Abstract
Background and purpose — No consensus exists on when to perform arthroscopic partial meniscectomy in patients with a degenerative meniscal tear. Since MRI and clinical tests are not accurate in detecting a symptomatic meniscal lesion, the patient’s symptoms often play a large role when deciding when to perform surgery. We determined the prevalence and severity of self-reported knee symptoms in patients eligible for arthroscopic partial meniscectomy due to a degenerative meniscal tear. We investigated whether symptoms commonly considered to be related to meniscus injury were associated with early radiographic signs of knee osteoarthritis.
Patients and methods — We included individual baseline items from the Knee injury and Osteoarthritis Outcome Score collected in 2 randomized controlled trials evaluating treatment for an MRI-verified degenerative medial meniscal tears in 199 patients aged 35–65 years. Each item was scored as no, mild, moderate, severe, extreme, and at least “mild” considering the symptoms present. Early radiographic signs of osteoarthritis, defined as a Kellgren and Lawrence grade of at least 1, were seen in 70 patients.
Results — At least monthly knee pain, pain during stair walking and when twisting on the knee, and lack of confidence in knee was present in at least 80% of the patients. Median severity was at least moderate for knee pain, pain when twisting on the knee, pain walking on stairs, lack of confidence in knee, and clicking. Mechanical symptoms such as catching were rare. Early radiographic signs of osteoarthritis were associated with an increased risk of self-reported swelling, catching, and stiffness later in the day; the odds ratio was 2.4 (95% CI 1.2–4.9), 2.3 (1.2–4.3), and 2.3 (1.1–5.0), respectively.
Interpretation — Middle-aged patients with a degenerative medial meniscus tear reported symptoms commonly associated with knee osteoarthritis. Frequent knee pain, presence of lack of confidence in the knee, and clicking did not distinguish those with a meniscal tear alone from those with early radiographic knee OA. Our findings support the notion that symptoms reported by those with a degenerative meniscal tear represent early signs of knee osteoarthritis.
MRI-verified meniscal tears are common in middle-aged and older individuals, with or without knee symptoms (Englund et al. Citation2008) and arthroscopic partial meniscectomy (APM) is one of the most commonly performed orthopedic procedures, carried out in at least half a million patients annually in the USA (Cullen et al. Citation2009). No consensus exists on when APM is indicated (Lyman et al. Citation2012) and several recent randomized controlled trials have reported no added benefit of APM compared with or in addition to non-surgical interventions (Thorlund et al. Citation2015, Kise et al. Citation2016). Further, the diagnostic criteria of a meniscal tear are not consistently defined and provision varies widely even within regions of the same country. MRI is increasingly used as a diagnostic tool. MRI can identify meniscal tears in symptomatic patients, but also detects asymptomatic meniscal tears in the general population (Englund et al. Citation2008). Even in the presence of a meniscal tear on MRI, coexisting knee osteoarthritis (OA) may be the primary cause of knee pain and symptoms (Englund et al. Citation2012). Thus, an MRI-verified tear in the presence of knee pain does not in itself provide an indication for APM. To identify whether the symptoms originate from the meniscal tear, the physician often relies on clinical tests. These tests are not accurate and repeat studies suggest that no single test can reliably diagnose symptomatic meniscal tears (Hegedus Citation2007).
Symptoms commonly considered related to meniscus injury include knee pain, giving way, and mechanical symptoms like clicking, locking, or catching, and there is some evidence for their validity in identifying symptomatic meniscal tears (Wagemakers et al. Citation2008, Niu et al. Citation2011). Patient-reported outcomes (PROs) are used to determine the patient’s perception of a disease, and the outcome from an intervention, but PROs are rarely used to obtain patient history or as diagnostic tools. This approach may, however, be appealing since PROs are not subjected to interviewer bias.
The aim of this study was, first, to determine the prevalence and severity of commonly assessed self-reported knee symptoms, including knee pain, clicking, catching, and giving way, by the use of a patient-administered questionnaire in middle-aged patients eligible for arthroscopic partial meniscectomy. Second, to investigate whether concomitant early radiographic signs of knee OA were associated with self-reported knee symptoms.
Patients and methods
We used a cross-sectional design and included baseline data collected in 2 different randomized controlled trials evaluating treatment of degenerative medial meniscal tears, the OMEX and the SLAMSHAM studies (ClinicalTrials.gov Identifier: NCT01002794 and NCT01264991) (Hare et al. Citation2013, Kise et al. Citation2016). The trials compared arthroscopic partial meniscectomy with exercise therapy or sham surgery, respectively. Patient characteristics, mean Knee injury and Osteoarthritis Outcome Score (KOOS) subscale scores and functional outcomes are published for the patients included in the OMEX study (Kise et al. Citation2016). Data on individual items from the KOOS have not been published.
Participants were between 35 and 65 years old with an MRI-verified degenerative medial meniscal tear, at least 2 months’ duration of knee pain and no previous significant trauma, found eligible for arthroscopic partial meniscectomy. Only patients with no or mild knee osteoarthritis (OA), Kellgren and Lawrence grade 0–2 (Kellgren and Lawrence Citation1957, Schiphof et al. Citation2011) were included. Eligibility for surgery was based on clinical examination by an orthopedic surgeon and the presence of a degenerative meniscal tear on MRI. An increased intra-meniscal signal (commonly a linear signal within the meniscus) was regarded as a meniscal tear when it communicated with the inferior or superior margin of the meniscus on at least 2 consecutive slices from the MRI investigation.
Patients were recruited through outpatient orthopedic clinics in Norway or Denmark between 2009 and 2013. In the OMEX study the sample size for the RCT determined the current study sample (n = 140). In the SLAMSHAM study, recruitment was at the time of data analysis still ongoing and study sample was determined by patients included in the RCT (n = 40) and by patients meeting all the inclusion criteria, but who declined participation, enrolled in a parallel cohort study (n = 19).
Assessments
Knee injury and Osteoarthritis Outcome Score (KOOS)
We used the KOOS to collect patient-reported knee symptoms (Roos et al. Citation1998). KOOS is validated for short- and long-term follow-up studies of knee injury and OA (Collins et al. Citation2016). KOOS questionnaires were filled out by the patients prior to randomization without the help of an interviewer. In the current study, we included all individual items from the subscales pain (7 items) and symptoms (9 items) and 1 item from subscale quality of life. These 17 items were selected since they represent clinical symptoms commonly thought to be associated with a meniscal tear (Wagemakers et al. Citation2008, Niu et al. Citation2011) (). Each item in KOOS is responded to by marking 1 of 5 response options on a Likert scale. For each individual item, presence of a symptom was defined as reporting at least mild symptoms; ticking the second to fifth out of the five Likert boxes representing no, mild, moderate, severe or extreme symptoms, or equivalent.
Radiographic scoring of the knee joint
The Kellgren and Lawrence (K&L) grade was used to assess structural disease severity. A preoperative weight-bearing posterior-anterior radiograph of both knees with a fixed-flexion radiography procedure, with use of SynaFlexer (Synarc, Newark, CA, USA), was performed. This provides radiography at the same position and is validated in determining joint-space width in knee osteoarthritis (Kothari et al. Citation2004). No radiograph of the patellofemoral joint was performed. Radiographs were assessed by an orthopedic surgeon when assessing patients for eligibility. A K&L grade of zero would imply no structural changes, a K&L grade of 1 a minor osteophyte of doubtful significance, and a K&L grade of 2 a definite osteophyte with unimpaired joint space (Kellgren and Lawrence Citation1957, Schiphof et al. Citation2011). Early radiographic knee OA was defined as a K&L score of 1 or 2.
Statistics
The prevalence of knee symptoms is given as the percentage with 95% confidence intervals (95% CI) and defined as patients reporting at least mild problems. Symptom severity is given as the median with interquartile range (IQR) for the severity grade (range, 0–4 (no, mild, moderate, severe, extreme or equivalent)) for each of the reported symptoms.
We used logistic regression to evaluate the association between concomitant structural disease and presence of a symptom while adjusting for age, gender, and BMI. Odds ratio, 95% CI, and p-values are given for all regression analyses.
Ethics, registration, funding, and potential conflicts of interest
The SLAMSHAM and OMEX studies are approved by the Research Ethics Committee of Region Zealand, Denmark and the Regional Ethical Committee, Health Region South-East, Oslo, Norway, respectively. Both studies are consistent with the Declaration of Helsinki and registered on ClinicalTrials.gov (Identifier: NCT01002794 and NCT01264991).
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. No authors have any conflict of interest to declare.
Results
The average age of the 199 patients was 48 years and 41% were women. 36% of the patients had early radiographic knee OA ().
Prevalence of symptoms with 95% CI in patients with an MRI-verifi ed degenerative meniscal tear and considered eligible for arthroscopic partial meniscectomy.
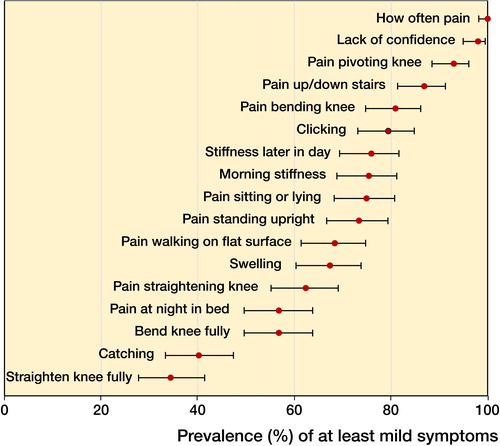
Table 1. Demographics of patients with an MRI-verified meniscal tear found eligible for arthroscopic partial meniscectomy
The 4 most commonly reported symptoms were frequent knee pain, lack of confidence in knee, pain when pivoting/twisting, and pain when walking up or down stairs. All 4 symptoms were reported by more than 80% of the patients (Figure). The least commonly reported symptoms were catching and difficulty straightening the knee fully, reported by less than 40% of the patients. All other symptoms were reported by 50–80% of the patients.
The median frequency for knee pain was “daily”, on a scale ranging from never, monthly, weekly, and daily to always. The median severity was “moderate” on a scale from no problems, mild, moderate, and “severe” to “extreme” for the following items: lack of confidence in knee, clicking, pain when pivoting/twisting, pain when walking up or down stairs, and pain when bending knee fully. The median for the 2 items with lowest severity, catching and difficulty straightening knee fully, was “no problems”. For the remaining 9 items, the median severity was “mild”.
The adjusted analysis for the association of early radiographic knee OA with presence of each of the 17 symptoms indicated that early structural disease (grade 1 or 2 on the K&L scale) was associated with a higher risk of self-reported swelling, catching, and stiffness later in the day than of no radiographic osteoarthritis ().
Table 2. Logistic regression analysis of association between radiographic knee OA and knee symptoms
Discussion
Key results
In this cross-sectional study of middle-aged patients eligible for APM we aimed to determine the prevalence and severity of self-reported knee symptoms and the association of early radiographic knee OA with presence of these symptoms. We found a prevalence of more than 80% of at least a moderate severity of the self-reported symptoms knee pain, lack of confidence, pain when pivoting/twisting, and pain walking up/down stairs. Mechanical symptoms such as catching and difficulty straightening knee were neither frequent nor severe. Early radiographic signs of knee OA were associated with higher risk of swelling, catching, and stiffness later in day.
Limitations
There are some limitations to our study. The cross-sectional design of the study did not allow for analysis of predictors of the outcome or causality. In addition, diagnostic sensitivity and specificity could not be determined since we had no “control group”, i.e. patients considered eligible by the surgeon but who failed to demonstrate a meniscal lesion on MRI. Another limitation is the use of RCT baseline data for a cohort study. Randomized trials have strict inclusion and exclusion criteria, and, despite being set to optimize external validity, included patients are more selected than if data from the full population having meniscus surgery had been included. Finally, the patellofemoral joint was not evaluated by MRI and a contribution of a possible engagement with the symptoms reported cannot be determined.
We defined early radiographic signs of knee OA as Kellgren and Lawrence grade ≥1. Commonly, a cut-off point of 2 on the K&L scale is used for definite radiographic knee OA (Kellgren et al. Citation1957). However, several studies have shown a strong association between the presence of osteophytes on radiography and the presence of self-reported symptomatic knee OA confirmed by MRI or arthroscopic visualization (Zhang et al. Citation2010). Therefore, we used K&L grade 1 as the cut-off point for concomitant radiographic signs of early knee OA.
Interpretation
Prevalence of symptoms
A recent study examined the reliability and validity of the clinical history relevant to meniscal tear (Niu et al. Citation2011). As a result, a Meniscal Symptom Index (MSI) consisting of 4 symptoms (localized pain, giving way, clicking, and catching) was identified to help standardize the clinical history ascertained by the clinician and eligibility for arthroscopic partial meniscectomy. The 4 symptoms included in the MSI were all to a varying degree present in our population.
Knee pain was present in all patients and had the greatest severity of all symptoms. This was expected since knee pain was one of the inclusion criteria for the RCTs from where our data were collected and is the most common symptom leading to APM (Lyman et al. Citation2012). The self-reported prevalence and severity of lack of confidence in the knee was also high. “Lack of confidence” is related but not identical to “giving way”, which is the wording used in the MSI. Asking patients about confidence in their knee is closely related to the extent to which the patient is actually troubled by his/her knee giving way as opposed to experiencing an actual giving way episode. Clicking is often thought to be a sound emanating from the meniscus subluxating from its place in the knee joint. However, clicking was not more common or severe than other self-reported symptoms.
Catching was the least reported symptom of all. This finding may seem surprising since catching is almost universally considered an absolute indication for surgery (Lyman et al. Citation2012). Other authors also reported a low incidence of catching/locking in cohorts defined by having meniscal tears (Wagemakers et al. Citation2008, Niu et al. Citation2011). Studies have shown that patients with catching may get better without surgery (Lim et al. Citation2009) and in 2 recent studies of arthroscopic partial meniscectomy, patients reporting catching or locking symptoms did not gain more benefit from APM than those without (Sihvonen et al. Citation2013, Gauffin et al. Citation2014). Therefore, even though catching or locking is generally acknowledged as an indication for meniscal surgery the evidence for its relation to a meniscal tear or being an added benefit from partial meniscectomy is scant.
We found 2 symptoms not included in the MSI, which were of high self-reported frequency and severity: pain when pivoting/twisting and pain going up/down stairs. Niu et al. (Citation2011) also reported a high incidence of pain on pivoting/twisting but this item was excluded from the MSI due to a low positive predictive value indicating that other knee conditions were more likely to produce this symptom. Pain going up/down stairs has not been previously described as a prevalent symptom in those with a meniscal tear and is thought to be more common in those with patellofemoral osteoarthritis (Chan et al. Citation2014). Radiography of the patellofemoral joint was not performed in our study to evaluate this possibility. It seems, however, that pain going up or down stairs is also common in cohorts defined by having structural damage in the tibiofemoral joint (Englund et al. Citation2005).
Association of knee symptoms with radiographic knee OA
Frequent knee pain, presence of lack of confidence in the knee, and clicking did not distinguish those with a meniscal tear alone from those with concomitant early radiographic knee OA. These symptoms were not specific to those with an MRI-verified degenerative meniscal tear only, and are common in patients with radiographic and symptomatic knee OA (Dieppe and Lohmander Citation2005) supporting that they represent early signs of knee OA. Indeed, Niu et al. (Citation2011) when developing the Meniscal Symptom Index reported that patients with concomitant knee OA had a higher prevalence of the symptoms included in the MSI compared with patients who had no knee OA. We found that, in the presence of a meniscal tear, concomitant early radiographic knee OA was associated with a higher risk of self-reported catching, swelling, and stiffness later in the day. No other differences in presence of symptoms were found. Swelling and stiffness are well-known symptoms in patients with knee OA. Catching, however, is more commonly recognized as a mechanical symptom, usually considered as emanating from a meniscal tear. A high prevalence of catching in those with knee OA indicates that the main cause of catching is not the meniscal tear in itself but instead the degenerative process of OA involving several structures of the joint. Our findings support previous reports suggesting that a degenerative meniscal tear is an early feature of knee OA (Englund et al. Citation2012, Guermazi et al. Citation2012).
The selection of patients with a medial meniscal tear eligible for APM is debated (Lyman et al. Citation2012, Jarvinen et al. Citation2014). The presence and severity of certain knee symptoms continues to play a prominent role in determining eligibility for surgery among the proponents of this intervention. However, we found that preoperative symptoms did not distinguish patients with overlapping knee conditions of degenerative meniscal tears and signs of structural disease in other joint structures including bone and cartilage. In our study, catching was more likely related to OA rather than the meniscal tear itself. The common use of catching as an indication for arthroscopic knee surgery in middle-aged patients with a degenerative meniscal tear is questionable and should be abandoned (Sihvonen et al. Citation2016).
In summary
Frequent knee pain, presence of lack of confidence in the knee, and clicking did not distinguish those with a meniscal tear alone from those with concomitant early radiographic knee OA. Our findings support the notion that symptoms reported by those with an MRI-verified degenerative meniscal tear should be considered as early signs of knee OA, and that neither mechanical nor other symptoms are attributable to the degenerative meniscal tear as such, but rather to the ongoing osteoarthritic process.
KBH, LSL, and EMR designed the study. KBH and NJK were responsible for data collection, while KBH analyzed the data and drafted the manuscripts. All authors contributed to the interpretation of data and to revision of the manuscript.
We would like to thank Silje Stensrud for collecting data in the OMEX study.
Acta thanks Raine Sihvonen and other anonymous reviewers for help with peer review of this study.
- Chan K K, Sit R W, Wu R W, Ngai A H. Clinical, radiological and ultrasonographic findings related to knee pain in osteoarthritis. PLoS ONE 2014; 9 (3): e92901.
- Collins N J, Prinsen C A, Christensen R, Bartels E M, Terwee C B, Roos E M. Knee Injury and Osteoarthritis Outcome Score (KOOS): Systematic review and meta-analysis of measurement properties. Osteoarthritis Cartilage 2016; 24 (8): 1317–29.
- Cullen K, Hall M, Golosinskiy A. Ambulatory surgery in the United States, 2006. National health statistics reports, National Center for Health Statistics 2009; 11: 1–28.
- Dieppe P, Lohmander L. Pathogenesis and management of pain in osteoarthritis. Lancet 2005; 365 (9463): 965–73.
- Englund M, Lohmander L S. Patellofemoral osteoarthritis coexistent with tibiofemoral osteoarthritis in a meniscectomy population. Ann Rheum Dis 2005; 64 (12): 1721–6.
- Englund M, Guermazi A, Gale D, Hunter D J, Aliabadi P, Clancy M, Felson D T. Incidental meniscal findings on knee mri in middle-aged and elderly persons. N Engl J Med 2008; 359 (11): 1108–15.
- Englund M, Roemer F W, Hayashi D, Crema M D, Guermazi A. Meniscus pathology, osteoarthritis and the treatment controversy. Nat Rev Rheumatol 2012; 8 (7): 412–19.
- Gauffin H, Tagesson S, Meunier A, Magnusson H, Kvist J. Knee arthroscopic surgery is beneficial to middle-aged patients with meniscal symptoms: A prospective, randomised, single-blinded study. Osteoarthritis Cartilage 2014; 22 (11): 1808–16.
- Guermazi A, Niu J, Hayashi D, Roemer F W, Englund M, Neogi T, Aliabadi P, McLennan C E, Felson D T. Prevalence of abnormalities in knees detected by MRI in adults without knee osteoarthritis: population based observational study (Framingham Osteoarthritis Study). BMJ 2012; 29 (345): e5339.
- Hare K B, Lohmander L S, Christensen R, Roos E M. Arthroscopic partial meniscectomy in middle-aged patients with mild or no knee osteoarthritis: A protocol for a double-blind, randomized sham-controlled multi-centre trial. BMC Musculoskeletal Disorders 2013; 14 (1): 71.
- Hegedus E J. Physical examination tests for assessing a torn meniscus in the knee: A systematic review with meta-analysis. J Orthop Sports Phys Ther 2007; 37: 541–50.
- Jarvinen T L, Sihvonen R, Englund M. Arthroscopy for degenerative knee: A difficult habit to break? Acta Orthop 2014; 85 (3): 215–17.
- Kellgren J H, Lawrence J S. Radiological assessment of osteoarthrosis. Ann Rheum Dis 1957; 16 (4): 494–502.
- Kise N J, Risberg M A, Stensrud S, Ranstam J, Engebretsen L, Roos E M. Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: Randomised controlled trial with two year follow-up. BMJ 2016; 354: i3740.
- Kothari M, Guermazi A, Ingersleben G, Miaux Y, Sieffert M, Block J, Stevens R, Peterfy C. Fixed-flexion radiography of the knee provides reproducible joint space width measurements in osteoarthritis. Eur Radiol 2004; 14 (9): 1568–73.
- Lim H C, Bae J H, Wang J H, Seok C W, Kim M K. Non-operative treatment of degenerative posterior root tear of the medial meniscus. Knee Surg Sports Traumatol Arthrosc 2009; 18 (4): 535–9.
- Lyman S, Oh L S, Reinhardt K R, Mandl L A, Katz J N, Levy B A, Marx R G. Surgical decision making for arthroscopic partial meniscectomy in patients aged over 40 years. Arthroscopy 2012; 28 (4): 492–501.
- Niu N N, Losina E, Martin S D, Wright J, Solomon D H, Katz J N. Development and preliminary validation of a meniscal symptom index. Arthritis Care Res 2011; 63 (2): 208–15.
- Roos E M, Roos H P, Lohmander L S, Ekdahl C, Beynnon B D. Knee Injury and Osteoarthritis Outcome Score (KOOS): Development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998; 28 (2): 88–96.
- Schiphof D, de Klerk B, Kerkhof H, Hofman A, Koes B, Boers M, Bierma-Zeinstra S. Impact of different descriptions of the Kellgren and Lawrence classification criteria on the diagnosis of knee osteoarthritis. Ann Rheum Dis 2011; 70 (8): 1422–7.
- Sihvonen R, Paavola M, Malmivaara A, Itälä A, Joukainen A, Nurmi H, Kalske J, Järvinen T L N. Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 2013; 369 (26): 2515–24.
- Sihvonen R, Englund M, Turkiewicz A, Jarvinen T L. Mechanical symptoms as an indication for knee arthroscopy in patients with degenerative meniscus tear: A prospective cohort study. Osteoarthritis Cartilage 2016; 24 (8): 1367–75.
- Thorlund J B, Juhl C B, Roos E M, Lohmander L S. Arthroscopic surgery for degenerative knee: Systematic review and meta-analysis of benefits and harms. BMJ 2015; 350: h2747.
- Wagemakers H P, Heintjes E M, Boks S S, Berger M Y, Verhaar J A, Koes B W, Bierma-Zeinstra S M. Diagnostic value of history-taking and physical examination for assessing meniscal tears of the knee in general practice. Clin J Sport Med 2008; 18: 24–30.
- Zhang W, Doherty M, Peat G, Bierma-Zeinstra M A, Arden N K, Bresnihan B, Herrero-Beaumont G, Kirschner S, Leeb B F, Lohmander L S, Mazieres B, Pavelka K, Punzi L, So A K, Tuncer T, Watt I, Bijlsma J W. EULAR evidence-based recommendations for the diagnosis of knee osteoarthritis. Ann Rheum Dis 2010; 69 (3): 483–9.
