Abstract
Background and purpose — Arthroscopic acromioplasty is still commonly used in the treatment of shoulder impingement syndrome, even though its benefits are questioned; randomized controlled studies have not shown any benefits when compared to non-operative treatment. In this randomized study, we investigated whether operative treatment protects from later rotator cuff rupture and whether it has any effect on the development of rotator cuff muscle volume.
Patients and methods — 140 stage-II impingement patients were randomized to a structured exercise group (n = 70) or to an operative group (n = 70). In the operative group, arthroscopic acromioplasty was performed, after which a similar structured exercise program was begun. MRI of the shoulder was done at baseline and at 5 years.
Results — There were no statistically significant differences in either the amount of perforating ruptures of the supraspinatus tendon or in the changes in muscle volume at 5 years. The grading of muscle fatty degeneration showed worse results in the operative group, but this difference was not statistically significant.
Interpretation — In this study, we found that arthroscopic acromioplasty does not have any long-term benefit based on radiological findings of muscle volumes. Also, the frequency of later rotator cuff rupture was similar irrespective of whether or not surgery was performed. Acromioplasty is not justified as a treatment for dynamic shoulder impingement syndrome.
Arthroscopic acromioplasty is commonly used in the treatment of shoulder impingement (Vitale et al. Citation2010, Yu et al. Citation2010), even though its benefits have been questioned (Brox et al. Citation1999, Haahr et al. Citation2006, Ketola et al. Citation2009, Citation2013). The operation does not appear to bring any additional value to the treatment compared to structured exercise treatment alone; nor is it cost-effective (Ketola et al. Citation2009, Citation2013). Acromioplasty is frequently used after failed non-operative treatment, yet there is no proof that these patients would benefit from the operation either (Ketola et al. Citation2015).
Acromial morphology changes with age. Increase in the numbers of type-III acromion, a hooked-type, has been reported in patients over 50 years of age. Yet the incidence of type-III acromions in symptomatic patients is lower than in asymptomatic patients, indicating that the presence of type-III acromion does not in itself produce impingement syndrome (Wang and Shapiro Citation1997). The incidence of both asymptomatic and symptomatic cuff tears increases with age (Yamaguchi et al. Citation2001, Nove-Josserand et al. Citation2005, Yamamoto et al. Citation2010). A long-term protective effect of arthroscopic acromioplasty on rotator cuff tendons has been suggested (Neer Citation1972, Citation1983), but this has not been verified by modern MRI studies.
In this randomized study, we analyzed 140 patients with shoulder impingement syndrome using MRI at baseline and after 5 years, to find out whether operative treatment does indeed protect from rotator cuff rupture later in life and whether it has any effect on the muscle volume.
Patients and methods
Between 2001 and 2004, we recruited 140 patients who had a clinically proven shoulder impingent syndrome that had been symptomatic for at least 3 months. The diagnosis was based on anamnestic information, typical symptoms, and clinical findings including the Neer injection test. MRI of the shoulder was taken. The patients were collected from the Kanta-Häme Health Care District, which had a population of 165,000 at the time of the recruitment. Only patients who had not had any previous shoulder operation were included in the study. The mean age of the patients at baseline was 47 (23–60) years (88 women). The mean height of the patients was 169 (151–193) cm (men 178 cm, women 164 cm).
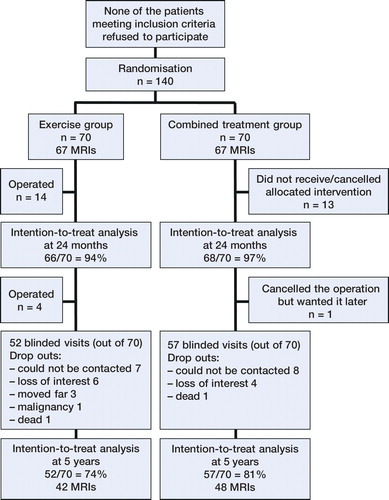
The patients represented in a flowchart according to the treatment groups (intention-to treat) at baseline, 2 years, and 5 years.
Self-reported pain on a visual analog scale (VAS; 0–10) was used as the primary health outcome measure.
At enrollment, 134 patients were examined with MRI scanning. 6 patients were not examined because of claustrophobia or obesity, or due to having metal implants in their bodies. At the 5-year control visit, we were able to reach 109 of the patients for clinical examination (52 in the exercise group and 57 in the combined treatment group) and a control MRI was done in 90 patients (42 and 48, respectively).
The patients were randomized to 2 treatment groups (Figure). In the combined treatment group, arthroscopic acromioplasty was carried out with a subsequent supervised and structured exercise regime. The same exercise regime was used in the other group also, but with no prior surgical treatment. For a full study protocol, see Ketola et al. (Citation2009), which reports the 2-year clinical results for these patients, including the cost effectiveness.
MRI of the shoulder was carried out at baseline before randomization. The MRI examinations were performed in 2 radiological centers belonging to the hospital district (Kanta-Häme Central Hospital and Forssa Regional Hospital).
At Kanta-Häme Central Hospital, the shoulders were scanned with a Philips Gyroscan Intera T10-NT 1.0 T magnetic resonance imaging system; at Forssa Regional Hospital, they were scanned with a Philips Gyroscan T5-NT 0.5 T system. In each imaging, a dedicated shoulder surface coil was used.
Follow-up MRI scanning was done 5 years after randomization, at Kanta-Häme Central Hospital with the 1.0 T MRI system described above. A dedicated shoulder surface coil was used. The scans were analyzed at Kanta-Häme Central Hospital on a Fuji PACS work station and at the Radiology Department, Tampere University Hospital on a Barco MFGD 2320 work station (with Impax DS3000 5.2 software).
MRI examinations were evaluated by 2 independent, experienced musculoskeletal radiologists. They both filled out a structured MRI form for each patient, and were blind regarding the patient’s medical history and treatment group. A separate form was filled out for the baseline and for the 5-year follow-up. Each patient’s results were evaluated on separate occasions to avoid intraobserver bias. The results obtained by the 2 radiologists were combined, and a consensus statement was prepared in cases with interobserver disagreement. The consensus statement was based on re-evaluation of the MRI results in such cases. These consensus values were used in further analyses.
The acromial shape was evaluated according to Bigliani as type-I (straight or flat), type-II (curved), or type-III (hooked) (Morrison et al. Citation1987) on sagittal MRI scans using at least 2 of the most lateral slices of the acromion (Bright et al. Citation1997, Mayerhoefer et al. Citation2005). At this point, other variations of the acromial form were also noted—as well as possible thickening of the coraco-acromial ligament and cranialization of the humerus (Saupe et al. Citation2006). The tendons were evaluated for tendinosis and possible tears. The muscle volume quantity was estimated using a method developed by Lehtinen et al. (Citation2003) in which the muscle volume is calculated based on the area of 2 T1-weighted sagittal scans. The volume was also estimated by the Tangent sign method (Zanetti et al. Citation1998).
The fatty degeneration of the muscles was graded according to the Goutallier method, using T1-weighted sagittal MRI slices. The grading was divided into 5 steps: stage 0 corresponds to a completely normal muscle, without any fatty streak; in stage 1, the muscle contains some fatty streaks; in stage 2, the fatty infiltration is important, but there is still more muscle than fat; in stage 3, there is as much fat as muscle; and in stage 4, more fat than muscle is present (Goutallier et al. Citation1994, Fuchs et al. Citation1999).
Statistics
McNemar’s test was used to compare the shape of the acromion before and 5 years after the intervention. Fisher’s exact test was used to compare Goutallier stages between operated and non-operated groups. Any p-value <0.05 was considered to be statistically significant. Statistical analyses were performed using IBM SPSS Statistics version 19.0.
Ethics and registration
The study was approved by the ethics committee of the hospital district (E09/2001) and is registered at ClinicalTrials.gov (identifier: NCT00349648).
Results
The volumes of m. supraspinatus, m. infraspinatus, and m. subscapularis at baseline are presented in , together with results from previously published studies—mainly concerning healthy shoulders. All the muscle volumes in this study diminished during follow-up. This change was statistically significant in m. supraspinatus (p = 0.004) but not in m. infraspinatus or subscapularis (p = 0.3 and p = 0.4, respectively).
Table 1. The volumes (cm3) of rotator cuff muscles at baseline and at 5 years with reference values from the previous literature
We also analyzed the muscle volumes in different subgroups: those patients who fully followed the randomized treatment protocol, either in the exercise group or the combined treatment group, and also those who wanted and had surgery in the exercise group during the 5 years of follow-up (18 patients). There were no statistically significant differences in changes in muscle volume between the groups. In the combined treatment group the volume of m. supraspinatus decreased by 7%, and in the exercise group it decreased by 4% (p = 0.6). The changes in m. subscapularis (p = 0.5) and m. infraspinatus (p = 0.9) were not significantly different between groups. The muscle volume of m. supraspinatus diminished by 10% in patients with a partial tear, and 23% in those diagnosed with total rupture.
The grading of muscle fatty degeneration showed that 65% of the patients who were operated had at least some fatty streaks, as compared to 54% in the non-operative group. This 11 percentage point difference was not statistically significant (p = 0.3). Overall, there were no significant differences between the groups regarding fatty degeneration of any grade (Table 2, see Supplementary data). The shape of the acromion according to Bigliani at baseline was type-I for 45% of patients, type-II for 43%, and type-III for 11%.
In total, 15 patients had a full-thickness tear of the supraspinatus tendon at 5 years. 8 of these had had acromioplasty. Of these patients, at baseline MRI 4 had type-I acromion, 9 had type-II acromion, and 2 had type-III acromion (p = 0.7).
At baseline, the proportion of pain-free patients (VAS 0–3) was 11% in Bigliani I, 4% in Bigliani II, and 8% in Bigliani III. Thus, no correlation was found between the shape of the acromion and pain. Mean values (VAS) for self-reported pain were 6.5 for type I, 6.8 for type II, and 6.5 for type III (p = 0.8).
The majority of the type-II acromions that had acromioplasty were still type-II at 5 years; none were type-I. One-third of the type-I acromions had turned to type-II. After acromioplasty, 5 of 6 acromions of type III were type I–II at 5 years. In the non-operated group, there were no statistically significant changes during the follow-up period (Table 3, see Supplementary data)
Effusion in the subacromial bursa was reported as being present or not. Most of the patients had subaromial bursal effusion at baseline (76%) and also at 5 years (80%). In those with no bursal irritation the mean self-reported pain value (VAS) was 6.8 at 5 years, and in those with subacromial bursal fluid it was 6.6 (p = 0.7).
The coraco-acromial ligament was more likely to be thickened at 5 years in patients who had had acromioplasty than in those who were not operated (44% vs. 20%; p = 0.02).
The mean subacromial distance at baseline was 8.2 mm in operated patients and 7.5 mm in those who were not operated (p = 0.03). Whether or not this minor difference is of any clinical importance is unclear.
Discussion
In the operated and the non-operated groups, we found a similar frequency of subsequent rotator cuff tendon ruptures and a similar difference in change in muscle volume both at baseline and at 5 years.
Arthroscopic acromioplasty has been given support on the assumption that by enhancing the mechanical situation, the supraspinatus muscle-tendon unit would degenerate more slowly; the decompression has been thought to prevent tendon ruptures in the long run (Bjornsson et al. Citation2010). In the present study, the procedure did not appear to protect from tendon rupture, or diminish the degeneration of the muscle mass.
Half of the non-operated patients had a completely normal supraspinatus muscle without any fatty streaks. The proportion was smaller in the operative group (35%), but this finding was not statistically significant.
The proportion of type-III acromion appears to become higher along with ageing. The prevalence is 16% at 30–50 years and 31% in individuals over 50 years of age (Gill et al. Citation2002). Any influence of acromial morphology on the rotator cuff tears has not been clearly proven. Still, some authors have considered it to be important while others have thought that the changes in morphology could be the result of the degenerative rotator cuff disease rather than the cause (Ozaki et al. Citation1988, Nicholson et al. Citation1996, Wang and Shapiro Citation1997, Shah et al. Citation2001). In our study, 11% of the patients (15 of 134) had type-III acromion. Only 2 of those 15 patients who had developed a supraspinatus rupture had a type-III acromion. Our findings are consistent with the results of Moor et al. (Citation2014) regarding the lack of association between Bigliani type of acromion and cuff tears. However, they considered the critical shoulder angle to be the most accurate predictor of a patient’s individual risk of experiencing rotator cuff tear. Also, Hyvönen et al. (Citation1998) have shown that a rotator cuff tear may appear after open acromioplasty, even though there was no evidence of a cuff lesion at the time of operation. In the present study, more than one-third of type-I acromions degenerated into type-II despite the treatment. The re-shaped form is not fully sustained in acromions of type II–III either.
Shoulder impingement syndrome involves a degree of inflammation of the bursa in the subacromial space (Bigliani et al. Citation1997). This reduces the volume of subacromial space. Based on our findings, this is a very common finding in these patients and does not correlate with the symptoms at all.
Our study had some strengths and weaknesses. There were 90 control MRI examinations at 5 years as compared to 134 at baseline. The radiological evaluations of the shoulders were done using MRI scans, including the Bigliani classification. Usually plain radiographs are used, but the MRI method has been shown to be accurate when using a combination of 2 MRI slices (Mayerhoefer et al. Citation2005). According to the current literature, MR arthrography is more sensitive in detecting rotator cuff tears than MRI alone. This is especially true with partial-thickness tears. We did not use arthrography, and this may to some extent have affected the incidence of minor cuff tears detected. However, the method was the same in both study groups, so the results in the groups are comparable.
In summary, after previously showing the inefficacy of the arthroscopic acromioplasty in improving subjective symptoms of the shoulder impingement syndrome, we now show that this procedure probably has no long-term benefit regarding the development of rotator cuff tendon ruptures, or regarding muscle volumes. Based on the combined results, it appears that arthroscopic acromioplasty is not justified in the treatment of shoulder impingement syndrome.
Supplementary data
Tables 2 and 3 are available on the Acta Orthopaedica website at www.actaorthop.org, identification number 9632.
SKe and IA planned the study. SKe and JL recruited the patients. SKe, JL, and IA organized the study. SKe collected and organized the data. PE and SKo performed the radiological evaluations. SKe and HH performed the statistical testing. JL and IA performed clinical analysis of the data. SKe and JL reviewed the literature. SKe wrote the draft manuscript and all the authors gave critical comments for improvement of the article.
- Bigliani L U, Levine W N. Subacromial impingement syndrome. J Bone Joint Surg Am 1997; 79(12): 1854–68.
- Bjornsson H, Norlin R, Knutsson A, Adolfsson L. Fewer rotator cuff tears fifteen years after arthroscopic subacromial decompression. J Shoulder Elbow Surg 2010; 19(1): 111–5.
- Bright A S, Torpey B, Magid D, Codd T, McFarland E G. Reliability of radiographic evaluation for acromial morphology. Skeletal Radiol 1997; 26(12): 718–21.
- Brox J I, Gjengedal E, Uppheim G, Bohmer A S, Brevik J I, Ljunggren A E, et al. Arthroscopic surgery versus supervised exercises in patients with rotator cuff disease (stage II impingement syndrome): a prospective, randomized, controlled study in 125 patients with a 2 1/2-year follow-up. J Shoulder Elbow Surg 1999; 8(2): 102–11.
- Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C. Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elbow Surg 1999; 8(6): 599–605.
- Gill T J, McIrvin E, Kocher M S, Homa K, Mair S D, Hawkins R J. The relative importance of acromial morphology and age with respect to rotator cuff pathology. J Shoulder Elbow Surg 2002; 11(4): 327–30.
- Goutallier D, Postel J M, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res 1994; (304): 78–83.
- Haahr J P, Andersen J H. Exercises may be as efficient as subacromial decompression in patients with subacromial stage II impingement: 4-8-years’ follow-up in a prospective, randomized study. Scand J Rheumatol 2006; 35(3): 224–8.
- Holzbaur K R, Murray W M, Gold G E, Delp S L. Upper limb muscle volumes in adult subjects. J Biomech 2007; 40(4): 742–9.
- Hyvönen P, Lohi S, Jalovaara P. Open acromioplasty does not prevent the progression of an impingement syndrome to a tear. Nine-year follow-up of 96 cases. J Bone Joint Surg Br 1998; 80(5): 813–6.
- Juul-Kristensen B, Bojsen-Moller F, Finsen L, Eriksson J, Johansson G, Stahlberg F, et al. Muscle sizes and moment arms of rotator cuff muscles determined by magnetic resonance imaging. Cells Tissues Organs 2000; 167(2-3): 214–22.
- Ketola S, Lehtinen J, Arnala I, Nissinen M, Westenius H, Sintonen H, et al. Does arthroscopic acromioplasty provide any additional value in the treatment of shoulder impingement syndrome?: a two-year randomised controlled trial. J Bone Joint Surg Br 2009; 91(10): 1326–34.
- Ketola S, Lehtinen J, Rousi T, Nissinen M, Huhtala H, Konttinen Y T, et al. No evidence of long-term benefits of arthroscopicacromioplasty in the treatment of shoulder impingement syndrome: Five-year results of a randomised controlled trial. Bone Joint Res 2013; 2(7): 132–9.
- Ketola S, Lehtinen J, Rousi T, Nissinen M, Huhtala H, Arnala I. Which patients do not recover from shoulder impingement syndrome, either with operative treatment or with nonoperative treatment? Acta Orthop 2015; 86(6): 641–6
- Lehtinen J T, Tingart M J, Apreleva M, Zurakowski D, Palmer W, Warner J J. Practical assessment of rotator cuff muscle volumes using shoulder MRI. Acta Orthop Scand 2003; 74(6): 722–9.
- Mayerhoefer M E, Breitenseher M J, Roposch A, Treitl C, Wurnig C. Comparison of MRI and conventional radiography for assessment of acromial shape. AJR Am J Roentgenol 2005; 184(2): 671–5.
- Moor B K, Wieser K, Slankamenac K, Gerber C, Bouaicha S. Relationship of individual scapular anatomy and degenerative rotator cuff tears. J Shoulder Elbow Surg 2014; 23(4): 536–41.
- Morrison D S, Bigliani L U, April E W. The morphology of the acromion and its relationship to rotator cuff tears. Orthop Trans 1987; 11: 439.
- Neer C S, 2nd. Anterior acromioplasty for the chronic impingement syndrome in the shoulder: a preliminary report. J Bone Joint Surg Am 1972; 54(1): 41–50.
- Neer C S, 2nd. Impingement lesions. Clin Orthop Relat Res 1983; (173): 70–7.
- Nicholson G P, Goodman D A, Flatow E L, Bigliani L U. The acromion: morphologic condition and age-related changes. A study of 420 scapulas. J Shoulder Elbow Surg 1996; 5(1): 1–11.
- Nove-Josserand L, Walch G, Adeleine P, Courpron P. Effect of age on the natural history of the shoulder: a clinical and radiological study in the elderly. Rev Chir Orthop Reparatrice Appar Mot 2005; 91(6): 508–14.
- Ozaki J, Fujimoto S, Nakagawa Y, Masuhara K, Tamai S. Tears of the rotator cuff of the shoulder associated with pathological changes in the acromion. A study in cadavera. J Bone Joint Surg Am 1988; 70(8): 1224–30.
- Saupe N, Pfirrmann CW, Schmid MR, Jost B, Werner CM, Zanetti M. Association between rotator cuff abnormalities and reduced acromiohumeral distance. AJR Am J Roentgenol 2006; 187(2): 376–382.
- Shah N N, Bayliss N C, Malcolm A. Shape of the acromion: congenital or acquired–a macroscopic, radiographic, and microscopic study of acromion. J Shoulder Elbow Surg 2001; 10(4): 309–316.
- Vidt M E, Daly M, Miller M E, Davis C C, Marsh A P, Saul K R. Characterizing upper limb muscle volume and strength in older adults: a comparison with young adults. J Biomech 2012; 45(2): 334–41.
- Vitale M A, Arons R R, Hurwitz S, Ahmad C S, Levine W N. The rising incidence of acromioplasty. J Bone Joint Surg Am 2010; 92(9): 1842–50.
- Wang J C, Shapiro M S. Changes in acromial morphology with age. J Shoulder Elbow Surg 1997; 6(1): 55–9.
- Yamaguchi K, Tetro A M, Blam O, Evanoff B A, Teefey S A, Middleton W D. Natural history of asymptomatic rotator cuff tears: a longitudinal analysis of asymptomatic tears detected sonographically. J Shoulder Elbow Surg 2001; 10(3): 199–203.
- Yamamoto N, Muraki T, Sperling J W, Steinmann S P, Itoi E, Cofield R H, et al. Contact between the coracoacromial arch and the rotator cuff tendons in nonpathologic situations: A cadaveric study. J Shoulder Elbow Surg 2010; 19(5): 681–7
- Yu E, Cil A, Harmsen W S, Schleck C, Sperling J W, Cofield R H. Arthroscopy and the dramatic increase in frequency of anterior acromioplasty from 1980 to 2005: an epidemiologic study. Arthroscopy 2010; 26(9 Suppl): S142–S7.
- Zanetti M, Gerber C, Hodler J. Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Invest Radiol 1998; 33(3): 163–70.
