Abstract
Background Postoperative migration of a joint prosthesis is related to the risk of late loosening. We have previously reported that oral treatment with clodronate reduced migration of the cemented NexGen total knee prosthesis during the first postoperative year, as measured by radiostereometry (RSA). Oral bisphosphonate treatment is sometimes unpleasant, and local treatment will enable higher local concentrations. We now report the results of local peroperative treatment with another bisphosphonate, ibandronate, with the same prosthesis.
Methods This is a double-blind, randomized study of 50 patients using RSA with maximal total point motion (MTPM) as primary effect variable. 1 mg ibandronate (1 mL) or 1 mL saline was applied to the tibial bone surface 1 min before cementation. RSA examination was done on the first postoperative day, and at 6, 12, and 24 months.
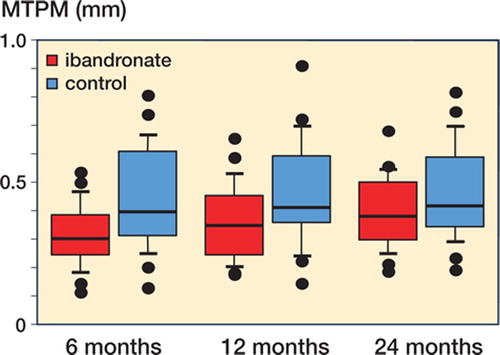
Results One ibandronate-treated patient died of unrelated causes, and 1 control patient refused to come for follow-up, leaving 24 patients in each group for analysis. There were no cases of aseptic loosening. By repeated measures ANOVA, migration (MTPM) was reduced by local application of ibandronate (p = 0.006). The effect was most pronounced at 6 months, with a reduction from 0.45 to 0.32 mm (95% CI for reduction: 0.04–0.21 mm). At 12 months, the migration from the postoperative examination was reduced from 0.47 to 0.36 mm (95% CI for reduction: 0.02–0.20 mm). At 24 months, the reduction was from 0.47 to 0.40 mm (95% CI: -0.01–0.16 mm).
Interpretation This is the first study to show improvement of prosthesis fixation by local pharmacological treatment in humans. The treatment appears to be safe, cheap, and easy to perform. However, the improvement in postoperative stability was not greater than with systemic clodronate treatment.
The risk of late loosening of cemented knee prostheses is related to early fixation, as measured by radiostereometric analysis (RSA) (Ryd et al. Citation1995). It was previously thought that early fixation (defined as migration during the first and second year, as measured by RSA) is a purely mechanical phenomenon. However, osteocytes next to an implant will die postoperatively because of the operative trauma or circulatory disturbance. This leads to increased bone resorption at the interface, and reduced quality of the fixation (Dhert et al. Citation1998). There is also a fracture repair response to the trauma, leading to increased bone formation. Early implant fixation should therefore be dependent on the balance between these two responses. Because bisphosphonates impair bone resorption, they should lead to a more positive balance, leading to better early fixation. This is indeed the case: we have shown that fixation of the tibial component of a total knee prosthesis is improved by giving a bisphosphonate orally once daily for the first half year after surgery (Hilding et al. Citation2000). The migration, measured by RSA, was reduced by one quarter during the first 6 months, and the difference between the groups persisted for 4 years (Hilding and Aspenberg Citation2006). We now report the results of a similar study in which the bisphosphonate was given locally during the operation.
Patients and methods
Overview
In a double-blind study, we randomized 50 patients who were scheduled to receive a NexGen cemented knee prosthesis, to local treatment with ibandronate (Bondronate; Roche) or placebo. Immediately before cementation, 1 mg of ibandronate (1 mL) or 1 mL saline was applied to the prepared tibial bone surface. Patients were examined with RSA postoperatively and at 6, 12, and 24 months.
The study was approved by the regional ethics committee and the Swedish national drug agency, and the patients signed an informed consent form.
Patients
We recruited 50 patients for this study, according to power calculations based on our previous series with systemic treatment. Inclusion criteria were gonarthrosis stage 3–5 according to Ahlbäck (Citation1968), and age 60–75 years. Exclusion criteria were cortisone or bisphosphonate medication, rheumatoid arthritis, or any other systemic illness affecting the skeleton—as well as generally poor health or inability to cooperate.
The operations were performed in the city of Köping by the first author in a standardized manner with cemented NexGen implants (Zimmer, Warsaw, IN). Tantalum markers of 0.8 mm were implanted in the proximal tibia (8–10 markers) and in the plastic insert (4 markers).
Randomization was done in blocks of 10 patients. Shortly before cementation, a sealed envelope with the patient's inclusion number on it was opened by a person outside the operating theater. She prepared a syringe with either 1 mL of ibandronate solution (Bondronat; Roche, Mannheim, Germany) or saline according to the instructions in the envelope, and sent it in to the surgical team. The paper from the envelope was immediately destroyed. This procedure meant that the person outside the operating theater was not blinded. This was unavoidable, as our study had no industrial support and thus identical placebo and treatment vials could not be produced. However, the person outside was not otherwise involved with the surgical team, and different people performed this task on different days. There was no way in which the surgeon could have been informed or infiuenced regarding the treatment. Moreover, the RSA analysis was done by a blinded technician in a different city (Linköping), who had never met the patients or the surgeon.
The operations were done in blood-less field, and the bone surfaces cleaned by high-pressure lavage. The porous tibial bone surface was gently dried with a cloth and the solution in the syringe was poured onto it. The solution was readily confined by the porous bone. After 1 min, cementation was started.
Radiographs for RSA were taken on the first postoperative day and at 6, 12, and 24 months. 2 films were taken simultaneously at a 90° angle with the knee inside a calibration cage, according to RSA standards. The analyses of the radiostereometric radiographs were done using the UmRSA 4.1 system.
Statistics
No values were excluded from the analysis. The primary effect variable chosen was MTPM of all time points combined, analyzed by repeated measures ANOVA (SPSS version 12.0). Appropriateness of the data ditribution was checked with Mauchly's test. Individual time points are described with confidence intervals for the difference between the means. We also studied translation along the y-axis (sinking) using the same tests, and rotation around the transverse and sagittal axes (backward-forward tilt and sideways tilt). Rotation was analyzed by F-test, because a difference in variation is likely to be more important than differences in mean values: both a high negative value and a high positive value represent undesired motion.
Results
One ibandronate-treated patient died of unrelated causes, and 1 control patient refused to come for follow-up, leaving 24 patients in each group for analysis. For these patients, 3 of the 144 scheduled follow-up visits were missed. All beads in the plastic insert were visible from both radiographic expo sures in 183 of the 189 examinations. All other data were complete.
There were no cases of aseptic loosening, by clinical criteria or radiographic zones. By repeated measures ANOVA, migration (MTPM) was reduced by local application of ibandronate (p = 0.006) . The effect was most pronounced at 6 months, with a reduction from 0.45 to 0.32 mm (95% CI for reduction: 0.04–0.21). At 12 months, the migration from the postoperative examination was reduced from 0.47 to 0.36 mm (95% CI: 0.02– 0.20). At 24 months, the reduction was from 0.47 to 0.40 mm (95% CI: -0.01–0.16 mm). Ibandronate also influenced prosthesis migration along the y-axis (repeated measures ANOVA, p = 0.009). By F-test, rotation either way around the transverse or sagittal axes was reduced at 6 months (p = 0.04 and 0.02, respectively), but not significantly at later time points .
Box plot showing 10th, 25th, 50th, 75th, and 90th percentile and outliers for MTPM at 6, 12, and 24 months. Controls in blue, ibandronate-treated in red.
Results for maximal total point motion (MTPM) and sinking (trans y) in mm, and for forward tilting (rot x) and medial tilting (rot z) in degrees. Mean differences between control and ibandronate groups are given with 95% confidence interval (CI). P-values for Levene's test for equality of variances and for t-test are not corrected for multiplicity of comparisons and should be regarded as being descriptive
The reduced MTPM as a result of ibandronate was accompanied by a reduced tendency of the prosthesis to “lift off” from the bone (negative values for y-translation), something which occurred in half of the controls. This appears to refiect reduced wobbling around the horizontal axes in the ibandronate group.
When we excluded the 6 patients for whom one bead was masked during an examination, the result remained significant (p = 0.01).
Discussion
These results show that local application of a bisphosphonate during total joint surgery reduces migration. This confirms our previous results that early migration is dependent on osteoclast activity, and that pharmacological treatment can have a measurable effect on the mechanics of total joint replacement surgery (Hilding et al. Citation2000, Hilding and Aspenberg Citation2006). The total dose was no higher than what is accepted for a single intravenous injection. Bisphosphonates tend to bind almost irreversibly to bone surfaces. Because we applied the bisphosphonate after lavage of exposed bone surfaces and with a blood-less field without local circulation, it is likely that only a small proportion entered the general circulation. The treatment takes 1–2 min and is inexpensive and simple, and appears to be safe.
The risk of aseptic loosening is related to postoperative migration. However, in the Swedish Knee Arthroplasty Registry (Citation2005), the revision rate at 10 years was around 5%, but only a quarter of these revisions were due to aseptic loosening. It is therefore likely that few of our 48 patients are at risk of aseptic loosening. In accordance with this, only 1 of our patients showed migration exceeding 0.25 mm during the second postoperative year, which is the cut-off level suggested to signal an increased risk (Ryd et al. Citation1995) (the value was 0.27 mm and may have been be a random error). Thus, if we regard migration as a surrogate variable for loosening, we would need to include enough patients to show a statistically significant reduction in the number of outliers above this cut-off level, something which is hardly possible. However, because we did find a reduction in the mean value—from little to even less migration—it is likely that the number of outliers in a larger sample would be reduced. It also appears likely that the improvement in fixation by adding a bisphosphonate could especially benefit patients with an increased risk of loosening, such as the young and very active.
We used MTPM as primary outcome variable because it is influenced by all kinds of movement. It is a less descriptive variable than rotations and translations of the center of gravity of the rigid body, but appears good for picking up group differences. It is therefore suited for comparisons between groups with identical implants. The other RSA variables in this study were not used for hypothesis testing, but appear to indicate that ibandronate reduced wobbling around vertical axes, similar to systemic clodronate (Hilding and Aspenberg Citation2006).
In our previous study with systemic treatment, the bisphosphonate was given for 6 months following the operation (Hilding et al. Citation2000). In the present study, it is possible that the bisphosphonate applied was slowly eliminated from the site, so that the local amount was likewise insufficient after 6 months. Preliminary data from rat experiments indicate that most of a radiolabeled bisphosphonate has been cleared away from a cancellous bone site 8 weeks after local application, obviously through osteoclastic resorption in spite of the bisphosphonate (data not shown). This might explain why we see no certain effect of the bisphosphonate on the migration rate after the first 6 postoperative months. However, according to the theory of early loss of fixation (Mjoberg Citation1997) and if we also consider previous RSA data (Ryd et al. Citation1995), it appears likely that the first 6 months is the critical period.
In normal bone remodeling, there is a coupling between bone resorption and bone formation. Accordingly, bisphosphonates reduce both bone resorption and formation in the treatment of osteoporosis. This is not so in situations such as implant fixation, where resorption and formation are uncoupled. Decreased resorption by a bisphosphonate leaves formation partially undisturbed, so that a net gain in bone is achieved. This net anabolic response has been observed in several animal models (Little et al. Citation2003, Bobyn et al. Citation2005), including models of early implant fixation. In one such model for cancellous bone, the net anabolic effect is more important for strength of fixation than the preservation of pre-existing bone (Wermelin et al. Citation2007). It is possible that this was also the case in our patients. We chose ibandronate, but there is no reason why a corresponding dose of any injectable bisphosphonate would not do instead.
This is the first study to show improvement of prosthesis fixation by local pharmacological treatment in humans. We used a bisphosphonate both for protection of pre-existing bone, but also as a net anabolic agent. Other anabolic agents, notably intermittent PTH, have shown even higher potency for improvement of implant fixation in animal models (Skripitz and Aspenberg Citation2004), and might be worth trying clinically.
PA has applied for a patent on a method for drug application to bone surfaces.
This study was supported by the Swedish Research Council (project 2031) and the strategic research program Materials in Medicine, Linkoping University, Sweden. Ulf Kallander, Linköping University, performed the RSA.
Contributions of authors
MH performed all the clinical work, including recruiting, operating, and following the patients. PA performed the analysis and wrote the manuscript. The study was conceived and planned by both authors together.
- Ahlbäck S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn (Stockh) 1968; 277(Suppl)7–72
- Bobyn J D, Hacking S A, Krygier J J, Harvey E J, Little D G, Tanzer M. Zoledronic acid causes enhancement of bone growth into porous implants. J Bone Joint Surg (Br) 2005; 87(3)416–20
- Dhert W J, Thomsen P, Blomgren A K, Esposito M, Ericson L E, Verbout A J. Integration of press-fit implants in cortical bone: a study on interface kinetics. J Biomed Mater Res 1998; 41(4)574–83
- Hilding M, Aspenberg P. Postoperative clodronate decreases prosthetic migration: 4-year follow-up of a randomized radiostereometric study of 50 total knee patients. Acta Orthop 2006; 77(6)912–6
- Hilding M, Ryd L, Toksvig-Larsen S, Aspenberg P. Clodronate prevents prosthetic migration: a randomized radiostereometric study of 50 total knee patients. Acta Orthop Scand 2000; 71(6)553–7
- Little D G, Smith N C, Williams P R, Briody J N, Bilston L E, Smith E J, Gardiner E M, Cowell C T. Zoledronic acid prevents osteopenia and increases bone strength in a rabbit model of distraction osteogenesis. J Bone Miner Res 2003; 18(7)1300–7
- Mjoberg B. The theory of early loosening of hip prostheses. Orthopedics 1997; 20(12)1169–75
- Ryd L, Albrektsson B E, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg (Br) 1995; 77(3)377–83
- Skripitz R, Aspenberg P. Parathyroid hormone--a drug for orthopedic surgery. Acta Orthop Scand 2004; 75(6)654–62
- The Swedish Knee Arthroplasty Register. 2005, Annual report http://www.knee.nko.se/english/online/uploaded-Files/107_SKAR2005_Englv2.pdf
- Wermelin K, Tengvall P, Aspenberg P. Surface bound bisphosphonates enhance screw fixation in rats. Increasing effect up to 8 weeks after insertion. Acta Orthop 2007; 78(3)385–92
