A 4-year-old girl was hit by car, as a pedestrian, and sustained a right distal fracture of the femur. Radiographs showed a dislocated distal femoral fracture without any apparent involvement of the physis (). The fracture was treated by closed reduction and percutaneous fixation with 2 Kirschner wires from laterally. One of the wires crossed the physeal growth plate laterally and anteriorly (). The transphyseal wire was drilled in one single attempt. The Kirschner wires were removed after 3 weeks, and a cast was kept for 5 weeks at which time radiographs indicated healing of the fracture. After this, full weight bearing was initiated gradually.
Figure 2. Percutaneous Kirschner-wire fixation, with one wire crossing the physeal plate anteriorly and laterally.
At the age of 12 years, the patient was referred to our hospital due to an increasing deformity in her right lower extremity (). Plain radiographs of her right knee showed a bony physeal bridge laterally and anteriorly in the distal femoral physis (), which was confirmed by MR imaging ().
Figure 3. Patient at the age of 12 years, with developing valgus deformity and shortening of the right lower extremity.
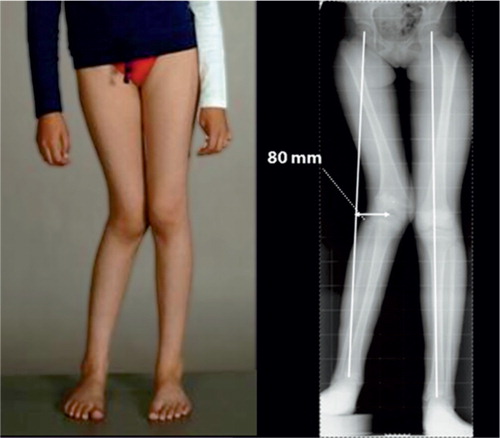
The patient was examined further in our hospital with standard 2-plane standing radiographs using long cassette exposures. The mechanical axis deviation was 80 mm laterally compared to the normal limb (). Deformity parameters were: 30 mm shortening, 20° valgus, and 20° recurvation. Rotational measures as assessed by CT were normal. At the time of surgery in our hospital, the patient had a skeletal age of 12 years and 4 months while the chronological age was 11 years and 7 months. The remaining growth in the affected physis was calculated to be 15 mm (Anderson et al. Citation1963) and the leg length discrepancy (LLD) at maturity was predicted to be 45 mm.
We performed an epiphysiodesis of the remaining intact part of the injured growth plate in the distal femur using percutaneous technique (Bowen and Johnson Citation1984). At the same time, a preoperatively fitted Taylor Spatial Frame was applied and a metaphyseal osteotomy in the distal femur was performed close to the physis. After 7 days, gradual correction was initiated with a lengthening rate of 1 mm per day. All deformity parameters were fully corrected, with the mechanical axis passing exactly through the center of the knee ().
Discussion
Injuries to the growth plate are most frequently caused by trauma or infection, or they can be iatrogenic as a result of surgery. Fractures of the long bones in the lower extremity with involvement of the physis are common injuries in children and adolescents (Mizuta et al. Citation1987, Mann and Rajmaira Citation1990, Peterson et al. Citation1994,). There are several classification systems to describe physeal injuries, but the Salter-Harris (1963) classification system is the most frequently used.
In our case, a partial physeal arrest resulted in a severe deformity with shortening and malangulation in the frontal and sagittal plane. However, there was no apparent direct involvement of the physis at the time of fracture.
Although injuries to the epiphysis and the metaphysis without apparent involvement of the growth plate might result in indirect damage to the physeal plate (Hresko and Kasser Citation1989, Ogden Citation1990, Perron et al. Citation2002), the location of the physeal bridge laterally and anteriorly made it most likely that it was caused by the temporary transphyseal pinning.
Whether transphyseal K-wire pinning or drilling would affect subsequent growth remains controversial. Various animal experiments have been attempted to investigate the effect of drilling on the physeal plate, and the conclusion has been that drill injuries that destroy less than 8–9% of the physis and small central destructions would not alter overall bone growth (Garces et al. Citation1994, Janarv et al. Citation1998). There is some experimental and clinical evidence that temporary crossing of the physeal plate with K-wires for internal fixation of dislocated joint injuries does not lead to bone bridging or growth disturbance (Boelitz et al. Citation1994, Yung et al. Citation2004). However, depending on the level of the surgeon's skill and experience, this technique may require one or more attempts—with potential damage to the physeal plate (Garces et al. Citation1994).
In our case, two K-wires (3 mm in diameter) were used for fracture fixation, whereas one wire was placed through the lateral and anterior part of the distal femoral physis with one single attempt. Considering the co-localization of the K-wire and the physeal bridge laterally and anteriorly in the distal femoral physis, we assume that the pinning of the K-wire led to permanent damage of the growth plate in this particular case.
The treatment options were: resection of the physeal bridge, physeal distraction, acute corrective osteotomy, or gradual correction using the Ilizarov method with complete epiphysiodesis of the affected physis. These procedures might be used in combination with contralateral shortening osteotomy or epiphysiodesis. However, in our opinion the best solution was to correct the affected bone. The nature of the deformity, with severe angulation and shortening, required a combined reconstructive procedure including both angular correction and adjustment of bone length.
We conclude that patients should be informed and observed subsequently after temporary transphyseal pinning, with clinical follow-up at intervals until skeletal maturity.
JH, HS, and LPK did the preoperative planning. JH and LPK operated the patient. JH and HS wrote the manuscript, and HS and LPK revised it.
- Anderson M, Green W T, Messner M B. Growth and predictions of growth in the lower extremities. J Bone Joint Surg (Am) 1963; 45: 1–14
- Boelitz R, Dallek M, Meenen N M, Jungbluth K H. Reaction of the epiphyseal groove to groove-crossing bore-wire osteosynthesis. Results of a histomorphologic small animal study. Unfallchirurgie 1994; 20: 131–7
- Bowen J R, Johnson W J. Percutaneous epiphysiodesis. Clin Orthop 1984; 190: 170–3
- Garces G L, Mugica-Garay I, Lopez-Gonzalez C N, Guerado E. Growth-plate modifications after drilling. J Pediatr Orthop 1994; 14: 225–8
- Hresko M T, Kasser J R. Physeal arrest about the knee associated with non-physeal fractures in the lower extremity. J Bone Joint Surg (Am) 1989; 71: 698–703
- Janarv P M, Wikstrom B, Hirsch G. The influence of transphyseal drilling and tendon grafting on bone growth: an experimental study in the rabbit. J Pediatr Orthop 1998; 18: 149–54
- Mann D C, Rajmaira S. Distribution of physeal and nonphyseal fractures in 2,650 long-bone fractures in children aged 0–16 years. J Pediatr Orthop 1990; 10: 713–6
- Mizuta T, Benson W M, Foster B K, Paterson D C, Morris L L. Statistical analysis of the incidence of physeal injuries. J Pediatr Orthop 1987; 7: 518–23
- Ogden J A. Anatomy and physiology of skeletal development. Skeletal injury in the child, W B Saunders, 1990; 2: 38–68
- Perron A D, Miller M D, Brady W J. Orthopedic pitfalls in the ED: pediatric growth plate injuries. Am J Emerg Med 2002; 20: 50–4
- Peterson H A, Madhok R, Benson J T, Ilstrup D M, Melton L J, III. Physeal fractures: Part 1. Epidemiology in Olmsted County, Minnesota, 1979–1988. J Pediatr Orthop 1994; 14: 423–30
- Salter R B, Harris W R. Injuries involving the epiphyseal plate. J Bone Joint Surg (Am) 1963; 45: 587–622
- Yung P S, Lam C Y, Ng B K, Lam T P, Cheng J C. Percutaneous transphyseal intramedullary Kirschner wire pinning: a safe and effective procedure for treatment of displaced diaphyseal forearm fracture in children. J Pediatr Orthop 2004; 24: 7–12