Patient 1
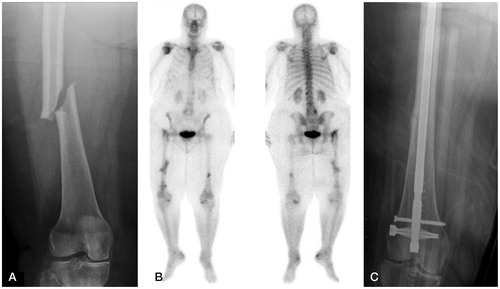
A 75-year-old woman with a history of metastatic breast and non-small-cell lung cancer tripped and fell onto her hip. Radiographs showed a right mid-shaft diaphyseal femoral fracture and the patient underwent anterograde intramedullary fixation (). The patient’s breast cancer was metastatic to the left iliac wing and spinal vertebra. She had been receiving monthly denosumab injections for the previous 2 years to help control her metastatic disease, and denied having any antecedent symptoms. Despite the fact that there was no evidence of malignancy upon histological review of intraoperative reamings, it was first assumed that the fracture resulted from a metastatic lesion. In retrospect, the initial fracture had the appearance of an atypical femoral fracture (AFF). The patient continued on denosumab and her right femur fracture healed, but 8 months later she developed insidious intermittent pain in her left thigh. The patient visited her oncologist after 1 month of symptoms, at which point radiographs and a bone scan were performed to rule out malignancy (). The bone scan did show increased activity in the left distal femoral diaphysis. The day after the scan, the patient fell and radiographs revealed a left distal-third femoral fracture showing atypical features, including lateral cortical thickening, for which she underwent retrograde intramedullary fixation ().
Figure 1. Patient 1. A. The right femur; initial atypical fracture. B. Bone scan imaging obtained to evaluate the presence of metastatic disease, demonstrating increased uptake in the left distal diaphysis of the femur. This uptake indicated stress changes within the bone prior to the completed atypical femoral fracture. C. Retrograde intramedullary nail fixation.
Patient 2
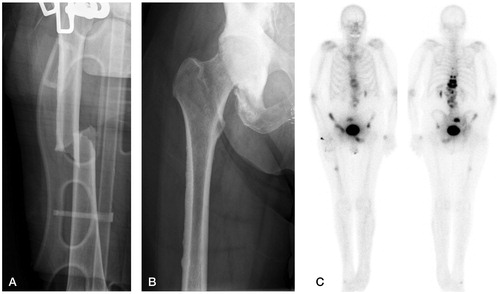
An 86-year-old man with a history of metastatic prostate cancer fell and radiographs showed a right transverse mid-shaft diaphyseal femoral fracture with lateral cortical thickening consistent with an atypical fracture (). The patient was treated with an anterograde intramedullary nail and the histology of intraoperative reamings was negative for malignancy. The patient had begun monthly denosumab treatments 3.5 years before the fracture to address metastatic disease in his pelvis and spine. In the year before his fracture, the patient noted right thigh pain and a radiograph taken 5 months before the fracture showed lateral cortical thickening of the diaphysis of his femur (). A bone scan at the time of this radiography showed increased uptake, and the lesion was deemed to be metastatic disease (). The patient was evaluated by an orthopedic surgeon who judged it to be a metastatic lesion, and this was followed by local irradiation of the thigh. 1 month before the injury, and after completing radiation, the patient was seen for orthopedic follow-up and continued to report thigh pain but no further intervention was pursued.
Figure 2. Patient 2. A. The right femur; atypical fracture. B. The right femur after the patient developed thigh pain, showing lateral cortical thickening of the diaphysis. C. Bone scan imaging obtained to evaluate the presence of metastatic disease, showing increased uptake in the right mid-diaphysis of the femur. This uptake was first thought to represent metastatic disease, although it ultimately proved to indicate stress changes within the bone prior to the completed atypical femur fracture.
Discussion
Anti-resorptive medications, primarily bisphosphonates, are used to treat osteoporosis and to help with pain related to metastatic bone disease. A possible complication of anti-resorptive medication is an atypical femoral fracture (AFF), which occurs most often in the femoral shaft (Koeppen Citation2013). Bisphosphonates bind to hydroxyapatite crystals in bone matrix, ultimately leading to decreased bone resorption (Drake et al. Citation2008). While this may lead to improved bone density, it also disrupts the normal homeostatic balance between osteoblasts and osteoclasts. This change may result in accumulation of micro-damage and ultimately an AFF (Mashiba et al. Citation2000, Visekruna et al. Citation2008). The true incidence of these atypical fractures in patients on bisphosphonate medication has been difficult to establish (Schilcher et al. Citation2015).
Denosumab is a more recently developed human monoclonal antibody that binds to the receptor activator of nuclear factor kappa-B ligand (RANK-L), preventing maturation, activation, and survival of osteoclasts (Rizzoli et al. Citation2010). It received FDA approval in 2010 for prevention of skeletal complications in patients with bone metastases and for treatment of post-menopausal women with osteoporosis. Although denosumab functions by a different mechanism than bisphosphonates, both reduce bone resorption. The initial results of the FREEDOM trial, a randomized trial of denosumab in 7,868 women, did not reveal any AFFs in participants (Cummings et al. Citation2009). The subsequent FREEDOM Extension noted only 2 AFFs during treatment with an overall rate of less than 1 fracture per 10,000 subject years (Bone et al. Citation2013, Papapoulos et al. Citation2015). The phase-III trials evaluating the use of denosumab for metastatic skeletal disease and multiple myleoma also did not report any AFFs (Lipton et al. Citation2012). Recently, reports have begun to suggest that denosumab, like bisphosphonates, can lead to the development of AFFs (Paparodis et al. Citation2013, Villiers et al. Citation2013, Drampalos et al. Citation2014, Schilcher and Aspenberg Citation2014, Thompson et al. Citation2014, Khow and Yong Citation2015, Selga et al. Citation2016). We present 2 cases where the patients developed AFFs while taking denosumab on a monthly basis for metastatic cancer, and in which prodromal symptoms were first thought to be related to new metastatic lesions and not to be secondary to developing fractures. We obtained informed written consent from both patients for publication of this report.
6 case reports have presented convincing evidence that AFFs may be associated with denosumab use for osteoporosis (Villiers et al. Citation2013, Drampalos et al. Citation2014, Schilcher and Aspenberg Citation2014, Thompson et al. Citation2014, Khow and Yong Citation2015, Selga et al. 2016). All the previous case reports have described AFFs observed in women receiving denosumab bi-annually for osteoporosis treatment. Our 2 patients apparently developed atypical femur fractures while on monthly denosumab treatment for metastatic malignancy. Patients receiving denosumab to minimize skeletal complications associated with metastatic cancer receive higher dosing (120 mg vs. 60 mg) and more frequent dosing (monthly vs. twice per year) than patients undergoing osteoporosis-related treatment (Lipton et al. Citation2012, Papoulos et al. 2015). The patients with AFFs in previous reports had had previous bisphosphonate therapy, whereas the patients described in this case report had no such exposure. Atypical femoral fractures have previously been reported in patients on high-dose bisphosphonate therapy for malignancy (Puhaindran et al. Citation2011). To our knowledge, there have not been any previous case reports of patients sustaining AFFs while on denosumab treatment for metastatic disease.
Our patients sustained AFFs 2, 3, and 3.5 years after initiation of denosumab therapy. These time intervals before fracture are longer than in previous reports, which have noted fractures after 1 week to 18 months of treatment (Paparodis et al. Citation2013, Villiers et al. Citation2013, Drampalos et al. Citation2014, Schilcher and Aspenberg Citation2014, Thompson et al. Citation2014, Khow and Yong Citation2015, Selga et al. 2016), but these previous reports may have been influenced by previous bisphosphonate use. A study of AFF with high-dose bisphosphonate therapy for malignancy found a median duration of treatment of 6 years (Chang et al. Citation2012), an interval that was notably longer than that observed in our patients.
The fractures observed in our patients met the criteria for an AFF according to the American Society of Bone and Mineral Research 2013 Task Force (Shane et al. Citation2014), in that they were located within the femoral diaphysis and satisfied all 5 major criteria including: low-energy mechanisms, originating from the lateral cortex, involving both cortices, being generally non-comminuted, and showing localized periosteal or endosteal thickening of the lateral cortex. The left femoral fracture observed in the first patient () appears to have been the most distal denosumab-induced AFF reported so far, requiring a retrograde nail, while still maintaining the classic hallmarks of an AFF.
As with our first patient, previous reports have highlighted the high frequency of bilateral involvement of denosumab-related AFFs with 1 case of simultaneous fractures (Selga et al. 2016), 2 cases with concurrent changes (Villiers et al. Citation2013, Thompson et al. Citation2014), and 1 case of sequential AFFs approximately 1 year apart (Drampalos et al. Citation2014). There have been similar findings in patients on high-dose bisphosphonate treatment for skeletal metastases, with 5 of 6 patients showing bilateral involvement in one series (Chang et al. Citation2012). In our patient, the initial fracture was not recognized as an AFF at the time—and was only recognized in retrospect at the time of the second fracture. Similarly, the initial cortical thickening, thigh pain, and increased uptake on bone scan in the second patient was misdiagnosed as metastatic disease, even after orthopedic evaluation. In a patient on denosumab treatment for metastatic cancer, the diagnostic differential for thigh pain must include an atypical femoral fracture that may require cessation of the medication and weight-bearing restrictions or prophylactic fixation.
- Bone H G, Chapurlat R, Brandi M, Brown J P, Czerwinski E, Krieg M A, Mellstrom D, Radominski S C, Reginster J Y, Resch H, Ivorra JA, Roux C, Vittinghoff E, Daizadeh N S, Wang A, Bradley M N, Franchimont N, Geller M L, Wagman R B, Cummings S R, Papapoulos S. The effect of three or six years of denosumab exposure in women with postmenopausal osteoporosis: Results from the FREEDOM extension. J Clin Endocrinol Metab 2013; 98(11): 4483–92.
- Chang S T, Tenforde A S, Grimsrud C D, O’Ryan F S, Gonzalez J R, Baer D M, Chandra M, Lo J C. Atypical femur fractures among breast cancer and multiple myeloma patients receiving intravenous bisphosphonate therapy. Bone 2012; 51(3): 524–7.
- Cummings S R, Martin J S, McClung M R, Siris E S, Eastell R, Reid I R, Delmas P, Zoog H B, Austin M, Wang A, Kutilek S, Adami S, Zanchetta J, Libanati C, Siddhanti S, Christiansen C, FREEDOM Trial. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 2009; 361(8): 756–65.
- Drake M T, Clarke B L, Khosla S. Bisphosphonates: Mechanism of action and role in clinical practice. Mayo Clin Proc 2008; 83(9): 1032–45.
- Drampalos E, Skarpas G, Barbounakis N, Michos I. Atypical femoral fractures bilaterally in a patient receiving denosumab. Acta Orthop 2014; 85(1): 3–5.
- Khow K S F, Yong T Y. Atypical femoral fracture in a patient treated with denosumab. J Bone Miner Metab 2015; 33(3): 355–8.
- Koeppen V A, Schilcher J, Aspenberg P. Dichotomous location of 160 atypical femur fractures. Acta Orthop 2013; 84(6): 561–4.
- Lipton A, Fizazi K, Stopeck A T, Henry D H, Smith M R, Shore N, Martin M, Vadhan-Raj S, Brown J E, Richardson G E, Saad F, Yardley D A, Zhou K, Balakumaran A, Braun A. Superiority of denosumab to zoledronic acid for prevention of skeletal-related events: A combined analysis of 3 pivotal, randomised, phase 3 trials. Eur J Cancer 2012; 48(16): 3082–92.
- Mashiba T, Hirano T, Turner C H, Forwood M R, Johnston C C, Burr D B. Suppressed bone turnover by bisphosphonates increases microdamage accumulation and reduces some biomechanical properties in dog rib. J Bone Miner Res 2000; 15(4): 613–20.
- Papapoulos S, Lippuner K, Roux C, Lin C J, Kendler D L, Lewiecki E M, Brandi M L, Czerwinski E, Franek E, Lakatos P, Mautalen C, Minisola S, Reginster J Y, Jensen S, Daizadeh N S, Wang A, Gavin M, Libanati C, Wagman R B, Bone H G. The effect of 8 or 5 years of denosumab treatment in postmenopausal women with osteoporosis: Results from the FREEDOM extension study. Osteoporos Int 2015; 26(12): 2773–83.
- Paparodis R, Buehring B, Pelley E, Binkley N. A case of an unusual subtrochanteric fracture in a patient receiving denosumab. Endocr Pract 2013; 19(3): e64–e68.
- Puhaindran M E, Farooki A, Steensma M R, Hameed M, Healey J H, Boland P J. Atypical subtrochanteric femoral fractures in patients with skeletal malignant involvement treated with intravenous bisphosphonates. J Bone Joint Surg Am 2011; 93(13): 1235–42.
- Rizzoli R, Yasothan U, Kirkpatrick P. Denosumab. Nat Rev Drug Discov 2010; 9(8): 591–2.
- Schilcher J, Aspenberg P. Atypical fracture of the femur in a patient using denosumab–a case report. Acta Orthop 2014; 85(1): 6–7.
- Schilcher J, Koeppen V, Aspenberg P, Michaëlsson K. Risk of atypical femoral fracture during and after bisphosphonate use: Full report of a nationwide study. Acta Orthop 2015; 86(1): 100–7.
- Selga J, Nuñez J, Minguell J, Lalanza M, Garrido M. Simultaneous bilateral atypical femoral fracture in a patient receiving denosumab: Case report and literature review. Osteoporos Int 2016; 27(2): 827–32.
- Shane E, Burr D, Abrahamsen B, Adler RA, Brown TD, Cheung AM, Cosman F, Curtis JR, Dell R, Dempster DW, Ebeling PR, Einhorn, Genant HK, Geusens P, Klaushofer K, Lane JM, McKiernan F, McKinney R, Ng A, Nieves J, O’Keefe R, Papapoulous S, Howe TS, van der Meulen MC, Weinstein RS. Atypical subtrochanteric and diaphyseal femoral fractures: Second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 2014; 29(1): 1–23.
- Thompson R N, Armstrong C L, Heyburn G. Bilateral atypical femoral fractures in a patient prescribed denosumab—a case report. Bone 2014; 61: 44–7.
- Villiers J, Clark D W, Jeswani T, Webster S, Hepburn A L. An atraumatic femoral fracture in a patient with rheumatoid arthritis and osteoporosis treated with denosumab. Case Rep Rheumatol 2013; 2013: 249872.
- Visekruna M, Wilson D, McKiernan F E. Severely suppressed bone turnover and atypical skeletal fragility. J Clin Endocrinol Metab 2008; 93(8): 2948–52.
