Abstract
Background and purpose Distal radius fractures are most often treated nonoperatively, but sometimes they are treated surgically when deemed unstable. Based on the literature, a consensus protocol for treatment has been developed in southern Sweden to aid clinicians in their decision making. We evaluated the results of this protocol prospectively using a validated outcome instrument (DASH) in a large consecutive and population based series of unselected patients.
Methods 581 patients were treated according the protocol. Age, sex, fracture side, and type of treatment were registered. The subjective outcome was measured by DASH. 133 patients were operated.
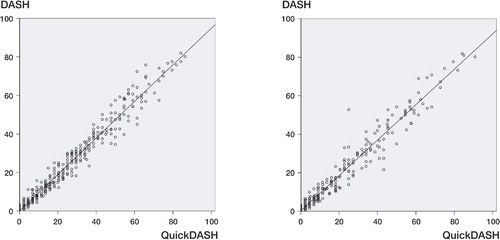
Results 75% of the patients returned the questionnaire. The median DASH score at 3 months was 18.3 and at 12 months it was 7.5. All treatment groups had low DASH scores at the final follow‐up. Reduced, nonoper ated fractures had a worse score (11.6) than undisplaced (4.2) or operated fractures (6.0). Age was the only other predictor, with older patients having a worse score. A correlation was found between the short‐version 11-item QuickDASH questionnaire and the full 30-item DASH, both at 3 months (r = 0.98) and at 1 year (r = 0.97) (p< 0.001 for both).
Interpretation Most patients have residual symptoms at 3 months after the fracture but are normalized at 1 year. Good final subjective result was achieved with the proposed protocol regardless of initial severity and treatment of the fracture, as indicated by a low median DASH score in all groups. There was correlation between QuickDASH and the full DASH, and the former could be used in future studies.
Distal radius fracture is the most common type of fracture, accounting for one‐sixth of all fractures at an emergency room (Lindau Citation2000). Several treatment options are available. Undisplaced fractures are casted and displaced fractures are reduced and casted. Unstable fractures are most often operated upon, especially if the fracture is impossible to reduce or to retain in a reduced position at the emergency ward, or when the fracture does not remain reduced at the follow‐up. Different types of operative fixation can be chosen and many authors have reported the results of various treatments for distal radius fractures.
A particular treatment protocol for the distal radius fracture has been used at Lund University Hospital since 1998. The type of treatment is standardized and depends upon the radiographic appearance, reducibility, and stability of the fracture as well as the age and demands of the patient (). The protocol was developed as a consensus document between the hospitals treating distal radius fractures in the southern Swedish region. Searching the literature, guidelines for treatment can be made for such a protocol, but (perhaps surprisingly) there is no robust evidence at present to suggest that any treatment method is superior to any other in the Cochrane metaanalysis reports, either for different types of conservative treatment (Handoll and Madhok Citation2003a) or for surgical treatment (Handoll and Madhok Citation2003b). The aim of the present study was therefore to collect prospective outcome data for the current treatment protocol in a distal radius frac ture cohort using a validated subjective outcome instrument.
Figure 1. Treatment protocol for distal radius fractures at Lund University Hospital and the hospitals in the southern Swedish region. The protocol gives guidelines, but the patient's demands and biological age are also considered when selecting treatment. a Displaced = dorsal angulation of > 10° and/or ulna plus of > 2 mm and/or articulation step of > 1 mm or volar angulation of > 25°
We monitored this distal radius fracture cohort for 2 years using the DASH instrument (Disabilities of the Arm, Shoulder and Hand,www.dash.iwh. on.ca), a site‐specific, validated outcome instrument for the upper extremities. In order to improve the treatment protocol, possible prognostic factors were registered for all fractures (such as age, sex, treatment method, and fracture side) and, for operated fractures, whether the type of operation or the time to surgery had an influence on the subjective patient outcome.
Patients and methods
Fracture treatment protocol
Undisplaced or minimally displaced fractures are treated in a short arm cast. The criteria for a displaced fracture are ulnar variance of more than 2 mm and/or intraarticular step of more than 1 mm, and/or dorsal angulation of more than 10° or a volar angulation of more than 25°. Displaced fractures () are treated with closed reduction under local anesthesia at the emergency ward, and a short arm splint. After 7-10 days, the patients are re‐examined and if the fracture has re‐dislocated radiographically, according to the criteria above, an operation with either external or internal fixation is proposed to the patient. The chronological and physiological age of the patient and his/her preferences and demands are considered in the decision to operate. The choice of external or internal fixation was not always based on the protocol. Due to the large number of patients, all fractures were not treated by a hand surgeon; hence, the operative method chosen sometimes reflected to some extent whether the patient was operated on by an orthopedic surgeon (n = 25) or a hand surgeon (n = 108). The latter may be more prone to open reduction, but at the same time takes care of more complex fractures. 5 of the 16 volar plates were done by an orthopedic surgeon. The remaining 54 open reductions were done by hand surgeons.
Figure 2. Drawing showing the cut‐off limits for radiographic malposition qualifying for surgery. A. Ulna plus: indication for operation is a distance of > 2 mm between the lines (normal value from -4 mm to +2 mm). B. Dorsal angulation: indication for operation is > 10° of dorsal tilt (normal value 10° (0-22) volar tilt as shown).
Patients with primary unstable fractures, impossible to either reduce or retain in an acceptable position according to the criteria described above, are operated. Out of 86 primary unstable fractures, 70 were operated by hand surgeons and of these, 21 were also included in a randomized study comparing external fixation to internal fixation. For 16 fractures, the decision to operate was made by the orthopedic surgeon on call who chose external fixation in every case. Finally, due to a high risk of secondary displacement, volarly dislocated fractures were operated with open reduction and a volar plate.
Surgical procedures
Extraarticular fractures are often treated with external fixation using a Hoffman type 1 bridging external fixator. Pins are inserted into the second meta carpal and into the radius proximal to the fracture. Clamps are attached to the pins and the fracture is reduced and fixated with a steel rod between the clamps (). Intraarticular comminuted and non‐comminuted fractures are treated with open reduction and internal fixation.
In the time period of the present study, we used the fragment‐specific wrist fixation system TriMed (Konrath and Bahler Citation2002, Schnall et al. Citation2006), which consists of a combination of pins and plates (). Commonly, 2 incisions are made through the first and fourth extensor compartment. The fracture is reduced and 2 pins are introduced at the tip of the radial styloid, obliquely and in a proximal direction exiting the radial cortex ulnarly and proximally. A stabilizing pin‐plate is threaded onto the styloid pins and the plate is secured to the radial side of the radius by 3-5 screws. Through the dorsal incision, a buttress pin and/or an ulnar pin‐plate is introduced for dorsal stability. In comminuted fractures with a bone defect, when additional stability is desired a bone graft substitute is used (Norian SRS) or occasionally bone graft from the iliac crest. Volar fractures are operated using a volar non‐locking plate (Keating et al. Citation1994) and the operation is performed with a volar modified Henry approach.
Patients
Over 2 years, all patients over the age of 18 with a distal radius fracture, presenting at the emergency department of Lund University Hospital, were registered prospectively in a database. The registration was approved by the institutional review board. Medical records and the radiographic charts were scrutinized weekly for radius fracture and its ICD code. 581 patients with 584 fractures were identified and given or sent a DASH questionnaire to fill out. During the first week after injury, patients were asked to report any pre‐fracture impairment. The DASH questionnaire was distributed again at 3 and 12 months after the fracture.
63 patients (47 women) were excluded from the original 581 patients. 11 patients died during the follow‐up time, 7 patients could not speak Swedish and could not fill out the questionnaire. 38 patients suffered from senile dementia. 7 other patients were excluded due to other simultaneous arm injuries. The excluded patients were older (72 (18-97) years, p < 0.001) but there was no significant difference regarding their sex, fracture side, or type of treatment. The remaining 518 patients had a mean age of 60 (19-93) years. 398 were female with a mean age of 63 (19-93) years, and 120 were male, with mean age 50 (19-92) years. 206 had fractured their right wrist, 309 their left, and 3 had bilateral fractures.
Patient groups
The 518 patients were divided into 3 groups according to their treatment. 220 patients had undisplaced fractures and were casted without reduction. 212 patients had fractures that were reduced. Both groups were treated in a short arm cast for 4-5 weeks. 86 of the patients had fractures that required an operation because they were either complex fractures that were impossible to reduce or volar Barton fractures.
In the group with reduced fractures, 47 of the 212 fractures showed a dislocation at the follow up appointment and were operated. The operations performed in these 133 patients were divided into 4 groups: external fixation (63 patients), internal fixation with the TriMed system (51 patients), internal fixation with volar plating (16 patients), and other procedures (3 patients: 1 screw fixation, and 2 with combined internal and external fixation) (). As in previous studies, we arbitrarily defined men less than 60 years of age and women below the age of 50 to constitute a non‐osteoporotic age group, as opposed to the older osteoporotic age group (Kopylov et al. Citation1993, Lindau et al. Citation1999)
DASH questionnaire
DASH is a self‐administered questionnaire that was developed by the AAOS and the Institute for Work and Health in Canada (Hudak et al. Citation1996). A Swedish version has been validated for use in upper extremity disorders but not specifically for distal radius fractures (Atroshi et al. Citation2000). The questionnaire consists of 30 questions evaluating different aspects of physical activity, severity of symptoms, and the effect of the injury on social activities. A score is calculated and the disability of the patient is estimated on a scale from 0 to 100, with 100 being the worst result. A minimum of 27 questions must be answered for the result to be valid and in order to calculate the DASH score. During the time of our study a shorter form, QuickDASH, consisting of 11 questions from the original DASH was developed and validated (Gummesson et al. Citation2006). We correlated the 30-item original DASH used in this study to the 11 identical questions in the short form QuickDASH.
The DASH form was given or sent to the patients directly after injury, and 3 and 12 months after injury. A reminder (with a new form) was sent after 2 weeks to patients who did not answer the first time. If more than 3 but less than 6 questions were left unanswered, the patients were asked to complete the form so that a score could be calculated. The patients mainly received the questionnaires by surface mail with written instructions, and only hospitalized patients were given the questionnaire personally.
Reference group
Although the patients were instructed to report any pre‐fracture impairment, it became clear early on in the study that replies from the first enquiry, asking for pre‐fracture symptoms, proved inconsistent. A small number of patients reported their pre‐fracture status as instructed but the majority instead reported their symptoms on the first week after the fracture. To be able to present baseline data, the questionnaire was sent to an age- and sex‐matched control group of 109 individuals taken from the Swedish National Population Registry. These reference controls came from the same catchment area and were born on the same day and were of the same sex as a randomly selected fraction of the radius fracture cohort (). In an accompanying letter, we asked these people to fill in the DASH form and also to state whether they had had a previous wrist fracture. 75 of the 109 (69%) indviduals responded.
Table 1. Baseline data for responders and non‐responders to the questionnaire and for the control group
Statistics
DASH data are ordinal; they showed a skewed distribution and therefore non‐parametric analyses were used, and the data were presented as median with interquartile range. Mean and standard deviation are included in the tables to enable comparison with previously published studies. A linear mixed effects model was used for multivariate analysis. Age, side of fracture, type of treatment, operation due to primary or secondary instability, and whether the patient was operated by a hand surgeon or an orthopedic surgeon were used as fixed effects and with random effect for each patient. For group comparisons, Mann‐Whitney tests were used. Correlation (Spearman) was determined between DASH and age at 3 and 12 months after the injury, and also between standard DASH forms and the shorter QuickDASH. Effect size was calculated and defined as mean change in score divided by the standard deviation of the first score. Effect sizes of 0.2 were considered small, 0.5 moderate, and > 0.8 large (Roos et al. Citation1998). The statistical analyses were performed with SPSS 14.0 for Windows. For calculation of power, we used PS power and sample size calculations (http://biostat. mc. vanderbilt.edu/twiki/bin/view/Main/PowerSampleSize).
Results
The 3-month questionnaire was completed by 389 (75%) patients and the 12-month questionnaire by 389 (75%) patients of the 518 initially recorded. 7% and 6% had more than 3 unanswered questions at 7 and 12 months, respectively. Thus, their questionnaires could not be used for analysis and 357 and 360 forms, respectively, were used for analysis. Elderly patients (osteoporotic men over 60 years of age and osteoporotic women over 50 years) more often filled out the form incorrectly (8%) than the younger group (1%). At 3 months, there was no statistically significant difference between the non‐responders and patients with invalidated forms (i.e. more than 3 questions unanswered) regarding age, sex, injured side, type of treatment, or type of operation. At 12 months, the patients who responded and had valid forms were younger than the non‐respondents (mean age 58 and 61 years, respectively). Also, the proportion of responders with fractures requiring an operation was lower.
A multivariate analysis revealed a worse DASH score for fractures that were reduced but not operated (p = 0.003), a worse DASH score with increasing age (p < 0.001), and a better DASH score at 12 months than at 3 months (p < 0.001).
The median DASH score for the whole group was 18 at 3 months and 7.5 at 12 months (p < 0.001). In the older osteoporotic age group, DASH scores were 23 and 9.2, respectively, (p < 0.001) and in the younger age group they were 12 and 5.0 (p < 0.001). There was a correlation between age and DASH at 3 months (r = 0.33, p = 0.01) and at 12 months (r = 0.28, p = 0.01). There was no statistically significant difference in DASH scores between fractures of the left and the right wrist. Women scored worse than men at 3 months (), but they were older (mean age 63) than the male group (mean age 52).
Table 2. DASH and QuickDASH data at 3 and 12 months (scale 0-100, with higher value meaning worse)
133 patients with 135 fractures were operated. 87 patients in the operated group returned the form at 3 months and 103 answered at 12 months. At 3 months, the median DASH score was 17 in the unoperated group: 14 for external fixation, 15 for volar plate, and 16 for the Tri‐Med group. At 12 months the scores were 5.8 for the unoperated group, 7.0 for external fixation, 4.3 for volar plate, and 7.0 for the Tri‐Med group (). Patients with primarily stable fractures treated with a cast had a median score of 17 at 3 months and 4.2 at 12 months. Patients with reduced fractures treated with closed reduction and casting had scores of 22 and 12, respectively, and the group of patients with operation as the primary treatment had scores of 15 and 5.5 at 3 and 12 months (). A correlation between DASH and Quick DASH was found both at 3 months (r = 0.984, p < 0.001) and at 1 year after injury (r = 0.974, p < 0.001)().
Table 3. DASH scores at 3 and 12 months (scale 0-100, with higher values meaning worse)
Figure 6. DASH scores for unoperated patients compared to scores for operated patients. A. Unoperated. B. Operated with external fixation. C. Operated with the TriMed system. D. Volar fractures operated with a volar plate. The box plot on the left shows the results at 3 months and that on the right at 12 months.
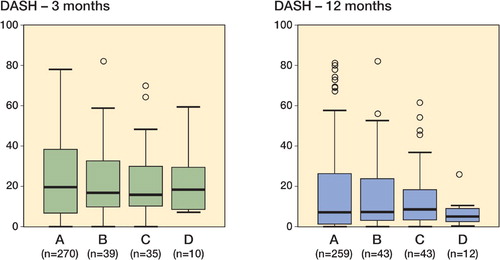
Figure 7. Correlation between the full 30-item DASH score (y‐axis) and the 11-item Quick DASH (x‐axis), at 3 months (left panel) (Spearman correlation 0.98, p < 0.001) and at 1 year (right panel) (Spearman correlation 0.97, p < 0.001).
Reference group
The median DASH score for the age- and sex‐matched reference group was 2.5 (0-9.2) for the whole group and 0.8 and 3.7, respectively, when considered as younger and older age groups. There was a significant difference between the DASH score of the control group and of patients with a distal radius fracture even after 12 months (p < 0.001), both for the whole group and when they were divided into groups of younger and older individuals ().
Table 4. DASH data at 12 months divided into age and gender groups and compared to the reference group
Discussion
In general, patients suffering from a distal radius fracture, regardless of type of treatment, end up with some degree of discomfort and loss of function in the first year. During the first 2 months after injury, the patients have severe problems with many daily activities but after 1 year these problems are minimal in the majority of cases (MacDermid et al. Citation2003). The other patients have residual symptoms after 1 year, and although the percentage of these patients may be small, the high incidence of distal radius fracture makes this group large. In our study, DASH scores showed a similar decreasing pattern in the time period between 3 and 12 months. The DASH score was higher in the fracture patients after 1 year (median 7.5, mean 17) than in the uninjured control group (median 2.5, mean 8.3). The protocol, with all the weaknesses of a non‐randomized design, appears to be adequate as it brings all fractures to a similar and good end‐result, but with a slightly poorer result for displaced and reduced fractures compared to the stable unreduced fractures. The reason for this might be a tendency not to operate re‐displaced fractures on elderly patients for whom demands are low. The mean and median DASH scores at 1 year were still low in all groups.
In this study, equal DASH scores were found in operated vs. non‐operated fractures, as well as, for internal vs. external fixation. Resuls are comparable to one other study using DASH comparing internal and external fixation (Westphal et al. Citation2005). However, DASH was primarily intended for evaluation of the effect of some kind of intervention—such as a surgical procedure with a considerable impact—and not to follow a cohort over time or to distinguish between 2 treatments. It has been used in case series for the TriMed system and the mean DASH score was reported to be 17 at 29 months (Konrath and Bahler Citation2002). Using the Pi‐plate, the median score at 2 years was 7.8 (Krukhaug and Hove Citation2004) and the mean was 14.5 (Rozental et al. Citation2003). However, when comparing the outcome of 2 reasonably good methods, we fear that DASH has limited sensitivity to changes, as suspected from the intermediate degree of responsiveness in our study, and less obvious differences might remain undetected. The responsiveness has been evaluated in upper extremity disorders in general and in distal radius fractures in particular; in the latter, DASH was shown to be sensitive with regard to changes from the time of injury to 6 months after injury with a high effect size of 2.3 (MacDermid et al. Citation2000).
In our study, the patients did not fully understand how to fill in the baseline protocol. Some patients reported pre‐fracture data and others post‐fracture data, which made the baseline data useless. When we instead used our normal material as baseline data, there was a large effect size of 1.12 for the 3-month results and a moderate effect size of 0.54 for the 12-month results. Perhaps a more sensitive tool would be necessary in order to evaluate a change over time, such as improvement between 3 and 12 months, without a drastic event such as an operation or fracture. In this study, a statistically significant subjective improvement occurred between 3 and 12 months, as expected, but the calculated effect size was a moderate 0.37. Using an outcome instrument with the sensitivity of DASH, even in a rather large group study such as ours (with more than 100 operated patients) it was not possible to determine the effect of the operation technique or to differentiate a primary operation from a secondary one. To our knowledge, no randomized published study has been capable of showing a difference in the outcome between 2 surgical methods using DASH. If one intends to design a randomized study out of the outcome data in this study with 85% power at p = 0.05, 66 patients must be included in each group to show a difference in DASH score of 10 scale steps, which is considered to be the minimal important change (Gummesson et al. Citation2003). Instead of including a large number of patients, it would be preferable to use an outcome instrument that is more sensitive to smaller changes or smaller differences between treatment modalities. Perhaps a more sensitive outcome instrument should be designed before conducting randomized trials to compare different treatments including, for example, different surgical methods.
In general, DASH as a universal follow‐up instrument required substantial administrative work to ensure an acceptable frequency of replies. Many patients did not fill in all the questions, as they did not feel that some of the questions were relevant to their situation. If 3 or more questions were unanswered, the reply was not considered valid and had to be disregarded. In a cohort consisting of mainly elderly patients, age did play a part in the frequency of invalid replies. In the group over 60 years of age, 8% sent in invalid forms as compared to 1% in the younger age group. Many of the elderly patients were mentally unfit, and relatives or nursing home staff reported that the respondent was unable to fill in the form. A reply frequency of 75% must be regarded as adequate in a cohort like this, but it could probably be improved by using a simpler outcome instrument. The short form of DASH, QuickDASH, contains only 11 questions. It may improve the response rate () and could be used instead of the full DASH.
In conclusion, it seems that the patients still have residual symptoms at 3 months but most of them have returned to the baseline by 1 year. Our treatment protocol means that similar, good subjective end‐results are achieved regardless of the initial severity of the fracture. However, patients with unstable fractures, initially reduced and treated with a cast but later operated on, tended to have poorer scores. This subgroup requires further investigation.
Contributions of authors
AA: setting up of project, planning, data collection, interpretation of data, statistics, and writing of the manuscript. MT: setting up of project, planning, statistics, interpretation of data, and writing of the manuscript. PK: setting up of project, planning, and writing of the manuscript.
The authors wish to thank Ewa Persson for excellent secretarial assistance and statistician Fredrik Nilsson, Competence Center for Clinical Research, Region Skåne (RSKC), for statistical advice. The project was supported by Region Skåne, Lund University Hospital, the Swedish Medical Research Council (project 09509), the Alfred Österlund Foundation, the Greta and Johan Kock Foundation, the Maggie Stephens Foundation, the Foundation for Support of Functionally Hindered Patients in Skåne, and the Faculty of Medicine, Lund University.
- Atroshi I, Gummesson C, Andersson B, Dahlgren E, Johansson A. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: reliability and validity of the Swedish version evaluated in 176 patients. Acta Orthop Scand 2000; 71(6)613–8
- Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord 2003; 4(1)11
- Gummesson C, Ward M M, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord 2006; 7: 44
- Handoll H H, Madhok R. Conservative interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev 2003a; 2, CD000314
- Handoll H H, Madhok R. Surgical interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev 2003b; 3, CD003209
- Hudak P L, Amadio P C, Bombardier C. Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 1996; 29(6)602–8
- Keating J F, Court-Brown C M, McQueen M M. Internal fixation of volar-displaced distal radial fractures. J Bone Joint Surg (Br) 1994; 76(3)401–5
- Konrath G A, Bahler S. Open reduction and internal fixation of unstable distal radius fractures: results using the trimed fixation system. J Orthop Trauma 2002; 16(8)578–85
- Kopylov P, Johnell O, Redlund-Johnell I, Bengner U. Fractures of the distal end of the radius in young adults: a 30-year follow-up. J Hand Surg (Br) 1993; 18(1)45–9
- Krukhaug Y, Hove L M. Experience with the AO Pi-plate for displaced intra-articular fractures of the distal radius. Scand J Plast Reconstr Surg Hand Surg 2004; 38(5)293–6
- Lindau T. Distal radial fractures and effects of associated ligament injuries. Lund University Thesis. 2000
- Lindau T, Aspenberg P, Arner M, Redlundh-Johnell Hag I, berg L. Fractures of the distal forearm in young adults. An epidemiologic description of 341 patients. Acta Orthop Scand 1999; 70(2)124–8
- MacDermid J C, Richards R S, Donner A, Bellamy N, Roth J H. Responsiveness of the short form-36, disability of the arm, shoulder, and hand questionnaire, patient-rated wrist evaluation, and physical impairment measurements in evaluating recovery after a distal radius fracture. J Hand Surg (Am) 2000; 25(2)330–40
- MacDermid J C, Roth J H, Richards R S. Pain and disability reported in the year following a distal radius fracture: a cohort study. BMC Musculoskelet Disord 2003; 4(1)24
- Roos E M, Roos H P, Lohmander L S, Ekdahl C, Beynnon B D. Knee Injury and Osteoarthritis Outcome Score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998; 28(2)88–96
- Rozental T D, Beredjiklian P K, Bozentka D J. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius. J Bone Joint Surg (Am) 2003; 85(10)1956–60
- Schnall S B, Kim B J, Abramo A, Kopylov P. Fixation of distal radius fractures using a fragment-specific system. Clin Orthop 2006; 445: 51–7
- Westphal T, Piatek S, Schubert S, Winckler S. Outcome after surgery of distal radius fractures: no differences between external fixation and ORIF. Arch Orthop Trauma Surg 2005; 125(8)507–14