Abstract
Background and purpose — Radiostereometric analysis (RSA) is an accurate method for measurement of early migration of implants. Since a relation has been shown between early migration and future loosening of total knee and hip prostheses, RSA plays an important role in the development and evaluation of prostheses. However, there have been few RSA studies of the upper limb, and the value of RSA of the upper limb is not yet clear. We therefore performed a systematic review to investigate the accuracy and precision of RSA of the upper limb.
Patients and methods — PRISMA guidelines were followed and the protocol for this review was published online at PROSPERO under registration number CRD42016042014. A systematic search of the literature was performed in the databases Embase, Medline, Cochrane, Web of Science, Scopus, Cinahl, and Google Scholar on April 25, 2015 based on the keywords radiostereometric analysis, shoulder prosthesis, elbow prosthesis, wrist prosthesis, trapeziometacarpal joint prosthesis, humerus, ulna, radius, carpus. Articles concerning RSA for the analysis of early migration of prostheses of the upper limb were included. Quality assessment was performed using the MINORS score, Downs and Black checklist, and the ISO RSA
Results — 23 studies were included. Precision values were in the 0.06–0.88 mm and 0.05–10.7° range for the shoulder, the 0.05–0.34 mm and 0.16–0.76° range for the elbow, and the 0.16–1.83 mm and 11–124° range for the TMC joint. Accuracy data from marker- and model-based RSA were not reported in the studies included.
Interpretation — RSA is a highly precise method for measurement of early migration of orthopedic implants in the upper limb. However, the precision of rotation measurement is poor in some components. Challenges with RSA in the upper limb include the symmetrical shape of prostheses and the limited size of surrounding bone, leading to over-projection of the markers by the prosthesis. We recommend higher adherence to RSA guidelines and encourage investigators to publish long-term follow-up RSA studies.
Total joint replacement for severe osteoarthritis (OA) of the shoulder, elbow, wrist, or trapeziometacarpal joint has become an accepted treatment option. Several implant systems have been developed with 10-year survival rates ranging between 63% and 92% for shoulder arthroplasty (Singh et al. Citation2011, Gadea et al. Citation2012, Denard et al. Citation2013, Fevang et al. Citation2015, Ten Voorde et al. Citation2015, Swedish Shoulder Arthroplasty Registry Citation2015), 64% and 91% for elbow arthroplasty (Dalemans et al. Citation2013, Mansat et al. Citation2013, Plaschke et al. Citation2014,), 60% and 71% for wrist arthroplasty (Krukhaug et al. Citation2011, Ward et al. Citation2011), and 91% and 94% for replacement of the trapeziometacarpal (TMC) joint (Krukhaug et al. Citation2014, Martin-Ferrero Citation2014, Semere et al. Citation2015). These long-term survival rates are inferior to those for total knee replacement (89–95%) and total hip replacement (96–100%) (Hallan et al. Citation2007, Gøthesen et al. Citation2013). Improvement of implant survival and of implant design in the upper limb is required, including assessment of the influence of implant modifications on survival. However, the numbers of upper limb implants are relatively low, and it can take 10 or even more years before signs of loosening become visible on standard radiographs. Radiostereometric analysis (RSA) enables accurate measurement of early migration within the first postoperative year. For hip and knee prostheses, a relation between early migration measured with RSA and future aseptic loosening has been shown (Grewal et al. Citation1992, Kärrholm et al. Citation1994, Ryd et al. Citation1995, Pijls et al. Citation2012a, Citation2012b). Thus, RSA plays an important role in the development, introduction, and evaluation of new implant designs.
Only a small number of RSA studies have been performed on the upper limb. Implants of the upper extremity are different from knee and hip prostheses in their size, shape, and joint kinematics. It is therefore questionable whether the usefulness and precision of RSA of the upper extremity is comparable to that of the lower extremity. To investigate the accuracy and precision of RSA in the upper limb, we performed a systematic review of the literature.
Methods
Data Sources and search strategy
A research protocol for this review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) (Moher et al. Citation2009) was published online at the PROSPERO international prospective register of systematic reviews (http://www.crd.york.ac.uk/prospero) under registration number CRD42016042014. A systematic literature search was performed in the electronic databases Embase, Medline (OvidSP), Cochrane, Web of Science, Scopus, Cinahl (EBSCO), and Google Scholar. The following keywords were used to build the literature search: radiostereometric analysis, shoulder prosthesis, elbow prosthesis, wrist prosthesis, trapeziometacarpal joint prosthesis, humerus, ulna, radius, carpus. The search was performed on April 25, 2015. Reference lists from included articles were screened to include relevant studies that were not directly found with the search. To avoid missing any literature that was published during the drafting of this review, the search was repeated in March 2016.
Inclusion criteria and study selection
Studies were included if they described RSA of prostheses of the shoulder, elbow, wrist, and carpometacarpal joints. All types of study design, both prospective and retrospective, and data retrieved from clinical and experimental studies were included. Studies were excluded if they used RSA for purposes other than measurement of migration of prostheses (e.g. joint kinematics, fracture stability, and skeletal growth). Only articles written in English were included. Selection of suitable studies was performed independently by 2 authors (BB and AB). Disagreements were solved by discussion, and a final decision was made by a third reviewer (GK) if there was disagreement.
Quality assessment
To assess the risk of bias, all articles were scored using 14 criteria from the revised version of the MINORS score (Slim et al. Citation2003) and the Downs and Black checklist (Downs and Black 1998) (Table 1, see Supplementary data). For every criterion that was met, 1 point was given. No points were given if the criterion was not met, or if the criterion was not applicable. To assess RSA-specific quality, all studies were scored using 11 items from a standard protocol that was developed by the International Organization for Standardization and the European Standards Working Group on Joint Replacement Implants (ISO 16087:2013(E)). This protocol was developed to facilitate comparison between different centers, and recommends inclusion of all these criteria when publishing RSA results. All the criteria can be found in Table 2 (see Supplementary data). The maximum score of the RSA-specific quality assessment was 20 points. 2 authors (BB and KK) assessed the quality independently. If consensus was not reached after discussion, a third reviewer (NM) was consulted.
Data extraction
Data were extracted by 1 investigator (BB) and extraction was done using a predefined template including the following topics: (1) study information: authors and year of publication; (2) study design: type of study, population size, and follow-up; (3) the joint involved, and prostheses and components used; (4) RSA details: marker-based or model-based RSA, use of double examinations, translation data (mm) and rotation data (˚), and data on accuracy and precision.
Outcomes
Accuracy can be defined as the closeness of a true value to the most probable value originating from a series of measurements (Sköldenberg and Odquist Citation2011). Thus, accuracy data were collected from studies that determined the accuracy by comparison with another method that calculates migration and that has a resolution substantially better than that of RSA.
To investigate the precision of translation and rotation values, we included all results from double examinations in clinical RSA studies. The standard deviations (SDs) of the migration calculated using double examination was used to determine the precision, defined as 1.96 × SD. Precision was calculated separately for the shoulder, elbow, and TMC joint. If prosthesis components were analyzed separately, precision was calculated for each component. If precision was given for all 3 axes (the x-, y-, and z-axis), the lowest precision was used to calculate the mean precision.
Results
Literature search
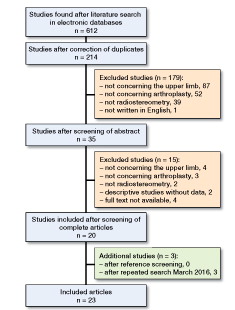
Our literature search resulted in 214 articles. After screening of titles and abstracts, 35 studies remained. Assessment of the full text resulted in 23 studies being included. Screening of references did not result in any additional inclusions. Repeating the literature search in March 2016 gave 3 additional studies (Ooms et al. Citation2015, Streit et al. Citation2015, Ten Brinke et al. Citation2016) ().
Studies included
14 studies involved the shoulder (Jónsson et al. Citation1990, Nagels et al. Citation2002, Rahme et al. Citation2004, Citation2006, Nuttall et al. Citation2007, Citation2009, Rahme et al. Citation2009, Sköldenberg and Odquist Citation2011, Stilling et al. Citation2012, Szerlip et al. Citation2012, Nuttall et al. Citation2012, Citation2014, Mechlenburg et al. Citation2014, Streit et al. Citation2015), 4 studies involved the elbow (Valstar et al. Citation2002, Rahme et al. Citation2005, Van der Lugt et al. Citation2010, DeVos et al. Citation2014), and 5 studies involved the TMC joint (Hansen et al. Citation2010, Hansen et al. Citation2011, Hansen and Stilling Citation2013, Ooms et al. Citation2015, Ten Brinke et al. Citation2016). No articles concerning the radiocarpal, distal radioulnar, metacarpophalangeal, or interphalangeal joints were found (Table 3, see Supplementary data).
Quality assessment
Assessment using the MINORS score and the Downs and Black checklist resulted in a mean quality score of 9 (3–14) points. 1 study (Rahme et al. Citation2009) had the maximum score of 14, but 8 studies did not achieve more than half of the points (Table 1, see Supplementary data).
Regarding the RSA-specific quality assessment, the mean score was 12 (1–17) points on a scale from 0 to 20. None of the studies included met all the criteria. The extent to which the different ISO criteria were met in the RSA studies varied considerably. The cutoff level for the rigid body fitting and accuracy data were given in 4 studies, while only 1 study presented the cutoff level for the condition number. Other criteria such as follow-up intervals, details of software, translation data, and the method of determining the implant position were given in almost all the studies included. All the RSA-specific quality scores can be found in Table 2 (see Supplementary data).
Accuracy
None of the studies included reported accuracy data from marker-based and model-based RSA. In 1 phantom experiment by Sköldenberg and Odquist (Citation2011), marker-free RSA was compared with standard (i.e. marker-based) RSA to determine the accuracy in a humeral head resurfacing prosthesis. Accuracy of translations of marker-free RSA varied between 0.22 and 0.47 mm. Accuracy of rotations varied between 0.92° and 1.56° compared to marker-based RSA (Table 3, see Supplementary data).
Precision
Shoulder – 8 shoulder studies reported precision values using double examinations in a clinical setting (5 glenoid components, 3 humeral components) (Nagels et al. Citation2002, Rahme et al. Citation2004, Citation2006, Nuttall et al. Citation2007, Rahme et al. Citation2009, Stilling et al. Citation2012, Mechlenburg et al. Citation2014, Streit et al. Citation2015). Sköldenberg and Odquist (Citation2011) described double examinations, although not in a clinical setting but in saw bone models. 2 additional studies by Nuttall et al. (Citation2009, Citation2012) reported precision values from a previous study by the same author (Nuttall et al. Citation2007), and they were not included in the precision analysis. The mean precision of the glenoid component was 0.18 mm for translations and 0.96˚ for rotations. For the humeral component, mean precision was 0.61 mm for translations and 5.34˚ for rotations.
Elbow – All 4 elbow studies gave precision values for the RSA technique. Van der Lugt et al. (Citation2010) reported precision data from a previous study (Valstar et al. Citation2002) and was not included, so that 3 studies remained in the precision analysis (1 humeral component, 1 ulnar component, and 1 both components). No double examinations were performed in the study by Valstar et al. (Citation2002) since permission for double examinations was not given by the institution’s ethics committee. To calculate the precision in this study, the first postoperative RSA radiograph was scanned and analyzed repeatedly. Despite the fact that no double examinations were performed, precision values from this study were included in our analysis.
The mean precision was 0.29 mm for translations of the humeral component and 0.66˚ for rotations. For the ulnar component, mean precision was 0.12 mm for translations and 0.56˚ for rotations.
TMC joint – Precision analysis of the trapezium component of the TMC joint prosthesis using clinical double examinations is described in 2 studies by Hansen et al. (Citation2010, 2013). In the first study (2010), 2 types of trapezium cups were analyzed using double examinations in both a phantom and a clinical study. Only precision data obtained from clinical experiments were included in this review. The mean precision of translations in the trapezium component was 0.93 mm. Precision of rotation measurements could only be given in the first study by Hansen et al. (Citation2010), and varied between 43° and 124°.
Clinical double examinations concerning the metacarpal stem were reported in 1 study (Hansen et al. Citation2010). Precision of translation measurements varied between 0.22 mm and 0.50 mm. Precision values for rotations varied between 11° and 25°.
Discussion
Main results
The purpose of this systematic review was to evaluate the accuracy and precision of radiostereometric analysis of prostheses of the upper limb. We found that RSA is a highly precise technique for detection of early migration of orthopedic implants of the upper limb. The precision values of translation measurements were comparable with those from RSA of total hip and knee arthroplasties (Ryd Citation1986, Vrooman et al. Citation1998, Ryd et al. Citation2000, Valstar et al. Citation2000). On the whole, the precision of rotations was lower than that of translation measurements. With regard to the shoulder, it is notable that the precision of rotations was lower in the humeral component than in the glenoid component. Studies on the humeral head resurfacing prosthesis showed especially poor precision values (Stilling et al. Citation2012, Mechlenburg et al. Citation2014). This might be due to the symmetrical shape of the implant, which constitutes a challenge when calculating rotations. Other implant designs with a highly symmetrical shape such as the trapezium Elektra screw cup and all-polyethylene cup were also found to have poor precision values (Hansen et al. Citation2010). The small size of the surrounding bone, especially in the trapezium bone, and the small number of markers that can be inserted around the prosthesis might lead to over-projection of the prosthesis over the markers and to a lack of detectable markers (Ten Brinke et al. Citation2016). On the other hand, a cadaver study by Ooms et al. (Citation2015) showed a higher precision than in clinical studies for both the trapezium and the metacarpal component of the TMC joint prosthesis. Although analysis can be performed in a more controlled environment in a cadaver study, these results indicate that migration measurement of the TMC joint prosthesis with higher precision should be possible. Thus, clinical research concerning the TMC joint should be done with a high degree of accuracy. RSA radiographs should be evaluated immediately, so that radiographs of higher quality can be taken at the same time if necessary.
The accuracy of RSA in the upper limb has barely been described. On the other hand, the accuracy of the technique with total hip and knee prostheses has been studied more extensively (Hansson et al. Citation1978, Kärrholm Citation1989, Valstar et al. Citation2005). Since the RSA technique in the lower limb and the upper limb is similar, accuracy data from hip and knee RSA studies might be extrapolated to the upper limb.
The predictive value of early migration for future loosening in upper limb arthroplasty did not fall within the scope of this review, since there are not enough data. The only scientific basis for the relation between early postoperative motion of the prosthesis and future outcomes is described in a study by Streit et al. (Citation2015). The authors noted a correlation between higher migration in the first 3 postoperative years and mean VAS pain scores. Furthermore, they found that radiolucencies were observed in approximately two-thirds of the prostheses in the high-motion group and in around one-fifth in the low-motion group. Although the role of radiolucent lines is still debated, the authors suggested the possibility of early micromotion where there are radiolucencies.
Quality of the studies included
A limitation of this review is the low number of articles included. Regarding the quality of the studies included, it can be noted that the adherence to existing guidelines (Valstar et al. Citation2005, ISO Standard (ISO 16087:2013(E)) was poor. As recommended in the ISO standard, precision should be assessed in each clinical RSA study using double examinations. Several studies did not report double examinations or referred to precision values from previous studies (Nuttall et al. Citation2009, Van der Lugt et al. Citation2010, Nuttall et al. Citation2012, Citation2014, Ten Brinke et al. Citation2016). For example, Nuttall et al. (Citation2009) presented a study on the humeral component of TSA and referred to precision values for the glenoid component (Nuttall et al. Citation2007). None of the studies that were included followed all the guidelines from the ISO standard. The most frequently ignored items were rigid body fitting error, cutoff levels for condition numbers, details of accuracy, and radiological details. These findings are in accordance with the findings of Mandanat et al. (2014), who described the low adherence to RSA guidelines in RSA studies on knee and hip arthroplasty. To improve the methodological quality and to make it easier to compare the results of studies from different centers, better adherence to the guidelines is recommended for future studies.
Future directions
Future research should focus on 3 main topics. First, to learn more about precision and accuracy of RSA, it is important to increase the number of RSA studies in shoulder, elbow, wrist, and hand arthroplasty. Secondly, long-term results are required to evaluate migration patterns in orthopedic implants and to investigate the predictive value of early migration for future loosening. The follow-up time in all but 4 studies included in this review was 2 years or less. We therefore encourage the authors of the RSA studies included to assess their patient cohorts after 5 and 10 years, to provide adequate follow-up data. Thirdly, given the predictive value of early migration in total knee and hip arthroplasty, RSA is an important tool in the development, introduction, and evaluation of orthopedic implants. This predictive value has not yet been proven in the upper limb, so the value of RSA in the upper limb is not yet clear. Future research should therefore concentrate on the predictive value of early migration for loosening of prostheses in the upper limb.
Conclusion
RSA is a highly precise method for measurement of early migration of orthopedic implants in the upper limb. However, the precision of rotation in several components has been poor. Challenges of RSA in the upper limb include the symmetrical shape of some components and the limited size of surrounding bone, leading to over-projection of the markers by the prosthesis. We recommend higher adherence to RSA guidelines and encourage investigators to present long-term follow-up RSA studies.
Supplementary data
Tables 1, 2, and 3 are available as supplementary data in the online version of this article http://dx.doi.org/10.1080/17453674.2017.1291872.
All the authors took part in drafting of the manuscript and data analysis. BB and AB performed study selection. BB and KK performed quality assessment and data extraction. All the authors read and approved the final manuscript.
We thank W. M. Bramer, medical librarian, for his support in the systematic search.
No competing interests declared.
IORT_A_1291872_SUPP.PDF
Download PDF (38.3 KB)- Dalemans A, De Smet L, Degreef I. Long-term outcome of elbow resurfacing. J Shoulder Elbow Surg 2013; 22 (11): 1455–60.
- Denard P J, Raiss P, Sowa B, Walch G. Mid- to long-term follow-up of total shoulder arthroplasty using a keeled glenoid in young adults with primary glenohumeral arthritis. J Shoulder Elbow Surg 2013; 22 (7): 894–900.
- DeVos M J, Verdonschot N, Luites J W, Anderson P G, Eygendaal D. Stable fixation of the IBP humeral component implanted without cement in total elbow replacement: a radiostereometric analysis study of 16 elbows at two-year follow-up. Bone Joint J 2014; 96-B (2): 229–36.
- Fevang B T S, Nystad T W, Skredderstuen A, Furnes O N, Havelin L I. Improved survival for anatomic total shoulder prostheses. Acta Orthop 2015; 86 (1): 63–70.
- Gadea F, Alami G, Pape G, Boileau P, Favard L. Shoulder hemiarthroplasty: outcomes and long-term survival analysis according to etiology. Orthop Traumatol Surg Res 2012; 98 (6): 659–65.
- Gøthesen O, Espehaug B, Havelin L, Petursson G, Lygre S, Ellison P, Hallan G, Furnes O. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994-2009. Bone Joint J 2013; 95-B (5): 636–42.
- Grewal R, Rimmer M G, Freeman M A. Early migration of prostheses related to long-term survivorship. Comparison of tibial components in knee replacement. J Bone Joint Surg Br 1992; 74 (2): 239–42.
- Hallan G, Lie S A, Furnes O, Engesaeter L B, Vollset S E, Havelin L I. Medium- and long-term performance of 11,516 uncemented primary femoral stems from the Norwegian arthroplasty register. J Bone Joint Surg Br 2007; 89 (12): 1574–80.
- Hansen T B, Stilling M. Equally good fixation of cemented and uncemented cups in total trapeziometacarpal joint prostheses. Acta Orthop 2013; 84 (1): 98–105.
- Hansen T B, Larsen K, Bjergelund L, Stilling M. Trapeziometacarpal joint implants can be evaluated by roentgen stereophotogrammetric analysis. J Hand Surg Eur Vol 2010; 35 (6): 480–5.
- Hansen T B, Meier M, Møller M C M, Larsen K, Stilling M. Primary cup fixation with different designs of trapeziometacarpal total joint trapezium components: a radiostereometric analysis in a pig bone model. J Hand Surg Eur Vol 2011; 36 (4): 285–90.
- Hansson L I, Olsson T H, Selvik G, Sunden G. A roentgen stereophotogrammetric investigation of innominate osteotomy (Salter). Acta Orthop Scand 1978; 49 (1): 68–72.
- Jónsson E, Lidgren L, Mjöberg B, Rydholm U, Selvik G. Humeral cup fixation in rheumatoid shoulders. Roentgen stereophotogrammetry of 12 cases. Acta Orthop Scand 1990; 61 (2): 116–7.
- Kärrholm J. Roentgen stereophotogrammetry: review of orthopedic applications. Acta Orthop 1989; 60 (4): 194–503.
- Kärrholm J, Borssén B, Löwenhielm G, Snorrason F. Does early micromotion of femoral stem prostheses matter? 4-7-year stereoradiographic follow-up of 84 cemented prostheses. J Bone Joint Surg Br 1994; 76 (6): 912–7.
- Krukhaug Y, Lie S A, Havelin L I, Furnes O, Hove L M. Results of 189 wrist replacements. A report from the Norwegian Arthroplasty Register. Acta Orthop 2011; 82 (4): 405–9.
- Krukhaug Y, Lie S A, Havelin L I, Furnes O, Hove L M, Hallan G. The results of 479 thumb carpometacarpal joint replacements reported in the Norwegian Arthroplasty Register. J Hand Surg Eur Vol 2014; 39 (8): 819–25.
- Mansat P, Bonnevialle N, Rongières M, Mansat M, Bonnevialle P. Experience with the Coonrad-Morrey total elbow arthroplasty: 78 consecutive total elbow arthroplasties reviewed with an average 5 years of follow-up. J Shoulder Elbow Surg 2013; 22 (11): 1461–8.
- Martin-Ferrero M. Ten-year long-term results of total joint arthroplasties with ARPE® implant in the treatment of trapeziometacarpal osteoarthritis. J Hand Surg Eur Vol 2014; 39 (8): 826–32.
- Mechlenburg I, Klebe T M, Døssing K V, Amstrup A, Søballe K, Stilling M. Evaluation of periprosthetic bone mineral density and postoperative migration of humeral head resurfacing implants: two-year results of a randomized controlled clinical trial. J Shoulder Elbow Surg 2014; 23 (10): 1427–36.
- Moher D, Liberati A, Tetzlaff J, Altman D G, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62 (10): 1006–12.
- Nagels J, Valstar E R, Stokdijk M, Rozing P M. Patterns of loosening of the glenoid component. J Bone Joint Surg Br 2002; 84 (1): 83–7.
- Nuttall D, Haines J F, Trail I I. A study of the micromovement of pegged and keeled glenoid components compared using radiostereometric analysis. J Shoulder Elb Surg 2007; 16(3suppl): S65–S70.
- Nuttall D, Haines J F, Trail I A. The effect of the offset humeral head on the micromovement of pegged glenoid components: A comparative study using radiostereometric analysis. J Bone Joint Surg Br 2009; 91 (6): 757–61
- Nuttall D, Haines J F, Trail I A. The early migration of a partially cemented fluted pegged glenoid component using radiostereometric analysis. J Shoulder Elbow Surg 2012; 21 (9): 1191–6.
- Nuttall D, Birch A, Haines J F, Trail I A. Radiostereographic analysis of a shoulder surface replacement: Does hydroxyapatite have a place? Bone Joint J 2014; 96B (8): 1077–81.
- Ooms E M, ten Brinke B, Mathijssen N M C, Blom I F, Deijkers R L M, Kraan G A. Feasibility of model-based Roentgen Stereophotogrammetric Analysis to evaluate early migration of the trapeziometacarpal joint prosthesis. BMC Musculoskelet Disord 2015; 16 (1): 295.
- Pijls B G, Nieuwenhuijse M J, Fiocco M, Plevier J W, Middeldorp S, Nelissen R G, Valstar E R. Early proximal migration of cups is associated with late revision in THA: a systematic review and meta-analysis of 26 RSA studies and 49 survivalstudies. Acta Orthop 2012a; 83 (6): 583–91.
- Pijls B G, Valstar E R, Nouta K-A, Plevier J W, Fiocco M, Middeldorp S, Nelissen R G. Early migration of tibial components is associated with late revision: a systematic review and meta-analysis of 21,000 knee arthroplasties. Acta Orthop 2012b; 83 (6): 614–24.
- Plaschke H C, Thillemann T M, Brorson S, Olsen B S. Implant survival after total elbow arthroplasty: a retrospective study of 324 procedures performed from 1980 to 2008. J Shoulder Elbow Surg 2014; 23 (6): 829–36.
- Rahme H, Mattsson P, Larsson S. Stability of cemented all-polyethylene keeled glenoid components. A radiostereometric study with a two-year follow-up. J Bone Joint Surg Br 2004; 86 (6): 856–60.
- Rahme H, Mattsson P, Larsson S. Stable fixation of the ulnar component in the Kudo elbow prosthesis. A radiostereometric (RSA) study of 13 prostheses with 2-year follow-up. Acta Orthop 2005; 76 (1): 104–8
- Rahme H, Mattsson P, Wikblad L, Larsson S. Cement and press-fit humeral stem fixation provides similar results in rheumatoid patients. Clin Orthop Relat Res 2006; 448: 28–32
- Rahme H, Mattsson P, Wikblad L, Nowak J, Larsson S. Stability of cemented in-line pegged glenoid compared with keeled glenoid components in total shoulder arthroplasty. J Bone Joint Surg Am 2009; 91 (8): 1965–72.
- Ryd L. Micromotion in knee arthroplasty. A roentgen stereophotogrammetric analysis of tibial component fixation. Acta Orthop Scand 1986; (Suppl 220): 1–80.
- Ryd L, Albrektsson B E, Carlsson L, Dansgård F, Herberts P, Lindstrand A, Regnér L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg Br 1995; 77 (3): 377–83.
- Ryd L, Yuan X, Löfgren H. Methods for determining the accuracy of radiostereometric analysis (RSA). Acta Orthop Scand 2000; 71 (4): 403–8.
- Semere A, Vuillerme N, Corcella D, Forli A, Moutet F. Results with the Roseland(®) HAC trapeziometacarpal prosthesis after more than 10 years. Chir Main 2015; 34 (2): 59–66
- Singh J A, Sperling J W, Cofield R H. Revision surgery following total shoulder arthroplasty: analysis of 2588 shoulders over three decades (1976 to 2008). J Bone Joint Surg Br 2011; 93 (11): 1513–7.
- Sköldenberg O, Odquist M. Measurement of migration of a humeral head resurfacing prosthesis using radiostereometry without implant marking: an experimental study. Acta Orthop 2011; 82 (2): 193–7.
- Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (Minors): development and validation of a new instrument. ANZ J Surg 2003; 73 (9): 712–6.
- Stilling M, Mechlenburg I, Amstrup A, Soballe K, Klebe T. Precision of novel radiological methods in relation to resurfacing humeral head implants: Assessment by radiostereometric analysis, DXA, and geometrical analysis. Arch Orthop Trauma Surg 2012; 132 (11): 1521–30.
- Streit J J, Shishani Y, Green M E, Nebergall A K, Wanner J P, Bragdon C R, Malchau H, Gobezie R. Analysis of glenoid component motion after total shoulder arthroplasty. Orthopedics 2015; 38 (10): 891–7.
- Swedish Shoulder Arthroplasty Registry. Annual report 2015. http://www.ssas.se/axel/reports.php
- Szerlip B, Muh S, Streit J J, Gobezie R. Humeral fixation in shoulder arthroplasty: does stem geometry matter? Semin Arthroplast 2012; 23 (2): 103–5.
- Ten Brinke B, Mathijssen N M C, Blom I, Deijkers R L M, Ooms E M, Kraan G A. Model-based roentgen stereophotogrammetric analysis of the surface replacement trapeziometacarpal total joint arthroplasty. J Hand Surg Eur Vol 2016; 41(9): 925–9.
- Ten Voorde P C, Rasmussen J V, Olsen BS, Brorson S. Resurfacing shoulder arthroplasty for the treatment of severe rheumatoid arthritis. Acta Orthop 2015; 86 (3): 293–7.
- Valstar E R, Vrooman H A, Toksvig-Larsen S, Ryd L, Nelissen R G. Digital automated RSA compared to manually operated RSA. J Biomech 2000; 33 (12): 1593–9.
- Valstar E R, Garling E H, Rozing P M. Micromotion of the Souter-Strathclyde total elbow prosthesis in patients with rheumatoid arthritis: 21 Elbows followed for 2 years. Acta Orthop Scand 2002; 73 (3): 264–72.
- Valstar E R, Gill R, Ryd L, Flivik G, Börlin N, Kärrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76 (4): 563–72.
- Van der Lugt J C T, Valstar E R, Witvoet-Braam S W, Nelissen R G H H. Migration of the humeral component of the Souter-Strathclyde elbow prosthesis: a long-term RSA study. J Bone Joint Surg Br 2010; 92 (2): 235–41.
- Vrooman H A, Valstar E R, Brand G J, Admiraal D R, Rozing P M, Reiber J H C. Fast and accurate automated measurements in digitized stereophotogrammetric radiographs. J Biomech 1998; 31 (5): 491–8.
- Ward C M, Kuhl T, Adams B D. Five to ten-year outcomes of the Universal total wrist arthroplasty in patients with rheumatoid arthritis. J Bone Joint Surg Am 2011; 93 (10): 914–9.