Abstract
Background and purpose Although there have been numerous publications on lumbar disc herniation (LDH) treated surgically, there has been little interest in sex differences. It has been shown in many studies that sex differences may be important in certain diseases. We therefore reviewed consecutive register material from one institution for possible gender differences in pre- and postoperative parameters in patients operated for lumbar disc herniation.
Patients and methods Pre- and postoperative parameters for all patients operated on at the Department of Orthopedics, Lund University Hospital over 6 years (2000–2005 inclusive) (301 patients, 165 males) were analyzed regarding sex differences.
Results Statistically significant and clinically relevant sex differences were found. Preoperatively, females had more pronounced back pain and disability, and also lower quality of life in some respects. At 1-year followup, females reported a higher rate of consumption of analgesics, a higher degree of postoperative back and leg pain, and less improvement regarding disability and some aspects of quality of life. Relative improvement, rate of return to work, and satisfaction with the outcome of surgery were not, however, statistically significantly different between females and males.
Interpretation There are statistically significant differences between the sexes in lumbar disc herniation surgery regarding basic demographic status and postoperative status, whereas the surgical effect is similar. Further investigations should focus on whether there is a true sex difference or whether these differences are due to selection for surgery, differences in proneness to seek medical advice or to accept/choose surgery, or other unknown factors.
Surgery for lumbar disc herniation is a common procedure. In Sweden (with about 9 million inhabitants) almost 2,000 operations are performed annually and disc surgery accounts for more than 40% of all lumbar spine operations (Strömqvist et al. Citation2005, Citation2007).
Absolute indications for lumbar disc surgery are cauda equina syndrome and progressive paresis. These two groups constitute less than 5% of all disc operations and the remainder is performed for pain, mainly radiating leg pain due to nerve root compression. Pain is a subjective experience and the indications for surgery differ greatly at the national level (NKO Citation2005) and also internationally (Deyo et al. Citation2006, Weinstein et al. Citation2006a).
The natural course of disc herniation is often benign; therefore, surgery is not usually considered until there have been 2–3 months of unremitting pain. In long-term follow-up studies, patients operated on for pain seem to benefit in the short term but less so in the long term (Weber Citation1983, Weinstein et al. Citation2006b, Gibson and Waddell Citation2007, Peul et al. Citation2007).
Patients operated on for lumbar disc herniation thus typically have a history of a minimum of 2–3 months of sciatica due to a disc herniation, verified by MRI or CT. Whether or not surgical treatment should be undertaken is the subject of discussion between the patient and the surgeon.
This means that normally there is a decisionmaking process before embarking on lumbar disc surgery. Thus, it would be of interest to study sex differences in patients selected for surgery. In addition, outcome after surgery might be of interest as this may reflect differences in pain experience, selection procedure, rehabilitation, and other factors. Although a large number of studies on surgical treatment of lumbar disc herniation have been published, there appears to have been very little interest in gender aspects.
The Swedish Spine Register includes (among other diagnoses) patients electively operated on for lumbar disc herniation, and preoperative parameters and outcome are registered. This database is thus a good source of information for studying the question of sex differences.
Patients and methods
Data from all 301 patients (165 males) from the Swedish Spine Register who were subjected to scheduled microscopic or open disc herniation surgery at the Department of Orthopedics, Lund University Hospital over 6 years (2000–2005) were collected for this study. Mean age was the same for both sexes: 42 (18–82) years.
The protocol of the register is entirely patientbased regarding pre- and postoperative data, while the surgeon enters surgical data. Preoperative data are taken on admission to hospital and postoperative data are taken at predefined follow-up intervals. For this study, the 1-year follow-up data were used.
The preoperative parameters are: diagnosis, sex, age, smoking habits, consumption of analgesics, walking distance, working ability, duration of leg and back pain before surgery, quality of life (SF- 36), leg and back pain (VAS), and—since 2002— also the Oswestry Disability Index (ODI), which is a disability score relating to back problems.
The postoperative parameters are the same as those preoperatively plus grading of improvement of leg and back pain, separately, on a Likert scale: pain-free, much better, somewhat better, unchanged, or worse; and also general satisfaction with outcome of surgery: satisfied, undecided, or dissatisfied.
Statistics
We used t-tests and ANCOVA analysis. Statistical analysis was performed using either SPSS version 14.0 or SAS version 9.0.
Results
Basic preoperative parameters
Most patients (of both sexes) had experienced leg and back pain 3–12 months before surgery. More than 10% in both groups had had pain exceeding 2 years.
The proportion of smokers was 36% in females and 27% in males. 56% of the females and 51% of the males had been working before surgery.
Two-thirds of patients had consumed analgesics on a regular basis before surgery (females 69%, males 64%) while 8% of the females and 12% of the males had not used analgesics. Preoperative walking distance was similar in both groups: 21% of females and 29% of males could walk for more than 1 km.
Scores
Back pain on a visual analogue scale (VAS) was rated higher by females (mean 52) than by males (mean 41) (p = 0.001). 42% of the females had pain that rated higher than 60 on the VAS scale, as compared to 27% of the males (p = 0.05) ().
Pain on the visual analogue scale (VAS) pre- and postoperatively regarding both back and leg; percentage distribution
Average VAS score for leg pain was 66 in females and 62 in males (p = 0.2) and the distribution was similar ().
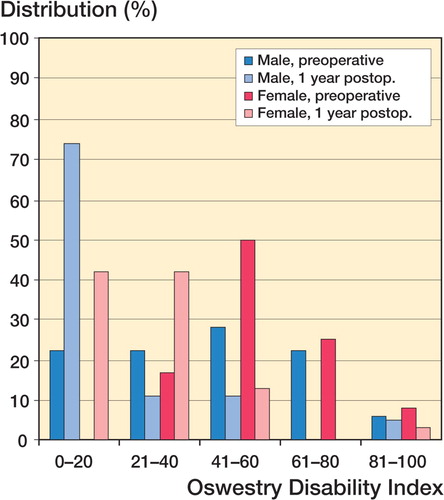
Mean value for ODI preoperatively was 55 in females and 45 in males (p = 0.07). No females reported absence of or minimal disability, i.e. a disability score of 0–20 ().
Figure 1. Disability according to the Oswestry Disability Index (ODI) before and one year after surgery, related to gender.
Regarding quality of life preoperatively (SF-36), differences between the sexes were seen regarding vitality (VT), general health (GH), and mental health (MH). Mean VT for females was 34 and for males it was 42 (p = 0.01). Mean GH for females was 64 and for males it was 73 (p = 0.01). Mean MH in females was 59, as compared to 66 in males (p = 0.05). Thus, in these three respects females showed a lower quality of life than males. Lower values for females were also seen in the other 5 domains, but the differences were not statistically significant ().
Figure 2. Preoperative SF-36 scores, related to gender. PF: physical function, RP: role physical, BP: bodily pain, GH: general health, VT: vitality, SF: social function, RE: role emotional, MH: mental health.
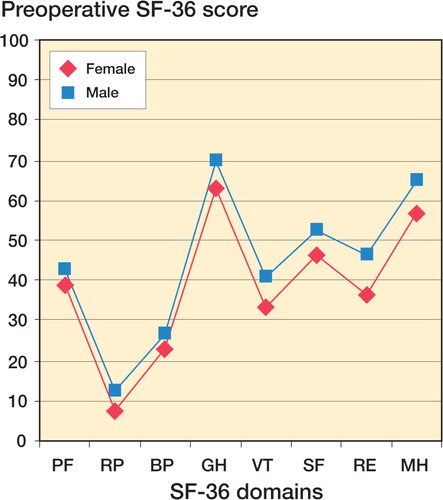
The aggregated mental score (MCS) was lower for females (38) than for males (43) (p = 0.02) while in the aggregated physical score (PSS), the values were not significantly different (29 vs. 31). Preoperative EQ VAS and EQ-5D scores were similar between the sexes. EQ VAS was 47 for males and 50 for females, while EQ-5D was 0.36 for both groups.
Surgical parameters
The most common level for surgery was L5/S1 for both females and males, followed by L4/L5, accounting for more than 85% of the operations. Open surgery was performed in 63% of females and 56% of males, and microscopic technique in the remainder.
Reoperation rate before 1-year follow-up was 2% for both sexes.
Postoperative parameters
At the 1-year follow-up, 35% of the females and 55% of the males consumed no analgesics at all (p = 0.002).
70% of the patients could walk more than 1 km one year after surgery, with no difference between the sexes.
Of the patients who had been working before surgery, one-third had returned to work within 3 months of surgery and a further one-third within 6 months. There was no statistically significant difference in sick-listing frequency or postoperative sick-listing time between females and males.
Scores
Mean postoperative back pain (VAS) score for females was 32 and for males it was 24 (p = 0.04). 32% of females and 56% of males estimated the back pain to have a score of < 10 (p = 0.0003) i.e. they were virtually pain-free ().
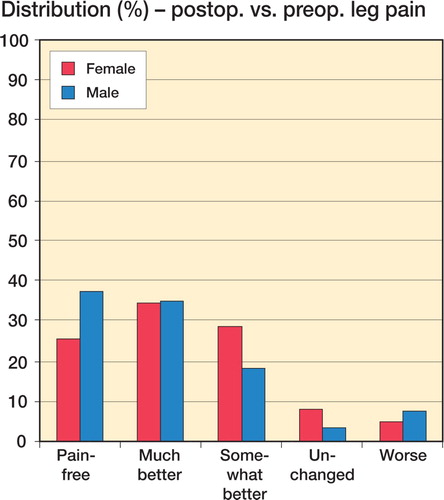
Both groups showed a dramatic improvement in leg pain compared to the situation preoperatively. Mean postoperative leg pain (VAS) score was 30 for females and 22 for males (p = 0.07). 39% of females and 56% of males estimated their leg pain to be less than 10 (p = 0.010) ().
Disability (ODI) score decreased in both sexes postoperatively, but to a lesser extent in females (26) than in males (15) (p = 0.04). Only 42% of females scored 0–20 (i.e. had no or insignificant disability) as compared to 74% of males (p = 0.008) ().
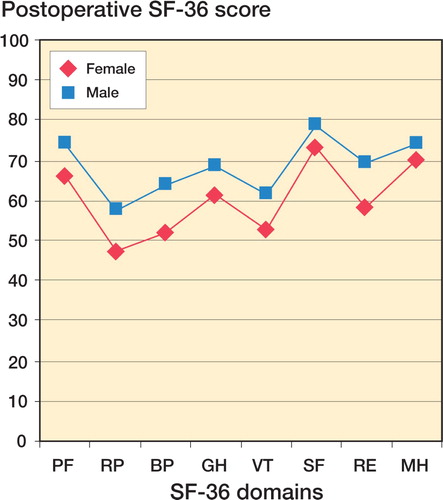
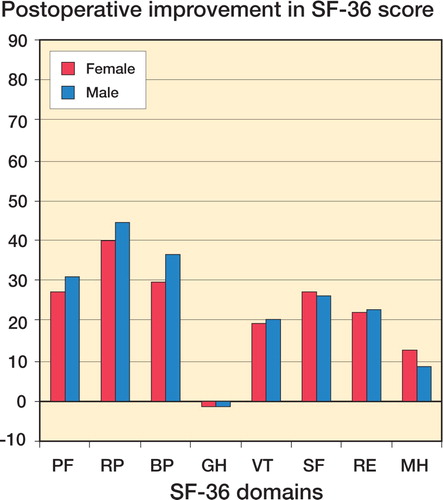
Quality of life improved postoperatively in both sexes (). Postoperative PF score was better for males (75) than for females (66) (p = 0.02). BP scored 64 and 52, respectively (p = 0.004), and VT score was 64 for males and 51 for females (p = 0.001). The aggregated mental and physical scores, MSC and PSC, the EQ-5D scores (0.64 and 0.62), and scores for the EQ VAS (62 and 68) were similar between the sexes.
Figure 3. SF-36 one year postoperatively, related to gender. PF: physical function, RP: role physical, BP: bodily pain, GH: general health, VT: vitality, SF: social function, RE: role emotional, MH: mental health.
Pre- and postoperative differences Back pain after surgery improved for 85% of females and for 85% of males, while 17% of the females and 34% of the males had no back pain at all at follow-up (). Almost 90% of patients operated reported improvement in leg pain compared to preoperatively, while 5% of females and 7% of males experienced increased leg pain postoperatively (), which suggests that back and leg pain improved to similar extents in females and males.
Figure 4. Patient-related change in back pain one year postoperatively compared to before surgery, related to gender.
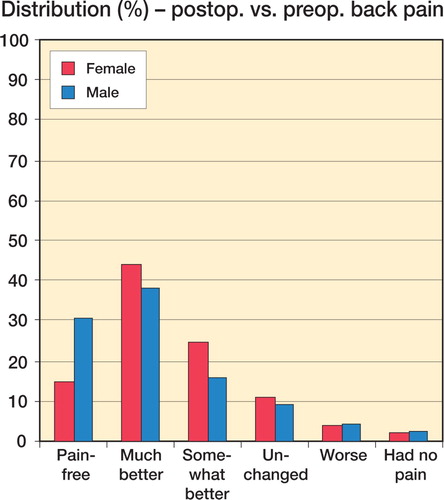
Figure 5. Patient-related change in leg pain one year postoperatively compared to before surgery, related to gender.
Comparison of the individual improvement in VAS pain for back and for leg (ANCOVA) showed no significant differences between the sexes. Mean improvement in back pain for females and males was 20 and 16 units, respectively, and mean improvement in leg pain was 36 and 40 units. Quality of life improved in all domains except GH (general health). The only sex-related differences were seen in BP, where females improved by a mean of 30 and males improved by a mean of 38 (p = 0.01) ().
Figure 6. Change in SF-36 scores one year postoperatively compared to before surgery, related to gender. PF: physical function, RP: role physical, BP: bodily pain, GH: general health, VT: vitality, SF: social function, RE: role emotional, MH: mental health.
Overall satisfaction with outcome of surgery was more or less identical in the two groups. 70% of females and 73% of males were satisfied, 20% and 18% were undecided, and 10% and 9% were dissatisfied.
In summary, patient-graded improvement after surgery and satisfaction were high and virtually the same in both sexes.
Loss-to-follow-up analysis
The loss to postoperative 1-year follow-up was 20%. These patients were compared to the remaining 80% regarding preoperative parameters and no differences were seen. Mean age of the patients lost to follow-up was 43, as compared to 42 years for those who were followed up. In the group of patients who were lost to follow-up, 53% were males and 47% were females, as compared to 55% and 45% of those who were followed up. The SF- 36 scores were similar. Mean preoperative back pain (VAS) score was 50 for those who were lost to follow-up and 48 in those who were followed up. The corresponding figures for leg pain were 67 and 64.
Discussion
When surgery for painful disc herniations is considered, there is a relative consensus on nonoperative treatment for the first 6–8 weeks. This opinion is strongly underlined by the long duration of preoperative symptoms in our study. A long duration of pain before treatment may also reflect waiting times for MRI, CT, and surgery—and possibly a restrictive attitude to surgical treatment—but it need not have a negative effect on the outcome (Peul et al. Citation2007).
Regarding gender differences in lumbar spine surgery, it has been documented that being female is a negative prognostic sign regarding outcome in spinal stenosis (Aalto et al. Citation2006). Regarding lumbar disc herniations, a few contradictory reports exist (Rasmussen Citation1996, Loupasis et al. Citation1999, Vucetic et al. Citation1999, Jansson et al. Citation2005). This was our incitement to study differences between the sexes in a large unselected group of patients who were operated for painful disc herniations.
The Swedish spine register was started in 1993 (Strömqvist and Jönsson Citation1993), and today it covers surgical treatment in more than 80% of the centers in Sweden that perform spinal surgery (Strömqvist et al. Citation2005). The pre- and postoperative data are entirely patient-based, which diminishes the risk of outcome bias. The loss to 1-year follow-up was 20%, which is lower than in most of the large studies that have been published (Spangfort Citation1972, Hoffman et al. Citation1993, Vucetic et al. Citation1999). Some of this loss can be explained by reoperation, incomplete registration, and death before follow-up. In our study, we found similar preoperative demographics in patients who were followed-up and not followed-up.
The proportion of smokers in females (36%) and males (27%) was clearly higher than national figures for Sweden (14% and 19%, respectively) (Statens folkhälsoinstitut Citation2004). This may be associated with the accelerated degenerative process of the discs from smoking (Battie et al. Citation1991), but it may also reflect differences in lifestyle between smokers and non-smokers (Rasmussen Citation1998).
We found a pronounced pain-relieving effect of lumbar disc herniation surgery, and the relative improvement was similar for both females and males. Whether the higher back pain estimation and lower quality-of-life estimation reported preoperatively by females is a sex-related effect, an effect of selection for surgery, or an effect of proneness to undergo surgery cannot be determined from this study, but it justifies closer scrutiny. This is also the case for the tendency to have higher degrees of remaining pain and greater disability according to ODI that we found in females postoperatively. These scores and some of the physical scores of the SF-36 showed better outcome in males than in females, despite the fact that general satisfaction with surgery was identical in both sexes. Another recent study (Häkkinen et al. Citation2007) also found higher disability (ODI) in females preoperatively, but this difference did not persist after surgery. The patient-based Swedish spine register reflects the subjective experiences of the patient pre- and postoperatively, whereas in previous large studies of lumbar disc herniation the outcome has been graded by the surgeon—or at times an unbiased observer (Spangfort Citation1972, Weber Citation1983). Furthermore, most studies on surgical treatment of lumbar disc herniation in the literature involve patients treated at a specialized unit whereas the results of the Swedish register reflect outcome on a national basis.
It must be noted that all surgeons in this study were male. Some studies hint at the possibility that females may be treated at a more advanced stage of disease (Katz et al. Citation2007, Council on Ethical and Judicial Affairs Citation2007). Other studies have demonstrated sex-related differences in musculoskeletal disorders (Fillingim et al. Citation2003, Keogh et al Citation2005, Wijnhoven et al Citation2007). Irrespective of these considerations, the relative improvement after surgery and satisfaction with outcome were similar for females and males in this study.
Another factor that relates to subjective satisfaction with outcome is preoperative expectations, which are in turn related to preoperative information given that is definitely not standardized on a national basis. However, the outcome of the protocol of the Swedish spine register has recently been validated in a test-retest analysis (Zanoli et al. Citation2006).
In conclusion, this study on LDH surgery demonstrates that there is more pronounced back pain and disability preoperatively—as well as lower quality of life in some respects—in females than in males. These differences persist postoperatively to some extent, but the relative improvement after surgery and satisfaction with outcome were the same for both sexes. The reasons for the preoperative differences are probably manifold, but require future studies for proper elucidation. The data presented here can be used for creation of more specific and individual-related indications for lumbar disc herniation surgery.
We are grateful to Caddie Zhou of the Swedish National Competence Center for Musculoskeletal Disorders for statistical advice and for performing statistical analysis.
No competing interests declared.
Contributions of authors
All authors contributed to the conception and design of the study. FS and MA performed data processing and prepared the manuscript. CH, BJ, and BS critically revised the manuscript.
- Aalto T J, Malmivaara A, Kovacs F, Herno A, Alen M, Salmi L, Kröger H, Andrade J, Jiménez R, Tapaninaho A, Turunen V, Savolainen S, Airaksinen O. Preoperative predictors for postoperative clinical outcome in lumbar spinal stenosis: systematic review. Spine 2006; 31: E648–63
- Battie M C, Videman T, Gill K, Moneta G B, Nyman R, Kaprio J, Koskenvuo M. Smoking and lumbar intervertebral disc degeneration: an MRI study of identical twins. Spine 1991; 16: 1015–21
- Council on Ethical and Judicial Affairs, American Medical Association. Gender disparities in clinical decision making. JAMA 2007; 266: 559–62
- Deyo R A, Mirza S K. Trends and variations in use of spine surgery. Clin Orthop Relat Res 2006; 443: 139–46
- Fillingim R B, Doleys D M, Edwards R R, Lowery D. Clinical characteristics of chronic back pain as a function of gender and oral opioid use. Spine 2003; 28(2)143–50
- Gibson J N, Waddell G. Surgical interventions for lumbar disc prolapse. Cochrane Database Syst Rev Jan, 2007; 24(1)CD001350
- Hoffman R M, Wheeler K J, Deyo R A. Surgery for herniated lumbar discs: a literature synthesis. J Gen Intern Med 1993; 8: 487–96
- Häkkinen A, Kautiainen H, Järvenpää S, Arkela-Kautiainen M, Ylinen J. Changes in the total Oswestry Index and its ten items in females and males pre- and post-surgery for lumbar disc herniation: A 1-year follow-up. Eur Spine J 2007; 16: 347–52
- Jansson K A, Németh G, Granath F, Jönsson B, Blomqvist P. Health-related quality of life in patients before and after surgery for a herniated lumbar disc. J Bone Joint Surg (Br) 2005; 87: 959–64
- Katz J N, Wright E A, Guadagnoli E, Liang M H, Karlson E W, Cleary P D. Differences between men and women undergoing major orthopaedic surgery for degenerative arthritis. Arthritis Rheum 2007; 37: 687–94
- Keogh E, McCracken L M, Eccleston C. Do men and women differ in their response to interdisciplinary chronic pain management?. Pain 2005; 114: 37–46
- Loupasis G A, Stamos K, Katonis P G, Sapkas G, Korres D S, Hartofilakidis G. Seven- to 20-year outcome of lumbar discectomy. Spine 1999; 24: 2313–7
- Nationellt Kompetenscentrum för Ortopedi. Indikationer för behandling inom ortopedi. 2005; Ver 1.1: 28–32.
- Peul W C, van Houwelingen H C, van den Hout W B, Brand R, Eekhof J A, Tans J T, Thomeer R T, Koes B W. Leiden- The Hague Spine Intervention Prognostic Study Group. Surgery versus prolonged conservative treatment for sciatica. N Engl J Med. 2007; 356(22)2239–43
- Rasmussen C. Lumbar disc herniation: social and demographic factors determining duration of disease. Eur Spine J 1996; 5: 225–8
- Rasmussen C. Lumbar disc herniation: favourable outcome associated with intake of wine. Eur Spine J 1998; 7: 24–8
- Spangfort E V. The lumbar disc herniation: A computer aided analysis of 2,504 operations. Acta Orthop Scand 1972; 142: 1–95
- Statens folkhälsoinstitut. Nationella folkhälsoenkäten “Hälsa på lika villkor?” – nationella data 2004. http://www.fhi.se/templates/Pag5849.aspx
- Strömqvist B, Jönsson B. Computerized follow-up after surgery for degenerative lumbar spine disease. Acta Orthop Scand 1993; 64(Suppl 251)138–42
- Strömqvist B, Fritzell P, Hägg O, Jönsson B. One-year report from the Swedish National Spine Registe. Swedish Society of Spinal Surgeons. Acta Orthop 2005; 76(Suppl 319)1–24
- Strömqvist B, Hedlund R, Jönsson B, Tullberg T. Ländryggens sjukdomar. Läkartidn 2007; 104: 1498–502
- Weber H. Lumbar disc herniation: a controlled, prospective study with ten years of observation. Spine 1983; 8: 131–40
- Weinstein J N, Lurie J D, Olson P R, Bronner K K, Fisher E S. United States' trends and regional variations in lumbar spine surgery: 1992–2003. Spine 2006a; 31: 2707–14
- Weinstein J N, Tosteson T D, Lurie J D, Tosteson A N, Hanscom B, Skinner J S, Abdu W A, Hilibrand A S, Boden S D, Deyo R A. Surgical vs nonoperative treatment for lumbar disk herniation. The Spine Patient Outcomes Research Trial (SPORT): A randomized trial. JAMA 2006b; 296: 2441–50
- Wijnhoven H A H, de Vet H C W, Picavet H S J. Sex differences in consequences of musculoskeletal pain. Spine 2007; 32(12)1360–7
- Vucetic N, Astrand P, Guntner P, Svensson O. Diagnosis and prognosis in lumbar disc herniation. Clin Orthop 1999, 361: 116–22
- Zanoli G, Nilsson L T, Strömqvist B. Reliability of the prospective data collection protocol of the Swedish Spine Register. Acta Orthop 2006; 77: 662–9