Abstract
Background and purpose — Large metal-on-metal (MoM) articulations are associated with metal wear and corrosion, leading to increased metal ion concentrations and unacceptable revision rates. There are few comparative studies of 28-mm MoM articulations with conventional metal-on-polyethylene (MoP) couplings. We present a long-term follow-up of a randomized controlled trial comparing MoM versus MoP 28-mm articulations, focused on metal ions and implant survival.
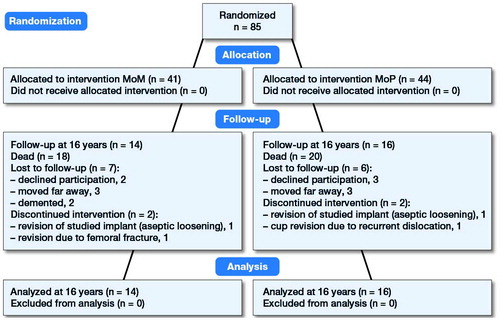
Patients and methods — 85 patients with a mean age of 65 years at surgery were randomized to a MoM (Metasul) or a MoP (Protasul) bearing. After 16 years, 38 patients had died and 4 had undergone revision surgery. 13 patients were unavailable for clinical follow-up, leaving 30 patients (n = 14 MoM and n = 16 MoP) for analysis of metal ion concentrations and clinical outcome.
Results — 15-year implant survival was similar in both groups (MoM 96% [95% CI 88–100] versus MoP 97% [95% CI 91–100]). The mean serum cobalt concentration was 4-fold higher in the MoM (1.5 μg/L) compared with the MoP cohort (0.4 μg/L, p < 0.001) and the mean chromium concentration was double in the MoM (2.2 μg/L) compared with the MoP cohort (1.0 μg/L, p = 0.05). Mean creatinine levels were similar in both groups (MoM 93 μmol/L versus MoP 92 μmol/L). Harris hip scores differed only marginally between the MoM and MoP cohorts.
Interpretation — This is the longest follow-up of a randomized trial on 28-mm MoM articulations, and although implant survival in the 2 groups was similar, metal ion concentrations remained elevated in the MoM cohort even in the long term.
The main failure mechanism of total hip arthroplasty (THA) with metal-on-polyethylene (MoP) articulations is aseptic implant loosening. It was hypothesized that the reduction in wear particles of alternative bearings such as metal-on-metal (MoM) implants would lead to less osteolysis and improved long-term implant survival. The MoM concept was quickly accepted and widely used, either in the form of hip resurfacing but also with traditional small-caliber heads such as the 28-mm diameter Metasul articulation (Weber Citation1996). Our group has previously shown that, in a joint simulator, the Metasul MoM bearing produced 100-fold fewer volumetric wear particles compared with a traditional MoP coupling (Anissian et al. Citation1999).
There are numerous clinical studies with satisfactory results of the Metasul MoM bearing after short- to mid-term (Dorr et al. Citation2000, Citation2004, Kim et al. Citation2004, Long et al. Citation2004, Sharma et al. Citation2007, Saito et al. Citation2010, Bernstein et al. Citation2012, Vendittoli et al. Citation2013, Bisseling et al. Citation2015) and long-term follow-up (Grubl et al. Citation2007, Eswaramoorthy et al. Citation2008, Marker et al. Citation2008, Dastane et al. Citation2011, Migaud et al. Citation2011, Randelli et al. Citation2012, Hwang et al. Citation2013, Innmann et al. Citation2014, Lass et al. Citation2014, Malek et al. Citation2015a). Still, there are several publications reporting less favorable outcomes (Levai et al. Citation2006, Nich et al. Citation2006, Lazennec et al. Citation2009, Tardy et al. Citation2015). Despite the great enthusiasm following the introduction of these alternative bearings, the number of comparative studies between alternative and conventional bearings is limited (Migaud et al. Citation2011). Most of the earlier studies are uncontrolled cases series. We have been able to find only 3 previous randomized controlled trials in which the Metasul MoM articulation is compared with conventional type and/or small-diameter head bearings (Zijlstra et al. Citation2010, Bjorgul et al. Citation2013, Desmarchelier et al. Citation2013).
Concerns were raised about the short- and long-term safety and function of MoM systems, and reports of adverse reactions in tissues surrounding the implants are numerous (Haddad et al. Citation2011). This, combined with a high early failure rate of several systems (Smith et al. Citation2012) caused the use of MoM implants to diminish considerably (Swedish Hip Arthroplasty Register, Annual Report Citation2015).
The aim of the present randomized controlled trial was to evaluate and compare cemented MoM with MoP THAs with 28-mm diameter heads in the long-term. 2- and 6-year data have been published previously (Dahlstrand et al. Citation2009, Hailer et al. Citation2011). The primary outcome measure of this follow-up study was serum metal ion concentrations of cobalt (Co) and chromium (Cr). Secondary outcome measures were implant survival, clinical parameters and radiographic results.
Patients and methods
Study design
From 1998 to 2001, 166 patients referred to the Department of Orthopaedics, Karolinska Hospital in Stockholm, Sweden for cemented total THA were assessed for inclusion. Inclusion criteria were age between 45 and 70 years and hip pain with radiographically confirmed osteoarthritis. Exclusion criteria were other diagnoses besides primary osteoarthritis, previous joint replacement surgery and osteosynthesis, weight exceeding 105 kg, drug abuse, mental disorders including cognitive impairment, osteoporosis, treatment with systemic corticosteroids for more than 3 months in the last year before surgery and refusal to participate in the study.
85 patients were randomized into 2 groups with a computer application using the minimization method to ensure equal size of cohorts: (1) MoM or (2) MoP articulation. The patients were blinded to the type of bearing that was used. The authors involved were not blinded. 2- and 6-year data for this cohort have been published previously (Dahlstrand et al. Citation2009, Hailer et al. Citation2011).
Implants and surgical technique
All patients were operated with a cemented, tapered, stainless steel MS30 stem with a matte surface (Sulzer, Winterthur, Switzerland) combined with a modular Co-Cr 28-mm diameter head. 2 types of articulations were used: a (1) Co-Cr liner fitted in a polyethylene cup, making it a MoM bearing (Metasul, Sulzer) and a (2) all-polyethylene cup, making it a MoP bearing (Protasul, Sulzer). The cups were made from ultra-high molecular weight polyethylene (UHMWPE, not highly cross-linked). Stems and cups were cemented with a high-pressure technique using Palacos with gentamicin (Heraeus, Hanau, Germany). All arthroplasties were performed through a posterior approach in an operating room with laminar air flow. 70 patients were operated by the same senior orthopedic surgeon (AS). The remaining 15 patients were operated by 3 other senior orthopedic surgeons.
Study population and follow-up
The primary study cohort consisted of 85 patients (n = 41 MoM and n = 44 MoP) after application of the inclusion and exclusion criteria (). The mean age at surgery was 65 (45–74) years and the mean BMI was 27 (19–39). The mean follow-up time after the index surgery was 16 (15–17) years. Of the original 85 patients, 38 patients had died, 4 patients had undergone revision surgery, and 13 patients were lost to clinical follow-up (). We were thus able to evaluate clinically 30 patients and 29 of them radiographically after 16 years (n = 14 MoM and n = 16 MoP).
Quantification of metal ion concentrations
Serum samples were collected and analyzed preoperatively as previously described (Dahlstrand et al. Citation2009, Hailer et al. Citation2011). At latest follow-up, blood was drawn using an intravenous cannula with the stainless-steel needle removed and the first 5 mL of blood discarded. 5 mL glass containers without additive were used (Vacutainer, BD, New Jersey, USA). All blood samples were centrifuged at 2000 G for 10 minutes and the serum was then transferred to acid-washed polypropylene storage tubes and stored at –20 °C until analysis. All materials used in collecting and storing the samples were chosen for their lack of metallic trace elements.
All samples were analyzed by an accredited external laboratory specialized in quantification of trace elements (ALS Scandinavia AB, Lulea, Sweden) using inductively coupled plasma sector field mass spectrometry, ICP-SFMS (Element 2, Therma Scientific, Waltham, USA). The detection levels were 0.05 μg/L for Co and 0.5 μg/L for Cr.
Clinical parameters
1 observer blinded for the type of bearing evaluated all patients clinically at latest follow-up. The Harris hip score (HHS) was calculated and compared with preoperative values. At follow-up, all reoperations and revisions since the index surgery were reviewed. Serum creatinine was measured in all patients.
Radiographic outcome
Anteroposterior and lateral radiographs were taken at latest follow-up and compared with postoperative radiographs by 1 radiologist (MCW). Radiolucent lines were categorized in 7 Gruen zones and in 3 DeLee acetabular zones. Femoral stem subsidence was detected measuring the distance between the lateral part of the stem in relation to the greater trochanter. Changes exceeding 5 mm were considered as migration. Moreover, the cup inclination angle was determined.
Statistics
All variables are summarized using standard descriptive statistics such as frequencies, means, ranges, and standard deviations. The distributions of metal ion concentrations were positively skewed. Except for a few outliers with higher ion concentrations, the majority of the subjects were found at the lower ends of concentrations. Means and 95% confidence intervals (CI) were determined after calculating the natural logarithms of Co and Cr concentrations, allowing for parametric comparisons to be made between groups. Comparisons were made using Student’s t-test for equality of means and 2-tailed significance was determined. For analysis of categorical variables, a chi-square (Fisher’s exact) test was used. Implant survival was calculated using Kaplan–Meier survival analysis and differences in survival between groups were assessed by use of the Mantel–Cox log rank test. A 2-sided p-value of ≤0.05 was considered statistically significant. All analyses were performed using the PASW statistics package version 23 (SPSS Inc., Chicago, Illinois, USA).
Ethics, registration, funding, and potential conflicts of interest
This prospective randomized study was performed according to the Helsinki Declaration and the CONSORT Statement. All patients gave informed consent and ethical approval was granted by the Regional Ethical Review Board in Stockholm (approval number: 2013/2116-31/3). The study was not registered at https://clinicaltrials.gov since it started prior to the launch of that site in the year 2000. The study was financially supported by institutional funds only. All authors declare that they have no conflict of interest.
Results
Metal ion concentrations
We found that the mean Co concentration was more than 4 times higher in the MoM (1.5 μg/L) compared with the MoP cohort (0.4 μg/L) (p < 0.001). The Cr concentration in the MoM cohort was double that of the MoP cohort (MoM 2.2 μg/L versus MoP 1.0 μg/L, p = 0.05) (, ).
Figure 2. Serum cobalt (Co) and chromium (Cr) concentrations preoperatively and at follow-up (MoM = metal-on-metal, MoP = metal-on-polyethylene, error bars =95% CI).
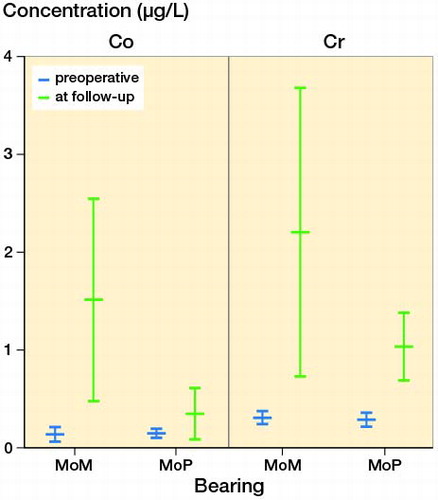
Table 1. Metal ion concentrations preoperatively and at follow-up after metal-on-metal (MoM) and metal-on-polyethylene (MoP) hip arthroplasty. Concentration (μg/L) values are mean (95% confidence interval)
Implant survival and reoperations
The cumulative 15-year survival with revision due to aseptic loosening as the endpoint was 96% (CI 88–100) in the MoM, and 97% (CI 91–100) in the MoP group.
In the MoM group, 1 patient had a revision of both the cup and stem due to aseptic loosening 13 years after the index operation. Another patient in that group had a cup and stem revision due to periprosthetic fracture after a fall 13 years postoperatively. In the MoP group, 1 patient had a cup revision due to recurrent dislocations 2 years postoperatively (no signs of loosening). A second patient in that group had a cup and stem revision due to aseptic loosening after 10 years. There were no macroscopic signs of metallosis or pseudotumors during revision surgery in any of the 4 mentioned cases. Moreover, there were no surgical procedures due to deep infection in either of the 2 groups during follow-up.
Clinical outcome
The mean HHS increased statistically significantly in both the MoM (from 38 to 91) and in the MoP cohort (from 37 to 95). The HHS was similar in both groups at latest follow-up. The mean creatinine level was 93 μmol/L for the MoM and 92 μmol/L for the MoP group at latest follow-up ().
Table 2. Patient characteristics. Values are numbers or mean (SD)
Radiographic outcome
There were no major differences concerning radiographic outcome when comparing the cemented cup and stem between the 2 groups. The radiolucent lines were evenly distributed in all 3 DeLee zones and in Gruen zones 1, 6, and 7 (). None of the implants migrated more than 5 mm. The cup inclination angle was similar in both groups (MoM 45° [CI 42–48] versus MoP 48° [CI 42–54]).
Table 3. Presence of radiolucent lines in cup zones (DeLee) and femoral zones (Gruen) at follow-up
Discussion
Failure of the MoM prosthesis may be indicated by high serum ion concentrations. We observed metal ion concentrations in a range similar to previous studies on the Metasul system. Zijlstra et al. (Citation2010) reported median values for Co with 1.1 μg/L and Cr with 1.0 μg/L at 10-year follow-up. Lazennec el al. (2009) documented median Co concentrations of 1.6 μg/L and Cr levels of 1.5 μg/L after 9 years. Migaud et al. (Citation2011) found a median Co concentration of 1.0 μg/L and Cr of 1.2 μg/L after 13 years. Savarino et al. (Citation2008) presented serum Co concentrations of 0.7 μg/L and Cr concentrations of 0.9 μg/L at 10-year follow-up. Patients suffering from severe disease in vital organs after surgery with MoM implants, where a high systemic load of Co and Cr was suspected to be the cause, showed in most cases ion concentrations that are 100- to 1000-fold of the mean concentrations seen in our study (Bradberry et al. Citation2014). No major renal function impairment was related to Metasul after 16-year follow-up in our patients, which is in accordance with other authors (Grubl et al. Citation2007, Marker et al. Citation2008, Migaud et al. Citation2011). Adverse reactions to metal debris such as metallosis, ALVAL, and pseudotumor that are complications often related to large diameter MoM heads (Haddad et al. Citation2011), were no reason for any reoperation in our cohort. The metal ion levels found in our study were far lower than the serum levels that are associated with metallosis (serum Cr levels >17 μg/L and serum Co levels >19 μg/L) (De Smet et al. Citation2008). Nevertheless, Hwang et al. (Citation2013) reported the development of 2 symptomatic cases with pseudotumors in a series of patients operated with the Metasul system, thus some concerns remain concerning small-diameter MoM THAs.
The head–neck taper metal junction may also be a source of corrosion creating additional metal debris in the joint (Osman et al. Citation2016). The elevation of Cr in our MoP-group at follow-up may be the result of the so called "trunnionosis" due to the modular head-neck components (Osman et al. Citation2016). Since a similar elevation was not seen in the Co concentration of the MoP group, another explanation could be that serum fractions from tubes without additives were analyzed at the 16-year follow-up compared with plasma fractions from tubes with sodium heparin at the previous follow-ups (Dahlstrand et al. Citation2009).
We observed small differences in 15-year implant survival between the 2 investigated groups (MoM 96% and MoP 97%). Our results concerning implant survival are similar to several other studies. Zijlstra et al. (Citation2010) followed 102 MoM and 98 MoP 28-mm diameter articulations and found an improved HHS at 10-year follow up and good implant survival in both groups (MoM 96% and MoP 97%). Eswaramoorthy et al. (Citation2008) reported a 94% prosthesis survival in 85 Metasul THAs after 10 years. Lass et al. (Citation2014) presented an 18-year survival rate of 93% with aseptic failure as the endpoint. The Metasul coupling demonstrated excellent survival in young patients with 100% at 12 years (Migaud et al. Citation2011) and 98% at 18 years (Hwang et al. Citation2013).
However, not all publications support these excellent results. Lazennec et al. (Citation2009) described a 9-year survival of 89% in 134 Metasul cups with revision for any reason, and 91% with revision for aseptic loosening as the endpoint. Bjorgul et al. (Citation2013) randomized 397 hips to receive Metasul MoM, MoP, or ceramic-on-polyethylene bearings in combination with a cemented stem. At 7-year follow-up, the MoM group had the lowest mean HHS, a higher rate of revision, and a higher incidence of radiolucent lines. The authors recommended that patients with 28-mm Metasul bearings should be followed carefully. Tardy et al. (Citation2015) revealed an implant survival rate of only 82% for aseptic revision and 88% for aseptic loosening in 106 Metasul THAs after 13 years. However, the authors concluded that most of the failures were not due to MoM bearing wear, but to other causes.
Both articulations in our study resulted in substantial clinical improvement at 16-year follow-up. The HHS increased in both groups and there was no difference between the MoM and MoP cohort at latest follow-up. A considerable improvement in the HHS at follow-up was described in other publications concerning the Metasul articulation (Lazennec et al. Citation2009, Saito et al. Citation2010, Zijlstra et al. Citation2010, Malek et al. Citation2015a).
Radiolucent lines around the cup were evenly distributed between DeLee zones 1 to 3 and there were no major differences between the MoM and MoP cohort. Only a few radiolucent lines were seen around the stem, mainly in Gruen zones 1, 6, and 7, without major differences between the 2 groups. We found no relationship between the occurrence of radiolucent lines and revisions. Most of the previous publications regarding the Metasul system report satisfactory radiographic outcome after long-term follow-up (Grubl et al. Citation2007, Dastane et al. Citation2011, Migaud et al. Citation2011, Randelli et al. Citation2012, Hwang et al. Citation2013, Innmann et al. Citation2014, Lass et al. Citation2014, Tardy et al. Citation2015). However, some authors questioned the durability of the Metasul cup due to early and progressive radiolucent lines and osteolysis (Levai et al. Citation2006, Nich et al. Citation2006, Malek et al. Citation2015a).
Our study has some limitations. Many patients had died (38/85) as a consequence of a high mean age at the index operation, and some patients were lost to follow-up (13/85) (). However, we have complete documentation on reoperations and implant survival on all patients. Because only 30 of our original 85 patients could be evaluated 16 years after the index surgery, we did not exclude patients who had had additional Co- and Cr-containing orthopedic implants at follow-up. This possible bias concerning metal ion concentrations should be considered when comparing our results with other publications. However, there was no statistically significant difference in the frequency of additional hip and knee implants between the 2 groups (). Metal ion analysis alone is not a very sensitive screening tool for adverse reactions to metal debris, which is often clinically "silent" (Malek et al. Citation2012). However, we did not use advanced imaging such as MRI, CT, or ultrasonography to establish or eliminate the presence of possible pseudotumors in our study. The Medicines and Healthcare products Regulatory Agency (MHRA) recommended in 2010 the use of whole blood to measure Co and Cr levels (Malek et al. Citation2015b). When we initiated the study in 1998, we chose to analyze serum metal ions, which was recommended at the time.
We did not perform a competing risk analysis. Competing risks such as death influence implant survival calculated according to Kaplan–Meier. Patients who died cannot be revised, and thus the risk of revision may be underestimated in elderly populations with long follow-up times and a relatively high mortality (Ranstam et al. Citation2011). However, since the mean age and death rate was similar in the 2 investigated groups, we may over-estimate general implant survival, but there is little reason to believe that a bias between groups would have been introduced.
Our prospective randomized study had an average follow-up of 16 years, which is quite long compared with other studies. There are no other prospective randomized trials comparing Metasul with other couplings with longer follow-up. The majority of surgeries were performed by a single surgeon who used the same technique and the same implants, which is a strength of our study.
In conclusion, the 2 investigated bearings did not differ statistically significantly regarding implant survival or radiographic results. It is reassuring that 28 mm MoM bearings seem safe and effective. However, serum Co and Cr concentrations were higher in the MoM compared with the MoP cohort. The use of MoM couplings raises concerns related to the long-term systemic increase of metal ion levels and possible adverse reactions to metal debris and ions. Due to the absence of clinical superiority of the MoM bearing and concerns regarding biological effects of MoM articulations we therefore recommend the use of MoP articulations.
HD: planning, data analysis, statistics, and writing; AS: planning, data analysis, and editing of the manuscript; MCW: data analysis and editing of the manuscript; LA: planning and editing of the manuscript; NPH and RJW: planning, data analysis, statistics, writing, and editing of the manuscript.
- Anissian H L, Stark A, Gustafson A, Good V, Clarke I C. Metal-on-metal bearing in hip prosthesis generates 100-fold less wear debris than metal-on-polyethylene. Acta Orthop Scand 1999; 70 (6): 578–82.
- Bernstein M, Desy N M, Petit A, Zukor D J, Huk O L, Antoniou J. Long-term follow-up and metal ion trend of patients with metal-on-metal total hip arthroplasty. Int Orthop 2012; 36 (9): 1807–12.
- Bisseling P, Smolders J M, Hol A, van Susante J L. Metal ion levels and functional results following resurfacing hip arthroplasty versus conventional small-diameter metal-on-metal total hip arthroplasty: A 3 to 5 year follow-up of a randomized controlled trial. J Arthroplasty 2015; 30 (1): 61–7.
- Bjorgul K, Novicoff W N, Andersen S T, Ahlund O R, Bunes A, Wiig M, Brevig K. High rate of revision and a high incidence of radiolucent lines around Metasul metal-on-metal total hip replacements: Results from a randomised controlled trial of three bearings after seven years. Bone Joint J 2013; 95-B (7): 881–6.
- Bradberry S M, Wilkinson J M, Ferner R E. Systemic toxicity related to metal hip prostheses. Clin Toxicol (Phila) 2014; 52 (8): 837–47.
- Dahlstrand H, Stark A, Anissian L, Hailer N P. Elevated serum concentrations of cobalt, chromium, nickel, and manganese after metal-on-metal alloarthroplasty of the hip: A prospective randomized study. J Arthroplasty 2009; 24 (6): 837–45.
- Dastane M, Wan Z, Deshmane P, Long W T, Dorr L D. Primary hip arthroplasty with 28-mm Metasul articulation. J Arthroplasty 2011; 26 (4): 662–4.
- De Smet K, De Haan R, Calistri A, Campbell P A, Ebramzadeh E, Pattyn C, Gill H S. Metal ion measurement as a diagnostic tool to identify problems with metal-on-metal hip resurfacing. J Bone Joint Surg Am 2008; 90 (Suppl 4): 202–8.
- Desmarchelier R, Viste A, Chouteau J, Lerat J L, Fessy M H. Metasul vs Cerasul bearings: A prospective, randomized study at 9 years. J Arthroplasty 2013; 28 (2): 296–302.
- Dorr L D, Wan Z, Longjohn D B, Dubois B, Murken R. Total hip arthroplasty with use of the Metasul metal-on-metal articulation: Four to seven-year results. J Bone Joint Surg Am 2000; 82 (6): 789–98.
- Dorr L D, Wan Z, Sirianni L E, Boutary M, Chandran S. Fixation and osteolysis with Metasul metal-on-metal articulation. J Arthroplasty 2004; 19 (8): 951–5.
- Eswaramoorthy V, Moonot P, Kalairajah Y, Biant L C, Field R E. The Metasul metal-on-metal articulation in primary total hip replacement: Clinical and radiological results at ten years. J Bone Joint Surg Br 2008; 90 (10): 1278–83.
- Grubl A, Marker M, Brodner W, Giurea A, Heinze G, Meisinger V, Zehetgruber H, Kotz R. Long-term follow-up of metal-on-metal total hip replacement. J Orthop Res 2007; 25 (7): 841–8.
- Haddad F S, Thakrar R R, Hart A J, Skinner J A, Nargol A V, Nolan J F, Gill H S, Murray D W, Blom A W, Case C P. Metal-on-metal bearings: The evidence so far. J Bone Joint Surg Br 2011; 93 (5): 572–9.
- Hailer N P, Blaheta R A, Dahlstrand H, Stark A. Elevation of circulating HLA DR(+) CD8(+) T-cells and correlation with chromium and cobalt concentrations 6 years after metal-on-metal hip arthroplasty. Acta Orthop 2011; 82 (1): 6–12.
- Hwang K T, Kim Y H, Kim Y S, Choi I Y. Is second generation metal-on-metal primary total hip arthroplasty with a 28 mm head a worthy option?: A 12- to 18-year follow-up study. J Arthroplasty 2013; 28 (10): 1828–33.
- Innmann M M, Gotterbarm T, Kretzer J P, Merle C, Ewerbeck V, Weiss S, Aldinger P R, Streit M R. Minimum ten-year results of a 28-mm metal-on-metal bearing in cementless total hip arthroplasty in patients fifty years of age and younger. Int Orthop 2014; 38 (5): 929–34.
- Kim S Y, Kyung H S, Ihn J C, Cho M R, Koo K H, Kim C Y. Cementless Metasul metal-on-metal total hip arthroplasty in patients less than fifty years old. J Bone Joint Surg Am 2004; 86-A (11): 2475–81.
- Lass R, Grubl A, Kolb A, Domayer S, Csuk C, Kubista B, Giurea A, Windhager R. Primary cementless total hip arthroplasty with second-generation metal-on-metal bearings: A concise follow-up, at a minimum of seventeen years, of a previous report. J Bone Joint Surg Am 2014; 96 (5): e37.
- Lazennec J Y, Boyer P, Poupon J, Rousseau M A, Roy C, Ravaud P, Catonne Y. Outcome and serum ion determination up to 11 years after implantation of a cemented metal-on-metal hip prosthesis. Acta Orthop 2009; 80 (2): 168–73.
- Levai J P, Descamps S, Roch G, Boisgard S. Early aseptic loosening of cemented cup in metal-on-metal total hip arthroplasties. Rev Chir Orthop Reparatrice Appar Mot 2006; 92 (6): 575–80.
- Long W T, Dorr L D, Gendelman V. An American experience with metal-on-metal total hip arthroplasties: A 7-year follow-up study. J Arthroplasty 2004; 19 (8 Suppl 3): 29–34.
- Malek I A, King A, Sharma H, Malek S, Lyons K, Jones S, John A. The sensitivity, specificity and predictive values of raised plasma metal ion levels in the diagnosis of adverse reaction to metal debris in symptomatic patients with a metal-on-metal arthroplasty of the hip. J Bone Joint Surg Br 2012; 94 (8): 1045–50.
- Malek I A, Rao S P, Rath N K, Mallya U N. Cemented metal-on-metal total hip replacement with 28-mm head: Prospective, long-term, clinical, radiological and metal ions data. Eur J Orthop Surg Traumatol 2015a; 25 (4): 749–55.
- Malek I A, Rogers J, King A C, Clutton J, Winson D, John A. The interchangeability of plasma and whole blood metal ion measurement in the monitoring of metal on metal hips. Arthritis 2015; 2015b: Article ID 216785.
- Marker M, Grubl A, Riedl O, Heinze G, Pohanka E, Kotz R. Metal-on-metal hip implants: Do they impair renal function in the long-term? A 10-year follow-up study. Arch Orthop Trauma Surg 2008; 128 (9): 915–19.
- Migaud H, Putman S, Krantz N, Vasseur L, Girard J. Cementless metal-on-metal versus ceramic-on-polyethylene hip arthroplasty in patients less than fifty years of age: A comparative study with twelve to fourteen-year follow-up. J Bone Joint Surg Am 2011; 93 (Suppl 2): 137–42.
- Nich C, Rampal V, Vandenbussche E, Augereau B. Metal-metal-backed polyethylene cemented hip arthroplasty: Mid-term results. Rev Chir Orthop Reparatrice Appar Mot 2006; 92 (2): 118–24.
- Osman K, Panagiotidou A P, Khan M, Blunn G, Haddad F S. Corrosion at the head-neck interface of current designs of modular femoral components: Essential questions and answers relating to corrosion in modular head-neck junctions. Bone Joint J 2016; 98-B (5): 579–84.
- Randelli F, Banci L, D’Anna A, Visentin O, Randelli G. Cementless Metasul metal-on-metal total hip arthroplasties at 13 years. J Arthroplasty 2012; 27 (2): 186–92.
- Ranstam J, Karrholm J, Pulkkinen P, Makela K, Espehaug B, Pedersen A B, Mehnert F, Furnes O, group N s. Statistical analysis of arthroplasty data. II. Guidelines. Acta Orthop 2011; 82 (3): 258–67.
- Saito S, Ishii T, Mori S, Hosaka K, Ootaki M, Tokuhashi Y. Long-term results of metasul metal-on-metal total hip arthroplasty. Orthopedics 2010; 33 (8). [Epub]
- Savarino L, Padovani G, Ferretti M, Greco M, Cenni E, Perrone G, Greco F, Baldini N, Giunti A. Serum ion levels after ceramic-on-ceramic and metal-on-metal total hip arthroplasty: 8-year minimum follow-up. J Orthop Res 2008; 26 (12): 1569–76.
- Sharma S, Vassan U, Bhamra M S. Metal-on-metal total hip joint replacement: A minimum follow-up of five years. Hip Int 2007; 17 (2): 70–7.
- Smith A J, Dieppe P, Vernon K, Porter M, Blom A W, National Joint Registry of E, Wales. Failure rates of stemmed metal-on-metal hip replacements: Analysis of data from the National Joint Registry of England and Wales. Lancet 2012; 379 (9822): 1199–204.
- Swedish Hip Arthroplasty Register, Annual Report 2015; http://www.shpr.se/en/.
- Tardy N, Maqdes A, Boisrenoult P, Beaufils P, Oger P. Small diameter metal-on-metal total hip arthroplasty at 13 years: A follow-up study. Orthop Traumatol Surg Res 2015; 101 (8): 929–36.
- Vendittoli P A, Riviere C, Roy A G, Barry J, Lusignan D, Lavigne M. Metal-on-metal hip resurfacing compared with 28-mm diameter metal-on-metal total hip replacement: A randomised study with six to nine years’ follow-up. Bone Joint J 2013; 95-B (11): 1464–73.
- Weber B G. Experience with the Metasul total hip bearing system. Clin Orthop Relat Res 1996; (329Suppl): S69–S77.
- Zijlstra W P, van Raay J J, Bulstra S K, Deutman R. No superiority of cemented metal-on-metal over metal-on-polyethylene THA in a randomized controlled trial at 10-year follow-up. Orthopedics 2010; 33 (3). [Epub]