In January 2003 a 63-year-old, otherwise healthy man presented at our department with clinical signs of osteoarthritis of the left hip. Plain radiographs showed osteoarthritis without signs of avascular necrosis (AVN) or osteoporosis (. No previous diseases or trauma had affected the patient's hip. After preoperative counselling on various surgical options, the patient was scheduled for a hip resurfacing procedure. Regular preoperative investigations showed normal values of hemoglobin, sodium, potassium, prothrombin time international normalized ratio (PTT-INR) and C-reactive protein, and a normal blood pressure was found.
Figure 1. A. Preoperative radiograph showing osteoarthritis of the left hip without signs of avascular necrosis (AVN) or large femoral head cysts. B. Postoperative radiographs showing ordinary implant position after resurfacing arthroplasty in anterior-posterior view (B1) and in axial view (B2). C. Radiographic follow-up 1 year postoperatively showing unchanged implant position. D. Radiographic follow-up 2 years postoperatively showing a discrete change in the position of the femoral component. E. Radiographs 3.5 years after the index procedure showing varus tilting of the femoral component and a fracture of the femoral neck in anterior-posterior view (E1) and in axial view (E2); panel E3 is a closeup of panel E1. F. Radiograph taken after revision surgery showing conventional femoral component equipped with a large-diameter metal head.
The patient then underwent a fourth-generation metal-on-metal hip resurfacing procedure with the Durom implant (Zimmer Inc., Warsaw, IN). The surgical approach was anterolateral according to Hardinge (Citation1982), with the patient in a lateral decubitus position. The anterior capsule was incised but the posterior capsule was not divided. No macroscopic signs of osteoporosis were seen and the bone stock in the femoral head was good. A 60mm acetabular component and a 54-mm femoral component were chosen, and gentamicin-loaded cement (Palacos R; Heraeus, Hanau, Germany) was used for fixation of the femoral component. Pulse lavage was used for cleaning of the femoral head, but without intraosseous suction. No intraoperative complications were recorded, and importantly, no notching of the femoral neck occurred. Perioperatively, the patient received antibiotic prophylaxis (cloxacillin 1 g×3 intravenously) and antithrombolytic treatment (tranexamic acid 1 g×1). Postoperative plain radiographs showed an ordinary implant position, and there was no notching of the femoral neck (). Postoperative recovery was uneventful; the patient was discharged 4 days after the procedure and was mobilized on crutches with partial weight bearing for 6 weeks.
Postoperatively, routine clinical and radiographic controls were performed after 1, 3, 6, 8, 12, and 24 months. Full weight bearing was allowed after 6 weeks, and the patient subsequently obtained a normal range of hip motion and was pain-free. By 3 months postoperatively, he had returned to his former activities of daily living and leisure, including work in his previous profession as a painter. Radiographic follow-up at 1, 6, 8, and 12 months indicated no signs of osteoporosis, loosening, AVN, or femoral neck fracture (). 2 years after the index procedure, the patient had no clinical symptoms but radiography indicated a discrete change in the position of the femoral component (.
3.5 years after the index procedure, the patient developed acute pain in the left groin and could not walk. There had been no trauma prior to this. A mildly displaced vertical fracture of the femoral neck adjacent to the rim of the femoral implant was found on plain radiography (. The revision procedure confirmed the diagnosis of femoral neck fracture. The femoral head fragment was stable in the component and no fibrous tissue or metallosis was found. The bony tissue remaining in the femoral component seemed non-vital and did not bleed upon manipulation. The cup was found to be stable, and the femoral component was revised to a conventional stemmed non-cemented prosthesis with a corresponding large-diameter metal head (CLS; Zimmer) (. Clinical and radiographic controls 4 months and 1 year postoperatively indicated no signs of loosening of the prosthesis. The patient returned to all of his previous activities within 3 months and he was satisfied at the latest follow-up (1 year after revision).
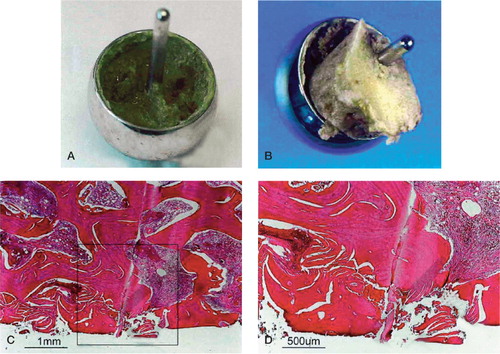
The retrieved femoral head component with surrounding tissue was analyzed macroscopically and microscopically. There were no findings of metallosis or osteoporosis. Histopathology showed the presence of necrotic bone with zones of non-vital bone in direct contact with the prosthesis shaft (), supporting the diagnosis of avascular necrosis.
Figure 2. A. Macroscopic view of the tissue in the femoral prosthetic component. B. Macroscopic view of the tissue in the prosthesis with the remaining part of the femoral neck. C. Histological analysis revealed zones of tissue with non-vital bone, where no vital osteocytes could be observed. The local bone necrosis was in direct contact with the stem of the prosthesis. D. Enlargement of the previous micrograph showing bony tissue without living cells.
Discussion
Novel techniques generate novel complications, and hip resurfacing has been reported to be associated with femoral neck fractures directly adjacent to the femoral implant (Australian Orthopaedic Association Annual Report 2007). Femoral neck fractures after hip resurfacing have previously been thought of as early complications that typically occur within the first 6 months. Here we report that this complication can also occur after much longer periods—in the case of our patient, 3.5 years after resurfacing.
Two main modes of failure of the femoral component have been pointed out as principal reasons for early revision after hip resurfacing: femoral neck fracture and aseptic loosening of the femoral component, with fractures being considered the more common complication. The incidence of femoral neck fracture as a complication after metal-on-metal resurfacing hip arthroplasty is assumed to be less than 2% (Table). Numerous theories have been developed in order to explain the occurrence of this complication, some indicating surgical factors related to the resurfacing procedure as such, and some focusing on patient-related factors.
Reports of femoral neck fractures after resurfacing arthroplasty of the hip. References have been sorted by the mean time to fracture, in ascending order
Some authors have proposed that the risk of femoral neck fracture is something that is inherent in the entire concept of resurfacing, because the epiphyseal blood supply to the remaining femoral head and neck is thought to be compromised by the procedure. A number of studies substantiate this hypothesis: retrieval studies on femoral heads after failed hip resurfacing have shown evidence of AVN under the femoral component, which may play a part in the development of fractures in the femoral neck region (Little et al. Citation2005, Campbell et al. Citation2006). It has been suggested that excessive reaming of the femur prior to resurfacing, thermal injury during cement polymerization, or cement penetration could all compromise epiphyseal vascularity and bone viability (Amstutz et al. Citation2004b, Little et al. Citation2005, Morlock et al. Citation2006, Gill et al. Citation2007).
One possible contributory factor to this proposed disruption of the epiphyseal blood supply is sur-gery-related damage to the retinacular vessels at the femoral head-neck junction. It has been shown that oxygen concentrations in the femoral head are instantly reduced by two-thirds when the external rotators are divided during a posterior approach in hip resurfacing, and in about one-third of the patients investigated the femoral head appeared to have remained completely avascular at the end of the procedure (Steffen et al. Citation2005).
Any possible damage to vessels important for epiphyseal blood supply could be a function of the type of surgical approach. Indeed, the posterior approach—with the risk of interfering with epiphyseal blood supply by dividing crucial branches of the medial circumflex artery—appears to be a risk factor for the failure of hip resurfacing (Steffen et al. Citation2005, Beaule et al. Citation2006, Khan et al. Citation2007), even though excellent outcomes have also been reported after this approach (Daniel et al. Citation2004). It has been hypothesized that anterolateral approaches such as the one described by Hardinge may be less prone to inducing such serious reductions in femoral head blood supply. A study using measurement of cefuroxime concentrations in bone as an indirect measure of femoral head perfusion showed that cefuroxime levels in the femoral head were significantly lower during the posterior approach than during an anterolateral transgluteal approach (Khan et al. Citation2007). Other surgical risk factors for femoral neck fracture after hip resurfacing are notching of the femoral neck and varus alignment, or inadequate seating of the femoral component (Amstutz et al. Citation2004b, Beaule et al. Citation2004b, Long and Bartel Citation2006, Anglin et al. Citation2007, Radcliffe and Taylor Citation2007).
Apart from these surgical factors, there are a number of patient-related factors that seem to increase the risk of revision following hip resurfacing. Data from the Australian joint replacement registry and investigations on smaller series have indicated that higher age and female sex are significant risk factors for revision, and a high body mass index also appears to contribute to early failure (Shimmin and Back Citation2005, Siebel et al. Citation2006, Australian Orthopaedic Association Annual Report 2007). Furthermore, injuries of the hip joint such as previous surgery due to trauma or pediatric disease, and also circulatory diseases such as AVN of the femoral head, have been implicated as additional risk factors. Bone quality in the femoral head and neck is also closely associated with the success of the hip resurfacing (Amstutz et al. Citation2004a, Schmalzried et al. Citation2005).
Most femoral neck fractures after hip resurfacing occur early, usually within the first 6–8 weeks (Table). The largest survey of this complication was published by Shimmin and Back (Citation2005), who described 50 femoral neck fractures in a nationwide cohort of 3,497 patients in Australia. In these cases, the mean time to fracture was 3.5 months, with the latest fracture occurring after 14 months. The literature available on the subject of femoral neck fracture after hip resurfacing indicates that this complication does not usually occur more than 2 years after the index procedure.
In retrospect, the discrete varus tilting of the femoral component observed in our patient after 2 years was probably an early indicator of AVN and subsequent femoral neck fracture, but at the time the patient was free of symptoms and physically active, both in his profession and during leisure. Clinical symptoms in the form of thigh pain did not become manifest before a total of 3.5 years had elapsed, which corresponds to the radiographically visible development of a femoral neck fracture. The report of successful closed management of periprosthetic femoral fractures after resurfacing seems to support our decision of expectancy at the follow-up after 2 years (Cossey et al. Citation2005).
It is difficult to determine the sequence of pathophysiological events that leads to periprosthetic fracture after resurfacing. We propose that surgery-induced AVN of the remaining femoral neck may be the primary event, after which either fracture or aseptic loosening of the femoral component, or both, occur(s) (). This hypothesis has been strengthened by the retrieval of the failed femoral component and ensuing microscopic investigation performed in our patient.
Figure 3. Avascular necrosis can lead to either femoral neck fracture or loosening, or both. Trauma can be an independent cause for femoral neck fractures.
In summary, in this report we present a most unusual case of femoral fracture after hip resurfacing 3.5 years after the index procedure, without the existence of putative risk factors such as advanced age, female sex, femoral neck notching, osteoporosis, posterior surgical approach, or varus positioning of the femoral component. We conclude that the risk of femoral neck fracture after hip resurfacing can be present also in the medium term. We thus counsel our patients accordingly, and recommend a systematic long-term follow-up of all resurfacing patients, even those without any risk factors.
- Amstutz H C, Beaule P E, Dorey F J, Le Duff M J, Campbell P A, Gruen T A. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg (Am) 2004a; 86(1)28–39
- Amstutz H C, Campbell P A, Le Duff M J. Fracture of the neck of the femur after surface arthroplasty of the hip. J Bone Joint Surg (Am) 2004b; 86(9)1874–7
- Anglin C, Masri B A, Tonetti J, Hodgson A J, Greidanus N V. Hip resurfacing femoral neck fracture influenced by valgus placement. Clin Orthop 2007, 465: 71–9
- Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA; 2007
- Back D L, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings. An independent prospective study of the first 230 hips. J Bone Joint Surg (Br) 2005; 87(3)324–9
- Beaule P E, Le Duff M, Campbell P, Dorey F J, Park S H, Amstutz H C. Metal-on-metal surface arthroplasty with a cemented femoral component: a 7-10 year follow-up study. J Arthroplasty (Suppl 3) 2004a; 19(8)17–22
- Beaule P E, Lee J L, Le Duff M J, Amstutz H C, Ebramzadeh E. Orientation of the femoral component in surface arthroplasty of the hip. A biomechanical and clinical analysis. J Bone Joint Surg (Am) 2004b; 86(9)2015–21
- Beaule P E, Campbell P A, Hoke R, Dorey F. Notching of the femoral neck during resurfacing arthroplasty of the hip: a vascular study. J Bone Joint Surg (Br) 2006; 88(1)35–9
- Campbell P, Beaule P E, Ebramzadeh E, LeDuff M, De Smet K, Lu Z, Amstutz H C. The John Charnley Award: a study of implant failure in metal-on-metal surface arthroplasties. Clin Orthop 2006, 453: 35–46
- Cossey A J, Back D L, Shimmin A, Young D, Spriggins A J. The nonoperative management of periprosthetic fractures associated with the Birmingham hip resurfacing procedure. J Arthroplasty 2005; 20(3)358–61
- Daniel J, Pynsent P B, McMinn D J. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg (Br) 2004; 86(2)177–84
- Gill H S, Campbell P A, Murray D W, De Smet K A. Reduction of the potential for thermal damage during hip resurfacing. J Bone Joint Surg (Br) 2007; 89(1)16–20
- Hardinge K. The direct lateral approach to the hip. J Bone Joint Surg (Br) 1982; 64(1)17–9
- Khan A, Yates P, Lovering A, Bannister G C, Spencer R F. The effect of surgical approach on blood flow to the femoral head during resurfacing. J Bone Joint Surg (Br) 2007; 89(1)21–5
- Little C P, Ruiz A L, Harding I J, McLardy-Smith P, Gundle R, Murray D W, Athanasou N A. Osteonecrosis in retrieved femoral heads after failed resurfacing arthroplasty of the hip. J Bone Joint Surg (Br) 2005; 87(3)320–3
- Long J P, Bartel D L. Surgical variables affect the mechanics of a hip resurfacing system. Clin Orthop 2006, 453: 115–22
- McMinn D, Treacy R, Lin K, Pynsent P. Metal on metal surface replacement of the hip. Experience of the McMinn prothesis. Clin Orthop 1996, 329 Suppl: S89–98
- Morlock M M, Bishop N, Ruther W, Delling G, Hahn M. Biomechanical, morphological, and histological analysis of early failures in hip resurfacing arthroplasty. Proc Inst Mech Eng [H] 2006; 220(2)333–44
- Radcliffe I A, Taylor M. Investigation into the effect of varus-valgus orientation on load transfer in the resurfaced femoral head: a multi-femur finite element analysis. Clin Biomech (Bristol, Avon) 2007; 22(7)780–6
- Schmalzried T P, Silva M, de la Rosa M A, Choi E S, Fowble V A. Optimizing patient selection and outcomes with total hip resurfacing. Clin Orthop 2005, 441: 200–4
- Shimmin A J, Back D. Femoral neck fractures following Birmingham hip resurfacing: a national review of 50 cases. J Bone Joint Surg (Br) 2005; 87(4)463–4
- Siebel T, Maubach S, Morlock M M. Lessons learned from early clinical experience and results of 300 ASR hip resurfacing implantations. Proc Inst Mech Eng [H] 2006; 220(2)345–53
- Steffen R T, Smith S R, Urban J P, McLardy-Smith P, Beard D J, Gill H S, Murray D W. The effect of hip resurfacing on oxygen concentration in the femoral head. J Bone Joint Surg (Br) 2005; 87(11)1468–74
- Treacy R B, McBryde C W, Pynsent P B. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg (Br) 2005; 87(2)167–70