Kroger H. P., Jurvelin J. S., Miettinen H. J., Suomalainen O. T., Alhava E. M. Periprosthetic bone loss after cemented total hip arthroplasty; a prospective 5year dual energy radiographic absorptiometry study of 15 patients. Acta Orthop Scand 2003; 74(1)31–6
- Wilkinson J. M., Peel N. F. A., Elson R. A., Stockley I., Eastell R. Measuring bone mineral density of the pelvis and proximal femur after total hip arthroplasty. J Bone Joint Surg (Br) 2001; 83: 283–8
- Wilkinson J. M., Hamer A. J., Rogers A., Stockley I., Eastell R. Bone mineral density and biochemical markers of bone turnover in aseptic loosening after total hip arthroplasty. J Orthop Res 2003; 21: 691–6
- Witzleb W. C., Menschikowski M. Urinary concentration of collagen metabolits in endoprosthesis loosening. Z Orthop Grenzgeb 2001; 139(3)240–4