Abstract
Background and purpose Periacetabular osteotomy is the treatment of choice in young adults with hip dysplasia. Patient morbidity and surgical outcome may depend on the choice of surgical approach. We compared the outcome of a new minimally invasive approach to that of the frequently used “classic” ilioinguinal approach.
Patients and methods We retrospectively evaluated our experience with the ilioinguinal and minimally invasive approaches, which were used in successive time periods at our institution between December 1998 and February 2007 (n=263). Intraoperative and early postoperative outcome factors together with analysis of hip joint survival were compared in well-defined study groups.
Results In the minimally invasive and ilioinguinal groups respectively, the median (interquartile range) intraoperative blood loss was 250 (200–350) mL and 500 (350–700) mL (p<0.001), the mean (95% CI) hemoglobin reduction was 2.0 (1.9–2.1) mmol/L and 2.5 (2.4–2.7) mmol/L (p<0.001), transfusion was required following 4% and 18% of the procedures (p<0.001), and the median (interquartile range) duration of surgery was 70 (60–75) min and 100 (80–120) min (p<0.001). Median (interquartile range) postoperative center-edge and acetabular index angles were 33˚ (30–36) and 2˚ (0–6), respectively, in the minimally invasive group and 31˚ (25–35) and 9˚ (1–14) in the ilioinguinal group. There were no cases of moderate or severe complications in the minimally invasive group and 3 cases of arterial thrombosis in the ilioinguinal group (3%). At follow-up of 5 years, the hip joint survival rates were 97% in the minimally invasive group and 93% in the ilioinguinal group.
Interpretation Given the accumulated experience of the surgeon, the outcome of the minimally invasive approach compares favorably with that of the ilioinguinal approach, and the results support continued use of the minimally invasive approach for periacetabular osteotomy. Using this approach, we did not encounter any complications and acetabular reorientation was not compromized.
Periacetabular osteotomy (PAO) is the joint-pre-serving treatment of choice in young adults with symptomatic hip dysplasia. In hip dysplasia there is insufficient acetabular coverage of the femoral head, and the surgical aim of PAO is to reorient the acetabulum to improve coverage and eliminate the pathological mechanics (Ganz et al. Citation1988, Søballe Citation2003, Jacobsen et al. Citation2006). This relieves pain and prevents development of early osteoarthritis, thus delaying or even preventing total hip replacement (Siebenrock et al. 1999, Peters et al. 2006, Garras et al. Citation2007).
Since the development of PAO (Ganz et al. Citation1988), several surgical approaches have been used. Most surgeons prefer the ilioinguinal or modified Smith-Petersen approaches (Hussell et al. Citation1999, Trumble et al. Citation1999, Søballe Citation2003, Pogliacomi et al. Citation2005). These “classical” approaches inflict an extensive amount of trauma on the tissues—and some involve detachment of muscles, such as the rectus femoris and sartorius. The type of surgical approach may affect the occurrence of complications, duration of surgery, intraoperative blood loss, transfusion requirements, and length of hospital stay (Davey and Santore Citation1999, Hussell et al. Citation1999, Trumble et al. Citation1999). Furthermore, the type of approach may affect the possibility of obtaining an optimal reorientation of the acetabulum, which is the cornerstone of PAO surgery. Given the possible impact on patient morbidity, there is a need to compare the potential benefits of a less invasive approach with those of a “classical” approach.
Table 1. Baseline characteristics
We have previously reported the technique, initial experience, and results of a new minimally invasive transsartorial approach for PAO (Troelsen et al. Citation2008a). The minimally invasive approach proved safe and was successful in minimizing tissue trauma without compromising the ability to obtain optimal reorientation of the acetabulum. However, this approach has not been compared with other surgical approaches.
The key research question was whether the minimally invasive approach produces an outcome similar to that of the previously used ilioinguinal approach. Accordingly, the specific aims were: (1) to compare intraoperative and early postoperative outcome factors of the ilioinguinal and minimally invasive approaches, and (2) to assess the medium-term hip joint survival after PAO surgery using each approach.
Patients and methods
All periacetabular osteotomies performed at our institution between December 1998 and February 2007 were registered in a database (n=450 procedures). In this study, we retrospectively assessed our experience with the ilioinguinal and minimally invasive approaches by means of database inquiry and evaluation of radiographic material. The ilioinguinal and minimally invasive approaches were used in successive time periods with no selection of patients. Before the procedures registered in the database, the senior author (KS) had practised on cadavers and had performed approximately 30 peri-acetabular osteotomies between October 1996 and December 1998 at another orthopedic facility. The minimally invasive approach was used from April 2003. The indications for surgery were symptomatic acetabular dysplasia, a center-edge (CE) angle of Wiberg of<25˚, a congruent hip joint, maintained range of motion, and preferably no or early signs of osteoarthritis (Tönnis grade 0–1). Only procedures performed with the senior author as the primary surgeon were included (n=349 procedures). To provide well-defined study groups, we excluded procedures performed on patients with dysplastic changes secondary to Legg-Calvé-Perthes disease (36), procedures including supplemental hip surgery (hardware removal and intertrochanteric osteotomy (21), procedures not performed using hypotensive anesthesia (14), and procedures performed using the modified Smith-Petersen approach (15). 263 procedures performed on 211 patients (174 of whom were females) comprised the study group. 98 procedures were performed using the ilioinguinal approach and 165 were performed using the minimally invasive approach. Of these 165 procedures, data from 94 procedures in 91 patients who were operated between April 2003 and August 2005 have previously been reported in a study using similar inclusion criteria (Troelsen et al. Citation2008a). Baseline characteristics of weight and sex showed no significant differences between groups, whereas the difference in age of 3.6 years was close to being statistically significant (p=0.05) (). The duration of follow-up ranged from 4.9 to 9.2 years in the ilioinguinal group and from 1.0 to 4.9 years in the minimally invasive group.
The following parameters were assessed and compared: intraoperative blood loss, hemoglobin reduction, transfusion requirements, duration of surgery, complications, length of hospital stay, acetabular reorientation achieved, and subsequent conversion to a total hip arthroplasty. Data available at database inquiry included: age, weight, sex, diagnosis, method of anesthesia, surgical approach, intraoperative blood loss, duration of surgery, supplementary surgery, complications, transfusion requirements, and length of hospital stay. Pre- and postoperative anteroposterior pelvic radiographs were taken routinely, as were blood specimens for determination of hemoglobin values pre- and postoperatively. Subsequent conversions to total hip arthroplasty in Danish hospitals were registered in the Danish Hip Arthroplasty Register.
Intraoperative blood loss was estimated from the contents of blood in suction bottles and swabs. The reduction in hemoglobin was calculated from the preoperative value and from the first available value on the first or second postoperative day. If transfusion was administered intraoperatively (3 patients), if patients had bilateral procedures (8), or if data were missing (3), the data were excluded from further analysis. Transfusion requirement was calculated as the total number of intraoperatively and postoperatively administered SAGM units. Duration of surgery was measured from the start of incision to closure of the skin. The occurrence of moderate and severe technical or neurovascular complications (injury to great vessels and nerves, arterial thrombosis, unintended fractures or extension of the osteotomy into the joint or through the posterior column, or deep infection) was available in the database. Length of hospital stay was calculated from the day of surgery to the day of discharge. In cases of long admissions due to severe or moderate complications, data were excluded from further analysis (3 patients). The degree of hip dysplasia preoperatively and the reorientation of the acetabulum achieved were assessed by measuring the center-edge (CE) angle of Wiberg (Citation1939) and the acetabular index angle of Tönnis (Citation1987) (). All angle assessments were performed by one observer (AT). If there was radiographic material missing (12 patients), or if it was of inferior quality (2), the data were excluded from further analysis. Procedures performed on foreign patients (13) were not available for analysis of hip joint survival. Weight data were missing for 9 patients. The data were complete for the remaining parameters.
Figure 1. This figure has been cropped from an anteroposterior pelvic radiograph and only the right hip is shown. A line of reference is constructed by drawing a line going through the most caudal points on the inferior ramus bilaterally. The center-edge angle of Wiberg is constructed by drawing a line perpendicular to the line of reference through the center of the femoral head, and another line from the center of the femoral head through the lateral limit of the sclerotic acetabular roof. The acetabular index angle of Tönnis is constructed by drawing 2 lines, both originating at the medial limit of the acetabular sclerotic roof. One line runs through the lateral limit of the acetabular sclerotic roof and another is drawn parallel to the line of reference.
Statistics
Normally distributed data are presented as means with 95% confidence intervals (CIs) and compared using a 2-sample t-test. Data that were not normally distributed are presented as median with interquartile range, and were compared using a 2sample Wilcoxon rank-sum (Mann-Whitney) test. For testing of differences in the proportion of procedures associated with transfusion requirements, Pearson's Chi-squared test was used. Kaplan-Meier survival analysis was performed with subsequent conversion to total hip arthroplasty as endpoint. The level of significance was set at p<0.05.
Surgical approaches
The ilioinguinal approach was used as previously described (Letournel Citation1993), but without lateral extension along the iliac crest. The skin incision extended from the anterior superior iliac spine, along the inguinal ligament, and terminated at the level of the pubic symphysis near the midline (). The inguinal ligament was incised, leaving the origins of the abdominal musculature and fascia attached to the proximal part of the split ligament. Further access was created by incising the iliopectineal fascia that separates the lacuna musculorum and lacuna vasorum. This allowed mobilization of the iliopsoas muscle which, combined with medial retraction of the external iliac vessels, allowed access to performance of the osteotomies through 2 windows—one medially and one laterally to the iliopsoas muscle.
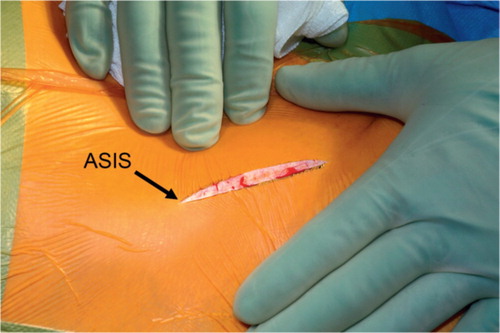
Figure 2. Lines of skin incisions for the ilioinguinal approach (blue line) and for the minimally invasive approach (red line) in relation to the bones. The anterior superior iliac spine (ASIS) is marked.
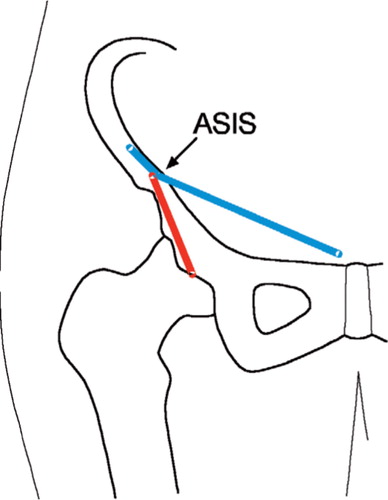
The surgical technique of the minimally invasive approach has been described previously in detail (Troelsen et al. Citation2008a). Briefly, an approximately 7-cm skin incision is made from the anterior superior iliac spine, running distally along the sartorius muscle ( and ). The lateral femoral cutaneous nerve is isolated and the inguinal ligament is cut at the attachment to the anterior superior iliac spine. The sartorius muscle is split in the direction of its fibers, the deep fascia of the muscle is cut, and to allow performance of the osteotomies the iliopsoas muscle and the medial part of the sartorius muscle are retracted medially. Due to limited direct visualization, it is necessary to use fluoroscopy when performing some of the osteotomies (Troelsen et al. Citation2008a). This is done to secure correct positioning of the osteotome to avoid unintended extension of the osteotomies.
Results
Clinical and radiographic outcome
Intraoperative blood loss, hemoglobin reduction, transfusion requirements, duration of surgery, and length of hospital stay were statistically significantly less in the minimally invasive group than in the ilioinguinal group (). When transfusion was required, a median of 2 blood units was transfused in both groups (). The preoperative measures of the CE angle and acetabular index angle showed that the dysplasia was slightly more pronounced in the ilioinguinal group. The reorientation of the acetabulum achieved, assessed by the CE angle, showed a difference between the ilioinguinal group (median 31˚, interquartile range: 25–35˚) and the minimally invasive group (median 33˚, interquartile range: 30–36˚) (p=0.006). The median acetabular index angle achieved in the minimally invasive group, 2˚ (interquartile range: 0–6˚), was statistically significantly different from that achieved in the ilioinguinal group (9˚; interquartile range: 1–14˚) (p<0.001) ().
Complications
In the ilioinguinal group there were 3/98 cases of arterial thrombosis, which occurred in April and May of 2000. The thrombosis occurred at the end of surgery or within a few hours postoperatively, and all patients received vascular intervention. One patient (a woman aged 49 years, a smoker) was subject to subsequent amputation at knee level; another (a man aged 33 years with Down's syndrome) had remaining loss of motor function and loss of sensation at the level of the ankle. The third patient (a woman aged 48 years) had no permanent injuries. In the latter case, thrombectomy was performed without delaying angiography and transfer of the patient.
In the minimally invasive group, there were no cases of moderate or severe neurovascular or technical complications.
Table 2. Clinical and radiographic outcome
Hip survival
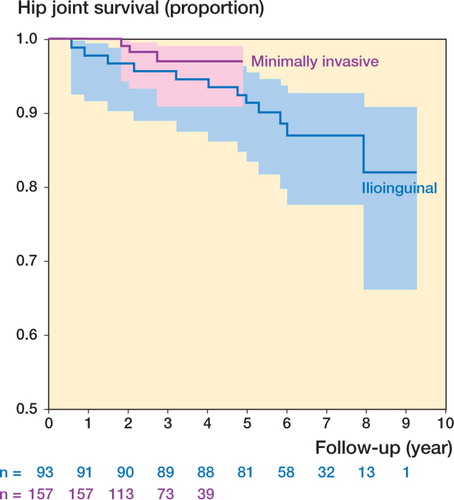
Kaplan-Meier analysis, with conversion to hip arthroplasty as the endpoint, showed a hip joint survival rate in the ilioinguinal group (93 procedures) of 93% (CI: 85–96%) at 4.9 years and of 82% (CI: 66–91%) at 9.2 years (range of follow-up: 4.9–9.2 years) (). There were 12 conversions to total hip arthroplasty at a median of 4.4 (0.6–7.9) years postoperatively.
In the minimally invasive group (157 procedures), the hip joint survival rate was 97% (CI: 91–99%) at 4.9 years (range of follow-up: 1.0–4.9 years) (). 3 hips were converted to total hip arthroplasty at 1.8, 2.0, and 2.7 years postoperatively.
Figure 4. Kaplan-Meier curves of hip joint survivorship following periacetabular osteotomy with conversion to total hip arthroplasty as the endpoint. The ilioinguinal group is blue and the minimally invasive group is red. The colored areas indicate the 95% confidence intervals of the survival rates. For every year of follow-up, the number of hip joints remaining in each group is given below the x-axis. Note that the y-axis does not start at zero.
Discussion
The choice of surgical approach for PAO may affect patient morbidity and surgical outcome (Davey and Santore Citation1999, Hussell et al. Citation1999, Trumble et al. Citation1999). Most surgeons prefer the ilioinguinal approach or the modified Smith-Petersen approach (Hussell et al. Citation1999, Trumble et al. Citation1999, Søballe Citation2003, Pogliacomi et al. Citation2005). However, these approaches cause an extensive amount of tissue trauma; thus, it is important to explore the potential benefits of a minimally invasive approach.
This study was performed as a retrospective database inquiry with no randomization of patients to the approaches used. Comparison of the approaches was done in large, well-defined study groups with no selection of patients, and the data used were collected prospectively.
The minimally invasive approach does not permit intraarticular surgical intervention. The approach can, however, be extended to make this possible. On the other hand, we have not found that intraarticular surgical intervention is necessary, and we have systematically avoided this when performing PAO surgery. Whether or not intraarticular exploration and intervention should be performed remains controversial. The medium- and long-term hip joint survival rates that we report in this study do not encourage us to change surgical strategy. In our department, labral pathology confirmed by MR arthrography is treated arthroscopically.
Intraoperative blood loss, hemoglobin reduction, transfusion requirements, and duration of surgery were statistically significantly lower in the minimally invasive group than in the ilioinguinal group. This may be attributed to the minimally invasive characteristics of the approach, but the accumulated experience of the senior author regarding every surgical aspect of PAO surgery may also have positively influenced the outcome of the minimally invasive approach. However, the low levels of intraoperative blood loss, hemoglobin reduction, transfusion requirements, and the short duration of surgery that we report in this study do not lead one to question the use of a minimally invasive approach in PAO surgery. Furthermore, this suggests that the minimally invasive characteristics are not confined to the length of the incision, but are also present during dissection and preparation for the osteotomies. In general, the results of the minimally invasive and ilioinguinal approaches in this study compare favorably with those in previous reports. There is great variation in the measures reported in the literature, with duration of surgery of approximately 2–3.5 hours and intraoperative blood loss of approximately 0.7–2 L being reported most frequently (Ganz et al. Citation1988, Davey and Santore Citation1999, Matta et al. Citation1999, Siebenrock et al. 1999, Trumble et al. Citation1999, Pajarinen and Hirvensalo Citation2003, Pogliacomi et al. Citation2005, Peters et al. 2006). However, in a previous study by Trousdale and Cabanela (Citation2003) the average intraoperative blood loss using a modified Smith-Petersen approach was 350 mL, which approximates the median blood loss of 250 mL that we found using the minimally invasive approach. The reduced median length of hospital stay in the minimally invasive group (7 days) compared to the ilioinguinal group (9 days) was not necessarily caused by the minimized tissue trauma, but may be attributable to general developments in reduction of length of hospital stay for surgical procedures of the hip. The length of hospital stay in both groups is similar to those reported by others (Matta et al. Citation1999, Pajarinen and Hirvensalo Citation2003, Pogliacomi et al. Citation2005).
Measured by the center-edge and acetabular index angles, the preoperative dysplasia was slightly but statistically significantly more pronounced in the ilioinguinal group than in the minimally invasive group. Together with the senior author's accumulated experience with acetabular reorientation, the differences—even though close to or confined to what can be attributed to measuring error (Troelsen et al. Citation2008b)—should be taken into consideration when interpreting the postoperative center-edge and acetabular index angles. Moreover, we have been using a measuring device for reliable intraoperative assessment of the center-edge and acetabular index angles since September 1999 (Troelsen et al. Citation2008b). The postoperative angle measurements in the minimally invasive group differ slightly (but statistically significantly) from those in the ilioinguinal group, and the median center-edge angle (33˚) and the acetabular index angle (2˚) achieved in the minimally invasive group imply that achieving optimal acetabular reorientation is not compromised by use of the minimally invasive approach. The postoperative center-edge and acetabular index angles in both the ilioinguinal and minimally invasive groups are similar to those reported in previous reports (Siebenrock et al. 1999, Peters et al. 2006, Garras et al. Citation2007).
The occurrence of arterial thrombosis when using the ilioinguinal approach has been described previously (Hussell et al. Citation1999). The vessels are exposed to both direct and indirect lesions, but retraction causing intimal damage is the most probable cause of thrombosis of the iliac or femoral arteries. The 3 cases that we observed in the ilioinguinal group occurred at a relatively early stage, suggesting that occurrence of this severe complication may also depend on the experience of the surgeon. To avoid permanent injuries, we recommend that clinical signs of arterial thrombosis should be reacted upon with acute surgical intervention, and with no delay caused by angiography or transfer of the patient to another surgical facility. Given the accumulated experience of the surgeon, the risk of neurovascular complications seems to have been eliminated when using the minimally invasive approach. Moderate and severe neurovascular complications following PAO surgery have been most frequently reported to occur at a rate of 0–5% using different surgical approaches (Trousdale et al. Citation1995, Matta et al. Citation1999, Trumble et al. Citation1999, Pogliacomi et al. Citation2005, Peters et al. 2006, Garras et al. Citation2007). The overall rate of moderate or severe technical or neurovascular complications is slightly higher, and the absence of these complications when using the minimally invasive approach compares favorably with the results of studies reporting outcome of PAO surgery including the initial experience with different surgical approaches.
Kaplan-Meier hip survival analysis has been performed in two previous studies, which reported survival rates of 80% at a follow-up of 5 years (Trousdale et al. Citation1995) and 7 years (Peters et al. 2006). The survival rate of 97% at a follow-up of 4.9 years in the minimally invasive group, and the survival rates in the ilioinguinal group of 93% and 82% at a follow-up of 4.9 years and 9.2 years, respectively, compares favorably with these reports. However, in these study groups concomitant femoral osteotomies were performed (Trousdale et al. Citation1995, Peters et al. 2006) and some patients were at advanced stages of osteoarthritis (Trousdale et al. Citation1995). The survival rates that we present here suggest that early and mid-term hip joint survival is not negatively affected when a minimally invasive approach is used. The increased awareness on the negative influence on outcome of advanced preoperative osteoarthritis (Trousdale et al. Citation1995, Siebenrock et al. 1999, Trumble et al. Citation1999) and other possible predictive factors will probably help to a better selection of patients leading to further improvement of the hip survival.
Given the accumulated experience of the surgeon, the intraoperative and early postoperative outcome of the minimally invasive approach compares favorably with that of the ilioinguinal approach, and the results support continued use of the minimally invasive approach. When using this approach, optimal acetabular reorientation is not compromised, and a good outcome is also suggested by the medium-term hip joint survival. One must pay attention to the risk of severe complications (i.e. arterial thrombosis) when using the ilioinguinal approach. We did not encounter any moderate or severe complications when using the minimally invasive approach. In general, PAO surgery is considered to be technically demanding. Using the minimally invasive approach requires, in our opinion, a good understanding of performing the osteotomies and reorienting the acetabulum. We therefore recommend that only surgeons with previous experience of the “classical” approaches should use the minimally invasive approach.
We thank Søren Johnsen, Alma Pedersen, and Frank Mehnert of the Department of Clinical Epidemiology, University of Aarhus, Denmark for their substantial contributions to development of the database and for their assistance in making the data accessible.
AT received funding from the Danish Rheumatism Association during conduction of this study.
No conflicts of interests declared.
The following authors designed the study (AT, BE, KS), collected the data (AT), analyzed the data (AT), wrote the manuscript (AT), and ensured the accuracy of the data and analysis (AT, BE, KS). All surgical procedures were performed by KS.
- Davey J P, Santore R F. Complications of periacetabular osteotomy. Clin Orthop 1999; 363: 21–32
- Ganz R., Klaue K., Vinh T S, Mast J W. A new periacetabular osteotomy for the treatment of hip dysplasias Technique and preliminary results. Clin Orthop 1988; 232: 26–36
- Garras D N, Crowder T T, Olson S A. Medium–term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg (Br) 2007; 89: 721–4
- Hussell J G, Mast J W., Mayo K A, Howie D W, Ganz R. A comparison of different surgical approaches for the peri–acetabular osteotomy. Clin Orthop 1999; 363: 64–72
- Jacobsen S., Rømer L., Søballe K. The other hip in unilateral hip dysplasia. Clin Orthop 2006; 446: 239–46
- Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop 1993; 292: 6276
- Matta M. J, Stover M D, Siebenrock K. Periacetabular osteotomy through the Smith–Petersen approach. Clin Orthop 1999; 363: 21–32
- Pajarinen J., Hirvensalo E. Two–incision technique for rotational acetabular osteotomy Good outcome in 35 hips. Acta Orthop Scand 2003; 74(2)133–9
- Peters C L., Erickson J A, Hines J L. Early results of the bernese periacetabular osteotomy: The learning curve at an academic medical center. J Bone Joint Surg (Am) 2006; 88: 1920–6
- Pogliacomi F., Stark A., Wallensten R. Periacetabular osteotomy. Good pain relief in symptomatic hip dysplasia., 32 patients followed for 4 years. Acta Orthop Scand 2005; 76(1)67–74
- Siebenrock K A., Scholl E., Lottenbach M., Ganz R. Bernese periacetabular osteotomy. Clin Orthop 1999; 363: 9–20
- Søballe K. Pelvic osteotomy for acetabular dysplasia. Acta Orthop Scand 2003; 74(2)117–8
- Troelsen A., Elmengaard B., Søballe K. A new minimally invasive transsartorial approach for periacetabular osteotomy. J Bone Joint Surg (Am) 2008a; 90: 493–8
- Troelsen A., Elmengaard B., Rømer L., Søballe K. Reliable angle assessment during periacetabular osteotomy with a novel device Clin Orthop. 2008b; 466: 1169–76
- Trousdale R T, Cabanela M E. Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop Scand 2003; 74(2)119–26
- Trousdale R T, Ekkernkamp A., Ganz R., Wallrichs S L. Peri–acetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg (Am) 1995; 77: 73–85
- Trumble S J, Mayo K A, Mast J W. The periacetabular osteotomy Minimum 2 year followup in more than 100 hips. Clin Orthop 1999; 363: 54–63
- Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Springer, BerlinGermany 1987
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Chir Scand 1939; 83(Suppl 58)5–135