Abstract
Background and purpose Correct positioning of the acetabular component is important in total hip arthroplasty (THA). We evaluated the effect of an imageless navigation system on the accuracy of cup positioning using a minimally invasive direct anterior approach.
Methods Hip replacements were performed in 44 cadaveric hips (22 cadavers) that were divided randomly into 2 groups. In the study group, THA was performed using an imageless navigation system. In the control group, no navigation system was used. CT scans were taken postoperatively. Using 3D reconstructions, the cup position was determined in relation to the frontal pelvic plane. The goal was to place each cup at 45° of inclination and 20° of anteversion, as recommended by the manufacturer.
Results In the navigated group, there was a statistically significantly smaller range of deviation from the target angles of inclination and anteversion relative to the control group.
Interpretation We conclude that imageless navigation improves the accuracy of cup placement in minimally invasive THA using the direct anterior approach.
In a previous cadaver study, we demonstrated that using an imageless navigation system allowed us to reduce the variability of cup placement (Nogler Citation2004). This was confirmed by the findings of others (Leenders et al. Citation2002, DiGioia et al. Citation2003, Parratte et al. Citation2007, Yu et al. Citation2007). This finding is important, because malpositioned acteabular components can result in dislocations, impingement, limited range of motion, and increased polyethylene wear (Parratte et al. Citation2007). It has been stated by some authors that the benefits of using a minimally invasive technique during total joint arthroplasty have not yet been proven (Bozic and Beriner 2007). However, others argue that the use of minimally invasive approaches combined with the development of new muscle-sparing techniques may be of benefit to the patient (Lin et al. Citation2007, Glaser et al. 2008). Although results using a cadaver model may not be directly applicable to a living patient, postoperative cup alignment can be represented with a good degree of accuracy by a cadaver model.
We have been using the direct anterior surgical approach to the hip for over 4 years. It is a true muscle-sparing approach that exposes the intermuscular plane between the sartorius and the tensor fascia latae muscles (Nogler Citation2004, Rachbauer Citation2005). We perform a single-incision approach using instruments designed with an offset, which helps to facilitate exposure and preparation of the acetabulum. All instruments have been designed to be navigable.
Having shown previously that navigation reduced the variability of acetabular cup positioning by means of an open surgical approach (Nogler et al. Citation2004), we hypothesized that a similar outcome would be obtained when using a minimally invasive direct anterior surgical approach.
Material and methods
We used 22 alcohol/glycerol-fixed human cadavers (13 female). The median BMI was 22 (20–28). All cadavers had a minimum hip flexion of 90°. The selection of specimens was based on their availability.
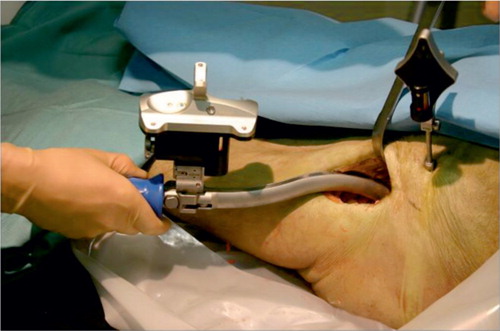
The sides for the navigated procedure and the manual procedure were identified using a computed randomization list. All cadavers were placed in supine position on a standard operating table. For reproducible determination of the frontal pelvic plane in the study group only, screws were drilled percutaneously into both superior iliac spines and both pubic tubercles. In all specimens, a minimally invasive direct anterior approach (DAA) to the hip joint was performed in which the space between the tensor fasciae latae and the sartorius muscle was used (). After opening and exposing the joint capsule, the femoral neck was osteotomized and the femoral head removed. The acetabulum was exposed using 4 retractors.
Figure 1. The muscular situation after skin incision. The index finger indicates the intermuscular plane between the sartorius and the tensor fasciae latae muscle (white arrows).

In the manual (control) group, reaming of the acetabulum and cup impaction were done immediately after exposure of the joint using standard hemispherical reamers. After reaching the correct size of reamer, a Trident hemispherical cup (Stryker Orthopaedics, Mahwah, NJ) was implanted using a curved cup impactor; no guidance tools of any kind were used for reaming or cup impaction.
For the navigated group, the device used was the Stryker Hip Navigation System with version 1.0 of the Hip Navigation Software (Stryker Leibinger, Freiburg, Germany) (). The specific geometric data of the instruments and implants were entered into the system software. In the navigated group, a pelvic tracker was mounted onto the iliac crest with a single tracker pin, and the frontal pelvic plane was detected by palpating the anterior superior iliac spine (ASIS) and pubic tubercles on both sides percutaneously using the navigation pointer. The depths of acetabulum, the articular surface, and the acetabular ring were each digitized using the navigation pointer. Reaming and cup impaction were performed under the constant guidance of the navigation device, which continuously displayed numerical values for anteversion and inclination of the cup. Our goal was to achieve 45° of inclination and 20° of anteversion for both groups.
Figure 2. Navigated cup placement with the navigation trackers mounted to the cup impactor and the pelvis.
After cup impaction, all specimens were CT-scanned. The CT settings used were 100 kV, 100 mA, rotation 0.8 sec, DFOV 15, noise index 20, and a slice thickness of 0.625 mm. The CT scanner used in the study was a General Electric Lightspeed 16 (GE Healthcare, WI). A 3D reconstruction of the pelvis was performed with HIP NAV Software (Stryker Leibinger, Freiburg, Germany) ().
Figure 3. Screen-capture image showing determination of the spatial orientation of the cup using the Stryker Hip Navigation System software.
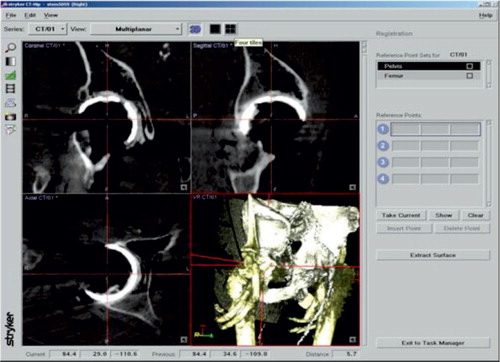
The frontal pelvic plane was used as a reference plane for orientation of the cup. 4 screws were placed on both ASIS and pubic turbercles in order to automatically define the frontal pelvic plane, which could then be reproduced precisely in CAT scans. The spatial orientation of the pelvis had no influence on cup anteversion or abduction. The coordinates of the head of the previously implanted screw in the pelvis were digitized, as were 3 points at the rim of the acetabular shells. Using these data, the pelvic plane, the cup entrance plane, and the angulations of these two planes were calculated.
Statistics
Statistical analysis was done using SPSS version 11.0. Non-parametric tests were used because the variables were not normally distributed. The differences between the groups were analyzed using Wilcoxon's matched pairs signed ranks test, which was chosen because it is the most commonly used non-parametric statistical method to analyze pairs of observations of continuous data, and the test requires independence between the individual pairs, but not within pairs. Equality of variances was proven by the Levene test. The results are expressed as median and interquartile range. The alpha level was set to 5%.
Results
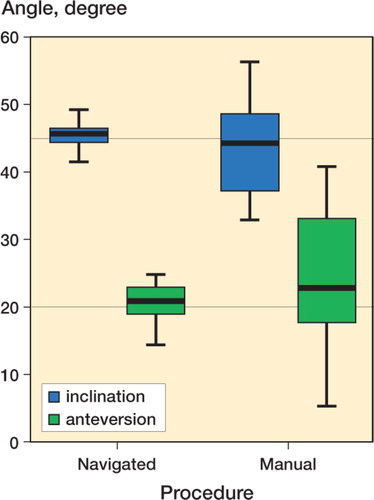
Postoperatively, it was possible to determine the two planes for all cups in all specimens. The variability of inclination and anteversion of the cup was smaller in the navigated cases than in the manual group (). A test of homogeneity, based on the median of variance of inclination and anteversion, showed highly significant deviations (p<0.001) between the navigated and manual procedures. The two groups showed significant differ- ences with regard to their deviation from the goal of 45° inclination and 20° anteversion (Table).
Figure 4. A box-and-whisker plot showing the results of cup inclination and anteversion in both groups. The heavy line is the median, contained in a box defined by the upper and lower quartiles, which is in turn contained in whiskers within which the central 95% of the ordered observations lie.
Discussion
Implant placement with a navigation system that orientates itself according to anatomical landmarks aims to improve the control that the surgeon has on implant position. The effectiveness of using a navigation system has been reported in several publications (Leenders et al. Citation2002, Nogler et al. Citation2004, Yu et al. Citation2007). This type of navigation system imitates manual guidance systems that orientate themselves with respect to the pelvic entrance plane. However, it attempts to achieve lower variance by measuring the entrance plane at the start of the procedure, so the measurements are available throughout the surgery whenever navigated tools are used for reaming or cup impaction.
The direct anterior approach to total hip arthroplasty has been used by several institutions for some time (Kennon et al. Citation2004, Matta et al. Citation2005). We have standardized the technique and developed specific instruments to accommodate the approach in a better way (Nogler Citation2004, Rachbauer Citation2005). This approach does not concentrate on a short skin incision but is truly intermuscular, because it uses a natural interval that provides direct access to the hip joint. Thus, the space in which the surgery has to be performed is defined by the anatomy of each patient.
As demonstrated in our previous study (Nogler et al. Citation2004), navigation can reduce the variability of cup positioning with an open surgical approach. Thus, we anticipated a similar reduction in variability in the positioning of a cup implanted using the direct anterior approach. The results reported here confirm this hypothesis. A cadaver study was used to permit precise measurement, something that can be achieved when anatomical landmarks are marked with screws for later CT-based identification. The use of cadavers also reduced the effect of other intervening factors such as bleeding, the effects of drapes, time pressure, and muscle tension.
For consistency, only one surgeon performed these implantations. That surgeon was not blinded to the technique used during implantation and during the postimplantation measurements. As we only used a cadaver model, only cup orientation could be measured. We assume that cup orientation is truly representative of the actual cup position even though it measures rotation only, and not translation. The cadavers used in this study were not surgically draped; nor were any of them extremely obese. Thus, we could only approximate the results that might be achieved during actual clinical procedures.
No competing interests declared.
ME performed the statistical analysis. EM and MT performed experimental set-up, the cup implantations, the CT scans, the measurements, analysis and interpretation of the results, and they wrote early drafts of the manuscript. MK and MN developed the hypothesis, designed the experimental set-up, and edited the manuscript.
- Bozic K J, Beringer D. Economic considerations in minimaly invasive total joint arthroplasty. Clin Orthop 2007; 463: 20–5
- DiGioia A M, Plakseychuk A Y, Levison T J, Jaramaz B. Mini-incision technique for total hip arthroplasty with navigation. J Arthroplasty 2003; 18(2)123–8
- Glaser D, Dennis D A, Komistek R. D, Miner T M. Clinical biomechanics award. Clin Biomech 2007, In vivo comparison of hip mechanics for minimally invasive versus traditional total hip arthroplasty, 2008 (in press)
- Kennon R, Keggi J, Zatorski L E, Keggi K J. Anterior approach for total hip arthroplasty: beyond the minimally invasive technique. J Bone Joint Surg (Am) 2004; 86(Suppl 2)91–7
- Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: a prospective and randomized study. Comput Aided Surg 2002; 7(2)99–106
- Lin D H, Jan M H, Liu T K, Lin Y F, Hou S M. Effects of anteriolateral minimally invasive surgery in total hip arthroplasty on hip muscle strength., walking speed., and functional score. J Arthroplasty 2007; 22(8)1187–92
- Matta J M, Shahrdar C, Ferguson T. Single-incision anterior approach for total hip arthroplasty on an orthopaedic table. Clin Orthop 2005; 441: 115–24
- Nogler M. Navigated minimal invasive total hip arthroplasty. Surg Technol Int. 2004; 12: 259–62
- Nogler M, Kessler O, Prassl A, Donnelly B, Streicher R, Sledge J B, Krismer M. Reduced variability of acetabular cup positioning with use of an imageless navigation system. Clin Orthop 2004; 426: 159–63
- Parratte S, Argenson J N, Flecher X, Aubaniac J M. Com-puter-assisted surgery for acetabular cup positioning in total hip arthroplasty: comparative prospective randomized study. Rev Chir Orthop Reparatrice Appar Mot 2007; 93(3)238–46
- Rachbauer F. Minimally invasive total hip arthroplasty via direct anterior approach. Orthopade. 2005; 34(11)1103–10
- Yu Z L, Wang L, Gui J. Accuracy improvement of acetabular component placement using non-image based surgical navigation system. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2007; 21(10)1057–61