Sir,—It was with great interest we read the article “High failure rate after internal fixation and beneficial outcome after arthroplasty in treatment of displaced femoral neck fractures in patients between 55 and 70 years: An observational study of 2,713 patients reported to the Norwegian Hip Fracture Register” by Bartels et al. (2018).
The article raised a lot of questions and we would like to make some comments regarding the conclusions drawn by the authors.
The authors concluded that younger patients operated on with an arthroplasty had a better health-related quality of life (EQ-5D), less pain, and better patient satisfaction compared with those patients operated on with internal fixation (IF).
First, in our opinion the follow-up was too short for studying surgical complications after an arthroplasty. The reason why an arthroplasty has not been the treatment of choice in younger age is the risk for long-term complications. It is therefore unclear why the follow-up was as short as one year.
Second, since this is a register study and not a RCT study it is a biased situation and there seem to be a lot of uncontrolled confounders, as always in register studies. Already in the choice of surgical treatment there is selection bias, i.e. the IF group consisted of considerably more men compared with the arthroplasty groups. This finding is not discussed at all. In the light of experience we know that younger men with hip fractures often have other considerable comorbidities and high alcohol consumption, factors that may have influenced the PROM data.
Furthermore there were only 549 out of 2,713 patients (20%) that answered the patient questionnaires (PROM). This leads to a problem with the external validity and the generalizability of the findings and is only mentioned briefly by the authors.
The authors have chosen to analyze patients with healed fractures together with those who had reoperation (IF group). This might have led to false low mean values (PROM), and further to the conclusion drawn by the authors, of a beneficial outcome of an arthroplasty compared with the IF group. The majority of the patients who did not need reoperation (70%), and therefore would be of greater interest to discuss, would probably have a higher EQ-5D index score if the groups were analyzed separately. This has been found in an earlier study (Campenfeldt et al. 2017). It is clear that those patients who need reoperation after IF suffer, but it is still unclear what the clinical outcomes are for the absolute majority of the IF group—those whose fractures heal. This is a relevant scientific question that still needs to be answered and this is not addressed at all in the present study.
Furthermore, the differences found in VAS and EQ-5D after 12 months between groups were low and the clinical relevance is questionable and consequently also the conclusion drawn by the authors.
Sir,—We thank Dr Hedström and colleagues for the comments on our recently published article.
The results of our study are not controversial; they actually confirm the results from randomized controlled studies, albeit in a slightly younger population. In RCTs on healthy individuals aged over 60 years, both Keating et al. (2006) and Frihagen et al. (2007) found better results after arthroplasty than after internal fixation. The strength of the current study is to confirm this in a national population, a finding with high external validity. The limitations are, as pointed out by Hedström and colleagues, the difficulties in obtaining patient-reported outcome from elderly patients. However, the Norwegian Hip Fracture Register is unique in its ambitions to achieve truly national reporting of PROM. The risk of residual confounding is addressed in the discussion. This is the downside of register studies. Nevertheless, national register studies are needed as a valuable complement to RCTs, thanks to their generalizability and large study population.
Hedström and colleagues suggest that a larger share of men with alcohol abuse in the IF group would lower the group’s mean PROM results. A pragmatic answer would be that these individuals are more often non-responders than responders.
We do agree that reoperation after THA can occur late. Chammout et al. (2012) followed patients with a mean age of 68 years for 17 years. 4 of 43 THA patients had reoperations between 4 and 9 years later. On the other hand, 20 of 57 IF patients had conversion to THA within 2 years, i.e. they were exposed to secondary THA with a known higher risk of revisions than a primary THA. As a final result after IF, 2 had Girdlestone procedures, 2 deep infections, and 1 was revised due to aseptic loosening. Thus starting with IF is apparently no guarantee to avoid revision of arthroplasties.
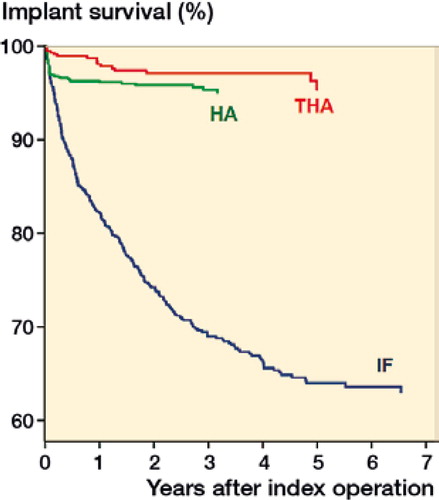
In our study, the patients had 1-year follow-up for PROM data and up to 8 years’ follow-up for implant-related problems. As seen in from our article, no major reoperations occurred later than 3 years postoperatively after hemiarthroplasty or later than 5 years postoperatively after total hip arthroplasty. This is in line with another study reporting no major reoperations between 2 and 5–7 years postoperatively in a medium follow-up of cemented hemiarthroplasties (Støen et al. 2014). In addition, patients with healed fractures do not gain a functional advantage or better relief from pain than those with uncomplicated replacements (Keating et al. 2006, Frihagen et al. 2007, Gjertsen et al. 2010, Leonardsson et al. 2010). Finally, to focus on only those with healed fractures after fixation is not meaningful from a patient point of view, as patients cannot choose whether to have successful healing or not.
Figure 2 Adjusted survival of implants for the different treatment groups with major reoperations as endpoint, distributed by primary treatment method. Cox regression analyses with adjustments for age, sex, and ASA classification (Bartels et al. (2018)).
In summary, with all respect for the caveats mentioned by Hedström and colleagues, we still think our conclusion that patients between 55 and 70 years of age with displaced intracapsular femoral neck fractures may benefit from treatment with arthroplasty is scientifically sound. The acceptance of such a suggestion is reflected by THA already being more common as primary treatment for displaced femoral neck fractures than IF in Sweden when patients reach around 58 years old (Swedish Fracture Register, Annual Report 2017).
Chammout G K, Mukka S S, Carlsson T, Neander G F, Stark A W, Skoldenberg O G. Total hip replacement versus open reduction and internal fixation of displaced femoral neck fractures: a randomized long-term follow-up study. J Bone Joint Surg Am 2012; 94(21): 1921-8.
Frihagen F, Nordsletten L, Madsen J E. Hemiarthroplasty or internal fixation for intracapsular displaced femoral neck fractures: randomised controlled trial. BMJ 2007; 335(7632): 1251-4.
Gjertsen J E, Vinje T, Engesaeter L B, et al. Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Joint Surg Am 2010; 92: 619-28.
Keating J F, Grant A, Masson M, Scott N W, Forbes JF . Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty: treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am 2006; 88(2): 249-60.
Leonardsson O, Sernbo I, Carlsson A, Akesson K, Rogmark C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures: results at ten years in a randomised study of 450 patients. J Bone Joint Surg Br 2010; 92(3): 406-12.
Støen R Ø, Lofthus C M, Nordsletten L, Madsen J E, Frihagen F. Randomized trial of hemiarthroplasty versus internal fixation for femoral neck fractures: no differences at 6 years. Clin Orthop Relat Res 2014; 472: 360-7.
Swedish Fracture Register Annual Report; 2017. https://stratum.registercentrum.se/#!page?id=1525
