Abstract
Background Childhood hip disorders including acetabular dysplasia, congenital hip dislocation, epiphysiolysis, and morbus Calvé-Legg-Perthes are well-established risk factors for the development of early osteoarthritis of the hip. These patients have an increased risk of undergoing a total hip arthroplasty (THA) operation early in their life. However, there are very few data on implant survival in such patients.
Methods We used data from the Danish Hip Arthroplasty Registry to identify patients who had been treated with a primary THA in Denmark between 1995 and 2005. Implant survival during early and late postoperative follow-up (< 6 months and>6 months, respectively) was assessed for patients treated with a primary THA due to childhood hip disorders, and compared with implant survival for THA patients with primary osteoarthritis.
Results 56,087 THA procedures included 53,694 (96%) hips with primary osteoarthritis, 890 (1.6%) with acetabular dysplasia, 565 (1.0%) with congenital hip dislocation, 267 (0.5%) with epiphysiolysis, and 404 (0.7%) hips with morbus Calvé-Legg-Perthes
Patients with acetabular dysplasia had an increased risk of revision during the 0–6-month postoperative period compared to patients with primary osteoarthritis (adjusted relative risk (RR)=1.9 (95% CI: 1.2–3.1)). These revisions were mainly performed due to dislocation of the THA, providing an adjusted RR of revision due to dislocation of 2.8 (95% CI: 1.6–4.9) compared to patients operated due to primary osteoarthritis. We found no statistically significant differences in risk of revision for the other childhood hip disorder groups during the early postoperative phase. In addition, we found no substantial differences in revision risk during later follow-up (0.5–12 years) for any of the childhood hip disorders compared to patients with primary osteoarthritis.
Interpretation We found an encouraging rate of long-term implant survival for patients with childhood hip disorders. The major concern is the increased risk of revision because of dislocation in the first 6 postoperative months for patients with acetabular dysplasia. However, the advent of alternative bearings and the use of large-diameter femoral heads may improve the outcome after primary THA in these patients.
Patients with childhood hip disorders represent a minority group among patients treated with total hip arthroplasty (THA). In the Danish Hip Arthroplasty Register (DHR), 4.3% of THAs have been performed due to these hip disorders (John-sen et al. 2006). Previous reports have concluded that primary THA provides good clinical results regarding function and pain relief in patients with pediatric hip disorders (Sochart and Porter Citation1997). However, the altered anatomy in patients with childhood hip disorders makes the THA surgery technically demanding. To provide valid implant survival studies on each single childhood hip disorder, it is therefore necessary to conduct large reg-ister-based cohort studies. Previous studies have mainly focussed on the long-term results, although measures to prevent revision may differ during short- and long-term follow-up.
In a previous study from the DHR, childhood hip disorders were found to be a predictor of short-term implant failure after primary THA, with a 2.6-fold increased relative risk of revision during the first postoperative month (Johnsen et al. Citation2006). No increased risk of implant failure was found during long-term follow-up. However, acetabular dysplasia, congenital hip dislocation, epiphysiolysis, and morbus Calvé-Legg-Perthes were combined into one group in that study and information on revision risk was therefore not available on the individual childhood hip disorders.
We therefore assessed the short- and long-term implant survival in patients with acetabular dysplasia, congenital hip dislocation, epiphysiolysis, and morbus Calvé-Legg-Perthes and compared the results with corresponding data for patients with primary osteoarthritis.
Patients and methods
Sources of data
The Danish Hip Arthroplasty Registry (DHR). The DHR is a nationwide clinical database that was established January 1, 1995 with the purpose of improving the monitoring and quality of both primary and revision total hip arthroplasty surgery in Denmark (Lucht Citation2000). All 45 orthopedics departments report to the register, including 8 departments located in private hospitals. Registration of primary THA and revisions is compulsory. Pre-, intra-, and postoperative data are collected prospectively using standardized forms. The intraoperative data are filled in by the operating surgeon immediately after surgery. The DHR was recently validated and the quality of the data was found to be high (Pedersen et al. Citation2004).
The National Registry of Patients (NRP). The NRP, which was established in 1977 (Andersen et al. Citation1999), records information on all discharges from public somatic hospitals in Denmark. The NRP contains information on dates of admission and discharge, and discharge diagnoses according to the International Classification of Diseases (eighth revision (ICD-8) until the end of 1993; tenth revision (ICD-10) thereafter). All discharge diagnoses are assigned by the physician who discharges the patient. Using the NRP, it is possible to construct the complete inpatient history of each patient.
The Civil Registration System (CRS). A unique personal identification number is given to all Danish citizens at birth or according to their date of birth. The CRS records information on changes in vital status of all Danish citizens, including changes of address, date of emigration, and since 1968) the date of death. Accurate linkage between the public Danish registers is possible at the level of individual patients using the personal identification number. Thus, we used the personal identification number to merge data from the DHR, the NRP, and the CRS.
Study population
From the DHR, we identified all primary THA procedures performed in Denmark between January 1, 1995 and December 31, 2006 due to primary osteoarthritis, acetabular dysplasia, congenital hip dislocation, epiphysiolysis, and morbus Calvé-Legg-Perthes (n=56,139). We excluded 32 patients who lived in Greenland or who had changed their personal identification number and therefore could not be properly followed up, and 20 patients with an incorrect revision date or missing indication for revision. Thus, 56,087 primary THA procedures were available for further analysis, including 18,234 bilateral procedures.
Outcomes
The primary outcome was time to revision for any reason, defined as a partial or complete removal or exchange of the components. Conditions not requiring removal or exchange of the components were not included (e.g. open or closed reduction, femoral osteosynthesis, open surgery due to deep or superficial infection, and operations due to wound problems). Follow-up started on the day of primary THA and ended on the day of revision, death, emigration, or on December 31, 2006, whichever came first. The follow-up after primary THA was divided into 2 periods. The initial period commenced on the day of surgery and continued until a revision was performed, or to 6 months after surgery. If patients had not undergone revision in the initial period, they were included in the second period, which extended until the end of follow-up. Secondary outcomes included the indication for revision and the duration of surgery according to diagnosis for primary THA. The average follow-up time was 4.6 years (range: 1 day to 12 years).
Covariates
We included sex, age, fixation technique, intraoperative complications, and co-morbidity as covariates. Age at the time of primary THA was divided into 5 groups: 10–49 years, 50–59, 60–69, 70–79, and≥80 years. Fixation technique was divided into 3 main categories: cemented, uncemented, and hybrid (hybrid A: uncemented acetabular component and cemented femoral component; hybrid B: cemented acetabular component and uncemented femoral component). Co-morbidity at the time of surgery was assessed with the Charlson co-morbid-ity index (Charlson et al. Citation1987). The index includes 19 major disease categories, translated into corresponding ICD-8 and ICD10 hospital discharge codes used in the NRP. The Charlson co-morbidity score applies a weighting of 1, 2, 3, or 6 points to each of the 19 disease categories and is then summated. We separated the patients into 3 levels: low-index (0), corresponding to patients with no previously recorded disease categories in the co-morbidity index; medium-index (patients with 1 or 2 disease categories); and high-index (patients with more than 2 disease categories). We also assessed the distribution of femoral head diameter, which has been available since January 1, 1997 and which was known for 92% of cases.
Statistics
The patients were divided into 5 study groups according to primary diagnosis for THA (primary osteoarthritis, acetabular dysplasia, congenital hip dislocation, epiphysiolysis, and morbus Calvé-Legg-Perthes), and we defined patients with primary osteoarthritis as being the reference group. We constructed cumulative implant failure curves for THA prostheses. Cox's proportional hazards regression analysis was used to compute hazards ratios as a measure of the relative risks (RRs) and 95% confidence intervals for each diagnosis for primary THA, compared with primary osteoarthritis as a reference. Adjusted RRs were controlled for age, sex, fixation technique, and co-morbidity. The Cox proportional hazards model was found suitable after applying log-log plots and Schoenfeld residuals. The hips were analyzed as independent observations, as described by Lie et al. (Citation2004). We calculated p-values using the t-test, and qq-plots were assessed to test for normal distribution. All analyses were calculated using the Stata statistical software package, release 9.0 (Stata Corporation, College Station, Texas).
Results
The 56,087 THA procedures included 53,694 patients (96%) with primary osteoarthritis, 890 (1.6%) with acetabular dysplasia, 563 (1.0%) with congenital hip dislocation, 267 (0.5%) with epiphysiolysis, and 404 patients (0.7%) with morbus Calvé-Legg-Perthes (). The operation time was longest in patients with congenital hip dislocation (median 103 min) compared to the reference group (primary osteoarthritis, median 81 min) (p<0.001).
Table 1. Characteristics of the patients undergoing primary THA between January 1, 1995 and December 31, 2006 who were registered in the Danish Hip Arthroplasty Registry
In general, patients with childhood hip disorders were younger and healthier than patients with primary osteoarthritis. In more than 80% of cases, they were treated with either a hybrid or an uncemented prosthesis. In comparison, 54% of patients with primary osteoarthritis were treated with a cemented prosthesis. In all groups, femoral head diameters of 28–30 mm were used most frequently. 18% of patients with acetabular dysplasia were treated with a femoral head larger than 30 mm, as compared to 8% of patients with primary osteoarthritis ().
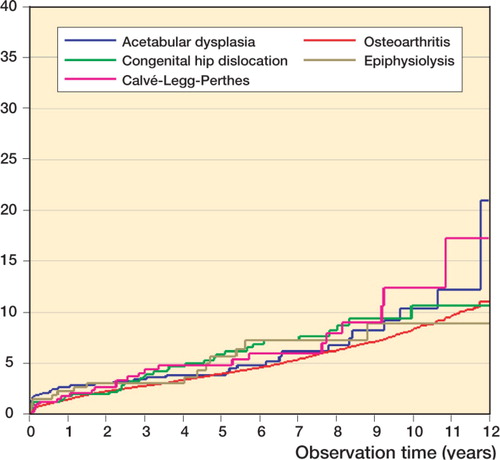
The cumulative implant failure rates for the childhood hip disorders were higher than for primary osteoarthritis. The 10-year failure rates for patients who were operated for primary osteoarthritis were 8.7% (95% CI: 8.2–9.2), 11% (95% CI: 7–27) for acetabular dysplasia, 11% (95% CI: 7.5–17) for congenital hip dislocation, 9.3% (95% CI: 5.2–17) for epiphysiolysis, and 13% (95% CI: 9.4–37) for morbus Calvé-Legg-Perthes.
In the initial 0–6-month follow-up period, the adjusted RR for revision in patients with acetabular dysplasia was 1.9 (95% CI: 1.2–3.1) compared with primary osteoarthritis (). The other childhood hip disorders were not associated with an increased RR for revision within the first 6 months after primary THA. In all 5 study groups, the main reason for revision surgery in this period was dislocation (). However, three-quarters (14/19) of the acetabular dysplasia patients underwent revision due to dislocation whereas 54% (303/563) of the primary osteoarthritis patients underwent revision surgery due to dislocation, within the first 6 postoperative months. This represents an adjusted RR for revision due to dislocation of 2.8 (95% CI: 1.6–4.9) for patients with acetabubecause lar dysplasia in the 6-month follow-up period compared with patients who were operated for primary osteoarthritis. All patients in the acetabular dysplasia group who were revised because of dislocation were treated with a femoral head size of 28 mm. No statistically significant differences were found for revisions done for ther reasons when comparing patients with individual childhood hip disorders with those with primary osteoarthritis.
Table 2. Relative risk of revision after primary THA due to childhood hip disorders compared to that for primary osteoarthritis during early (0–0.5 years) and late (0.5–12 years) postoperative follow–up
In the 6-month to 12-year follow-up period, the crude RR for revision in the congenital hip dislocation patients was 1.3 (95% CI: 1.0–1.9), indicating an increased risk of revision (). However, there were no apparent differences in the RR estimates among the diagnoses for primary THA after adjusting for potential confounding (adjusted RR = 1.0 (95% CI: 0.7–1.5)). 3 of 24 revisions in the acetabular dysplasia group had been performed because of aseptic loosening of the acetabular component, or of both implant components. In contrast, patients in the primary osteoarthritis group were revised due to the same indications in 28% of cases (461/1,641) (). Otherwise, comparisons between the groups did not reveal any major differences in the indications for revision.
Table 3. Indications for revision, 0–6 months
Table 4. Indications for revision, 6 months to 11 years
Discussion
The strengths of our study are the availability of nationwide population-based data sources with high validity overall, and participation of many surgeons (Pedersen et al. Citation2004). The sources included detailed and prospectively collected data, which are rarely available—including laterality of both primary THAs and revisions—and the complete hospitalization history of each individual since 1977. The data sources were accurately linked using the personal identification number of each patient. Furthermore, compared to existing reports, our study population was relatively large.
Our study also has some limitations. Although a previous report from the DHR showed that the positive predictive values of diagnoses registered in the DHR were high (Pedersen et al. Citation2004), we cannot entirely exclude misclassification of diagnoses. On the other hand, we have no reason to believe that misclassification of diagnosis is differential, i.e. dependent on outcome. In addition, as in all observational studies, we cannot entirely exclude the possibility of residual confounding and unmeasured confounding (e.g. surgeon volume, the patient's use of medication and level of physical activity during follow-up, compliance with rehabilitation, measurement of hip abnormality). Lastly, parts of our analysis concerning RR estimates for specific indications for revision were inconclusive because there were too few observations.
Acetabular dysplasia
In this group of patients, the increased RR of revision in the 0–6-month follow-up period is of concern. These revisions were mainly performed due to dislocation. This finding has not been reported previously in the literature. However, it seems plausible because of the more difficult local anatomy of the acetabulum in these patients, which makes positioning of the acetabular component technically demanding. Also, patients with acetabular dysplasia often have extreme anteversion of the proximal femur, which governs the anteversion of the femoral component and thereby increases the risk of anterior dislocation.
In contrast, our findings regarding the long-term implant survival rates in patients with acetabular dysplasia are in accordance with the results of previous studies (MacKenzie et al. Citation1996, Sochart and Porter Citation1997, Gill et al. Citation1998, Furnes et al. Citation2001). Furnes et al. (Citation2001) reported comparable results in a cohort study based on data from the Norwegian Arthroplasty Register. As in the present paper, in comparing the long-term implant survival, these authors did not find any significant differences between acetabular dysplasia and primary osteoarthritis.
The major concern in THA surgery in patients with acetabular dysplasia has been high rates of revision due to aseptic loosening of the acetabular component, as reported by MacKenzie et al. (Citation1996) as well as Sochart and Porter (Citation1997). In these studies, surgery was performed between 1966 and 1982; however, there have been substantial improvements in both surgical technique and prosthetic design since then. Furthermore, our findings that 3 out of 43 of the revisions were due to aseptic loosening are not exactly comparable to the aforementioned studies because of the shorter follow-up period in our study compared to that of Sochart and Porter. These authors reported 25-year follow-up results and found an average time to revision of the acetabular component of 16 years. This may explain the low rates of revision due to aseptic loosening of the acetabular component in our study.
Congenital hip dislocation
Previous studies on THA operations performed between 1966 and 1994 have reported 10-year implant survival rates of between 83% and 97% in patients with congenital hip dislocation, compared to 89% in our study (Linde et al. Citation1988, Garvin et al. Citation1991, Sochart and Porter Citation1997, Hartofilakidis and Karachalios Citation2004). It may be most relevant to compare our findings with the study from the Norwegian Arthroplasty Register, as it also represents a large nationwide register-based cohort study. That register reported a 10-year survival rate of 82% for all patients with congenital hip dislocation, as compared to 91% if the patients were treated with a cemented Charley prosthesis (Furnes et al. Citation2001). This represented an increased RR of revision of 1.3 in patients with congenital hip dislocation compared to patients with primary osteoarthritis. Also, Furnes et al. reported an increased relative risk of revision due to dislocation in this group. We found a similar 10-year implant survival rate in our study; however, we found no increased risk of revision compared to patients with primary osteoarthritis. This may be somewhat surprising, as the anatomical changes in patients with congenital hip dislocations pose technical difficulties comparable to those in patients with acetabular dysplasia. Thus, we would have suspected an increased risk of revision in these patients.
Morbus Calvé-Legg-Perthes and epiphysiolysis
To our knowledge, there has been only one study on the prognosis after THA in patients with epiphysiolysis and morbus Calvé-Legg-Perthes, from the Norwegian Arthroplasty Register (Furnes et al. Citation2001). In that study, the 10-year survival rates for epiphysiolysis and morbus Calvé-Legg-Perthes were 81% (95% CI: 75–86%) and 96% (95% CI: 91–100) if the patients were treated with the cemented Charnley prosthesis. Comparison with patients treated with THA due to primary osteoarthritis revealed no differences in the RR estimates for revision after adjusting for confounders. We have confirmed these results in the present study, although the failure rates in our study were generally lower (at 9% and 13% for epiphysiolysis and morbus Calvé-Legg-Perthes, respectively).
In general, the patients were younger and healthier in the childhood hip disorder groups. Considering the high level of activity in such patients, we find the long-term implant survival in our study encouraging.
The major concern in our study is the increased risk of revision because of dislocation in the first 6 postoperative months for patients with acetabular dysplasia. Thus, initiatives aimed at reducing the risk of revision in the 6 months following THA should be considered in these patients, including increased awareness of the anatomical reconstruction, orientation of components, femoral offset, and restoration of leg length. We believe that the advent of alternative bearings such as metal-metal or ceramic-ceramic and the use of larger-diam-eter femoral heads may improve the stability and implant survival in THA surgery for these patients. In addition, custom-made femoral components may be preferable in order to obtain correct anteversion of the neck.
This study was supported by the Danish Rheumatism Association and the Orthopaedic Research Foundation in Aarhus. The authors thank Anders Riis (statistician) for support with statistics and Anne Hjelm (Secretary at the Danish Hip Arthroplasty Register).
No competing interests declared.
TMT, ABP, and SPJ: study design, data analysis, and manuscript preparation. KS: head of the research group, study design, and manuscript preparation
- Andersen T F, Madsen M, Jorgensen J, Mellemkjoer L, Olsen J H. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 1999; 46: 263–8
- Charlson M E, Pompei P, Ales K L, MacKenzie C R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–83
- Furnes O, Lie S A, Espehaug B, Vollset S, Engesaeter L B, Havelin L I. Hip disease and the prognosis of total hip replacements. J Bone Joint Surg (Br) 2001; 83: 57986, A review of 53,698 primary total hip replacements reported to the Norwegian Arthroplasty Register 1987-99
- Garvin K L, Bowen M K, Salvati E A, Ranawat C S. Long-term results of total hip arthroplasty in congenital dislocation and dysplasia of the hip. A follow-up note. J Bone Joint Surg (Am) 1991; 73: 1348–54
- Gill T J, Sledge J B, Muller M E. Total hip arthroplasty with use of an acetabular reinforcement ring in patients who have congenital dysplasia of the hip. Results at five to fifteen years. J Bone Joint Surg (Am) 1998; 80: 969–79
- Hartofilakidis G, Karachalios T. Total hip arthroplasty for congenital hip disease. J Bone Joint Surg (Am) 2004; 86: 242–50
- Johnsen S P, Sorensen H T, Lucht U, Soballe K, Overgaard S, Pedersen A B. Patient-related predictors of implant failure after primary total hip replacement in the initial, short- and long-terms: A nationwide Danish follow-up study including 36 984 patients. J Bone Joint Surg (Br) 2006; 88: 1303–8
- Lie S A, Engesaeter L B, Havelin L I, Gjessing H K, Vollset S E. Dependency issues in survival analyses of 55,782 primary hip replacements from 47,355 patients. Stat Med. 2004; 23: 3227–40
- Linde F, Jensen J, Pilgaard S. Charnley arthroplasty in osteoarthritis secondary to congenital dislocation or subluxation of the hip. Clin Orthop. 1988; 227: 164–171
- Lucht U. The Danish Hip Arthroplasty Register. Acta Orthop Scand. 2000; 71: 433–9
- MacKenzie J R, Kelley S S, Johnston R C. Total hip replacement for coxarthrosis secondary to congenital dysplasia and dislocation of the hip. Long-term results. J Bone Joint Surg (Am) 1996; 78: 55–61
- Pedersen A, Johnsen S, Overgaard S, Soballe K, Sorensen H T, Lucht U. Registration in the danish hip arthroplasty registry: completeness of total hip arthroplasties and positive predictive value of registered diagnosis and postoperative complications. Acta Orthop Scand 2004; 75: 434–41
- Sochart D H, Porter M L. The long-term results of Charnley low-friction arthroplasty in young patients who have congenital dislocation, degenerative osteoarthrosis, or rheumatoid arthritis. J Bone Joint Surg (Am) 1997; 79: 1599–617