Abstract
Background and purpose — Maximal total point motion (MTPM) measured by radiostereometry (RSA) is widely used as a predictor of total knee arthroplasty (TKA) loosening. We compared the ability of different RSA measurements at different time points to predict loosening of tibial TKA components in the long term.
Patients and methods — 116 TKAs in 116 patients were included in our analysis. 16 (14.8–17.4) years after surgery, 5 tibial components had been revised due to aseptic loosening. Receiver operating characteristic curves were calculated in order to investigate the specificity and sensitivity of different RSA parameters at different thresholds.
Results — Rotation around the transverse (x-) axis measured 2 years postoperatively had the best predictive value of all parameters, with an area under the curve (AUC) of 80%. Using a threshold of 0.8 degrees, a specificity of 85% and a sensitivity of 50% were reached. The AUC for tibial component distal translation was 79% and it was 77% for proximal translation, whereas it was only 68% for MTPM.
Interpretation — Rotation of the cemented tibial component around the transverse axis, proximal translation, and distal translation are slightly better at predicting aseptic loosening than MTPM, and tibial component migration measured after 2 years gives a good prediction of aseptic loosening up to 15 years.
The amount of early migration as measured by radiometric analysis (RSA) can serve as an indicator of the risk of revision of both hip and knee prostheses. The accuracy of RSA is estimated to be around 0.2 mm for translation along the 3 axes in space and 0.5 degrees for rotation around the 3 axes (Grewal et al. Citation1992, Ryd et al. Citation1995, Nelissen et al. Citation1998). It has therefore been proposed that RSA can identify unstable implants as early as 1 year postoperatively (Pijls et al. Citation2012a, Citationb).
The notion that maximal total point motion (MTPM) of tibial components used in total knee arthroplasty (TKA) correlates with the risk of revision for aseptic loosening was initially based on very few studies (Grewal et al. Citation1992, Ryd et al. Citation1995), but new evidence to support this previous work has recently emerged. A meta-analysis of RSA-based studies on early implant migration indicated a correlation of MTPM with 10-year revision rates of TKA (Pijls et al. Citation2012b). Long-term follow-up of total hip arthroplasty cohorts previously investigated by RSA confirmed RSA-based predictions of subsequent acetabular or femoral component loosening (Hauptfleisch et al. Citation2006, Nieuwenhuijse Citation2012, Pijls et al. Citation2012a), but—at least to our knowledge—no such long-term investigations have been performed on a cohort of TKA patients.
MTPM is not the only way of describing tibial component micromotion. RSA allows the measurement of migration along and rotation around all 3 axes in space, and MTPM is an aggregate parameter describing the amount of translation of the implant. MTPM does not specify the direction of this vector in space. Negative translation of tibial components along the y-axis is commonly expressed as distal translation (or “subsidence”), and positive translation along this axis is termed proximal translation (or “lift-off”). Distal and proximal translation have also been used in predicting later loosening, and a threshold of >0.2 mm translation of the center of the tibial component along the y-axis is considered to be a good predictor of subsequent implant loosening (Nelissen et al. Citation1998).
Thus, RSA is a precise instrument for prediction of long-term stability of TKA implants, but several questions remain unclear: (1) Does MTPM indeed have the optimal predictive value when compared with other measurements of tibial component migration? (2) What are the thresholds of acceptable migration when predicting long-term failure? (3) Can reliable prediction be obtained as early as 1 year postoperatively?
Our primary hypothesis was that MTPM is not the best predictor of later aseptic loosening of the tibial component. The secondary hypothesis was that 2 years should have elapsed after surgery in order to obtain the best prediction. In this study, we analyzed RSA data from 3 separate randomized controlled trials with a median of 16 years of follow-up. We investigated the sensitivity and specificity of RSA measurements obtained at various time points and their ability to predict long-term outcome by analyzing receiver operating characteristic (ROC) curves.
Patients and methods
Study population
The current study population was based on 3 randomized controlled trials on cemented TKA conducted at the Department of Orthopedics, Uppsala University Hospital between November 1994 and June 1999, as described previously (Adalberth et al. Citation2000, Citation2001, Citation2002). 2 studies consisted of patients randomized to either metal-backed or all-polyethylene tibial components, using the Freeman-Samuelsson prosthesis (Sulzer Orthopedics AG, Zug, Switzerland) in 1 study and the Anatomical Graduated Component prosthesis (Biomet, Warsaw, IN) in the other. The third study consisted of patients who all received a metal-backed Anatomic Modular Knee prosthesis (DePuy, Warsaw, IN) and who were randomized to 2 different bone cements (CMW-1 or Palacos R with gentamicin). These 3 studies covered a total of 124 patients with 131 TKAs. There were 84 women and 40 men, and 7 patients were operated bilaterally. 8 TKAs were excluded from the RSA analysis described in the original studies due to inappropriate marking of the prosthesis and/or the tibial bone, resulting in insufficient conditional numbers or mean errors. Furthermore, in the present study on the pooled cohorts, in bilaterally operated patients only the knee that was operated on first was included in our analysis in order to avoid dependency issues ().
Figure 1. Flow chart describing the 3 initial study populations and the pooled study cohort. AGC – Anatomic Graduated Components knee (Biomet). See also abbreviations in .
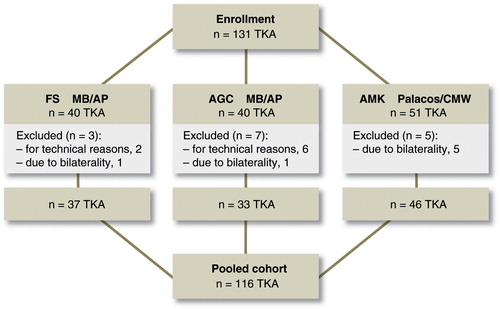
AMK – Anatomic Modular Knee (DePuy) fixed with CMW1 cementThe exclusion process described above resulted in a pooled cohort of 116 patients with 116 TKAs that were analyzed by RSA after a mean follow-up of 16.0 (14.8–17.4) years. Using the Swedish Knee Arthroplasty Register (SKAR) and our local database, we were able to identify all the patients who underwent TKA revisions, and we identified all deceased patients with their dates of death. During the follow-up period, 8 TKAs had been revised, 5 due to aseptic loosening, 1 for instability, 1 for infection, and 1 with resurfacing of the patella. 50 patients had died during the follow-up period. The revisions for aseptic loosening were all due to late loosening, occurring approximately 10 years after the index operation (mean 10.4 years). Of those 5 patients who were revised for aseptic loosening of the tibial component, 4 were men, and 4 of 5 revisions were related to 1 specific prosthesis type (Freeman-Samuelsson). 2 of the patients were overweight (). The 5 patients who underwent revision of the tibial component for aseptic loosening were defined as having reached the relevant endpoint of our analysis.
Table 1. Demographics of the 5 patients who were revised due to aseptic loosening
Radiostereometric analysis
The methodology of the RSA examinations used in our cohort has been described in detail previously (Adalberth et al. Citation2000, Citation2001, Citation2002). Briefly, 7 to 9 tantalum spheres (RSA Biomedical Innovations, Umeå, Sweden) with a diameter of 0.5 or 0.8 mm were inserted into the proximal tibial metaphysis. Furthermore, 6 similar spheres were inserted into the polyethylene of the tibial component. The initial radiostereometric examination (reference examination) was performed 7–10 days after the operation, a time point when weight bearing had been initiated. Further examinations were performed after 4, 12, and 24 months.
The radiostereometric investigations were performed using UmRSA software (RSA Biomedical Innovations). The patients were examined supine with the knee of interest positioned inside a calibration cage. At the initial reference examination, the knee was positioned with the anatomical axes of the knee parallel to the axes of the laboratory coordinate axes. The RSA technique of the current setup has been presented previously (Selvik 1989, Nilsson and Kärrholm Citation1993, Nilsson et al. Citation1995).
Since the tantalum markers in the tibial components were not inserted in exactly the same places in all patients, standardized positions for measurements of prosthetic translations were reconstructed on the tibial component (Nilsson and Kärrholm Citation1993). These positions were located at the edges (medially, laterally, anteriorly, posteromedially, and posterolaterally) and at the center of the tibial component.
The micromotions of the tibial component in relation to the tibia were recorded using the tantalum markers in the proximal tibia as the fixed reference segment. The rotations were expressed as rotations around the transverse axis (x-axis, anterior-posterior rotation), the longitudinal axis (y-axis, internal-external rotation), and the sagittal axis (z-axis, varus-valgus rotation) of the knee. In each implant, the greatest negative value for y-translation at the standardized points was referred to as distal translation (sometimes referred to as “subsidence”), and the greatest positive y-translation was referred to as proximal translation (sometimes referred to as “lift-off”). If all points of measurement showed negative y-translation, proximal translation was 0 mm, and if all points showed positive y-translation, distal translation was 0 mm. MTPM described the vectorial length of the 3-dimensional translation of the standardized point at the tibial component that moved the most (Ryd Citation1986, Valstar et al. Citation2005). Absolute values were used to describe the magnitude of migration or rotation.
Double RSA examinations were performed in all patients at all follow-up times. The precision of RSA was calculated as the 99% prediction interval (± 2.58 × SD) around the mean of all double examinations, assuming a normal distribution. Thus, the cut-off levels for significant rotations were > ± 0.15 degrees for the transverse (x-) axis, > ± 0.2 degrees for the longitudinal (y-) axis, and > ± 0.1 degrees for the sagittal (z-) axis. The corresponding value for translations along the longitudinal (y-) axis was > ± 0.1 mm.
Statistics
Frequencies, means, medians, and ranges were used to describe data distribution, whereas estimation uncertainty was assessed using 95% confidence intervals (CIs). Distributions of numerical variables were assessed by visual inspection of histograms and by using the Shapiro-Wilk test. In accordance with previously published findings (Aspenberg et al. Citation2008), RSA data were heavily skewed, so medians and interquartile ranges (IQRs) were calculated. Differences in RSA measurements between groups were therefore described using a nonparametric confidence interval and by calculating an estimator for the difference of the location parameters (sometimes described as the “median difference”). There is a statistically significant difference between groups when the confidence interval does not include 0. Wilcoxon’s rank sum test was used to calculate p-values.
ROC curves were calculated and plotted in order to investigate the specificity and sensitivity at various thresholds for rotation around the x-axis, rotation around the y-axis, rotation around the z-axis, proximal translation, distal translation, and MTPM at 2 years postoperatively. This allowed calculation of the area under the curve (AUC), which can be considered to be a measure of how well a certain numerical measurement will predict outcome, and different measures can be compared with each other.
Ethics
The 3 randomized studies mentioned above had the approval of the Uppsala Ethics Committee (approval number 104/93), but since these studies were initiated during the 1990s, they were not registered at clinicaltrials.gov. The long-term follow-up of the pooled cohort described in this manuscript was approved by the same committee (approval number 2012/013). Since the endpoints of our present study were not related to the endpoints of the original randomized studies, our present report does not follow the CONSORT protocol.
Results
4 months postoperatively, there were no differences in the amount of micromotion of the tibial component between the group revised for aseptic loosening and the non-revised group. 1 year postoperatively, the tibial components that were revised due to aseptic loosening had slightly higher proximal translation of the periphery of the tibial component (median 0.37 mm, 95% CI: –0.14 to 1.5) than the non-revised group (median 0.20 mm, CI: 0.22–0.34; p = 0.05). Distal translation of the periphery of the tibial component, MTPM, and rotations around the x-, y-, and z-axes did not differ statistically significantly between the 2 groups after 4 months ( and ).
Table 2. Tibial component migration and rotation measured by RSA, up to 2 years. For definitions of migration along and rotation around the 3 axes, see Patients and methods
Table 3. Median differences in tibial component migration and rotation between revised and unrevised tibial components.
After 2 years, the difference in proximal translation of the periphery of tibial components between the revised group (median 1.01 mm, CI: 0.17–1.51) and the non-revised group (median 0.28 mm, CI: 0.31–0.46) was statistically significant (p = 0.04). Distal translation of the periphery of the tibial component and rotation around the transverse (x-) axis were also statistically significantly higher in the revised components (median distal translation −0.64 mm, CI: −1.23 to −0.19; and median rotation 0.69 degrees, CI: −0.05 to 1.85) than in the non-revised components (median distal translation −0.26 mm, CI: −0.43 to −0.29; and median rotation 0.32 degrees, CI: 0.35 − 0.57). As at earlier examinations, the MTPM did not differ statistically significantly between revised and non-revised components after 2 years ().
Tibial component rotation around the transverse (x-) axis measured 2 years postoperatively was the best predictor of loosening, with an AUC of 80% (). Using a threshold of 0.8 degrees, a specificity of 85% (CI: 76–92) and a sensitivity of 50% (CI: 0–100) were reached () Distal translation of the periphery of the tibial component measured 2 years postoperatively had an AUC of 79% with a specificity of 77% (CI: 68–86) and a sensitivity of 60% (CI: 20–100) at a threshold of 0.6 mm migration. Proximal translation of the periphery of the tibial component measured 2 years postoperatively had an AUC of 77%, with a specificity of 90% (CI: 84–96) and a sensitivity of 60% (CI: 20–100) at a threshold of 0.9 mm migration. In contrast, the AUC of MTPM measured after 2 years was 68% ().
Figure 2. ROC curve for tibial component rotation around the transverse (x-) axis as measured by RSA after 2 years, showing thresholds at 0.2° and 0.8°. The blue error bars indicate the 95% confidence intervals around the specificity and sensitivity for the indicated thresholds of 0.2° and 0.8°.
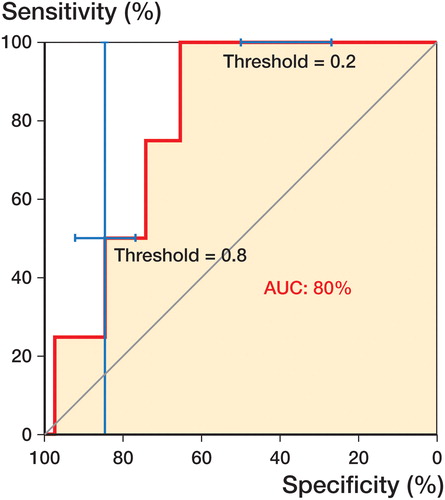
Figure 3. ROC curve for maximal total point motion (MTPM) of the tibial component as measured by RSA after 2 years, showing threshold at 1.0 mm. The blue error bar indicates the 95% confidence intervals around the specificity and sensitivity for the indicated threshold of 1 mm.
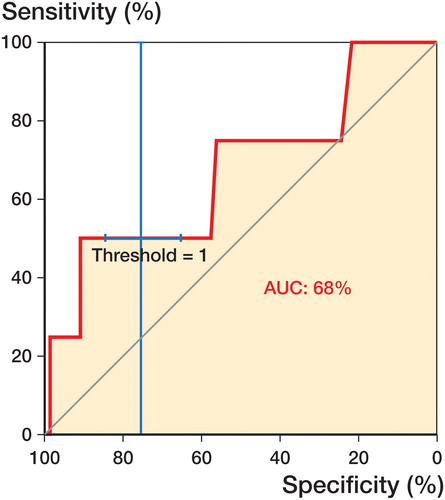
Table 4. Sensitivity and specificity, with different thresholds of migration or rotation, for prediction of aseptic tibial component loosening. All measurements were performed 2 years after the index procedure
Discussion
Most studies reporting RSA measurements on TKA implants have focused on MTPM as the main predictor of subsequent loosening. MTPM is an aggregate parameter describing the amount of translation and rotation of an implant. In addition, it is dependent on the stability and visibility of all markers during the follow-up. Furthermore, movement of the polyethylene liner in relation to the metal base plate in modular TKA has been described (Rao et al. Citation2002), and these movements mostly occur as rotations in the horizontal plane (i.e. internal-external rotation), equivalent to antero-posterior (AP) and medial-lateral (ML) translations (Nilsson et al. Citation2003). In cases where markers have been inserted into the liner, it is impossible to differentiate the amount of such recorded movements occurring between the liner and the baseplate from movements occurring between the baseplate and underlying bone. Thus, in our opinion parameters other than MTPM might possibly be more suitable as predictors of long-term loosening.
In the present study, rotation of the tibial component around the transverse axis (the x-axis) and the associated parameters distal translation and proximal translation of the periphery of the tibial component, measured 2 years postoperatively, were better predictors of subsequent revision due to aseptic loosening than MTPM. Furthermore, measurements performed at earlier time points were not as well suited to predict outcome as measurements performed at 2 years. Although the parameter proximal translation of the tibial component measured 1 year postoperatively differed between revised and non-revised components, this finding was only of borderline statistical significance.
Many studies have indicated that there is a correlation between early RSA measurements and subsequent failure of TKA components, and it has been claimed that continuous motion exceeding 1–2 mm during the first 2 years after the index operation indicates a poor prognosis (Ryd et al. Citation1995). However, a systematic comparison of the predictive ability of different RSA parameters obtained at different time points has never been performed.
Previous RSA studies on cemented tibial components have suggested an initial, minor migration (maximum distal translation: < 0.15 mm; x- or z-rotation: < 0.2 degrees) followed by subsequent minimal migration (Nilsson et al. Citation1999, Carlsson et al. Citation2005, Nilsson et al. Citation2006). However, this pattern of migration is quite different in uncemented tibial components, such as those based on trabecular metal. In such tibial components, a greater amount of migration over a prolonged period of several months (mostly the initial 3 months postoperatively) is finally followed by either stabilization or loosening of the prosthesis (Henricson et al. Citation2008). These differences between different modes of fixation must be kept in mind when comparing cemented and uncemented tibial components (Henricson et al. Citation2013), and our findings may therefore not be extrapolated to tibial components used in uncemented TKA.
The ability of different RSA parameters to predict outcome has been debated (Ryd et al. Citation1995, Pijls et al. Citation2012a, Citationb). Distal and proximal translation have been used in predicting later loosening, and a threshold of 0.2 mm was chosen as the cut-off point defining instability (Nelissen et al. Citation1998). In that paper, distal and proximal translation were measured at the center of the tibial component—as opposed to the periphery of the implant, where translations were measured in our study. Since it is likely that the points at the periphery of the implant move more than the center, our chosen cut-off value of 0.6 mm was higher and gave a specificity of 77%. A recent meta-analysis on this subject indicated an 8% increase in 10-year revision rates for every 1-mm increase in MTPM, but that study concentrated on MTPM measured 1 year postoperatively, mainly because other parameters are not consistently reported in the literature (Pijls et al. Citation2012b).
The present study had several limitations. The good long-term clinical results with few revisions reduced the precision of our statistical analyses, as reflected by wide confidence intervals. Thus, we advise caution when generalizing our results to a general population. In the analysis of RSA data, it is important to study migration patterns over time. In our study, we focused on absolute migration up to 2 years, and this limits the conclusions that can be drawn on migration patterns at later time points. In addition, different bone densities can influence the amount of early migration, a parameter that we cannot control for. Moreover, our study is based on historical RSA examinations performed with analog methods and analyzed with historical software. It is possible that re-analysis of our material with modern equipment would have resulted in improved precision and more exact measurements.
In summary, this study indicates that RSA measurements other than the widely used MTPM may be better predictors of the risk of long-term loosening, and our data confirm that there is a strong association between tibial component micromotion measured after 2 years (rotation around the transverse axis, proximal translation, and distal translation) and the risk of revision due to aseptic loosening up to 15 years. Future studies on the migration of tibial components used in TKA should therefore direct more attention to tibial component rotation around the transverse axis, and the associated parameters proximal and distal translation of the periphery of the tibial component.
AG and NPH initiated and designed the present study. AG collected data. Statistical analysis and interpretation was done by AG and NH. AG and NPH drafted the manuscript and KGN and GA revised it. GA conducted the original studies on which the present study was based.
No competing interests declared.
- Adalberth G, Nilsson K G, Byström S, Kolstad K, Milbrink J. Low-conforming all-polyethylene tibial component not inferior to metal-backed component in cemented total knee arthroplasty: prospective, randomized radiostereometric analysis study of the AGC total knee prosthesis. J Arthroplasty 2000; 15(6): 783–92.
- Adalberth G, Nilsson KG, Byström S, Kolstad K, Milbrink J. All-polyethylene versus metal-backed and stemmed tibial components in cemented total knee arthroplasty. A prospective, randomised RSA study. J Bone Joint Surg Br 2001; 83(6): 825–31.
- Adalberth G, Nilsson K G, Kärrholm J, Hassander H. Fixation of the tibial component using CMW-1 or Palacos bone cement with gentamicin: similar outcome in a randomized radiostereometric study of 51 total knee arthroplasties. Acta Orthop Scand 2002; 73(5): 531–8.
- Aspenberg P, Wagner P, Nilsson K G, Ranstam J. Fixed or loose? Dichotomy in RSA data for cemented cups. Acta Orthop 2008; 79(4): 467–73.
- Carlsson A, Björkman A, Besjakov J, Önsten I. Cemented tibial component fixation performs better than cementless fixation. Acta Orthop 2005; 76(3): 362–9.
- Grewal R, Rimmer M G, Freeman F A R. Early migration of prostheses related to long-term survivorship. Comparison of tibial components in knee replacement. J Bone Joint Surg (Br) 1992; 74: 239–42.
- Hauptfleisch J, Glyn-Jones S, Beard D J, Gill H S, Murray D W. The premature failure of the Charnley Elite-Plus stem. J Bone Joint Sur (Br) 2006; 88-B: 179–83.
- Henricson A, Linder L, Nilsson KG. A trabecular metal tibial component in total knee replacement in patients younger than 60 years. A two-year radiostereophotogrammetric analysis. J Bone Joint Surg (Br) 2008; 90: 1585–93.
- Henricson A, Rösmark D, Nilsson K G. Trabecular metal tibia still stable at 5 years. Acta Orthop 2013; 84 (4): 398–405.
- Nelissen R G, Valstar E R, Rozing P M. The effect of hydroxyapatite on the micromotion of total knee prostheses. A prospective, randomized, double-blind study. J Bone Joint Surg (Am) 1998; 80 (11): 1665–72.
- Nieuwenhuijse M J. Good diagnostic performance of early migration as a predictor of late aseptic loosening of acetabular cups. J Bone Joint Surg (Am) 2012; 94: 874–80.
- Nilsson K G, Kärrholm J. Increased varus-valgus tilting of screw-fixated knee prostheses. Stereoradiographic study of uncemented versus cemented tibial components. J Arthroplasty 1993; 8:529–40.
- Nilsson K G, Kärrholm J, Carlsson L, Dalén T. Hydroxyapatite coating versus cemented fixation of tibial component in total knee arthroplasty. Prospective randomized comparisation of hydroxyapatite-coated and cemented tibial components with 5-Year follow-up using radiostereometri (RSA). J Arthroplasty 1999; 14(1): 9–20.
- Nilsson K G, Kärrholm J, Linder L. Femoral component migration in total knee arthroplasty: randomized study comparing cemented and uncemented fixation of the Miller-Galante 1 design. J Orthop Res 1995; 13: 347–56.
- Nilsson K G, Henricson A, Dalen T. In vivo determination of modular tibial insert micromotion. Trans Orthop Res Soc. 2003; 28: 1402.
- Nilsson K G, Henricson A, Norgren B, Dalén T. Uncemented HA-coated implant is the optimum fixation for TKA in the young patient. Clin Orthop Relat Res 2006; 448: 129–39.
- Pijls B G, Nieuwenhuijse M J, Fiocco M, Plevier J W M, Middeldorp S, Nelissen R G, Valstar E R. Early proximal migration of cups is associated with late revision in THA. Acta Orthop 2012a; 83(2): 135–41.
- Pijls B G, Valstar E R, Nouta K A, Plevier J W M, Fiocco M, Middeldorp S, Nelissen R G. Early migration of tibial components is associated with late revision. Acta Orthop 2012b; 83(6): 614–24.
- R Development Core Team. A language and environment for statistical computing. 2012. http://www.R-project.org/
- Rao A R, Engh G A, Collier M B, Lounici S. Tibial interface wear in retrieved total knee components and correlations with modular insert motion. J Bone Joint Surg Am 2002; 84-A(10): 1849–55.
- Ryd L. Micromotion in knee arthroplasty: a roentgen stereophotogrammetric analysis of tibial component fixation. Acta Orthop Scand 1986; Suppl 220: 1–60
- Ryd L, Albrektsson B, Carlsson L, Dansgard F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Surg (Br) 1995; 77-B(3): 377–83.
- Valstar E R, Gill R, Ryd L, Flivik G, Börlin N, Kärrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop 2005; 76(4): 563–72.
