Abstract
Background and purpose In the classic Hirabayashi procedure, the lamina door is tethered open by sutures between the spinous process and facet capsule or para-vertebral muscle. Our early experiences showed, however, that the loosened sutures result in dislodgement and reclosure of the lifted lamina. We present a modified method to ensure secure fixation and prevent restenosis due to hinge closure.
Patients and methods 12 patients with cervical spon-dylotic myelopathy underwent unilateral open-door laminoplasty using suture anchor fixation between 2000 and 2004. The sutures were tied and fixed onto the holed lateral mass screws, instead of using the conventional suture technique. We used radiography, MRI, and CT for imaging studies. The Nurick score was used to assess severity of myelopathy, and the Japanese Orthopedic Association (JOA) score was used to evaluate clinical outcomes before surgery and at the last follow-up visit.
Results All patients experienced functional improvement of at least 1 Nurick score after surgery. The JOA score for the 12 patients increased significantly from 6.9 (SD 3.0) before surgery to 13 (SD 1.6) at final follow-up. Postoperative radiography and CT showed increased sagittal diameter and canal expansion. Average preoper-ative and postoperative ranges of motion for the cervical spine were 48 (SD 4.6) and 36 (SD 2.7), respectively. No neurological deterioration due to hinge reclosure and no major surgery-related complications were observed during the follow-up period.
Interpretation Open-door laminoplasty using suture anchor fixation effectively maintains expansion of the spinal canal and resists closure while preserving alignment and flexibility. This modified technique is easy to use, has a low complication rate, and provides marked functional improvement for patients with cervical spon-dylolytic myelopathy.
Because of unfavorable long-term outcomes associated with laminectomy, expansive laminoplasty has gradually become a preferred procedure for almost all patients with cervical myelopathy or myelora-diculopathy caused by multilevel spinal stenosis, with the exception of those with preoperatively established kyphotic deformity or segmental instability (Nakano et al. Citation1988, Heller et al. Citation2001). In Citation1973, Oyama et al. first proposed an expansive laminoplasty using Z-plasty of thinned lamina. The procedure did not gain widespread use, as it is time consuming and requires exceptional skill. In Citation1978, Hirabayashi introduced unilateral open-door laminoplasty, a reportedly simpler and safer approach than Z-shaped laminoplasty (Hirabayashi et al. Citation1983). In the classic Hirabayashi technique, the lamina door is tethered open via sutures through the spinous process and facet capsule or paraver-tebral muscle, which are then tied to prevent closure of the lifted lamina. We developed a modified method using suture anchor fixator to secure fixation, and now present the technique and the clinical results of our first 12 patients.
Patients and methods
BetweenJanuary 2000 and January 2004,12patients (7 males) underwent open-door laminoplasty using suture anchor fixation for treating cervical spondy-loltic myelopathy at our institution. Mean patient age at surgery was 62 (56–68) years. All patients met the following enrollment criteria: (1) a clear history of progressive neurological deficit due to cervical spondylotic myelopathy, (2) comparable radiography, MRI, and CT findings verifying multilevel cervical stenosis, and (3) acceptable cervical spine alignment without kyphotic deformity or radiological signs of instability. Patients with ossification of the posterior longitudinal ligaments or a history of cervical spine surgery were excluded. 9 patients had 4 levels of decompression (C3–6), and 3 patients had 5 levels of decompression (C3–7).
The number of lateral mass screws used was based on the cervical spine level requiring decompression. After surgery, patients wore a neck collar for 4-week protection, and began isometric exercises to rehabilitate the cervical spine as permitted by wound pain.
We evaluated patient outcome using the Nurick score (Nurick Citation1972) and the Japanese Orthopedic Association (JOA) score (Hirabayashi et al. Citation1983). The Nurick score was used to assess the severity of myelopathy, and the JOA score was adopted to evaluate the clinical outcomes before surgery and at the last follow-up visit. The JOA score recovery rate was calculated based on the following equation: recovery rate (%) = (final JOA score - preop-erative JOA score) / (17 - preoperative JOA score) x 100%.
Canal diameter was defined as the distance from the posterior aspect of the intervertebral disc to the anterior edge of the spinous process, based on a cross-sectional view on CT. Cervical ROM was measured as the angle between C2 and C7 on lateral maximal flexion and extension radiographs. The mean follow-up period was 32 (24–50) months.
Statistics
The Wilcoxon signed rank test and paired Student's t-test were used to compare results before and after surgery. A p-value of < 0.05 was considered statistically significant.
Surgical technique
The patient is placed in prone position and prepared with the neck in mild flexion. The spinous process, cervical lamina, and associated lateral mass from C2 to T7 are approached in a standard fashion. Connecting holes are created using a 2-mm cutting burr on both sides of each spinous process at the decompression levels. Insertion holes for the lateral mass screws are prepared at the hinge side. The holes are drilled approximately 11 mm deep into the surrounding bony structure. The gutter is first drilled on the lateral margin of the lamina on the open side. A high-speed spherical cutting burr is initially employed to remove the outer cortex and cancellous bone. The retained groove bottom is resected using a diamond burr. The bony gutter on the hinge side is drilled slightly more laterally than that on the open side, to prevent the lamina hinge from becoming unstable. As the inner cortex in thinned, the spinous process is pushed carefully using repetitive movements.
When the lamina door is ready to be opened, the holed lateral mass screws are inserted into the holes prepared previously, deepening until the screw hole remains exposed. The titanium alloy screw component (14 mm long and 4 mm in diameter) of the Window anterior cervical plate system (A-spine, Taiwan) is employed to create a hole at the neck portion. Once the holed screws are fixed into the lateral mass, non-absorbable sutures are passed through the screw holes and drilled holes in the spinous process ().
Figure 1. The insert (A) shows a holed lateral mass screw and a non-absorbable stitch. The sutures introduced previously are tied tightly to keep the lifted lamina open (B).
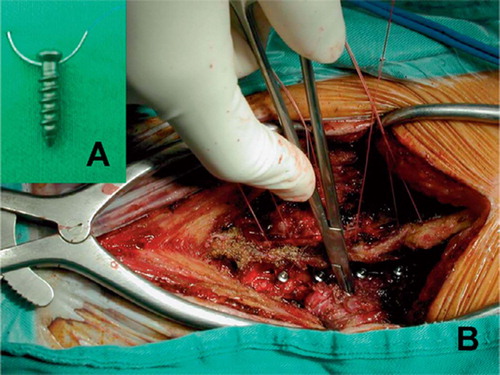
Just before opening the lamina, the patient's neck is changed to neutral position. The lamina door is then raised incrementally from C7 to C3 by bending open the hinge in a greenstick fashion. Until the lamina door on the open side becomes almost horizontal, the sutures introduced previously are tied tightly to prevent closure of the lifted lamina.
Results
No restenosis due to hinge closure was noted and there were no major surgery-related complications (). Progression of myelopathy was arrested in all patients. The Nurick score improved from 3 (2–4) before surgery to 2 (1–3) after surgery (p = 0.002). The mean JOA score increased from 6.9 (SD 3.0, range 2–12) before surgery to 13 (SD 1.6, range 10–15) at final follow-up (p < 0.001).
Figure 2. Comparison of postoperative and postoperative axial CT scans revealed widening of the spinal canal after unilateral open-door laminoplasty using suture anchor fixation.
1 patient experienced transient motor paresis in the C5 segment postoperatively, which recovered spontaneously within 3 months.
By radiography, none of the patients had progressive kyphotic deformity postoperatively compared to preoperative alignment. Mean canal diameter increased from 9.2 (SD 0.8, range 8.5–11) to 14 (SD 1.2, range 12–17) at intervertebral disc level on axial CT scan (p < 0.001). Mean ROM of the cervical spine decreased from 48 (SD 4.6, range 38–52) before surgery to 36 (SD 2.7, range 32–40) at final follow-up (p < 0.001).
Discussion
The choice of treatment for multilevel cervical spondylotic myelopathy has been debated (Wada et al. Citation2001, Edwards et al. Citation2002). Optional procedures include posterior approaches, such as a laminectomy or laminoplasty, and anterior approaches, such as a corpectomy or adjacent multiple discec-tomies. Laminoplasty is preferable, as it has fewer complications and less functional impairment (Nakano et al. Citation1988, Heller et al. Citation2001).
Table 1. Patient demographic data and clinical outcomes
Table 2. Comparison of axial CT scan and radiographic parameters before and after surgery
Various modifications and supplementary instruments for laminoplasty have been devised to maintain hinge patency and provide secure fixation, such as hydroxyapatite spacer, ceramic lamina, miniplate osteosynthesis, and allogenic or autogenous bone grafting (Hase et al. Citation1991, Hoshi et al. Citation1996, O'Brien et al. Citation1996). Autografts are certainly the ideal spacer, with considerable osteogenic and osteoconductive potential. However, donor site morbidity, limited availability, and a second operation to harvest the graft are important disadvantages of autografts (Goulet et al. Citation1997). Allografts provide structural support similar to nonvascular-ized cortical autografts; however, the source is limited and the risk of virus transmission cannot be eliminated (Tomford Citation1995). The cost of commercial bone substitutes limits their use in developing and underdeveloped countries. Furthermore, the healing process between an artificial spacer and host bone is another issue (An et al. Citation1995). In addition, insertion of screws into a floating lamina is technically demanding and time consuming when a miniplate is used to fix a lamina door.
In considering the above-mentioned drawbacks and the difficulty in maintaining a patent lamina hinge, we developed a suture anchor fixator that consists only of holed screws and non-absorbable sutures. When used with unilateral open-door laminoplasty, this modified technique provides secure fixation and prevents restenosis prior to hinge union. The instrument is user-friendly for experienced spine surgeons, and easier than conventional expansive laminoplasty with adjunctive procedures for maintaining hinge patency.
Graham et al. (Citation1996) investigated the clinical safety of lateral mass screws by determining the anatomical location and clinical complications in a consecutive patient series. There was only a 1.8% per-screw risk of radiculopathy when bicortical screw purchase was attempted. In a mechanical study comparing the safety and efficacy of uni-cortical screws and bicortical lateral mass screws for cadaveric cervical spines, Seybold et al. (Citation1999) reported no statistically significant difference in pullout strength, or pullout strength in association with zone placement for both screws. They suggested using 14-mm unicortical lateral mass screws (effective length, 11 mm) placed in a superolateral trajectory in the adult cervical spine to provide equivalent pullout strength with a considerably lower risk of injury than that when using longer bicortical screws placed in a similar orientation, regardless of the slight variation in desired trajectory. Several studies have also shown lateral mass screw technique to be mechanically sound and technically reproducible (An et al. Citation1991, Heller et al. Citation1991). The learning curve is short for surgeons who are already familiar with cervical spine surgery.
The clinical outcomes obtained with this modified technique were as good as those in other studies, judging by the recovery rates given in the literature (Naito et al. Citation1994, Yue et al. Citation2000, Park and Heller Citation2006). Postoperative interlaminar bony fusion with reduced cervical ROM has been reported to occur in patients undergoing laminoplasty (Seichi et al. Citation2001, Kawaguchi et al. Citation2003, Iizuka et al. Citation2006). In our modified method with secure anchor fixation, the ROM values were not compromised, which may have been due to the possibility of undergoing early physiotherapy.
In conclusion, this simple technique is easy to use with a minimum of complications, and most importantly, it effectively maintains spinal canal expansion and resists closure of the open lamina through secure fixation.
No funds were received in support of this work. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Contributions of authors
SCY examined all patients, collected the data, and prepared the manuscript. CCN and WJC performed the surgery and revised the article for intellectual content. CHW and SWY supervised the statistical analyses and proofread the manuscript.
- An H S, Gordin R, Renner K. Anatomic considerations for plate-screw fixation of the cervical spine. Spine 1991; 16: S548–51
- An H S, Simpson J M, Glover J M, Stephany J. Comparison between allograft plus demineralized bone matrix versus autograft in anterior cervical fusion. A prospective multi-center study. Spine 1995; 20: 2211–6
- Edwards C C, II, Heller J G, Murakami H. Corpectomy versus laminoplasty for multilevel cervical myelopathy: an independent matched-cohort analysis. Spine 2002; 27: 1168–75
- Goulet J A, Senunas L E, DeSilva G L, Greenfield M L. Autogenous iliac crest bone graft. Complications and functional assessment. Clin Orthop 1997, 339: 76–81
- Graham A W, Swank M L, Kinard R E, Lowery G L, Dials B E. Posterior cervical arthrodesis and stabilization with a lateral mass plate. Clinical and computed tomographic evaluation of lateral mass screw placement and associated complications. Spine 1996; 21: 323–8
- Hase H, Watanabe T, Hirasawa Y, Hashimoto H, Miyamoto T, Chatani K, Kageyama N, Mikami Y. Bilateral open laminoplasty using ceramic laminas for cervical myelopathy. Spine 1991; 16: 1269–76
- Heller J G, Carlson G D, Abitbol J J, Garfin S R. Anatomic comparison of the Roy-Camille and Magerl techniques for screw placement in the lower cervical spine. Spine 1991; 16: S552–7
- Heller J G, Edwards C C, II, Murakami H, Rodts G E. Laminoplasty versus laminectomy and fusion for multilevel cervical myelopathy: an independent matched cohort analysis. Spine 2001; 26: 1330–6
- Hirabayashi K. Expansive open-door laminoplasty for cervical spondylotic myelopathy. Shujutsu 1978; 32: 1159–63
- Hirabayashi K, Watanabe K, Wakano K, Suzuki N, Satomi K, Ishii Y. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine 1983; 8: 693–9
- Hoshi K, Kurokawa T, Nakamura K, Hoshino Y, Saita K, Miyoshi K. Expansive cervical laminoplasties--observations on comparative changes in spinous process lengths following longitudinal laminal divisions using autogenous bone or hydroxyapatite spacers. Spinal Cord 1996; 34: 725–8
- Iizuka H, Iizuka Y, Nakagawa Y, Nakajima T, Toda N, Shimegi A, Tsutsumi S, Takagishi K. Interlaminar bony fusion after cervical laminoplasty: its characteristics and relationship with clinical results. Spine 2006; 31: 644–7
- Kawaguchi Y, Kanamori M, Ishihara H, Ohmori K, Abe Y, Kimura T. Pathomechanism of myelopathy and surgical results of laminoplasty in elderly patients with cervical spondylosis. Spine 2003; 28: 2209–14
- Naito M, Ogata K, Kurose S, Oyama M. Canal-expansive laminoplasty in 83 patients with cervical myelopathy. A comparative study of three different procedures. Int Orthop 1994; 18: 347–51
- Nakano N, Nakano T, Nakano K. Comparison of the results of laminectomy and open-door laminoplasty for cervical spondylotic myeloradiculopathy and ossification of the posterior longitudinal ligament. Spine 1988; 13: 792–4
- Nurick S. The pathogenesis of spinal cord disorder associated with cervical spondylosis. Brain 1972; 95: 87–100
- O'Brien M F, Peterson D, Casey A T, Crockard H A. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization. A computerized morphometric analysis. Spine 1996; 21: 474–83
- Oyama M, Hattori S, Noriwaki N. A new method of cervical laminectomy. Chubuseisaisi 1973; 16: 792–4
- Park A E, Heller J G. Outcomes review of laminoplasty for the treatment of multilevel cervical spondylotic myelopathy. Curr Opin Orthop 2006; 17: 268–73
- Seichi A, Takeshita K, Ohishi I, Kawaguchi H, Akune T, Anamizu Y, Kitagawa T, Nakamura K. Long-term results of double-door laminoplasty for cervical stenotic myelopathy. Spine 2001; 26: 479–87
- Seybold E A, Baker J A, Criscitiello A A, Ordway N R, Park C K, Connolly P J. Characteristics of unicortical and bicortical lateral mass screws in the cervical spine. Spine 1999; 24: 2397–403
- Tomford W W. Transmission of disease through transplantation of musculoskeletal allografts. J Bone Joint Surg (Am) 1995; 77: 1742–54
- Wada E, Suzuki S, Kanazawa A, Matsuoka T, Miyamoto S, Yonenobu K. Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy: a long-term follow-up study over 10 years. Spine 2001; 26: 1443–7
- Yue W M, Tan C T, Tan S B, Tan S K, Tay B K. Results of cervical laminoplasty and a comparison between single and double trap-door techniques. J Spinal Disord 2000; 13: 329–35
