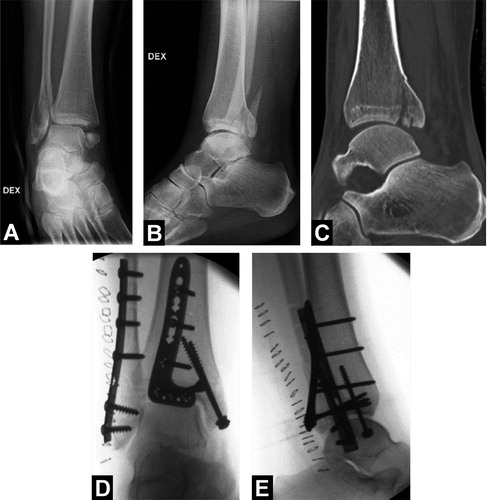
A 39-year-old previously healthy woman sustained a dislocated trimalleolar ankle fracture as a result of a low-energy twisting injury. The fracture was reduced and stabilized at the emergency department (). After reduction, the foot was vital and sensation and motor function were normal. Because of the tendency of the ankle joint to dislocate posteriorly, we decided to fix the posterior malleolar fracture with an anatomic locking plate through a posterolateral approach.
Figure 1. A and B.The trimalleolar ankle fracture following closed reduction at the emergency department. C. Computed tomography revealing the extent of the posterior malleolar fracture. D and E. Intraoperative fluoroscopic images.
The surgery went according to plan and postoperative radiographs were considered acceptable (). However, during the first postoperative day the patient developed severe pain in her foot that was unresponsive to pain medication. Sensation was impaired at the dorsal and plantar aspects of the foot. Active flexion of toes was intact, but passive extension of the foot caused pain at the level of the ankle. The foot was warm, but neither the dorsalis pedis artery nor the posterior tibial artery was palpable or could be detected with Doppler ultrasound. Because of the absent distal pulses, a computed tomography angiography (CTA) was performed 24 h after surgery. The CTA revealed a bilateral dominant peroneal artery as the only artery supplying vascularity to the foot (). However, vascular occlusion was not evident on CTA. Because of the intense pain, urgent revision surgery was done 36 h after primary surgery. During the surgery, a sural nerve entrapment in the subcutaneous sutures was observed.The nerve was liberated, the peroneal muscles were found to be vital, and there were no signs of compartment syndrome. It is, however, noteworthy that posterior neurovascular structures were not explored during the procedure.
Figure 2. Computed tomography angiography revealing a vascular anomaly where a bilateral dominant peroneal artery was the only artery supplying vascularity to the foot.

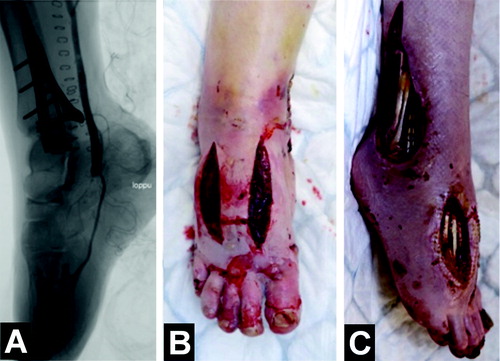
After the revision surgery, pain in the foot became worse, awakening suspicion of vascular impairement or damage to the posterior tibial nerve, and a re-revision surgery was performed on the day after the first revision. In the re-revision surgery, the posterior tibial nerve was found to be intact, but the peroneal artery was pulseless, running on top of the posterior plate. The patient was referred to the Department of Vascular Surgery, where a catheter-directed thrombolysis was performed twice to dissolve the clot (). However, the peroneal artery kept clotting and a bypass surgery and fasciotomies of the foot were eventually required 5 days after the first surgery (). Despite successful vascular reconstruction, the patient developed severe ischemic damage in her foot with persistent intense pain and extensive soft tissue necrosis, which ultimately led to a transtibial amputation.
Figure 3. Angiography showing occlusion of the peroneal artery at the level of the tip of the posterior plate (white arrows). Despite efforts to dissolve the occlusion with catheter-directed thrombolysis, the artery kept clotting.
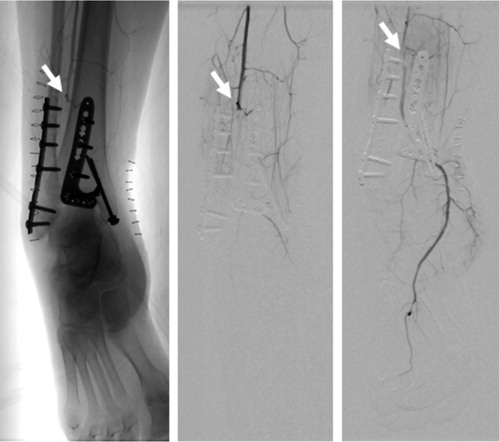
Figure 4. A. Occlusion of the peroneal artery was bypassed with a vein graft, and control angiography of the bypass graft showed blood flow to the plantar and digital arteries. B. Fasciotomies were performed due to the risk of compartment syndrome following revascularization. C. Despite the bypass, the patient developed severe ischemic damage, resulting in persistent foot pain and extensive soft tissue necrosis.
Discussion
In ankle fractures involving the posterior malleolus, there has recently been an increased interest in simultaneous plate fixation of both the posterior malleolus and the fibular fracture through a posterolateral approach (Little et al. Citation2013). Studies have shown that fixation of the posterior malleolus increases the stability of the tibiofibular joint, and may therefore improve the clinical outcome (Gardner et al. Citation2006, Miller et al. Citation2010, Irwin et al. Citation2013). Clinical studies have also noted fewer major wound complications in patients treated with a posterolateral approach (Little et al. Citation2013), although the neurovascular structures are at higher risk (Jowett et al. Citation2010, Lidder et al. Citation2014).
The sural nerve provides sensation to the lateral aspect of the foot, and entrapment of the nerve can cause numbness and pain to this area of the foot (Talbot et al. Citation2005, Jowett et al. Citation2010). It lies subcutaneously in the posterolateral aspect of the ankle and can be easily damaged when using a posterolateral approach to the ankle (Talbot et al. Citation2005, Jowett et al. Citation2010). It is therefore important to identify the nerve and protect it during the operation, especially during wound closure. In our patient, a subcutaneous suture accidentally entrapped the sural nerve, causing not only pain and numbness in the lateral aspect of the foot but also an important delay in diagnosing the critical problem, ultimately leading to a transtibial lower leg amputation. To our knowledge, a severe pain in the entire foot is not a typical finding in patients with a solitary sural nerve entrapment, and with such findings other reasons for numbness and intensive pain should be assessed—which, however, was erroneously not done in our patient. Furthermore, as compartment syndrome of the foot is very rare following ankle fracture surgery (Guo et al. Citation2010, Neilly et al. Citation2015), vascular impairment must be considered when a patient presents after surgery with pain that is disproportionate to the extent of the injury.
The main vascular supply to the foot is normally provided by the tibialis posterior, the tibialis anterior, and the peroneal arteries (Kelikian and Sarrafian Citation2011). Importantly, a recent systematic review showed that in 5% of patients the peroneal artery may be a dominant artery supplying blood flow to the foot (Abou-Foul and Borumandi Citation2016).
Bifurcation of the peroneal artery may be located as close as 4 cm from the tibial plafond, making the posterior branch of the peroneal artery susceptible to injury during plating of the posterior malleolus (Lidder et al. Citation2014). In patients with lower extremity pulses that are not palpable, a noninvasive CTA should be performed to exclude any vascular anomalies. In our patient, the distal pulses were not palpable, although the foot was warm. The CTA revealed a dominant peroneal artery. Notably, there appeared to be adequate blood flow to the foot, and the occlusion of the artery was not evident on the CTA. We believe that the plate may have impeded a proper visualization of the arterial occlusion on the CTA, and that a conventional or digital substraction angiography would have been more accurate.
Anatomic reduction and stable fixation of a posterior malleolar fracture are associated with good functional outcome (van den Bekerom et al. Citation2009) and may reduce the risk of posttraumatic osteoarthritis (Drijfhout van Hoof et al. Citation2015). As anatomic reduction of the posterior fragment can be achieved more easily through the posterolateral approach (Verhage et al. Citation2016), this approach can be recommended for patients with more complicated posterior malleolar ankle fracture patterns. A recent study showed that there was no difference in functional outcome following screw or plate fixation of the posterior malleolar fragment (Erdem et al. Citation2014). Thus, in younger patients with good bone quality and also in patients with non-comminuted posterior malleolar fractures, less invasive screw fixation should probably be used instead of bulky plates—especially in patients without posterior instability following fixation of both medial and lateral malleoli. We believe that in our patient, an injury to the dominant posterior vessel could have been avoided without extensive exposure of the posterior malleolus and without application of a bulky posterior locking plate in the posterior part of the ankle.
The fixation of the ankle fracture in our patient followed current recommendations. However, the vascular anomaly resulted in a devastating complication following simple ankle fracture surgery. With this disaster, some important points should be considered. Firstly, in younger patients with good bone quality, screws should probably be used instead of bulky plates for posterior malleolar fragment fixation. Secondly, in patients with metal implants close to the vessel, the implants may impede proper interpretation of a CTA, and a conventional angiography would be more accurate in detecting vascular injury. Thirdly, a clinical examination of the vascular status both pre- and postoperatively is utterly important in patients with ankle fractures. When there is severe pain postoperatively, the surgeon should immediately suspect a vascular injury.
- Abou-Foul A K, Borumandi F. Anatomical variants of lower limb vasculature and implications for free fibula flap: Systematic review and critical analysis. Microsurgery 2016; 36 (2): 165–72.
- Drijfhout van Hooff C C, Verhage S M, Hoogendoorn J M. Influence of fragment size and postoperative joint congruency on long-term outcome of posterior malleolar fractures. Foot Ankle Int 2015; 36 (6): 673–8.
- Erdem M N, Erken H Y, Burc H, Saka G, Korkmaz M F, Aydogan M. Comparison of lag screw versus buttress plate fixation of posterior malleolar fractures. Foot Ankle Int 2014; 35 (10): 1022–30.
- Gardner M J, Brodsky A, Briggs S M, Nielson J H, Lorich D G. Fixation of posterior malleolar fractures provides greater syndesmotic stability. Clin Orthop Relat Res 2006; 447: 165–71.
- Guo S, Sethi D, Prakash D. Compartment syndrome of the foot secondary to fixation of ankle fracture–a case report. Foot Ankle Surg 2010; 16 (3): e72–5.
- Irwin T A, Lien J, Kadakia A R. Posterior malleolus fracture. J Am Acad Orthop Surg 2013; 21(1): 32–40.
- Jowett A J, Sheikh F T, Carare R O, Goodwin M I. Location of the sural nerve during posterolateral approach to the ankle. Foot Ankle Int 2010; 31 (10): 880–3.
- Kelikian A S, Sarrafian S (eds). Sarrafian’s anatomy of the foot and ankle: descriptive, topographic, functional (3rd ed). Philapdelphia. Lippincot Williams & Wilkins 2011.
- Lidder S, Masterson S, Dreu M, Clement H, Grechenig S. The risk of injury to the peroneal artery in the posterolateral approach to the distal tibia: a cadaver study. J Orthop Trauma 2014; 28 (9): 534–7.
- Little M T, Berkes M B, Lazaro L E, Sculco P K, Helfet D L, Lorich D G. Complications following treatment of supination external rotation ankle fractures through the posterolateral approach. Foot Ankle Int 2013; 34 (4): 523–9.
- Miller A N, Carroll E A, Parker R J, Helfet D L, Lorich D G. Posterior malleolar stabilization of syndesmotic injuries is equivalent to screw fixation. Clin Orthop Relat Res 2010; 468 (4): 1129–35.
- Neilly D, Baliga S, Munro C, Johnston A. Acute compartment syndrome of the foot following open reduction and internal fixation of an ankle fracture. Injury 2015; 46 (10): 2064–8.
- Talbot M, Steenblock T R, Cole P A. Posterolateral approach for open reduction and internal fixation of trimalleolar ankle fractures. Can J Surg 2005; 48 (6): 487–90.
- van den Bekerom M P, Haverkamp D, Kloen P. Biomechanical and clinical evaluation of posterior malleolar fractures. A systematic review of the literature. J Trauma 2009; 66 (1): 279–84.
- Verhage S M, Boot F, Schipper I B, Hoogendoorn J M. Open reduction and internal fixation of posterior malleolar fractures using the posterolateral approach. Bone Joint J 2016; 98-B (6): 812–7.
