Abstract
Background and purpose — Patient-reported outcome (PRO) is recognized as an important tool for evaluating the outcome and satisfaction after total hip arthroplasty (THA). We wanted to compare patient-reported outcome measure (PROM) scores from patients with ceramic-on-ceramic (CoC) THAs and those with metal-on-metal (MoM) THAs to scores from patients with metal-on-polyethylene (MoP) THAs, and to determine the influence of THA-related noise on PROM scores.
Patients and methods — We conducted a nationwide cross-sectional questionnaire survey in a cohort of patients identified from the Danish Hip Arthroplasty Registry. The PROMs included were: hip dysfunction and osteoarthritis and outcome score (HOOS), EQ-5D-3L, EQ VAS, UCLA activity score, and questions about noise from the THA. The response rate was 85% and the number of responders was 3,089. Of these, 45% had CoC THAs, 17% had MoM THAs, and 38% had MoP THAs, with a mean length of follow-up of 7, 5, and 7 years, respectively.
Results — Compared to MoP THAs, the mean PROM scores for CoC and MoM THAs were similar, except that CoC THAs had a lower mean score for HOOS Symptoms than did MoP THA. 27% of patients with CoC THAs, 29% with MoM THAs, and 12% with MoP THAs reported noise from their hip. For the 3 types of bearings, PROM scores from patients with a noisy THA were statistically significantly worse than those from patients with a silent MoP THA. The exception was noisy CoC and MoM THAs, which had the same mean UCLA activity score as silent MoP THAs.
Interpretation — A high proportion of patients reported noise from the THA, and these patients had worse PROM scores than patients with silent MoP THAs.
Due to problems related to polyethylene wear particles (Jacobs et al. Citation1994), ceramic-on-ceramic (CoC) and metal-on-metal (MoM) bearings have been introduced as alternatives to metal-on-polyethylene (MoP) bearings. In population-based studies from hip arthroplasty registries, the medium-term survival of CoC THA equalled that of MoP THA. In contrast, medium-term survivorship for MoM THA was lower than that for MoP THA, especially for specific component brands of MoM THA. The main cause of revision for CoC THA was dislocation (1.2%), and for MoM THA it was aseptic loosening (1.9%) (Varnum et al. Citation2015a, Citationb). As survival and causes of revision differed for different types of bearings, one could also ask whether patient-reported outcomes (PROs) would be different for different bearings in THA. To our knowledge, only 2 studies have examined the influence of different bearings on PROs. A study from a single center in the UK, involving 911 patients with a mean follow-up of 2.4 years after index surgery, found no relationship between bearings and patient-reported outcome measure (PROM) scores (Smith et al. Citation2012). In a study from the National Joint Registry for England and Wales (NJR), the EQ-5D index was compared for different bearings after 6 months of follow-up (Jameson et al. Citation2015). These studies were, however, limited by the small number of patients, the lack of generalizability, and the short follow-up.
An alternative outcome reported for THA is noise. In a meta-analysis, the reported prevalence of squeaking from CoC bearings was 4.2% (Owen et al. Citation2014), but other studies have reported prevalences ranging from less than 1% (Capello et al. Citation2008) to 36% (Swanson et al. Citation2010). Noises from MoM and MoP bearings have also been reported (Jarrett et al. Citation2009, Bernasek et al. Citation2011), but only a few authors have studied the influence of bearing noise on PROs and health-related quality of life (Restrepo et al. Citation2010, Sexton et al. Citation2011).
We therefore conducted a nationwide cross-sectional questionnaire survey in a cohort of patients registered in the Danish Hip Arthroplasty Registry (DHR). We examined the association between CoC, MoM, and MoP bearings and both generic and disease-specific PROM scores. Furthermore, we examined the prevalence and types of noises from the 3 types of bearings and the association between noise and postoperative PROM scores.
Patients and methods
The population of Denmark is approximately 5.6 million, and every Danish citizen has a unique, 10-digit civil registration number.
Sources of data
The Civil Registration System (CRS) was established in 1968 (Schmidt et al. Citation2014). It contains data on address, date of emigration, date of death, and whether or not people are protected against inquiries from researchers.
The DHR, founded in 1995 (Lucht Citation2000), is a nationwide, population-based clinical database containing prospectively collected data on primary THAs and revisions. The registry was validated in 2004 (Pedersen et al. Citation2004) and has a coverage of 100%, since all the orthopedic departments and private clinics report to the registry. The completeness of the DHR has been about 95% (for both primary procedures and revisions) for many years, relative to the Danish National Patient Registry (DNPR), which is considered to be the gold standard—as departments are reimbursed by the authorities when they report to the DNPR.
The DNPR was established in 1977, and contains data on all admissions and discharges from Danish hospitals, including diagnoses and surgical procedure codes. Since 1994, diagnoses have been classified according to the Danish version of the International Classification of Diseases, tenth edition (Schmidt et al. Citation2015). Based on data from the DNPR, the Charlson comorbidity index (CCI) using 10-year history of hospitalization was determined at the time of receiving PROMs (Charlson et al. Citation1987, Thygesen et al. Citation2011). The CCI is composed of 19 major disease categories, each weighted with 0, 1, 2, 3, or 6 points. The index score is provided by the sum of these weightings, and patients were classified according to 3 levels of comorbidity: low-index (individuals with a score of 0 prior to the time of receiving PROMs), moderate-index (individuals with 1 or 2 points), and high-index (individuals with more than 2 points) (Groot et al. Citation2003).
Study population
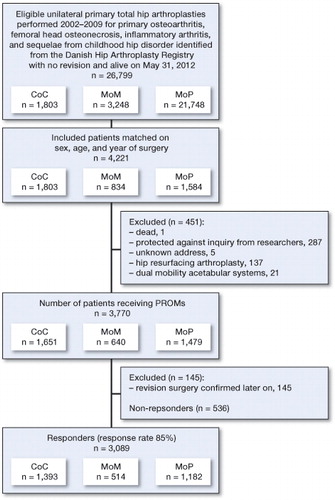
The study population consisted of patients who had stemmed THA with CoC, MoM, or MoP bearings, and who were operated for primary osteoarthritis (OA), femoral head osteonecrosis, inflammatory arthritis, or sequelae from childhood hip disorder (Figure). In MoP bearings, the polyethylene could be either ultra-high-molecular-weight or highly cross-linked polyethylene.
Registration of type of bearings in the DHR started in 2002. From this registry, we identified all patients who had undergone primary THA with CoC bearings between January 1, 2002 and December 31, 2009, with no revisions registered in the DHR and still alive on May 31, 2012. Each CoC patient was matched according to sex, age at primary surgery, and year of surgery to 1 patient with MoM bearings and 1 patient with MoP bearings. These patients had to fulfill the same inclusion criteria as the CoC patients. However, it was not possible to define a unique match to every patient with CoC THA in patients with MoM and MoP THA, which resulted in unequal groups. When a patient underwent bilateral THA, only the first was eligible for this study due to the statistical assumption of independent observations. Patients were excluded if they had protection against inquiry from researchers, if they had an unknown address, or if they had received hip resurfacing arthroplasty and a dual-mobility acetabular system—due to the different prosthetic/mobility concept (and therefore different prognosis).
3,770 patients were eligible for the study and received PROMs. Patients who send back answered PROMs were classified as responders (n = 3,089). Patients were classified as non-responders if they returned unanswered PROMs (n = 31) or if they did not send back the PROMs at all (n = 505). 145 patients answered that they had undergone revision surgery. This may have been due to delay of registration of revision in the DHR or to revision surgery after May 31, 2012, and these 145 patients were excluded. Since patients received the questionnaire on November 1, 2012, the minimum follow-up was 2.8 years from primary THA.
PROMs
A complete questionnaire including an addressed and pre-paid return envelope was mailed in paper form to the patient. The questionnaire comprised an introduction letter, disease-specific and generic PROMs, and questions about noise from the THA. In the introduction letter, it was clearly pointed out that the questionnaire should be answered on the basis of the left or right THA when the patient had undergone bilateral THA. We included questions covering background data such as height and weight for calculation of BMI. Due to the possible delay in registration of revision data in the DHR, the patients were asked if they had had revision surgery in that particular THA. If necessary, 1 reminder letter was sent. Returned questionnaires were scanned electronically using a validated automated forms-processing technique (Paulsen et al. Citation2012a).
HOOS. The hip disability and osteoarthritis outcome score (HOOS) (Nilsdotter et al. Citation2003) is disease-specific. It was constructed by adding dimensions dealing with function in sport and recreation and hip-related quality of life to the Western Ontario and McMaster Universities osteoarthritis index (WOMAC) (Bellamy et al. Citation1988). HOOS includes 5 subscales: pain, other symptoms, activities of daily living, sport and recreation function, and hip-related quality of life. It is a validated instrument (Klassbo et al. Citation2003, Nilsdotter et al. Citation2003) and is recommended for evaluation of patients with hip OA who undergo non-surgical treatment and surgical interventions such as THA (Thorborg et al. Citation2010). For each subscale, a score between 0 and 100 is calculated (with 100 indicating no symptoms and 0 indicating extreme symptoms). The subscale score can be calculated if at least 50% of the items on the subscale have been answered (HOOS scoring instructions are available at http://www.koos.nu/index.html).
EQ-5D-3L. The EQ-5D-3L describes the health-related quality of life from a social point of view (EQ-5D index) and from the patient’s point of view (EQ visual analog scale (VAS)) (The EuroQol Group Citation1990, Brooks Citation1996). The EQ-5D index is determined from 5 dimensions—mobility, self-care, usual activities, pain/discomfort, and anxiety/depression—and the patient choses 1 of 3 levels of severity for each dimension: no problems, some/moderate problems, and extreme problems. Based on the time trade-off method (Dolan et al. Citation1996), a value set ranging from −0.624 to 1, where 1 indicates full health and 0 represents being dead, constitutes the Danish culture-adjusted EQ-5D index (Wittrup-Jensen et al. Citation2009). The EQ VAS is determined when the patients value their current state of health on a scale ranging from 0 (“worst imaginable”) to 100 (“best imaginable”).
UCLA activity score. The University of California, Los Angeles (UCLA) activity score is disease-specific and has 10 descriptive activity levels ranging from wholly inactive and dependent on others (level 1) through moderate activities such as unlimited housework and shopping (level 6), to regular participation in impact sports such as jogging or tennis (level 10) (Amstutz et al. Citation1984). The UCLA activity score has been found to be the most appropriate scale for assessment of physical activity levels in patients undergoing total joint replacement (Naal et al. Citation2009).
Information on noise. We asked all the patients if they had experienced noise from their THA. If so, the patient was asked to describe the noise as squeaking, creaking, grating, clicking, or “other”. Furthermore, the patients were asked to answer questions about onset (time after surgery at which the noise started), frequency (daily, weekly, more seldom than weekly), audibility (whether the noise could be heard only by the patient or by others), activities triggering the noise (rising from a chair, sitting down, bending, walking, walking upstairs or downstairs, climbing a high stair, or some other activity), and personal impact (the degree to which noise led to reduced physical function and inhibited being together with other people). The questions about noise were developed during the test phase, based on 18 patients who were randomly selected from patients admitted to the Department of Orthopaedic Surgery, Vejle Hospital, for primary THA surgery. In addition, the questions were tested by 3 patients who had undergone revision of their CoC THA due to noise.
Statistics
Characteristics of the study population, response rate for every item, the rate of discarded subscale scores, and characteristics of noise from the THA were calculated as proportions. Chi-square test was used to compare proportions between groups. Responders and non-responders were compared with prevalence-proportion ratios (PPRs). Time period from surgery to onset of noise from the THA is presented as median and interquartile range (IQR) and was compared by Kruskal-Wallis test due to skewness. Univariate linear regression was used to compute and compare mean values of age, time since index surgery when receiving PROMs, and BMI between the 3 bearing groups. Multivariate linear regression was used to assess and compare mean values of PROM subscale scores between the bearing groups. Adjustments in the multivariate linear models were made for the categorical variables sex, diagnosis, CCI, year of surgery, fixation, and femoral head size as categorized in . Adjustment for the continuous variables age and BMI was performed by restricted cubic splines to allow for a non-linear dependency of PROM subscale scores and each variable. Due to the large study population, 5 knots placed at the 0.05, 0.275, 0.5, 0.725, and 0.95 percentiles were used on the splines (Harrell Citation2001). All estimates are presented with 95% confidence intervals (CIs). To adjust for departure of normality of the outcomes in the regression analyses, all CIs were based on bootstraps with 100 samplings with replacement at the patient level. In all analyses, MoP was considered to be the standard bearing and was therefore used as reference. Any p-value below 0.05 was considered significant, and a mean difference including 95% CI different from 0 indicates a statistically significant finding at the 5% significance level. Statistical analyses were carried out with Stata Statistical Software release 14.1.
Table 2. Demographics of patients classified as responders and having ceramic-on-ceramic (CoC), metal-on-metal (MoM), or metal-on-polyethylene (MoP) total hip arthroplasties. Values are number of patients and percentage in each group
Ethics
This study was approved by the Danish Data Protection Agency (entry no. 2010-41-4926) and by Statens Serum Institut for procuration of data from the DNPR (FSEID 00000467).
Results
Non-responders vs. responders
The response rate was 85% (3,089 of 3,625). Compared to responders, the non-responders were younger and less likely to be diagnosed with OA, but more likely to have comorbidity. Furthermore, compared to responders, fewer non-responders had cementless THA and more had cemented THA, and fewer had CoC bearings and more had MoP bearings ().
Table 1. Characteristics of non-responders and responders. Values are number of patients and percentage in each group and prevalence-proportion ratio (PPR), non-responders vs. responders, with 95% confidence interval
Description of the study population
In the study population (n = 3,089), 45% underwent CoC THA, 17% underwent MoM THA, and 38% underwent MoP THA. There was a similar distribution of sexes in the 3 bearing groups. Patients with CoC and MoM bearings were statistically significantly younger than patients with MoP bearings, and patients with MoM bearings had significantly lower BMI than patients with MoP bearings. BMI levels were similar for patients with CoC and MoP bearings. Significantly more patients with MoM bearings were diagnosed with OA than patients with MoP and CoC bearings, and patients with MoP bearings had significantly more comorbidity than patients with the other bearings. 15% of the patients with MoM bearings had their THA implanted during the period 2002–2005, whereas 56% of patients with CoC bearings and 55% of patients with MoP bearings underwent surgery during the same period. For the period 2006–2009, the corresponding percentages were 85%, 44%, and 45% for MoM, CoC, and MoP bearings. Most patients in all 3 bearing groups had cementless THA. Most patients with MoP bearings had femoral head sizes of 28 mm or less, whereas most patients with CoC bearings had 32-mm femoral heads and patients with MoM bearings mostly had femoral head sizes of 36 mm or more. Mean length of follow-up was similar in the CoC and MoP groups, but the mean length of follow-up was shorter in the MoM group than in the MoP group ( and ).
Table 3. Association between patients with total hip arthroplasty with ceramic-on-ceramic (CoC), metal-on-metal (MoM), and metal-on-polyethylene (MoP) bearings, crude mean values, and crude mean differences of age, BMI, and follow-up. 95% confidence intervals are given in parentheses
Missing items and subscales
Apart from the HOOS item A6 about difficulties when “walking on a flat surface”, which had a higher proportion of missing answers in the MoP group, no differences in the proportions of missing items in the HOOS, EQ-5D index, EQ VAS, and UCLA activity score were found between the 3 bearing groups (Tables 4–6, see Supplementary data). The proportion of discarded subscale scores and discarded BMI due to missing items was low, and there was no difference in the distribution between the bearing groups (Table 7, see Supplementary data).
Comparison of subscale scores between bearing groups
For HOOS Symptoms, the adjusted mean score was significantly worse for the CoC group than for the MoP group (adjusted mean difference (aMD): −2.3 (95% CI: −4.1 to −0.5)). No other stastistically significant adjusted differences were found for the other HOOS subscales, EQ-5D index, EQ-5D VAS, or UCLA activity score when comparing the CoC and MoM groups to the MoP group (Table 8, see Supplementary data).
Noise
27% of patients with CoC bearings, 29% of patients with MoM bearings, and 12% of patients with MoP bearings had experienced noise from the THA. Patients with CoC THA mainly experienced clicking and creaking noises, and patients with MoM and MoP bearings mainly experienced clicking, grating, and creaking noises. Half of the patients were unable to recall how long after surgery noise was experienced for the first time. Median onset of noise after surgery was 10 months for CoC bearings, 0 months for MoM bearings, and 5 months for MoP bearings (p = 0.02). Of the patients with noise from the THA, 33–47% experienced noise on a daily or weekly basis, and 4–12% indicated that the noise was always audible to other people. Noises were mainly present when bending in patients with CoC and MoM bearings and when walking in patients with MoP bearings. In 36–47% of patients, noise from the THA led to some degree of reduction in physical activity, and 6–16% of patients stated that to some degree noise from the THA hindered being with other people ().
Table 9. Prevalence and characteristics of types of noises from total hip arthroplasties in patients with ceramic-on-ceramic (CoC), metal-on-metal (MoM), and metal-on-polyethylene (MoP) bearings. Values are number of patients and percentage in each group
Stratified analyses for the 3 types of bearings with and without noise showed statistically significantly worse adjusted mean scores in all HOOS subscales, EQ-5D index, and EQ-5D VAS for patients who experienced noise from their CoC, MoM, or MoP THA than for patients who had silent MoP THAs. For all subscales, the aMD was greatest for noisy MoP THAs. No difference was found between noisy CoC and MoM THAs and silent MoP THAs only in the ULCA activity score, but patients with noisy MoP THAs had significantly lower mean UCLA activity scores than patients with silent MoP THAs. No significant aMD was found in any subscale between the CoC and MoM groups without noise and the MoPgroup without noise (Table 10, see Supplementary data).
Discussion
In this population-based, cross-sectional questionnaire survey we found similar mean scores in the 5 HOOS subscales, EQ-5D index, EQ VAS, and UCLA activity score in patients with CoC, MoM, and MoP THAs after 5–7 years of follow-up. Patients with MoP THA reportedly experienced less noise than MoM and CoC THA patients. Regardless of which bearing they had, patients with noise had worse subscale scores than patients with silent MoP THAs.
Comparison of the main findings with those in other studies
Jameson et al. (2015) compared the EQ-5D index 6 months after primary THA with CoC, MoP, or ceramic-on-polyethylene (CoP) bearings in 4,596 patients. The median postoperative EQ-5D index was higher for CoC THA and lower for CoP THA. However, when comparing changes in preoperative and postoperative EQ-5D index between bearing groups, no differences were found using multivariable analysis. We did not determine the change in EQ-5D index, as no preoperative values were available, but after 5.1–6.9 years of follow-up, we found similar EQ-5D index scores in patients with CoC, MoM, and MoP bearings.
In January 2012, the Danish Broadcasting Corporation started a series of news items on the adverse events and risks of having MoM bearings, and the negative publicity continued in the Danish media throughout the spring of 2012. For this study, the questionnaire was mailed to the patients on November 1, 2012. Although an increased risk of revision has been found for MoM (Varnum et al. Citation2015b), similar PROM scores were found for MoM THA and MoP THA. One explanation of this might be that patients are not revised due to functional impairment or pain, but it is more likely to have been due to concerns about having a MoM THA, elevated metal ion levels, or radiological findings such as pseudotumors. However, PROs capture a different aspect of outcome after THA than revisions.
Noise
We found a prevalence of noise from CoC THA of 27%, which is lower than the prevalence of 33% reported by Jarrett et al. (Citation2009). For MoM bearings, however, the prevalence of noise of 29% in our study was much higher than that already reported for squeaking (1.5%) (Bernasek et al. Citation2011). The prevalence of noise from MoP THAs in our study was 3 times the prevalence of 4% reported earlier (Jarrett et al. Citation2009). This might be explained by differences in reporting noise. In the study by Jarrett et al. (Citation2009), the patients answered a questionnaire at follow-up visits, and patients who were unable to come in for the visits were interviewed by telephone, whereas in the study by Bernasek et al. (Citation2011), all the patients were interviewed by telephone. Thus, differences in questionnaires and methods might give different results. Satisfaction or PROs was described in several studies on squeaking CoC THAs. Sexton et al. (Citation2011) found that a squeaking THA had similar patient satisfaction or Harris hip score (HHS) as silent hips. Other authors have reported similar HHS, SF-36, or WOMAC in patients with and without squeaking CoC THAs (Restrepo et al. Citation2010). These reports contrast with our findings. However, in a recent study, noise was found to be associated with pain (Nam et al. Citation2016). The cause of noise from THAs may be multifactorial, but an association between higher inclination angle and squeaking was found in MoM THAs (Bernasek et al. Citation2011), and CoC THAs with an acetabular component orientation outside the range between 15° and 35° of anteversion and between 35° and 55° of inclination were more likely to produce squeaking (Walter et al. Citation2007).
The patient-acceptable symptom state (PASS) of 3 HOOS subscales, EQ-5D index, and EQ VAS 1 year postoperatively has been estimated. The PASS was 91 for HOOS Pain, 88 for HOOS Sport, 83 for HOOS QoL, 0.92 for EQ-5D index, and 85 for EQ VAS (Paulsen et al. Citation2014). In the present study, only the crude mean of HOOS Pain, HOOS QoL, and EQ-5D index for silent THAs almost reached values for PASS, whereas PROM scores for noisy THAs were worse. This indicates that THAs with noise may not only have statistical significance but also clinical significance when compared to silent THAs. In contrast, we consider the significantly worse adjusted mean difference for HOOS Symptoms of −2.3 for the CoC group compared to the MoP group not to be clinically relevant.
Methodological considerations
The strengths of the present study included the nationwide population-based design. The registries that provided data for the study have a documented good overall validity (Andersen et al. Citation1999, Pedersen et al. Citation2004, Citation2006). Furthermore, the PROMs used in the study are all well validated (Brooks Citation1996, Nilsdotter et al. Citation2003, Naal et al. Citation2009, Wittrup-Jensen et al. Citation2009, Thorborg et al. Citation2010, Paulsen et al. Citation2012b, Citation2014), and the response rate was high.
The study also had several limitations. The matching and selection of patients was based on those who had received a CoC THA. These patients had a greater proportion of males, were younger, and had less comorbidity than patients with MoP THA, which might result in confounding by indication. Furthermore, since the response rate depended slightly on the type of bearing, we may have introduced selection bias in the study. Also, the question about onset of noise from the THA may be influenced by recall bias. Although the questions about noise from the THA had been tested before administration, the questions were not psychometrically validated, and no retests were performed before they were administered.
In order to reduce the confounding effects of sex, age, and follow-up time, patients with MoM and MoP THAs were matched to patients with CoC THAs according to sex, age at primary surgery, and year of surgery. As it was impossible to identify a unique match in patients with MoM and MoP bearings for all the patients with CoC THAs, some patients with MoM and MoP THAs were matched to more than 1 CoC THA patient. To maintain the matched design, 2 responders with different bearings should have been excluded, if their unique match with the third bearing was a non-responder. This would have reduced the study population substantially. Thus, when performing the regression analyses, the matching was ignored and instead adjustments for sex, age, and year of surgery were performed to account for these confounders. Surgical approach was not adjusted for, since 96% of patients undergoing primary THA in Denmark have been operated through a posterolateral approach (Danish Hip Arthroplasty Registry Citation2015). There might still have been the possibility of unmeasured confounding, as we had no information of the patient’s preoperative function, smoking habits, civil status, educational level, or income.
The quality of PROM data depends on the proportion of missing data. Missing data were managed in accordance with the specifications in the manual for each PROM, and the amount of missing data was lower than seen in previous studies on Danish THA patients (Paulsen et al. Citation2012b). The very low proportion of missing data in the present study would not have had any substantial influence on our results.
Conclusion
In this nationwide, population-based cross-sectional study, we found similar mean scores in the 5 HOOS subscales, EQ-5D index, EQ VAS, and UCLA activity score in patients with a CoC, MoM, or MoP THA after a mean follow-up of 7, 5, and 7 years, respectively. 27% of patients with CoC bearings, 29% of patients with MoM bearings, and 12% of patients with MoP bearings had experienced noise from their THA. There were worse mean subscale scores for all types of bearings and subscales when comparing noisy THAs with silent MoP THAs, except for patients with noisy CoC and MoM THAs who had mean UCLA activity scores similar to those in patients with silent MoP THAs. The most unfavorable PROM scores were found for noisy MoP THAs, which may have clinical significance.
Supplementary data
Tables 4–8, and 10 are available on the website of Acta Orthopaedica (www.acta-orthop.org), identification number 9804.
All the authors designed the study protocol. CV and ABP collected the data. The analyses were planned by all the authors and they were carried out by CV. CV wrote the initial draft of the manuscript, which was critically revised by all the authors.
The study was supported financially by the Danish Rheumatism Association and the Region of Southern Denmark.
- Amstutz H C, Thomas B J, Jinnah R, Kim W, Grogan T, Yale C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am 1984; 66 (2): 228–41.
- Andersen T F, Madsen M, Jorgensen J, Mellemkjoer L, Olsen J H. The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 1999; 46 (3): 263–8.
- Bellamy N, Buchanan W W, Goldsmith C H, Campbell J, Stitt L W. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988; 15 (12): 1833–40.
- Bernasek T, Fisher D, Dalury D, Levering M, Dimitris K. Is metal-on-metal squeaking related to acetabular angle of inclination? Clin Orthop Relat Res 2011; 469 (9): 2577–82.
- Brooks R. EuroQol: the current state of play. Health Policy 1996; 37 (1): 53–72.
- Capello W N, D’Antonio J A, Feinberg J R, Manley M T, Naughton M. Ceramic-on-ceramic total hip arthroplasty: update. J Arthroplasty 2008; 23 (7 Suppl): 39–43.
- Charlson M E, Pompei P, Ales K L, MacKenzie C R. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40 (5): 373–83.
- Danish Hip Arthroplasty Registry. Annual Report 2015. 2015.
- Dolan P, Gudex C, Kind P, Williams A. The time trade-off method: results from a general population study. Health Econ 1996; 5 (2): 141–54.
- Groot V d, Beckerman H, Lankhorst G J, Bouter L M. How to measure comorbidity: a critical review of available methods. J Clin Epidemiol 2003; 56 (3): 221–9.
- Harrell F E. Regression modeling strategies: with applications to linear models, logistic regression, and survival analysis. Springer, New York 2001.
- Jacobs J J, Shanbhag A, Glant T T, Black J, Galante J O. Wear Debris in Total Joint Replacements. J Am Acad Orthop Surg 1994; 2 (4): 212–20.
- Jameson S S, Mason J M, Baker P N, Gregg P J, Deehan D J, Reed M R. No functional benefit of larger femoral heads and alternative bearings at 6 months following primary hip replacement. Acta Orthop 2015; 86 (1): 32–40.
- Jarrett C A, Ranawat A S, Bruzzone M, Blum Y C, Rodriguez J A, Ranawat C S. The squeaking hip: a phenomenon of ceramic-on-ceramic total hip arthroplasty. J Bone Joint Surg (Am) 2009; 91 (6): 1344–9.
- Klassbo M, Larsson E, Mannevik E. Hip disability and osteoarthritis outcome score. An extension of the Western Ontario and McMaster Universities Osteoarthritis Index. Scand J Rheumatol 2003; 32 (1): 46–51.
- Lucht U. The Danish Hip Arthroplasty Register. Acta Orthop Scand 2000; 71 (5): 433–9.
- Nam D, Barrack T, Johnson S R, Nunley R M, Barrack R L. Hard-on-hard bearings are associated with increased noise generation in young patients undergoing hip arthroplasty. Clin Orthop Relat Res 2016. [Epub ahead of print]
- Nilsdotter A K, Lohmander L S, Klassbo M, Roos E M. Hip disability and osteoarthritis outcome score (HOOS)–validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 2003; 4: 10.
- Naal F D, Impellizzeri F M, Leunig M. Which is the best activity rating scale for patients undergoing total joint arthroplasty? Clin Orthop Relat Res 2009; 467 (4): 958–65.
- Owen D H, Russell N C, Smith P N, Walter W L. An estimation of the incidence of squeaking and revision surgery for squeaking in ceramic-on-ceramic total hip replacement: a meta-analysis and report from the Australian Orthopaedic Association National Joint Registry. Bone Joint J 2014; 96-B (2): 181–7.
- Paulsen A, Overgaard S, Lauritsen J M. Quality of data entry using single entry, double entry and automated forms processing-an example based on a study of patient-reported outcomes. PLoS One 2012a; 7 (4): e35087.
- Paulsen A, Pedersen A B, Overgaard S, Roos E M. Feasibility of 4 patient-reported outcome measures in a registry setting. Acta Orthop 2012b; 83 (4): 321–7.
- Paulsen A, Roos E M, Pedersen A B, Overgaard S. Minimal clinically important improvement (MCII) and patient-acceptable symptom state (PASS) in total hip arthroplasty (THA) patients 1 year postoperatively. Acta Orthop 2014; 85 (1): 39–48.
- Pedersen A, Johnsen S, Overgaard S, Soballe K, Sorensen H T, Lucht U. Registration in the danish hip arthroplasty registry: completeness of total hip arthroplasties and positive predictive value of registered diagnosis and postoperative complications. Acta Orthop Scand 2004; 75 (4): 434–41.
- Pedersen C B, Gotzsche H, Moller J O, Mortensen P B. The Danish Civil Registration System. A cohort of eight million persons. Dan Med Bull 2006; 53 (4): 441–9.
- Restrepo C, Matar W Y, Parvizi J, Rothman R H, Hozack W J. Natural history of squeaking after total hip arthroplasty. Clin Orthop Relat Res 2010; 468 (9): 2340–5.
- Schmidt M, Pedersen L, Sorensen H T. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 2014; 29 (8): 541–9.
- Schmidt M, Schmidt S A, Sandegaard J L, Ehrenstein V, Pedersen L, Sorensen H T. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449–90.
- Sexton S A, Yeung E, Jackson M P, Rajaratnam S, Martell J M, Walter W L, Zicat B A, Walter W K. The role of patient factors and implant position in squeaking of ceramic-on-ceramic total hip replacements. J Bone Joint Surg Br 2011; 93 (4): 439–42.
- Smith A J, Wylde V, Berstock J R, Maclean A D, Blom A W. Surgical approach and patient-reported outcomes after total hip replacement. Hip Int 2012; 22 (4): 355–61.
- Swanson T V, Peterson D J, Seethala R, Bliss R L, Spellmon C A. Influence of prosthetic design on squeaking after ceramic-on-ceramic total hip arthroplasty. J Arthroplasty 2010; 25 (6 Suppl): 36–42.
- The EuroQol Group. EuroQol - a new facility for the measurement of health-related quality of life. Health Policy 1990; 16 (3): 199–208.
- Thorborg K, Roos E M, Bartels E M, Petersen J, Holmich P. Validity, reliability and responsiveness of patient-reported outcome questionnaires when assessing hip and groin disability: a systematic review. Br J Sports Med 2010; 44 (16): 1186–96.
- Thygesen S K, Christiansen C F, Christensen S, Lash T L, Sorensen H T. The predictive value of ICD-10 diagnostic coding used to assess Charlson comorbidity index conditions in the population-based Danish National Registry of Patients. BMC Med Res Methodol 2011; 11: 83.
- Varnum C, Pedersen A B, Kjaersgaard-Andersen P, Overgaard S. Comparison of the risk of revision in cementless total hip arthroplasty with ceramic-on-ceramic and metal-on-polyethylene bearings. Acta Orthop 2015a; 86 (4): 477–84.
- Varnum C, Pedersen A B, Makela K, Eskelinen A, Havelin L I, Furnes O, Karrholm J, Garellick G, Overgaard S. Increased risk of revision of cementless stemmed total hip arthroplasty with metal-on-metal bearings. Acta Orthop 2015b; 86 (4): 469–76.
- Walter W L, O’Toole G C, Walter W K, Ellis A, Zicat B A. Squeaking in ceramic-on-ceramic hips: the importance of acetabular component orientation. J Arthroplasty 2007; 22 (4): 496–503.
- Wittrup-Jensen K U, Lauridsen J, Gudex C, Pedersen K M. Generation of a Danish TTO value set for EQ-5D health states. Scand J Public Health 2009; 37 (5): 459–66.