Abstract
Background and purpose The most reliable results when treating an infected total knee arthroplasty have been obtained with a two-stage reimplantation protocol. We have used a simple technique for hand-made spacers and now report the outcome.
Patients and methods 30 patients with an infected total knee arthroplasty (TKA) were treated with a 2- stage reimplantation protocol. Spacers were built and customized to the type of defect using only 2 retractors and a high-speed tip burr. Partial weight bearing and discharge from the hospital were encouraged in the time between surgeries. 29 of 30 patients (97%) had successful reimplantations and they were followed for an average of 3 (2–5) years.
Results Range of motion with the articulating spacer averaged 80° (55–100) and 21 of the 30 patients achieved motion greater than 75°. At the latest follow-up, there were no reinfections. According to the Knee Society score (KSS), the results were considered excellent or good in 25 patients, and fair or poor in 4 of the 29 patients with reimplantations. Motion after reimplantation averaged 107° (90–120).
Interpretation One of the key factors related to a successful outcome with a two-stage reimplantation procedure is to keep the joint mobile and functional in the time between surgeries. Hand-made articulating spacers retain most of the advantages of more complex spacers in terms of mobility, pain, bone loss, success, or re-infection rate—with the major advantages of price and universal availability. Limitations related to this technique include potential knee instability, the need to walk with an orthosis, and the risk of subluxations.
Infection is one of the worst complications of a total knee arthroplasty procedure. It has been reported to affect between 2% and 3% of primary procedures, with double these rates in cases of revision arthroplasty (Mulvey and Thornhill Citation2001). Revision of an infected total knee arthoplasty is 3–4 times more expensive than the index procedure, and twice the cost of an aseptic revision (Hebert et al. Citation1996).
The goal of treatment of an infected knee arthroplasty is to eradicate the infection while preserving the function of the extremity. The surgeon can affect the final result at 3 fundamental steps: (1) the initial joint debridement, (2) the protocol and type of spacer used between operations, and (3) the surgical technique and selection of prosthesis at reimplantation (Whiteside Citation1994).
The most accepted and consistent results have been achieved with a two-stage reimplantation protocol including the removal of all the prosthetic components and the insertion of a temporary, antibiotic- loaded spacer between surgeries followed by a 4–6-week course of intravenous antibiotics, and then a delayed implantation of a new prosthesis fixed with antibiotic-loaded cement (Windsor et al. Citation1990, Haddad et al. Citation2001, Hoffman et al. Citation2005).
Proposed advantages of the articulating spacers include maintenance of function and motion of the knee, minimization of soft tissue contractures, preservation of bone stock, and the possibility of delivering high concentrations of antibiotics. Spacers also reduce the need for extensile exposures at reimplantation and facilitate patient comfort and early hospital discharge (Calton et al. Citation1997, Haddad et al. Citation2000).
Although articulating spacers were introduced 20 years ago, surgeons have continuously described new modifications of spacers to adapt them to their specific technical and budgetary constraints. Most modifications have yielded good results (Insall et al. Citation1983, Cohen et al. Citation1988, Booth and Lotke Citation1989, Duncan et al. Citation1992, McPherson et al. Citation1995, Siebel et al. Citation2002, Durbhakula et al. Citation2004, Ha Citation2006, Mcavoy and Ries Citation2006). The simplest, cheapest, and universally available method for making articulating spacers is to build them during surgery (Villanueva et al. Citation2006).
We examined the outcome of a uniform technique of making hand-made articulating knee spacers. The procedure only requires three basic surgical tools, it does not involve autoclaving, and it does not require the use of trial plastic molds or of metallic components.
Patients and methods
30 patients (23 females), with an infected total knee arthroplasty were treated with a 2-stage revision protocol that included the use of a custom handmade antibiotic-loaded articulating spacer built using a standardized technique. 26 patients had osteoarthritis and 4 patients had rheumatoid arthritis. All patients were reviewed retrospectively. We together started to perform this technique at the institution of the first author, and later on at other hospitals. The series include consecutive patients in which 2-stage reimplantation was considered the best option for treatment. Mean age at the time of treatment was 71 (64–82) years. 9 patients had had multiple previous operations on the infected knee. Time to our treatment, since the index arthroplasty, averaged 18 (1–144) months.
Before our procedure, 14 patients had had posterior stabilized designs (PS), 13 patients had had a cruciate retaining prosthesis (CR), and 4 patients had had revision designs including wedges and stems (2 with a PS model and 2 with a deepdish ultracongruent polyethylene component). 2 patients had had a quadriceps snip at the time of a previous revision. None of the cases had been operated using minimum invasive surgery.
Staphylococcus aureus (SA) and coagulase-negative Staphylococcus (CNS) were each present in 12 of the patients, with 3 meticillin-resistant SA, 9 non-meticillin-resistant SA, 5 meticillin-resistant CNS, and 7 non-meticillin-resistant CNS. Enterobacteriae were present in 6 cases and anaerobes and streptococci were present in 3 other cases. In 3 cases, a polimicrobial infection was diagnosed.
At the first stage of surgery, all prosthesis components were removed and an extensive debridement of the knee was done. Samples were then taken for microbiological culture and pathological analysis, including intraoperative frozen sections to establish “definitive criteria of infection” (Atkins et al. Citation1998).
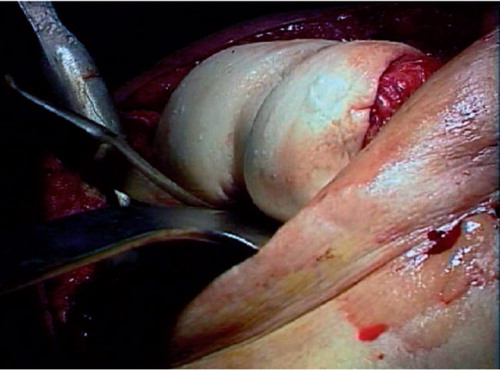
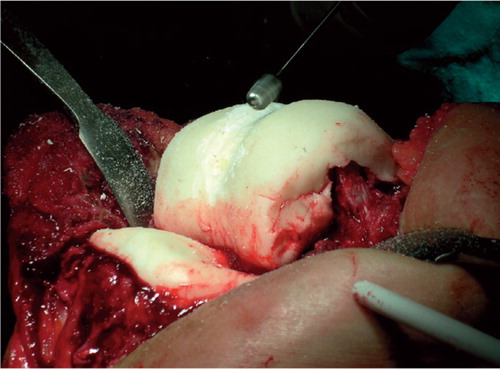
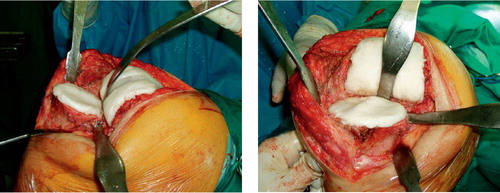
The articulating spacer. 3 g of antibiotics (7.5%) per pack of cement was used in all but 4 cases. All spacers were constructed with CMW 1 with gentamycin (De Puy), to which 2 extra grams of gentamycin or 2 extra grams of vancomycin were added, or Simplex (Stryker-Howmedica) cement, to which 3 g of extra gentamycin or vancomycin per pack were added. The cement was modeled in its doughy phase to avoid excessive interdigitation in the remaining bone, and to facilitate its removal at reimplantation. The surgeon must know the time at which the cement cures and hardens with the antibiotics added. No pre-manufactured molds were used and no trial or previously autoclaved components were used to build the spacer. A Hohmann retractor, a curved osteotome, and a high-speed tip burr were all the surgical tools required. The components of the spacer were conformed manually following the basic guidelines that we have previously described (Villanueva et al. Citation2006) (–).
Figure 1. The grooves, the central crest on the tibial component, and the trochlear groove on the femoral component can be seen. This shape of the spacer increases conformity and reduces instability.
A continuous passive motion program was started within 24 h postoperatively with a Kinetec, progressing slowly in flexion and never surpassing 90° () to avoid potential subluxation and locking of the spacer. Isometric exercises with and without bracing were encouraged, as well as active flexion and extension exercises with the heel resting on the bed or on the hand of a physiotherapist.
Partial weight bearing with the aid of crutches or a cane was allowed as tolerated. An extension or hinge orthosis of the knee was worn during ambulation until soft tissue healing had occurred. If slight or mild laxity remained, the brace was worn until reimplantation.
Antibiotic therapy was instituted by the infectious diseases specialist and the patient entered a “hospital at home” program after discharge from the hospital.
After discontinuation of antibiotics for at least 2 weeks, reimplantation was performed guided by intraoperative fresh-frozen samples, with more than 5 polymorphonuclear leukocytes (PMN) per high-power field being considered predictive of infection. In patients with inflammatory diseases, we based our decision on previous aspiration cultures. 2 cases had false positive histology and reimplantation was delayed for 15 days—when the cultures taken were negative (Fehring and McAllister Citation1994, Lonner et al. Citation1996). At reimplantation the same type of cement-loaded antibiotic was used, limiting the percentage of antibiotic to 2.5% of the final composite.
Results (Table)
Reimplantation was performed in 29 of the 30 patients (97%) at an average time of 14 (8–130) weeks. In a patient with rheumatoid arthritis, reimplantation was delayed 2.5 years due to the patient's initial rejection of prosthetic knee reimplantation after 3 exchanges of the spacer because of persistent infection. One patient finally required an arthrodesis after several debridements and impairment of the extensor mechanism. At reimplantation, we used 21 semiconstrained implants (intercondylar stabilized), 6 posterior stabilized implants, and 2 rotating-hinge prostheses.
Range of motion (ROM) with the spacer averaged 80° (55–100). 21 patients achieved a motion greater than 75° with the articulating spacer.
At reimplantation, tibial tuberosity osteotomy was performed in the 2 patients who had the poorest motion between surgeries, and 5 “quadriceps snips” were performed. One patient required a proximal Insall's realignment at the second stage of surgery. His final motion was 5–100°. Another patient required the realignment at the first stage, due to extensor mechanism and surgical wound dehiscence.
3 patients had a mild extension lag at the final follow-up. One of them had required an Insall's realignment at reimplantation (ROM 5–110°) and the other 2 a tibial tuberosity osteotomy (ROM 5–110° and 10–100°, respectively).
According to the Knee Society score (KSS), the results following reimplantation were excellent (85–100 points) or good (70–84 points) in 25 patients and fair (60–69 points) or poor (less than 60 points) in 4 patients. Average motion after reimplantation was 107° (90–120°).
3 cases had complications directly related to the spacer. These included 2 subluxations, manually reduced, and a fracture of the posterior condyles of the femoral spacer. In 4 cases with segmentary defects, 1 component had to be rebuilt during the first surgery to obtain adequate shape and stability.
Discussion
In the treatment of infected total knee arthroplasties, the importance of every single factor affecting the final outcome (extensive debridement, time from clinical onset, the infecting microorganism, the dosage and combination of antibiotics, type of spacer, the technique, and prostheses selection at reimplantation) still remains to be defined as the series and techniques reported are not uniform— and hence difficult to compare. The use of articulating spacers as part of a 2-stage reimplantation protocol has, however, proven to be important in the eradication of infection and preservation of joint function (Haleem et al. Citation2004)—regardless of multiple modifications that include the use of specific molds and the use and resterilization of trial components or previous implants (Insall et al. Citation1983, Cohen et al. Citation1988, Booth and Lotke Citation1989, Duncan et al. Citation1992, McPherson et al. Citation1995, Goldstein et al. Citation2001, Siebel et al. Citation2002, Durbhakula et al. Citation2004, Ha Citation2006, MacAvoy and Ries Citation2006). The use of these complex systems has not been generalized, however, and hand-made spacers are probably the most commonly used.
Cases of infected knee arthroplasties
We have recently described a step-by-step technique to construct articulating spacers with just 3 basic surgical tools, thus representing an inexpensive method that is applicable in all operating theaters (Villanueva et al. Citation2006). Our findings in this consecutive series of 30 patients imply that our hand-made spacers function as well as more complex constructs.
29 of 30 patients were successfully reimplantated without recurrence of infection at the most recent follow-up, at a minimum of 2 years. 25 of 29 patients had excellent or good results and only 4 had fair or poor results according to the KS score. Partial weight bearing and discharge from the hospital were possible in the time between surgeries. Range of motion (ROM) with the spacer averaged 80° and after reimplantation it was 107°.
2 patients required a tibial tubercle osteotomy at reimplantation and 3 patients had an extension lag, but it could be partially related to limited ROM with the spacer in only 1 case. Other advantages of spacers, such as minimizing the retraction of the extensor mechanism, preventing muscle atrophy and pain, preservation of bone stock (Calton et al. Citation1997), and good knee motion (Hoffman Citation2005) all appear to be achieved with our hand-made spacers.
Complications included two subluxations, reduced with a “Lachman test” maneuver, and a spacer broken at the posterior condyle, which did not affect knee mobility. The need to rebuild the spacer in cases with considerable defects reflected the learning curve of a manual procedure and did not affect the final result, but it lengthened surgical time. Specific problems when building the spacer were excessive tissue tension, lack of posterior capsule release that prevented extension of the posterior part of the femoral spacer (leading to instability of the femoral component), and elevation of the posterior part of the tibial component—creating an anterior slope or inclination that limited flexion and caused anterior subluxation ().
The possibility of adding high doses of antibiotic is another advantage of spacers. It has been verified that the intraarticular levels of antibiotics are higher in this way than with parenteral antibiotic therapy alone (McLaren and Spooner Citation1996, Jiranek et al. Citation2006), thus avoiding the development of antibiotic resistance.
It has been shown that the maximum quantity of antibiotic to be added that will not affect the mechanical properties of the cement is around 5% of the total weight of the cement (Haddad et al. Citation2001, Jiranek et al. Citation2006). However, most authors use much higher doses of antibiotic in the temporary spacers used between surgeries. These systems should not be used for longer than 8–12 weeks, which is not enough for the expected increase in fragility of the cement to have any clinical relevance.
Hoffmann et al. (Citation2005) reported 50 cases in which they mixed tobramycin with the cement in a 12% proportion to give the final composite. They had a 12% reinfection rate, but the authors used spacers including plastic and metal components. MacAvoy and Ries (Citation2006) used a 9% antibioticcement composite with a ball and socket technique not involving plastic or metal components. They had a 30% reinfection rate at 18 months, probably related to the co-morbidities of their patient population. Using 10–12% antibiotic in the cement-antibiotic composite, Ha (Citation2006) treated 12 cases with a spacer made of cement alone, and there were no recurrences of the infection. Durbhakula et al. (Citation2004) used silicone molds (ALACS) to build their spacers without the inclusion of cement or plastic elements. The authors used an antibiotic-loaded cement spacer with a mean proportion of antibiotic of 8%. 2 of 24 patients had persistent infection at the time of intended reimplantation.
Our spacers did not include plastic or metallic elements, and the cement proportion was 7.5%. This could be a real limitation of hand-made spacers because with proportions higher than 10%, the cement becomes stiffer and more difficult to model—so we were using theoretically suboptimal dosages (Jiranek et al. Citation2006). However, our high rate of eradication of infection compares to other reports using higher proportions, reflecting that this factor alone is only part of a successful protocol. 2 patients required repeated debridements: 1 had successful reimplantation and 1 was finally arthrodesed. There have been no recurrences of infection at a minimum 2 years follow-up.
We used semi-constrained designs at reimplantation in 21 patients. In a series of 13 patients with severe bone loss or collateral ligaments deficiencies, MacAvoy and Ries (Citation2006) only used constrained designs in 5 cases. In their series of 50 patients, Hoffmann et al. (Citation2005) reported 36 reimplantations performed with ultracongruent designs, with the same proportion of semi-contrained as in our series.
It may be expected that some residual laxity of the knees with the cemented spacers might contribute to secondary damage of the collateral ligaments, but this is not our experience. In cases of revision knee surgery, one frequently needs a higher level of constriction than in the prior surgery and 17 cases in our series already had a posterostabilized design at the time of onset of infection, some including stems, steering the preference of the surgeon at reimplantation to a semi-constrained design rather than to a posterostabilized prosthesis (Lampe and Hiller Citation2005). We used the hinge designs in 2 multioperated patients with severe bone loss, soft tissue damage, and poor functional status.
We found a similar final result regardless of the time elapsed between the initial surgical debridement and final reimplantation. As long as the joint remains functional with controlled mobility and partial weight bearing, the final outcome seems not to be jeopardized.
In summary, hand-made articulating spacers appear to function as well as more complex, expensive spacers.
Acknowledgement
No competing interests declared A video illustrating this technique was given an award by the American Academy of Orthopaedic Surgeons (AAOS), San Diego 2007.
Link: http://www4.aaos.org/product/productpage.cfm?code=17102
Contributions of authors
All authors have used the technique described, contributed cases to the series, and participated in writing of the manuscript.
- Atkins B, Athanasou N, Deeks J, Crook D W M, Simpson H, Peto T E, McLardy-Smith P, Berendt A R. Prospective evaluation of criteria for microbiological diagnosis of prosthetic-joint infection at revision arthroplasty. J Clin Microbiol 1998; 36: 2932–9
- Booth R E, Jr, Lotke P A. The results of spacer block technique in revision of infected total knee arthroplasty. Clin Orthop 1989, 248: 57–60
- Calton T F, Fehring T K, Griffin W L. Bone loss associated with the use of spacer blocks in infected TKA. Clin Orthop 1997, 345: 148–54
- Cohen J C, Hozack W J, Cuckler J M, Booth R E. Two-stage reimplantation of septic total knee arthroplasty: report of three cases using an antibiotic- PMMA spacer block. J Arthroplasty 1988; 3: 369–77
- Duncan C P, Beauchamp C P, Masri B. The antibiotic loaded joint replacement system: A novel approach to the management of the infected knee replacement. J Bone Joint Surg (Br) 1992; 74(3)296
- Durbhakula S M, Czajka J, Fuchs M D, Uhl R L. Antibioticloaded articulating cement spacer in the 2-stage exchange of infected total knee arthroplasty. J Arthroplasty 2004; 19: 768–74
- Goldstein W, Kepplin M, Well R, Berland K. Temporary articulating methylmethacrylate antibiotic spacer (TAMMAS). A new method of intraoperative manufacturing of a custom articulating spacer. J Bone Joint Surg (Am) 2001; 83(2)92–7
- Fehring T K, McAlister J A. Frozen histologic section as a guide to sepsis in revision joint arthroplasty. Clin Orthop 1994, 304: 229–37
- Ha C W. A technique for intraoperative construction of antibiotic apacers. Clin Orthop 2006, 445: 204–9
- Haddad F S, Masri B A, Campbell D, MacGraw R W, Beauchamp C P, Duncan C P. The PROSTALAC functional spacer in two-stage revision for infected knee replacements. J Bone Joint Surg (Br) 2000; 82: 807–12
- Haddad F, Masr B, Duncan C. Cement spacers in knee surgery. 1891–1914. “Surgery of the knee”3. Churchil Livingstone. 2001, Insall- Scott
- Haleem A A, Berry D J, Hanssen A D. Mid-term to longterm followup of two-stage reimplantation for infected total knee arthroplasty. Clin Orthop 2004, 428: 35–9
- Hebert C K, Williams R E, Levy R S, Barrack R L. Cost of treating an infected total knee replacement. Clin Orthop 1996, 331: 140–5
- Hoffman A A, Goldberg T, Tanner A M, Kurtin S M. Treatment of infected total knee replacement arthroplasty using an articulated spacer. 2 to 12 year experience. Clin Orthop 2005, 430: 125–31
- Insall J N, Thompson F M, Brause B D. Two stage reimplantation for the salvage of infected TKA. J Bone Joint Surg (Am) 1983; 65(8)1087–98
- Jiranek W A, Arlen D, Hanssen A D, Greenwald A S. Antibiotic- loaded bone cement for infection prophylaxis in total joint replacement. J Bone Joint Surg (Am) 2006; 88: 2487–500
- Lampe F, Hille E. Failure in contraint: Too little. Total knee arthroplasty. A guide to get better performance, J Bellemans, M Ries, J Victor, 2005; 74–84
- Lonner J H, Desai P, Dicesare P E, Steiner G, Zuckerman J D. The reliability of analysis of intraoperative frozen sections for identifying active infection during revision hip or knee arthroplasty. J Bone Joint Surg (Am) 1996; 78: 1553–8
- MacAvoy M C, Ries M D. The ball and socket articulating spacer for infected total knee arthroplasty. J Arthroplasty 2006; 20: 757–62
- McLaren A C, Spooner C E. Salvage of infected total knee components. Clin Orthop 1996, 331: 146–50
- McPherson E J, Lewonowski K, Dorr L D. Use of an articulated PMMA spacer in the infected TKA. J Arthroplasty 1995; 10: 87–9
- Mulvey T, Thornhill T. Infected total knee arthroplasty: 1875–1890. Surgery of the knee3, Insall- Scott. Churchil Livingstone. 2001
- Siebel T, Kelm J, Porsch M, Regitz T, Neumann W H. Twostage exchange of infected knee arthroplasty with an prosthesis like interim cement spacer. Acta Orthop Belg 2002; 68(2)150–6
- Villanueva M, Rios A, Pereiro J, Chana F, Fahandez-Saddi H. Hand made articulating spacers for infected total knee arthroplasty. A technical note. Acta Orthop Scand 2006; 77: 329–32
- Whiteside L A. Treatment of infected total knee arthroplasty. Clin Orthop 1994, 299: 169–72
- Windsor R E, Insall J N, Urs W K, Miller D V, Brause B D. Two stage reimplantation for the salvage of total knee arthroplasty complicated by infection: further followup and refinement of indications. J Bone Joint Surg Am 1990; 72: 272–8