Abstract
Background and purpose There have been few reports regarding the proximally based sural artery flap, which is useful for reconstruction of soft tissue defects around the knee and on the proximal third and middle third of the lower leg. Here we report our experience with 10 patients.
Patients The defects in our 10 cases were around the knee (4), on the proximal third of the lower leg (4), and on the middle third (2). 8 patients had fasciocutaneous flaps and 2 had adipofascial flaps. The flap size ranged from 4 to 10 cm in length, and from 5 to 8 cm in width. The pedicle length ranged from 12 to 20 cm.
Results All 10 flaps survived. Congestion and tip necrosis occurred in 1 case with a fasciocutaneous flap, which healed without complications. A superficial infection occurred in 1 case with a fasciocutaneous flap, which healed with antibiotic treatment. Necrosis of grafted skin occurred in 2 cases of adipofascial flap; only one of them, however, required additional surgery. No morbidity of the donor site and no functional deficits were detected in any of the 10 cases.
Interpretation The proximally based sural artery flap is useful for reconstruction of soft tissue defects around the knee joint and on the proximal third and middle third of the lower leg. It is a relatively easy and reliable procedure.
The knee area and upper third of the lower leg have an abundance of vessels and muscles. Thus, it appears possible that soft tissue defects in these sites may be treatable with a variety of reconstructive methods, but the outcomes of these methods may be unsatisfactory for several reasons. A local flap with muscles might yield unsatisfactory cosmetic and functional results, and both the perforator flap and free flap procedures are associated with technical difficulties (Rajacic et al. Citation1999, Shim and Kim Citation2006). The skin has less redundancy and a poor arterial supply below the proximal third of the lower leg, and superficial venous return in this area is frequently rendered ineffective. Hence, soft tissue defects that occur in this region are difficult to cover.
Since Hasegawa et al. (Citation1994) modified the neu‐rocutaneous flap procedure developed by Masquelet et al. (Citation1992), several articles have described the effectiveness and usefulness of a distally based superficial sural artery flap (Rajacic et al. Citation1996, Huisinga et al. Citation1998, Le Fourn et al. Citation2001). However, there have been few published clinical reports regarding proximally based sural artery flaps.
We evaluated the outcome of the proximally based sural artery flap for the reconstruction of soft tissue defects around the knee and on the proximal third and middle third of the lower leg.
Patients and methods
Between 1999 and 2006, 10 patients in our department (7 males) underwent reconstructions of soft tissue defects around the knee or on the proximal third or middle third of the lower leg with proxi‐mally based sural artery flaps. All patients were treated by the senior author (SJC). The mean age at the time of reconstruction was 43 (28-68) years. The mean flap size was 37 (20-60) cm2. The mean pedicle length was 16 (12-20) cm ().
Summary of patients
Surgical technique
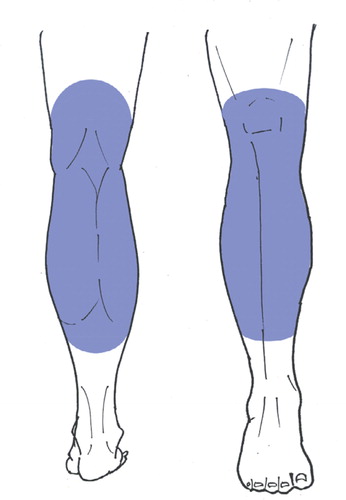
The patient was placed in the lateral decubitus position under general anesthesia, and a tourniquet was used during surgery. The flap was designed to be 1-2 cm larger in diameter than the defect in order to avoid tension at the suture site. Also, the flap had a tendency to shrink after being elevated. The donor site was centered on an imaginary line on the posterior calf, which indicated the course of the lesser saphenous vein and sural nerve (A). The length of the pedicle was determined while placing the pivot point of the pedicle on the popliteal fossa, where the superficial sural artery originates from the popliteal artery. After determination of the flap design and pedicle length, we simulated the elevation of the flap and the rotation of the pedicle with gauze to make certain that the pedicle was appropriate in length and was not entangled on rotation.
Figure 1. A. After estimating the size and shape of the recipient site, the pivot point and pedicle length were determined and the donor site was designed. The fasciocutaneous flap was to be centered on an imaginary line on the posterior calf, thereby indicating the course of the lesser saphenous vein (V) and sural nerve (N). B. At the midpoint of the lower leg, the sural nerve penetrates the deep fascia and courses between the two heads of the gastrocnemius muscle. The neurovascular structures may adhere to the surrounding tissues at this point, thereby necessitating careful dissection.
After the skin incision, the subcutaneous fascia was dissected at the distal margin of the designed flap, and the flap and pedicle were elevated. The sural nerve, superficial sural artery, and lesser saphenous vein were identified, and the flap and pedicle (which was about 2-3 cm in width) were constructed to include all three of them. The sural nerve and saphenous vein were then ligated at the distal end of the flap. At the midpoint of the lower leg, the sural nerve penetrates the deep fascia and follows a course between the two heads of the gastrocnemius muscle. The neurovascular structures may adhere to the surrounding tissues at this point, which requires a careful dissection (B). The pedicle was rotated at the pivot point. Unlike distally based sural artery flap, there is no decisive standard regarding the pivot point of proximally based sural artery flap. We decided that the pivot point should be located at least 2 cm distal to the popliteal crease if possible, so that the pedicle would not be entangled and not be tensioned. Then a subcutaneous tunnel was constructed to allow the flap and pedicle to pass to the recipient site. The tunnel was incised and covered with a split‐thickness skin graft if the pedicle was compressed through excessive tension under the tunnel. We recommend that the pedicle should be made slightly longer (by at least 1-2 cm) than is needed to avoid tension. After the flap was placed on the recipient site, the tourniquet was deflated and the circulation of the flap was checked. The incision used to elevate the flap and pedicle was then closed. The donor site was covered with a split‐thickness skin graft if it was difficult to close primarily, which often occurred when it was 5 cm or more in width. The closer to the ankle joint the donor site was, the more frequently it was covered by skin graft due to the reduced mobility of the surrounding soft tissue. When the flap was attached to the recipient site, the tourniquet was kept deflated and the flap was sutured with no tension. With this proximally based sural artery flap, we could cover small- to medium‐sized soft tissue defects of the lower leg around the knee joint and on the proximal and middle lower legs, except the defect occurred in the course of the pedicle, which accompanies the lesser saphenous vein and sural nerve ().
After the operation, we did not use any immo‐bilizer but avoided compression of the pivot point. We did not allow vigorous motion of the knee joint during the first week. The stitches were removed after 2 weeks.
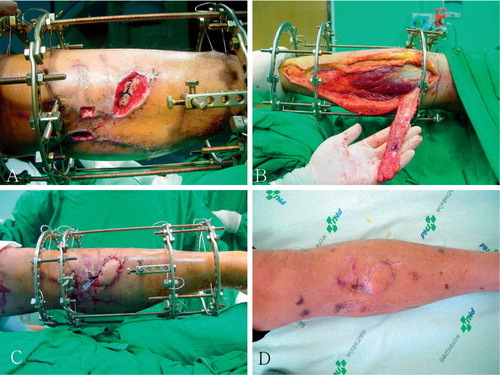
Case 4 ()
A 40-year‐old man had sustained open fractures of the right femur and tibia. A 5 cm x 8 cm soft tissue defect with scarring and fibrosis occurred because of necrosis and infection, and reconstruction was done using a proximally based sural artery flap. The flap was medially transposed to cover the defect. After division of the subcutaneous tunnel to reduce tension to the pedicle, a split‐thickness skin graft was performed on the short segment of the pedicle in the medial aspect of the knee, where the skin and subcutaneous tissue were scarred and fibrosed. Because the defect of the donor site was 6 cm in width and located near the ankle joint with less mobility of the surrounding tissue, the donor site was also covered with a split‐thickness skin graft. The defect healed without complications, and at the last follow‐up the patient was satisfied with this thin sensate flap.
Figure 3. A. A 40-year‐old man with a prepatellar area skin defect of the right leg as a result of open fractures of the femur and tibia. B. A proximally based superficial sural artery flap, which was 6 cm x 10 cm in size with a 20-cm pedicle length, was elevated. C. After dividing the subcutaneous tunnel in order to reduce tension to the pedicle, a split‐thickness skin graft was conducted on the short segment of the pedicle in the medial aspect of the knee, where the skin and subcutaneous tissue were scarred and fibrosed. D. The patient was satisfied with this thin sensate flap at the 30-month follow‐up examination.

Case 5 ()
A 37-year‐old man had sustained a comminuted open fracture of the left tibia. The fracture was fixated with an Ilizarov apparatus, and reconstruction for a 4 cm x 6 cm soft tissue defect was conducted with a proximally based sural artery flap. The flap was elevated from the posterior calf. The pivot point of the flap was located 5 cm distal to the popliteal fossa, where the surrounding soft tissue was scarred and fibrosed due to several previous operations including skin grafting. The flap was medially transposed under a subcutaneous tunnel without being divided to cover the defect. The defect healed without complications.
Figure 4. A: A 37-year‐old man sustained a skin defect and bone exposure in the anterior aspect of the left lower leg. Proximally based superficial sural artery flap was performed to cover this defect. B. The proximally based sural artery flap was 5 cm x 7 cm in size, and 18 cm in pedicle length. C. A photograph taken immediately after surgery. D. At the 1-year follow‐up examination, the flap had healed well.
Results
The mean surgical time for elevation of the flap was 35 (20-50) min, and no morbidity of the donor site and no functional deficits of the knee or ankle were detected in any of the cases. All 10 flaps survived, in 9 cases without any complications. In the remaining case with a fasciocutaneous flap, postoperative congestion was observed for several days and a tip necrosis occurred, but finally healed without complications. This case was the first in which reconstruction using a proximally based sural artery flap was conducted. We did not include the lesser saphenous vein in the pedicle. In another one of the fasciocutaneous flaps, a superficial necrosis occurred because of infection in the recipient site, but the wound healed after antibiotic therapy.
Marginal necrosis of the grafted skin occurred in 2 cases in which adipofascial flaps were used. One of them healed after the advancement of the adjacent soft tissue, and the other healed without any additional surgical management. The grafted skin on the donor site healed uneventfully in all cases except one, in which the grafted skin was partially necrosed. It healed eventually without any additional surgical treatment. We had to open the subcutaneous tunnel in 5 cases (cases 1, 3, 4, 6, and 8) in order that the pedicle would not be compressed. In all cases, the sensory loss of the dorsolateral aspect of the foot occurred, but no complaints were registered during the follow‐up period. Most of the patients were satisfied with these thin sensate flaps.
Discussion
As has been well reported in the literature, the distally based sural artery flap is reliable—with a high survival rate due to the relatively constant blood supply and ease of elevation, so that no microsurgical technique is required (Rajacic et al. Citation1996, Le Fourn et al. Citation2001). It requires no sacrifice of muscles and major arteries, and can be performed in a one‐stage operation. However, indication for this reconstruction treatment is limited to defects in the distal third of the tibia, around the ankle and foot (Touam et al. Citation2001, Akhtar and Hameed Citation2006). Regarding the proximally based sural artery flap, 4 cases were listed in the tables of a report (Meyer et al. Citation2002), but no details of the procedure or outcome were described. There have been few published clinical reports on proximally based sural artery flap. Our experience indicates that the outcome of the proximally based sural artery flap is similar to or superior to that of the distally based sural artery flap, and it is desirable that the lesser saphenous vein be included in the pedicle during elevation. A distally based sural artery flap survives with the blood supply from the anastomoses between the sural and peroneal arteries above the lateral malleolar area of the ankle, despite the proximal ligation of the sural artery. On the other hand, a proximally based sural artery flap—in which the proximal arterial supply is conserved—is more desirable from a physiological standpoint.
Soft tissue defects with infection after total knee arthroplasty or open fractures of the proximal tibia are not uncommon. The proximally based sural artery flap is a good choice for reconstruction of such defects. There is no morbidity of the donor site and minimal damage to the muscles, and the technique can provide excellent cosmetic results with a thin and sensate flap. The method also provides stretchable and sensate skin with a gliding undersurface, which does not restrict the excursion of the extensor apparatus. There is no need for microsurgical techniques, and an excellent survival rate can be expected provided there is constant blood supply. These flaps can cover not only the knee joint region and the proximal third of the lower leg, but also the middle third of the lower leg with sufficient pedicle length. The disadvantages of this flap include sensory disability in the dorsolateral aspect of foot, and scarring of the donor site can produce inferior cosmetic results. However, in our experience these problems are minor.
We used two types of flaps, the fascicutaneous flap and the adipofascial flap. Some of the fasciocutaneous flaps were congested for several days postoperatively. The first case did not include the lesser saphenous vein in the pedicle, and a trivial tip necrosis occurred in this patient. After this case, we included the lesser saphenous vein in the pedicle and no congestion or necrosis occurred.
For reconstruction as a treatment for defects on the middle third of the lower leg, the flap should be elevated from the posterior aspect of the superior portion of the ankle for sufficient pedicle length. Marginal necrosis of the grafted skin occurred in these two cases with adipofascial flaps, perhaps because of the prolonged pedicle length and the absence of cutaneous tissue.
Contributions of authors
SJC: senior author, preparation of the study, and surgical operation. IBK: writing of the manuscript. WRP: review of patient data and writing of the manuscript. HTK: preparation of the study.
No competing interests declared.
- Akhtar S, Hameed A. Versatility of the sural fasciocutane-ous flap in the coverage of lower third leg and hind foot defects. J Plast Reconstr Aesthet Surg 2006; 59(8)839–45
- Hasegawa M, Torii S, Katoh H, Esaki S. The distally based superficial sural artery flap. Plast Reconstr Surg 1994; 93(5)1012–20
- Huisinga R L, Houpt P, Dijkstra R, Storm van Leeuwen J B. The distally based sural artery flap. Ann Plast Surg 1998; 41(1)58–65
- Le B Fourn, Caye N, Pannier M. Distally based sural fas-ciomuscular flap: anatomic study and application for filling leg or foot defects. Plast Reconstr Surg 2001; 107(1)67–72
- Masquelet A C, Romana M C, Wolf G. Skin island flaps supplied by the vascular axis of the sensitive superficial nerves: anatomic study and clinical experience in the leg. Plast Reconstr Surg 1992; 89(6)1115–21
- Meyer C, Hartmann B, Horas U, Kilian O, Heiss C, Schnet-tler R. Reconstruction of the lower leg with the sural artery flap. Langenbecks Arch Surg 2002; 387(7-8)320–5
- Rajacic N, Darweesh M, Jayakrishnan K, Gang R K, Jojic S. The distally based superficial sural flap for reconstruction of the lower leg and foot. Br J Plast Surg 1996; 49(6)383–9
- Rajacic N, Gang R K, Darweesh M, Abdul F N, Kojic S. Reconstruction of soft tissue defects around the knee with the use of the lateral sural fasciocutaneous artery island flap. Eur J Plast Surg 1999; 22(1)12–6
- Shim J S, Kim H H. A novel reconstruction technique for the knee and upper one third of lower leg. J Plast Reconstr Aesthet Surg 2006; 59(9)929–34
- Touam C, Rostoucher P, Bhatia A, Oberlin C. Comparative study of two series of distally based fasciocutaneous flaps for coverage of the lower one-fourth of the leg, the ankle, and the foot. Plast Reconstr Surg 2001; 107(2)383–92