Abstract
Background and purpose — There has been increasing alarm regarding metal-on-metal (MoM) joint replacements leading to elevated levels of metal ions and adverse reactions to metal debris (ARMDs). There is little information available concerning the prevalence of and risk factors for these adverse reactions, except with MoM hip joint replacements. We determined the levels of metal ions in blood and the rate of revision due to ARMDs in patients treated with MoM hinge total knee arthroplasty (TKA).
Patients and methods — 22 patients with TKAs and MoM hinge connecting mechanisms were studied for whole-blood chromium and cobalt levels at 6 months, 1 year, and/or ≥2 years after surgery. Possible ARMDs were investigated by MRI. 12 patients with TKAs and metal-on-polyethylene (MoP) connecting mechanisms served as controls.
Results — The cobalt levels were over 5 ppb in 19 of the 22 patients in the MoM group and in 1 of the 12 patients in the MoP group. The chromium levels were over 5 ppb in 11 of the 22 patients in the MoM group and in none of the 12 patients in the MoP group. Pseudotumors were operated in 4 of the 22 patients in the MoM group and in none of the patients in the MoP group.
Interpretation — Our results clearly show that the MoM hinge TKA carries a high risk of increased levels of systemic metal ions and also local ARMD, leading to complicated knee revisions. We therefore discourage the use of MoM hinge TKA.
Large bone and soft tissue defects are often encountered at treatment of bone tumors and treatment of failed primary knee replacements. Reconstruction often requires constrained hinge knee implants.
To increase the mechanical durability of the hinge mechanism, a metal-on-metal (MoM) hinge was developed in the early 2000s. It made use of the widely used MoM concept in hip replacement. Modern machinery and tribology enabled the construction of precise metal articulations, which (at least in simulator tests) demonstrated superior mechanical properties and less wear, making it possible to also redesign the restricted rotating hinge knee. However, there has been an alarmingly high incidence of adverse reactions to metal debris (ARMDs) in patients with MoM hip replacements (Cohen Citation2012), which has led to questions about the fate of the MoM hinge knee replacements. We conducted a case-control study in patients with either bone tumors or complicated knee revisions using hinge TKA MoM. We compared blood metal ion concentrations in patients with MoM hinge TKAs and with metal-on-polyethylene (MoP) hinge TKAs, and also the rates of revision due to ARMDs in patients treated with MoM hinge knee TKR and MoP hinge mechanisms (which acted as a control group).
Patients and methods
Study population
Between September 2010 and December 2014, we performed 22 operations in 22 consecutive patients using the Modular Universal Tumor and Revision System hinge TKA (MUTARS; Implantcast, Buxtehude, Germany) with an MoM connecting mechanism. The mean length of follow-up was 3 (1–6) years. The prosthesis was needed to reconstruct a bone deficit in the distal femur in 17 patients and a bone deficit in the proximal tibia in 5 patients. The indication for surgery was malignant bone tumor in 9 patients and revision arthroplasty in 13 patients. Patients who had had other MoM joints earlier were excluded.
Control group
12 patients who had received the MUTARS hinge knee, which used the PEEK-OPTIMA locking mechanism with an MoP connecting mechanism, served as controls and were consecutively operated on during time intervals from July 2007 to August 2010 and from January 2015 to September 2015, with a mean follow-up of 2 (0–7) years. TKA was needed to reconstruct the bone deficit in the distal femur in all 12 patients. The indication for surgery was malignant bone tumor in 5 patients and revision arthroplasty in 7 patients. We used both CoCr alloy MoM joints and titanium nitride- (TiN-) coated CoCr alloy MoM joints. Patients with other MoM joints were excluded. Demographics for the study population and the control group are summarized in .
Table 1. Clinical and laboratory findings
Serum metal ion analysis, blood collection, and histological analysis
After the recall of the ASR hip resurfacing prosthesis, we established a systematic screening program for all patients with any type of MoM joint. From January 2012, all patients attending this program were examined clinically, including measurement of whole-blood levels of cobalt (Co) and chromium (Cr) ions. MRI was done on bone tumor patients routinely as a follow-up study, mainly to investigate local recurrences—and also for revision patients when they had continuous or progressive symptoms. Revision surgery for ARMD was only considered if the patient had elevated levels of metal ions, a continuously symptomatic knee or progressive symptoms, and a pseudotumor visible by MRI.
Blood metal ion levels were regarded as elevated if either Co or Cr exceeded 5 parts per billion (ppb). Whole-blood samples were collected using a 21-mm gauge needle connected to a Vacutainer system (Becton, Dickinson and Company, Franklin Lakes, NJ) and trace element tubes containing sodium ethylenediaminetetraacetic acid (EDTA). At the Finnish Institute for Occupational Health, standard procedures have been established for the measurement of Co and Cr ions using a dynamic reaction cell inductively coupled plasma (quadrupole) mass spectrometer (Agilent 7500 cx; Agilent Technologies, Santa Clara, CA).
Blood samples were taken at 6 months, 1 year, and/or ≥2 years. MRI scans were taken using two 1.5 T scanners (Siemens Magnetom Avanto; Siemens Healthcare, Erlangen, Germany, and GE Sigma HD; General Electric Healthcare, Wauwatosa, WI) with parameters designed to limit metal artifacts. All MRIs were graded using the MRI pseudotumor grading published by Hart et al. (2012). During revision surgery, tissue samples were collected for histopathological analysis.
Definition of ARMD
Failure was classified as being secondary to ARMD if one of following criteria (Reito et al. Citation2013) was met: metallosis or macroscopic synovitis was present in the joint, a pseudotumor was encountered during revision, and/or a moderate to high number of perivascular lymphocytes was seen in the histopathological specimen with tissue necrosis and/or fibrin deposition. In addition, there was no evidence of component loosening or periprosthetic fracture perioperatively. Infection was ruled out using at least 5 bacterial cultures obtained during revision surgery.
Statistics
Data were analyzed for statistically significant differences between the different implant groups. Due to the asymmetrical distribution of all parameters, non-parametric tests (Kruskal-Wallis test, Mann-Whitney U test) were used. Differences in proportions were assessed using Fisher’s exact test. ANOVA was used to test the effects of 2 outcome variables (Co and Cr) and time/length was used as the exposure variable in MoM patients. The repeated-measures ANOVA was used to test the effects of 2 outcome variables—the Co and Cr levels and time/length of exposure—on the release of ions in MoM patients. Testing for normality of data showed normal distribution, but as there were few data and metal ion concentrations have a tendency to be skewed to the right, logarithmic transformation was performed before the repeated-measures ANOVA test. Mean differencies between time points were close to equal and Mauchly’s test of sphericity was 0.9, supporting sphericity; thus, the sphericity-assumed test was used to analyze statistical significance between groups. Any p-values less than 0.05 were considered to be significant. All analyses were done with SPSS Statistics 21.0.
Results
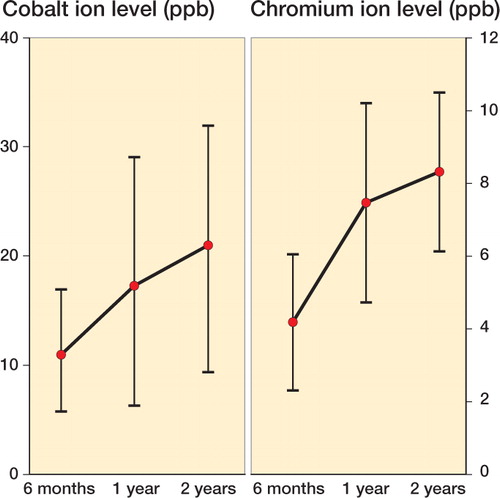
The median and mean whole-blood concentrations of Co and Cr were higher in patients with a MoM hinge prosthesis than in those with a MoP hinge prosthesis (Co: 18 ppb vs. 1.7 ppb; Cr: 6.6 ppb vs. 1.4 ppb; p < 0.001) (, ). The Co levels were more than 5 ppb in 19 of the 22 patients in the MoM group and in 1 of the 12 patients in the MoP group. The Cr levels were more than 5 ppb in 11 of the patients in the MoM group and none of the patients in the MoP group. The Co and Cr levels increased significantly with time (). Co levels increased significantly with time, and they were 11 ppb (95% CI 5.8–17), 17 ppb (CI 6.2–29), and 21 ppb (CI 9.4–31) at 6 months, 1 year, and ≥2 years, respectively (p < 0.001) (). The increase in Cr ions was 4.2 ppb (CI 2.3–6.1), 7.5 ppb (CI 4.7–10), and 8.3 ppb (CI 6.2–11) at 6 months, 1 year, and ≥2 years, respectively (p < 0.001)(). There was no difference in blood metal ion levels in patients with a TiN-coated MoM hinge and in those with a standard MoM hinge.
Figure 1. Comparison of cobalt ion levels (left panel) and chromium ion levels (right panel), in ppb. The bottom, middle, and top horizontal lines of the boxes represent the first quartile, the median, and the third quartile. The ends of the whiskers correspond to the limits of the data, beyond which any values are considered anomalous. Dots show the outler levels measured. The horizontal line corresponds to 5 ppb.
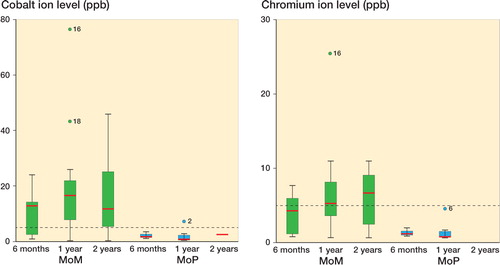
Figure 2. Changes in mean serum cobalt levels (left) and mean serum chromium levels (right)in ppb at different time points, with 95% confidence intervals measured by repeated-measures ANOVA.
Based on MRI, in the MoM group, 8 fluid collections with thick or irregular walls resembling Hart grade 2a pseudotumors were detected. A more solid pseudotumor resembling Hart grade 3 was observed in 2 patients. Mean length was 12 (4–20) cm. All these patients had metal ion levels over 5 ppb. In the MoP group, 2 of the 12 MRIs showed fluid collections and 2 of the 12 images were negative for a fluid signal. All these patients had metal ion levels under 5 ppb. Despite the fact that we systematically used a a metal artifact-reducing sequences (MARS) technique, prosthesis metal caused severe artifacts in all MRIs.
4 patients in the MoM group underwent revision surgery because of pseudotumors. 2 of these patients had received a MoM hinge prosthesis because of bone malignancy and 2 had received one in complicated knee revision arthroplasty (, and ). None of the patients in the MoP group were reoperated. In the MoM group, there was symptomatic cardiac failure in 2 patients with high-grade osteosarcoma. They were also treated with neo- and adjuvant chemotherapy.
Figure 3. Images from a 25-year-old man who had undergone distal femoral replacement 1 year earlier due to a primary bone tumor. He had a swelling in the region of the operated knee. Axial view showed a thin-walled cystic pseudotumor with liquid-like low signal intensity (left panel). Aspirations were repeatedly negative for bacterial growth and showed the typical appearance of metal reaction (right panel).
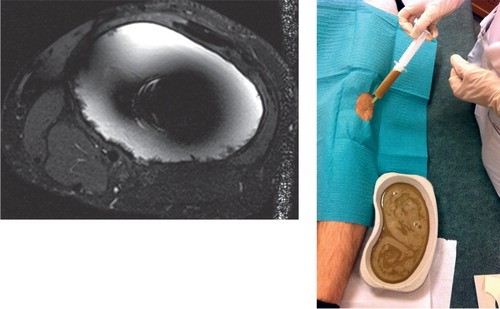
Figure 4. A 72-year-old man had a revision arthroplasty with hinge MoM after multiple failed knee arthroplasty revisions. After 3 years, he developed a massive soft tissue expansion around the distal femur. During revision arthroplasty, a thick-walled pseudotumor with solid components was encountered.

Table 2. Revisions due to adverse reaction to metal debris
Discussion
In this case-control study, we assessed the incidence of having metal ion levels over 5 ppb and ARMD in patients who had undergone a hinge EPR at the distal femur or proximal tibia, with a MoM or MoP joint. We found a strikingly high occurrence of metal ion levels over 5 ppb. Whole-blood metal ion levels exceeding 5 ppb were found in 19 of 22 patients who had received a MoM hinge knee, with the highest values being 77 ppb for Co and 26 ppb for Cr. In 12 patients treated with an otherwise identical hinge knee replacement, except for the MoP hinge mechanism, only a single patient had a Co level of more than 5 ppb.
Metal particles and release of Co and Cr ions from wear and corrosion of orthopedic implants with MoM articulations can cause adverse effects systemically and locally (known as ARMDs) (Langton et al. Citation2010, Citation2011, Lainiala et al. Citation2014, Briggs et al. Citation2015, Chen et al. Citation2016). In MoM total hip joints, the incidences of elevated blood metal ions reported have depended on the prosthesis used, but they have varied between 10% and 30% (Langton Citation2011, Reito et al. Citation2015). The threshold of 5 ppb for abnormal metal ion levels in systemic circulation has been associated with pseudotumor formation (Bisschop et al. Citation2013) and unexplained failure of MoM hips (Hart et al. Citation2011), and is a major reason for revisions in hip arthroplasties (Langton Citation2010). Thus, the high proportion of patients with blood metal ion levels over 5 ppb in our study is most alarming. The indications for performing revision surgery due to ARMD are controversial (Matharu et al. Citation2017). Currently accepted guidelines recommend revision arthroplasty in patients with hip replacement when the patient has abnormalities in imaging and progressively rising Co/Cr levels of more than 7 ppb (Drummondet al. Citation2015). Revision of a TKA because of an evident or suspected ARMD must be carefully considered; the risk of infection leading to amputation is high (Jeys et al. Citation2003, Hardes et al. Citation2006, Shehadeh et al. Citation2010, Dhanoa et al. Citation2015).
Large resections due to bone tumors or complicated revisions lead to dead space surrounding the TKA. This space tends to fill with fluids, and may resemble fluid collections in pseudotumors. In addition, even though the metal artifact reduction sequence technique in MRI produces good-quality images near metal implants, a TKA still causes substantial metal artifacts and reduced visibility close to the hardware, disturbing the analysis of structures and tumorous masses. We had a high proportion of patients with fluid collections around the TKA; however, it is difficult to distinguish between seroma effusion and liquid pseudotumors. In addition, even though a high number of patients with fluid collections had metal ion levels exceeding 5 ppb, the MRI findings might overestimate pseudotumors.
There have been few data published concerning blood metal ion levels following total joint replacements other than total hip arthroplasty. Friesenbichler et al. (Citation2014) reported results following total knee arthroplasty using 3 different fixed-hinge TKAs: the Howmedica Modular Resection System, the Limb Preservation System, and the S-ROM Noiles. They found increased levels of Co and Cr in patients with these prosthesis types (Friesenbichler et al. Citation2014), which is consistent with our results. They proposed that the increased concentration was from corrosion of the implant and conical junctions of the modular parts due to fretting. We hypothesize that the elevated levels of metal ions originate mainly from the MoM hinge mechanism since only the articulating parts of this prosthesis are made of Co-Cr-molybdenum alloy, and titanium segmental parts are connected by screw fixation without any conical junction. We believe that our findings support this hypothesis, as 19 of 22 patients with a TKA using a MoM hinge mechanism had blood metal ion levels over 5 ppb—as compared to only 1 of 12 patients with an identical TKA system apart from the MoP hinge mechanism. For the MoP hinge mechanism to wear out, the PEEK-OPTIMA locking mechanism would have to be broken.
In vitro studies and animal studies have shown a large number of potential adverse effects of implant metals. Documentation of systemic effects in patients with MoM hip replacements has relied much on case reports (Machado et al. Citation2012, Tower Citation2012, Dahmset al. Citation2014). However, 1 recent study has suggested that elevated metal ions may also have an important role in heart failure (Gillam et al. Citation2016). 2 of our patients with extremely high blood metal ion levels also developed heart failure. However, both of these patients had been treated with chemotherapy for their bone sarcoma, which may have induced this. A recent systematic review suggested that a cobalt concentration of less than 300 ppb is unlikely to cause adverse hematopoietic, cardiovascular, neurological, or reproductive system effects (Finley et al. 2012). However, this subject may still be under-reported and under-investigated in patients with MoM joints.
Both blood metal ion measurement and MRI have been useful in the diagnosis of ARMD. However, measurement of metal ions only for systematic screening of ARMD is not supported by the current literature (Pahuta et al. Citation2016). The patients who are operated with hinge TKA are often young bone sarcoma patients treated simultaneously with chemotherapy, or elderly patients with a long history of multiple revisions. Thus, we do not know the value of measuring blood metal ions in these patients for the purpose of screening and diagnosing ARMD. In our patients, the interpretation of MRI findings was challenging. However, we suggest that there should be closer follow-up of such patients—with clinical examination and metal ion measurement. In cases with a clinical abnormality and elevated metal ion levels (> 5 ppb), additional imaging is advisable.
In summary, our results clearly show that this MoM hinge TKA carries a high risk of having elevated levels of systemic metal ions and local ARMD, leading to complicated knee revisions. Thus, we strongly discourage the use of MoM hinge TKA, as there are safer options available.
ML, AE, and JN designed the study. ML, JN, TKP, PN, TL, and KP participated in data collection. ML and AR performed the statistical analyses, ML wrote the first draft, and revised the manuscript. JP performed the histological analysis. All the authors contributed to preparation of the manuscript.
No competing interests declared.
- Bisschop R, Boomsma M F, Van Raay J J, Tiebosch A T, Maas M, Gerritsma C L. High prevalence of pseudotumors in patients with a Birmingham Hip Resurfacing prosthesis: a prospective cohort study of one hundred and twenty-nine patients. J Bone Joint Surg Am 2013; 95 (17): 1554–60.
- Briggs T W, Hanna S A, Kayani B, Tai S, Pollock R C, Cannon S R, Blunn G W, Carrington R W. Metal-on-polyethylene versus metal-on-metal bearing surfaces in total hip arthroplasty: a prospective randomised study investigating metal ion levels and chromosomal aberrations in peripheral lymphocytes. Bone Joint J 2015; 97-B (9): 1183–91.
- Chen S Y, Chang C H, Hu C C, Chen C C, Chang Y H, Hsieh P H. Metal ion concentrations and semen quality in patients undergoing hip arthroplasty: A prospective comparison between metal-on-metal and metal-on-polyethylene implants. J Orthop Res 2016; 34(3): 544–51.
- Cohen D. How safe are metal-on-metal hip implants? BMJ 2012; 344: e1410.
- Dahms K, Sharkova Y, Heitland P, Pankuweit S, Schaefer J R. Cobalt intoxication diagnosed with the help of Dr House. Lancet 2014; 383 (9916): 574.
- Dhanoa A, Ajit Singh V, Elbahri H. Deep Infections after endoprosthetic replacement operations in orthopedic oncology patients. Surg Infect 2015; 16 (3): 323–32.
- Drummond J, Tran P, Fary C. Metal-on-metal hip arthroplasty: a review of adverse reactions and patient management. J Funct Biomater 2015; 6 (3): 486–99.
- Friesenbichler J, Sadoghi P, Maurer-Ertl W, Szkandera J, Glehr M, Ogris K, Wolf M, Weger C, Leithner A. Serum metal ion concentrations in paediatric patients following total knee arthroplasty using megaprostheses. Biomed Res Int 2014; 2014: 817257.
- Gillam M H, Pratt N L, Inacio M C, Roughead E E, Shakib S, Nicholls S J, Graves S E. Heart failure after conventional metal-on-metal hip replacements. Acta Orthop 2016: 1–9. [Epub ahead of print]
- Hardes J, Gebert C, Schwappach A, Ahrens H, Streitburger A, Winkelmann W, Gosheger G. Characteristics and outcome of infections associated with tumor endoprostheses. Arch Orthop Trauma Surg 2006; 126 (5): 289–96.
- Hart A J, Sabah S A, Bandi A S, Maggiore P, Tarassoli P, Sampson B, J A S. Sensitivity and specificity of blood cobalt and chromium metal ions for predicting failure of metal-on-metal hip replacement. J Bone Joint Surg Br 2011; 93 (10): 1308–13.
- Jeys L M, Grimer R J, Carter S R, Tillman R M. Risk of amputation following limb salvage surgery with endoprosthetic replacement, in a consecutive series of 1261 patients. Int Orthop 2003; 27 (3): 160–3.
- Lainiala O, Eskelinen A, Elo P, Puolakka T, Korhonen J, Moilanen T. Adverse reaction to metal debris is more common in patients following MoM total hip replacement with a 36 mm femoral head than previously thought: results from a modern MoM follow-up programme. Bone Joint J 2014; 96-B (12): 1610–7.
- Langton D J, Jameson S S, Joyce T J, Hallab N J, Natu S, Nargol A V. Early failure of metal-on-metal bearings in hip resurfacing and large-diameter total hip replacement: A consequence of excess wear. J Bone Joint Surg Br 2010; 92 (1): 38–46.
- Langton D J, Joyce T J, Jameson S S, Lord J, Van Orsouw M, Holland J P, Nargol A V, De Smet K A. Adverse reaction to metal debris following hip resurfacing: the influence of component type, orientation and volumetric wear. J Bone Joint Surg Br 2011; 93 (2): 164–71.
- Machado C, Appelbe A, Wood R. Arthroprosthetic cobaltism and cardiomyopathy. Heart Lung Circ 2012; 21 (11): 759–60.
- Matharu G S, Pandit H G, Murray D W. Poor survivorship and frequent complications at a median of 10 years after metal-on-metal hip resurfacing revision. Clin Orthop Relat Res 2017; 475(2): 304–14.
- Pahuta M, Smolders J M, van Susante J L, Peck J, Kim P R, Beaule P E. Blood metal ion levels are not a useful test for adverse reactions to metal debris: A systematic review and meta-analysis. Bone Joint Res 2016; 5 (9): 379–86.
- Reito A, Puolakka T, Elo P, Pajamaki J, Eskelinen A. High prevalence of adverse reactions to metal debris in small-headed ASR hips. Clin Orthop Relat Res 2013; 471 (9): 2954–61.
- Reito A, Elo P, Puolakka T, Pajamaki J, Eskelinen A. Femoral diameter and stem type are independent risk factors for ARMD in the large-headed ASR THR group. BMC Musculoskelet Disord 2015; 16: 118.
- Shehadeh A, Noveau J, Malawer M, Henshaw R. Late complications and survival of endoprosthetic reconstruction after resection of bone tumors. Clin Orthop Relat Res 2010; 468 (11): 2885–95.
- Tower S S. Arthroprosthetic cobaltism associated with metal on metal hip implants. BMJ 2012; 344: e430.
