Abstract
Background Primary arthroplasty and internal fixation are the two main options for treatment of displaced femoral neck fractures. Despite the fact that there have been several randomized studies, the optimal treatment in the elderly is still controversial. In the present study, based on data from the Norwegian Hip Fracture Register, we compared satisfaction, pain, and quality of life 4 months after surgery in patients over 70 years of age with a displaced femoral neck fracture operated with internal fixation or with a bipolar hemiarthroplasty.
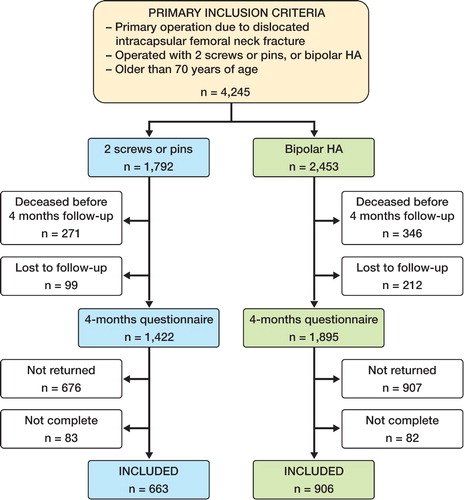
Patients and methods Data on 1,569 fractures in patients over 70 years of age operated with internal fixation (n = 663) or hemiarthroplasty (n = 906) were registered in the hip fracture register. The register also included data on patient satisfaction, pain, and quality of life (EQ-5D) assessed 4 months after surgery using VAS scales and EQ-5D health questionnaires.
Results Patients operated with hemiarthroplasty had less pain (VAS 27 vs. 41), were more satisfied with the result of the operation (VAS 33 vs. 48), and had better EQ-5D index score 4 months postoperatively (0.51 vs. 0.42) than patients who were operated with internal fixation.
Interpretation Our findings suggest that elderly patients with displaced femoral neck fracture should be treated with arthroplasty.
Every year in Norway, approximately 9,000 patients are hospitalized and operated on due to hip fractures (Directorate for Health and Social Affairs, Citation2005). Femoral neck fractures constitute 53–60% of the hip fractures and two-thirds of these fractures are displaced (Rogmark et al. Citation2002, Thorngren et al. Citation2002, Gjertsen et al. Citation2008). While most authors advocate osteosynthesis for younger patients and for those with undisplaced fractures, there is still controversy as to how to treat displaced femoral neck fractures in elderly patients (Chua et al. Citation1997, Bhandari et al. Citation2005, Iorio et al. Citation2006). There seems, however, to be a growing opinion that treatment should be based on the patient’s age, functional demands, and individual risk profile (Tidermark Citation2003, Blomfeldt et al. Citation2005a, Rogmark and Johnell Citation2005).
Primary arthroplasty and internal fixation (IF) with nails or screws are the two main options for treatment of displaced femoral neck fractures. In recent randomized, controlled trials total hip arthroplasties (THAs) have been shown to provide superior functional outcome to IF—as assessed by Harris hip score (Johansson et al. Citation2000) and EQ-5D (Tidermark et al. Citation2003a, Blomfeldt et al. Citation2005a, Keating et al. Citation2006).
Another study found that hemiarthroplasty (HA) provided a superior outcome than IF as treatment for displaced fractures in the elderly (Rogmark et al. Citation2002). In elderly patients with severe cognitive impairment randomized, controlled studies showed poor results for HA when compared to IF as treatment for displaced femoral neck fractures (Ravikumar and Marsh Citation2000, Blomfeldt et al. Citation2005b). A Cochrane review comparing IF and arthroplasty found no definite differences in pain and residual disability (Parker and Gurusamy Citation2006). A hip fracture is associated with increased mortality; half of the patients may die within 5 years (Ohman et al. Citation1969, Jensen and Tondevold Citation1979). It is therefore important to achieve a good outcome as soon as possible. Thus, we believe that evaluation of different treatment modalities during the first postoperative months is important. We compared IF and bipolar HA as treatment for dislocated femoral neck fractures in patients over 70 years of age using patient satisfaction, pain, and quality of life 4 months after surgery as outcome.
Patients and methods
The Norwegian Hip Fracture Register (NHFR) started registration of hip fractures in January 2005 (Gjertsen et al. Citation2008), and the aim of this national prospective study is to improve the quality of care. National recommendations on treating dislocated femoral neck fractures with prostheses exist in Norway (Directorate for Health and Social Affairs, Citation2005); however, the decision on whether to use screws/pins or HA is based on the preference of individual hospitals.
From January 2005 through December 2006, 13,104 proximal femur fractures were registered in the NHFR. Of these, 5,224 patients were registered as having a primary operation due to a dislocated femoral neck fracture. Our primary inclusion criteria were patients over 70 years old who were operated due to a dislocated femoral neck fracture (Garden III and IV) with 2 screws/pins or a bipolar HA. 4,245 patients fulfilled these criteria (). Patients who died during the first 4 postoperative months were excluded. We also excluded patients who emigrated during this period, and patients with an unknown address (). The remaining 3,317 patients received a questionnaire from the registry 4 months after surgery. No reminders were sent to patients who did not answer the questionnaire. 1,583 patients who did not return the questionnaire, and 165 patients whose questionnaire was not filled in a satisfactory way were excluded from further analysis. These two groups of patients were older (mean age 82, SD 6.2), had higher ASA scores (American Society of Anaesthesiologists, Citation1963), and were more often cognitively impaired (32%) than the patients who returned the questionnaire. The differences were statistically significant for all three variables (p < 0.001). Finally, 1,569 fractures operated with IF (n = 663) and HA (n = 906) remained for further analyses.
Patient and operative data were obtained from a form filled in by the surgeon immediately after the operation. To determine the presence of cognitive impairment, the surgeons, if in doubt, used the clock-drawing test (Shulman Citation2000). Both primary operations and reoperations were registered at all 55 hospitals performing hip fracture surgery in Norway (Gjertsen et al. Citation2008).
Any reoperations were linked to the primary operations using the patient’s national social security number. The definition of a reoperation was any operation performed due to complications after the primary operation, including removal of osteosynthesis material, closed reduction of dislocated hemiprostheses, revision to an HA or a THA, and soft tissue revisions.
The 4-months questionnaire included the Norwegian translation of the EuroQol (EQ-5D) (Brooks, Citation1996). An EQ-5D index score of 1 indicated the best possible health state and a score of 0 indicated a health state similar to death. Some health states were given a negative score, which indicated a health state worse than death. The patients were also asked to assess their preoperative EQ-5D.
Furthermore, the patients were asked to fill in a visual analog scale (VAS) concerning average pain from the operated hip during the previous month. A value of 0 indicated no pain and a value of 100 represented unbearable pain. The patients also filled in a VAS to describe how satisfied they were with the result of the operation. The value 0 represented very satisfied while the value 100 represented very dissatisfied. Finally, we used the Charnley classification for functional assessment (Charnley Citation1979).
In the analysis, all patients included in the study remained in the same group (IF or HA) according to the intention-to-treat principle, whether or not a reoperation was performed. 65 of the patients in the IF group had already been reoperated with an HA at the time of the 4-month evaluation. Since the reoperated patients could not be expected to demonstrate good clinical outcome (pain, satisfaction, and quality of life) in a very short time after reoperation, we also performed additional analyses without the reoperated patients in both treatment groups. Separate analyses for patients with cognitive impairment, and for patients in different age groups (70–79 years, 80–89 years, and 90–99 years), were also done. We also performed subanalyses on patients in Charnley class A, i.e. patients with involvement of the ipsilateral hip only and no involvement of other joints or systemic problems limiting activity.
Records with information on dates of death and emigration were obtained from the Norwegian Register of Vital Statistics. The Norwegian Data Inspectorate approved the recording of data, and all patients signed an informed consent form.
Statistics
The Pearson chi-square test was used for comparison of categorical variables in independent groups. The independent samples t-test (Student’s t-test) was used for parametric scale variables in independent groups. All tests were two-sided. The p-values in were adjusted for potential confounders (age, sex, cognitive impairment, ASA-class, and preoperative delay of surgery) with general linear models (GLMs). In the figures, mean values with standard error of the mean are presented. All results were considered statistically significant at the 5% level. The analyses were performed using SPSS software version 13.0.
Results
Patients operated with an HA were older, were more often female, and had a higher preoperative delay compared to patients operated with IF. There were no statistically significant differences in the preoperative ASA score, cognitive impairment, and EQ-5D index score ().
Table 1. Baseline characteristics of patients
In the HA group, uncemented prostheses accounted for 22% of the total. Only contemporary uncemented implants were used. No Austin Moore or Thompson prostheses were reported (). After 4 months, 110 patients had been reoperated, 92 in the IF group and 18 in the HA group.
Table 2. Types of implants
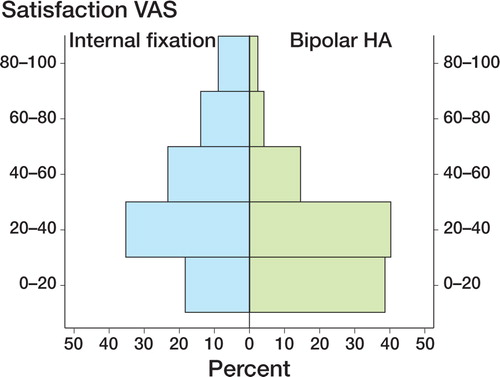
Patients in the IF group had more pain than patients in the HA group 4 months after surgery (p < 0.001). More patients in the HA group were satisfied with the result of the operation than those in the IF group (p < 0.001) (). Even after reoperated patients had been excluded, patients in the IF group had more pain and were less satisfied 4 months after surgery than patients in the HA group (p < 0.001) ().
Table 3. Pain and satisfaction with the result of the operation, derived 4 months postoperatively from visual analog scales (VAS)
Most of the patients with unbearable pain were found in the IF group and most patients with minimal pain were found in the HA group (). Most of the satisfied patients were found in the HA group while most of the dissatisfied patients were found in the IF group ().
Figure 2. The degree of pain derived from a visual analog scale (VAS) 4 months postoperatively. The figure shows the distribution of pain for the 2 different treatment groups. 0 indicates no pain and 100 indicates unbearable pain.
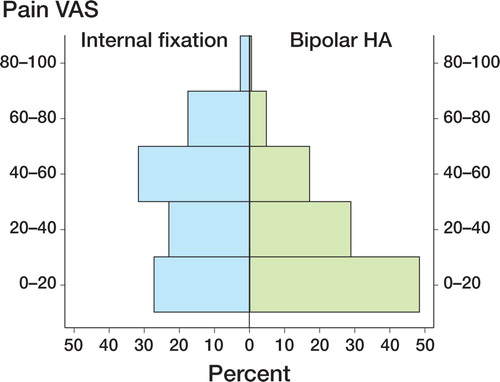
Figure 3. The degree of satisfaction with the result of the operation, derived from a visual analog scale (VAS) 4 months postoperatively. The figure shows the distribution of patient satisfaction for the 2 different treatment groups. 0 indicates very satisfied and 100 indicates very dissatisfied.
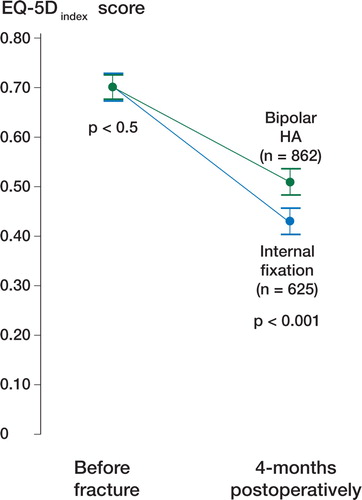
Only 625 IF patients and 862 HA patients had filled in both the preoperative EQ-5D and the 4- month EQ-5D questionnaire correctly. The preoperative EQ-5D index scores were equal in the IF and the HA groups: 0.68 and 0.69, respectively (). 4 months postoperatively, an inferior EQ-5D index score was found for the IF group (0.42) compared to the HA group (0.51) (p < 0.001). The decline in EQ-5D index score was 0.26 for the IF group and 0.19 for the HA group (p < 0.001) (). When separate analyses were performed excluding all reoperated patients in both treatment groups, the EQ-5D index score was 0.43 for the IF group (n = 488) and 0.51 for the HA group (n = 843) (p < 0.001).
Figure 4. Health-related quality of life (EQ-5D index score) for patients at 0 and 4 months. 0 indicates the worst possible health state and 1.0 indicates full health. The p-values are given for differences between the treatment groups (general linear model).
Preoperatively, no differences between the two groups in any of the 5 dimensions of the EQ-5D could be detected (). 4 months after surgery, the HA group was more mobile than the IF group (p < 0.001). Moreover, they had less problems with self-care (p = 0.001) and in performing their usual activities (p < 0.001) than the IF group. Finally, the HA group had less pain or discomfort than the patients operated with IF (p < 0.001) (). No difference in anxiety/depression was found between the two groups.
Table 4. Quality of life (EQ-5D) for patients operated with internal fixation or bipolar hemiarthroplasty
Separate analyses on patients suffering from dementia, patients in different age groups, and patients who had been walking without problems prior to the fracture showed practically the same differences regarding pain, satisfaction, and EQ-5D index score. Also, separate analyses on patients in Charnley class A showed similar differences regarding these outcomes. Finally, there were no statistically significant differences in pain, satisfaction, and EQ-5D index score between uncemented and cemented hemiprostheses.
Discussion
We found that patients operated with a bipolar hemiarthroplasty due to a dislocated femoral neck fracture had less pain, were more satisfied with the result of the operation, and had a better quality of life 4 months postoperatively than patients operated with internal fixation.
Quality of life
We found a marked reduction in EQ-5D index score postoperatively in both treatment groups. The patients treated with a bipolar HA did, however, have a better EQ-5D index score at 4 months than the IF group. Tidermark et al. (Citation2003b) found a reduction in EQ-5D index scores at 4, 12, and 24 months in patients with displaced femoral neck fractures treated with IF, even when the fracture had healed uneventfully. In elderly patients with severe cognitive impairment, Blomfeldt et al. (Citation2005b) found a lower quality of life for uncemented HA according to the EQ-5D at 2-year follow-up compared to IF. We found that HA was also superior to IF for the patients with cognitive impairment. One reason for this difference in results between studies could be that different implants were used. While Blomfeldt et al. used the unipolar Austin Moore uncoated uncemented hemiprosthesis—which is documented to be inferior (Australian Orthopaedic Association Citation2007)— most of the prostheses used in our study were cemented, and the uncemented prostheses used were all modern, hydroxyapatite-coated implants. The results of cemented HAs have been reported to be better than the results of uncemented, uncoated HAs concerning pain, walking ability, use of walk aids, and ADL (Khan et al. Citation2002). Keating et al. (Citation2006) found that there were no statistically significant differences between IF and bipolar HA when the EQ-5D was used 4, 12, and 24 months postoperatively. Our study had more patients, however, and therefore higher power.
We found a good correlation between the EQ-5D index scores and the other outcome variables at 4 months; i.e. patients reported similar pain and satisfaction scores. This is in accordance with an earlier study that showed a good agreement between the EQ-5D index scores and other outcome variables such as pain, mobility, independence in ADL, and independent living status (Tidermark et al. Citation2002).
Pain
Patients treated with an IF had more pain 4 months after surgery than patients treated with a primary HA (VAS scores: 41 and 27, respectively). This is in accordance with one study from Sweden (Rogmark et al. Citation2002). Other studies have, however, reported no statistically significant difference in pain between IF and HA (Parker and Pryor Citation2000, Keating et al. Citation2006). In the study by Parker and Pryor, uncemented, uncoated Austin Moore hemiprostheses were used.
Strengths and limitations of the study
Results from observational, register-based studies (cohort studies) are less conclusive than those from randomized clinical trials. If potential confounders are controlled for, however, observational studies may give results that are similar to those of controlled, randomized trials (Benson and Hartz Citation2000). Only known and measured confounders can, of course, be adjusted for in observational studies, whereas randomized studies take account of all confounders—both known and unknown. On the other hand, observational studies have several advantages over controlled, randomized studies, including lower cost, greater timeliness, and a wider range of patients. Our study represents the results from the whole country, and of the average surgeon, and not only the results from one specialized clinic, as in many randomized studies. Considering the high age and considerable comorbidity of the patients, the 60% response to the patient questionnaire was as expected, but a higher compliance would have strengthened our results. The patients who did not return the questionnaire were generally older, more cognitively impaired, and had a higher ASA class than the patients who responded. Since we had no EQ-5D scores for the patients who failed to respond, we can of course not be sure of any differences in quality of life in the two groups. However, preoperative age, cognitive impairment, and ASA class were similar for the non-responders in the 2 treatment groups. Consequently, the comparison of the treatment groups was reliable. The relatively high number of patients lost to follow-up may also reflect the fact that many of these frail patients are transferred to nursing homes when discharged from hospital; thus, they cannot be contacted at their permanent address.
In summary, 4 months after surgery, a bipolar hemiarthroplasty showed good results—better than those after screw or pin fixation—in dislocated femoral neck fractures in patients over 70 years of age. A longer follow-up will be necessary to determine whether the superior outcomes of hemiarthroplasty persist in the long term.
Acknowledgement
The authors thank all the Norwegian orthopedic surgeons who have loyally reported to the register. The Norwegian Hip Fracture Register is funded by the Regional Health Board of Helse-Vest RHF.
No competing interests declared.
Contributions of authors
This study represents close teamwork by the orthopedic surgeons JEG, TV, LBE, LIH, OF, and JMF, and statistician SAL. All authors participated in the interpretation of the results and in preparation of the manuscript. JEG, SAL, and JMF performed the statistical analyses. JEG was mainly responsible for writing the manuscript.
- American Society of Anaesthesiologists. New classification of physical status. Anaesthesiology 1963; 111
- Australian Orthopaedic Association, National Joint Replacement Registry. Annual Report 2007. Http://www.dmac.adelaide.edu.au/aoanjrr/aoanjrr.jsp
- Benson K, Hartz A J. A comparison of observational studies and randomized, controlled trials. N Engl J Med 2000; 342: 1878–86
- Bhandari M, Devereaux P J, Tornetta P, III, Swiontkowski M F, Berry D J, Haidukewych G, Schemitsch E H, Hanson B P, Koval K, Dirschl D, Leece P, Keel M, Petrisor B, Heetveld M, Guyatt G H. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg (Am) 2005; 87: 2122–30
- Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Comparison of internal fixation with total hip replacement for displaced femoral neck fractures. Randomized, controlled trial performed at four years. J Bone Joint Surg (Am) 2005a; 87: 1680–8
- Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg (Br) 2005b; 87: 523–529
- Brooks R. EuroQol: the current state of play. Health Policy 1996; 37: 53–72
- Charnley J. Low friction arthroplasty of the hip. Springer Verlag, Berlin 1979
- Chua D, Jaglal S B, Schatzker J. An orthopedic surgeon survey on the treatment of displaced femoral neck fracture: opposing views. Can J Surg 1997; 40: 271–7
- Directorate for Health and Social Affairs. Faglige retningslinjer for forebygging og behandling av osteoporose og osteoporotiske brudd, Oslo, 2005
- Gjertsen J-E, Vinje T, Furnes O, Engesaeter L B, Havelin L I, Steindal K, Fevang J. The Norwegian Hip Fracture Registe. Experiences after the first 2 years and 14,582 reported operations. Acta Orthop 2008; 79: 583–93
- Iorio R, Schwartz B, Macaulay W, Teeney S M, Healy W L, York S. Surgical treatment of displaced femoral neck fractures in the elderly: a survey of the American Association of Hip and Knee Surgeons. J Arthroplasty 2006; 21: 1124–33
- Jensen J S, Tondevold E. Mortality after hip fractures. Acta Orthop Scand 1979; 50: 161–7
- Johansson T, Jacobsson S A, Ivarsson I, Knutsson A, Wahlstrom O. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures: a prospective randomized study of 100 hips. Acta Orthop Scand 2000; 71: 597–602
- Keating J F, Grant A, Masson M, Scott N W, Forbes J F. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg (Am) 2006; 88: 249–60
- Khan R J, MacDowell A, Crossman P, Datta A, Jallali N, Arch B N, Keene G S. Cemented or uncemented hemiarthroplasty for displaced intracapsular femoral neck fractures. Int Orthop 2002; 26: 229–32
- Ohman U, Bjorkegren N A, Fahlstrom G. Fracture of the femoral neck. A five-year follow up. Acta Chir Scand 1969; 135: 27–42
- Parker M J, Gurusamy K. Internal fixation versus arthroplasty for intracapsular proximal femoral fractures in adult. Cochrane Database Syst Rev 2006; CD001708
- Parker M J, Pryor G A. Internal fixation or arthroplasty for displaced cervical hip fractures in the elderly: a randomised controlled trial of 208 patients. Acta Orthop Scand 2000; 71: 440–6
- Ravikumar K J, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur-–13 year results of a prospective randomised study. Injury 2000; 31: 793–7
- Rogmark C, Johnell O. Orthopaedic treatment of displaced femoral neck fractures in elderly patients. Disabil Rehabil 2005; 27: 1143–9
- Rogmark C, Carlsson A, Johnell O, Sernbo I. A prospective randomised trial of internal fixation versus arthroplasty for displaced fractures of the neck of the femur. Functional outcome for 450 patients at two years. J Bone Joint Surg (Br) 2002; 84: 183–8
- Shulman K I. Clock-drawing: is it the ideal cognitive screening test?. Int J Geriatr Psychiatry 2000; 15: 548–61
- Thorngren K G, Hommel A, Norrman P O, Thorngren J, Wingstrand H. Epidemiology of femoral neck fractures. Injury 2002; 33(Suppl 3)C1–C7
- Tidermark J. Quality of life and femoral neck fracture. Acta Orthop Scand 2003; 74(Suppl 309)1–42
- Tidermark J, Zethraeus N, Svensson O, Tornkvist H, Ponzer S. Femoral neck fractures in the elderly: functional outcome and quality of life according to EuroQol. Qual Life Res 2002; 11: 473–81
- Tidermark J, Ponzer S, Svensson O, Soderqvist A, Tornkvist H. Internal fixation compared with total hip replacement for displaced femoral neck fractures in the elderly. A randomised, controlled trial. J Bone Joint Surg (Br) 2003a; 85: 380–8
- Tidermark J, Zethraeus N, Svensson O, Tornkvist H, Ponzer S. Quality of life related to fracture displacement among elderly patients with femoral neck fractures treated with internal fixation. 2002. J Orthop Trauma 2003b; 17: S17–S21