Abstract
Background and purpose — In total hip replacements, stem design may affect the occurrence of periprosthetic femoral fracture. We studied risk factors for fractures around and distal to the 2 most used cemented femoral stems in Sweden.
Patients and methods — This is a register study including all standard primary Lubinus SPII and Exeter Polished stems operated in Sweden between 2001 and 2009. The outcome was any kind of reoperation due to fracture around (Vancouver type B) or distal to the stem (Vancouver type C), with use of age, sex, diagnosis at primary THR, and year of index operation as covariates in a Cox regression analysis. A separate analysis of the primary osteoarthritis patient group was done in order to evaluate eventual influence of the surgical approach (lateral versus posterior) on the risk for Vancouver type B fractures.
Results — The Exeter stem had a 10-times (95% CI 7–13) higher risk for type B fractures, compared with the Lubinus, while no statistically significant difference was noticed for type C fractures. The elderly, and patients with hip fracture or idiopathic femoral head necrosis, had a higher risk for both fracture types. Inflammatory arthritis was a risk factor only for type C fractures. Type B fractures were more common in men, and type C in women. A lateral approach was associated with decreased risk for Type B fracture.
Interpretation — Stem design influenced the risk for type B, but not for type C fracture. The influence of surgical approach on the risk for periprosthetic femoral fracture should be studied further.
Periprosthetic femoral fracture (PPFF) is more common in uncemented stems (Hailer et al. Citation2010, Thien et al. Citation2014, Abdel et al. Citation2016). In cemented stems, higher risk for fracture has been reported for “force-closed” (e.g., Exeter Polished, CPT), compared with “shape-closed” stems like Lubinus SPII and Charnley (Lindahl et al. Citation2005, Thien et al. Citation2014, Broden et al. Citation2015, Palan et al. Citation2016). However, most of the previous studies have focused on fractures treated with stem revision (Thien et al. Citation2014, Palan et al. Citation2016), and hence mainly fractures around a loose stem. It is probable that the shape and the surface finish of the stem contribute to the risk for Vancouver type B fractures (fractures around or close to a femoral stem) (Broden et al. Citation2015, Palan et al. Citation2016). Little research has been done to investigate whether the design of the stem can affect the risk for suffering a fracture distal to the stem (Vancouver type C) (Lowenhielm et al. Citation1989).
The majority of hip arthroplasty registries report only primary procedures and revisions. Therefore, type C fractures, treated in principle with open reduction and internal fixation (ORIF) without revision, are not reported. A recent register study from Sweden (Chatziagorou et al. Citation2018), revealed that only 17% of these fractures were reported to the Swedish Hip Arthroplasty Register (SHAR). Type C fractures were numerically more common among Lubinus SPII stems, while type B fractures predominated after insertion of an Exeter stem. These figures were, however, not related to the numbers at risk in each group. We are not aware of any study where the majority of type C fractures treated without revision were included. Nothing is known regarding the influence of surgical approach on the risk for postoperative periprosthetic fracture around a total cemented hip prosthesis.
Both the Exeter and the Lubinus stems are frequently used in Sweden. Between 2000 and 2016, 104,081 Lubinus SPII and 53,358 Exeter stems were used in primary total hip replacements (THR) (Karrholm et al. Citation2017). This corresponds to two-thirds of all primary THRs during this period. Previous studies have shown that Exeter stems run increased risk of revision due to periprosthetic fractures, whereas less is known about the risk for reoperation including also operative treatment with osteosynthesis and without stem exchange.
We compared the Lubinus SPII and the Exeter Polished stem as risk factors for Vancouver type B and C fractures. Other risk factors studied were age, sex, diagnosis at the primary THR, year of index operation, and surgical approach. We hypothesized that Lubinus stems might run an increased risk of type C fractures because of the high resistance of this stem to undergoing type B fractures ending up in a revision. To include all types of surgical procedures of the operated femur with relation to the hip prosthesis inserted, our primary outcome was any reoperation due to periprosthetic fracture.
Patients and methods
All primary standard Lubinus SPII and Exeter Polished stems used in THRs between 2001 and 2009, and reported to the SHAR, were included. We studied reoperations for any reason, and specifically due to PPFF between 2001 and 2011, to include a minimum of 2 years’ follow-up (maximum follow-up 11 years). Follow-up ended at the date of reoperation for any reason, death, emigration, or on December 31, 2011, whichever came first. Reoperation was defined as any further surgical intervention related to the index hip arthroplasty irrespective of whether the prosthesis or parts of it have been exchanged, extracted, or left untouched. All type A fractures (fractures of the greater and lesser trochanter), conservatively treated periprosthetic fractures, and fractures occurring during insertion of a primary stem (intraoperative fractures) were excluded. The SHAR records stem characteristics prospectively, for all primary and secondary arthroplasties. Stem length is one of these parameters, and during the study period (2001–2011), the standard length for both involved stems was 150 mm. Stem lengths other than 150mm were excluded. Further exclusion criteria are presented in a flow chart (). Surgical treatment of fracture types excluded for various reasons was labelled as reoperation due to causes other than PPFF in the analyses ().
Figure 1. Flow chart. Of the 73,630 originally included patients, 70,981 remained for analysis. Standard stem length was 150 mm for both Exeter and Lubinus SPII.
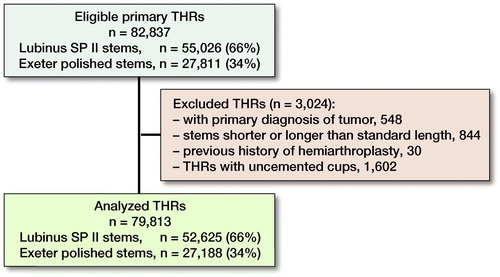
Table 1. Periprosthetic fractures (n = 31) primarily excluded
Data for the primary THRs and the reoperations were derived from the SHAR. The reporting of primary hip arthroplasties is almost complete (98%) (Karrholm et al. Citation2017), whereas the reporting of reoperations is poorer (Söderman et al. Citation2000, Lindgren et al. Citation2014). Therefore, data linking was done between the SHAR and the National Patient Register (NPR), in order to detect even PPFFs not registered with the SHAR. Cross-matching for the other types of reoperations was not done. The NPR holds information on all inpatient care since 1987, and all outpatient care since 2001. Both private and public healthcare providers have had to report to the NPR since 2001. All medical records of reoperations due to fracture were collected and scrutinized to detect all femoral fractures in patients with a primary THR. The information provided in the case records was also used for fracture classification by GC, according to the Vancouver classification system (Brady et al. Citation1999). A detailed description of the classification process, as well as its validation, is described in a previous publication (Chatziagorou et al. Citation2018). Bilateral observations were included as previous studies have indicated that this will not cause significant problems related to dependency (Ranstam et al. Citation2011).
Statistics
Statistical calculations were done using IBM SPSS statistics 23 (IBM Corp, Armonk, NY, USA). To identify eventual demographic differences between the Lubinus and the Exeter group, a chi-squared test and Mann–Whitney test were used. The 10-year survival was calculated with Kaplan–Meier analysis (log rank test). We plotted survival curves for the covariates included, and log–log plots to test that the Cox proportional hazard model was fulfilled. A Cox regression model was used to analyze the relative risk for reoperation due to PPFF. Adjustment for age, sex, type of stem, and diagnosis at the time of primary THR, as well as the year of index operation, was performed. The distribution of the population into age groups was done according to the age at the time of the primary operation. The aim was to have as equally sized groups as possible. Diagnosis was separated into primary osteoarthritis (OA), inflammatory arthritis, hip fracture, idiopathic femoral head necrosis, and various (including sequel to childhood hip disease). Censored were cases with cause of reoperation other than PPFF, excluded cases (), patients who died without any reoperation, or those who had not been reoperated until the end of 2011. The surgical approach (lateral versus posterior), as a risk factor for Vancouver type B fracture, was studied in a subgroup analysis. Complete information on surgical approach was available in 43,639 Lubinus and in 22,271 Exeter cases with primary OA. Missing data were 9 cases for each stem (). In the other groups of diagnoses, up to 97.5% (hip fracture) had missing information. Therefore, we chose to include only those patients operated due to primary OA and with a lateral or posterior incision. P-values were 2-sided with a significance level < 0.05, and 95% confidence intervals (CI) were calculated.
Table 6. Distribution of surgical approach among hips with primary OA. Values are frequency (%)
Ethics, funding, and potential conflicts of interest
The study was approved by the Central Ethical Review Board in Gothenburg (Entry number: 198-12, Date: 2012-04-05). There was no financial support for this research. The authors declare no conflict of interest.
Results
Study population
Between 2001 and 2009, 82,837 primary Lubinus SPII and Exeter Polished femoral stems were inserted in 73,630 patients. The data linking with the NPR resulted in a total of 626 PPFFs (295 of these were registered only in NPR), giving 4,233 reoperations between 2001 and 2011. After the exclusions ( and ), there were 79,813 primary THRs (70,981 patients), with 2,626 first-time reoperations (2,597 patients) left for analysis. 465 of the reoperations (462 patients) were due to periprosthetic femoral fracture. The mean follow-up time was 5.6 years. A slightly higher proportion of men was noted in the Lubinus SPII group (). The Exeter group had, proportionally, more patients classified as idiopathic femoral head necrosis and “various.” The cups used with the Lubinus and the Exeter stems are presented in .
Table 2. Patient demographics and reoperations
Table 3. Type of cups (all cemented) used with Lubinus SPII and Exeter Polished stems. Values are frequency (%)
Vancouver type and risk factors
The proportion of reoperations due to PPFF was higher in the Exeter than in the Lubinus group, as reflected in the survival analyses (, ). The commonest fracture type observed after insertion of a Lubinus SPII stem was Vancouver type C (74%), whereas type B fractures were more common after use of Exeter Polished stems (73%, ). The Exeter stem had a 3.5-times higher risk for PPFF (B or C), and a 9.6-times higher risk for type B fracture when compared with the Lubinus SPII (). There was no statistically significant difference between the 2 groups regarding the risk of type C fracture.
Figure 2. Cumulative survival (unadjusted) for periprosthetic femoral fracture. Numbers at risk at the end of 10 years’ follow-up were: 2,903 for the Lubinus SPII group, and 1,518 for the Exeter Polished group. 2(a): All fractures studied (Type B and C fractures). Mean survival at 10 years was 99.4% (SE 0.06) for the Lubinus SPII, and 97.9% (SE 0.17) for the Exeter Polished (log rank test p < 0.001). 2(b): Type B fractures. Mean survival at 10 years was 99.8% (SE 0.04) for the Lubinus SPII, and 98.6% (SE 0.11) for the Exeter Polished (log rank test p < 0.001). 2(c): Type C fractures. Mean survival at 10 years was 99.6% (SE 0.05) for the Lubinus SPII, and 99.3% (SE 0.11) for the Exeter Polished (log rank test p = 0.08).
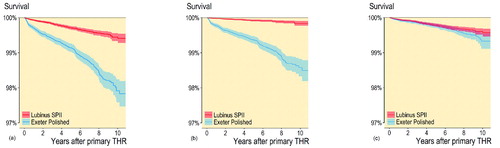
Table 4. Distribution of periprosthetic femoral fractures according to the Vancouver classification system. Values are frequency (%)
Table 5. Risk factors, adjusted hazard ratios (HR), and 95% confidence intervals (CI) for reoperation due to periprosthetic femoral fracture
Overall, women more frequently sustained fractures distally to the stem, whereas men had a higher risk for fracture around the stem, and a slightly higher risk for PPFF in general (type B or C). The risk for fracture increased with age, irrespective of whether age was studied as a continuous or a categorical variable. Patients aged 80 years and older had the highest risk for both type B and C fractures, compared with patients younger than 64 years ().
Inflammatory arthritis, when compared with primary OA, did not affect the risk for fracture around a stem, but distal to it. Patients with hip fracture or idiopathic femoral necrosis had approximately 3 times higher risk for type B fractures, and 4 times for type C (). The later the year for the index operation, the more likely the patient would suffer a type B fracture. No corresponding time-related change in risk was observed as regards type C fractures. The subgroup analysis (lateral versus posterior approach) was done in 43,271 Lubinus SPII stems and 21,562 Exeter Polished stems, inserted due to primary OA (). 1,077 stems operated with other surgical approaches were excluded from this analysis. Stems inserted with the posterior approach had a 1.6-times higher risk for suffering a Vancouver type B fracture compared with those inserted with a lateral approach ().
Table 7. Risk factors, adjusted hazard ratios (HR), and 95% confidence intervals (CI) for reoperation due to Vancouver type B fracture
Discussion
Several previous studies have demonstrated an increased risk for periprosthetic fracture of the Exeter when compared with the Lubinus stem (Lindahl et al. Citation2005, Thien et al. Citation2014). To our knowledge, this is the first study that distinguished between Vancouver type B and type C fractures, based on extensive research to include all reoperations. Earlier studies have either looked at the overall risk for periprosthetic fracture (Lindahl et al. Citation2005, Palan et al. Citation2016), or the risk for revision due to fracture (Cook et al. Citation2008, Thien et al. Citation2014) (mainly Vancouver type B2 and type B3 fractures), for one or both of these stems. Our main finding is that the Lubinus SPII did not have a higher risk for type C fractures, despite the fact that almost 3 out of 4 fractures around this stem were located distal to it (see ). The finding that the Exeter Polished stem had a higher risk for fracture (type B and overall), confirms earlier publications (Lindahl et al. Citation2005, Thien et al. Citation2014). The commonest fracture type in this material was, however, type C (see ). This observation results from an almost complete registration of fractures treated with osteosynthesis only, and without any stem revision (Chatziagorou et al. Citation2018). In Sweden, type B fractures are more common in uncemented stems, and type C fractures in cemented stems (Chatziagorou et al. Citation2018), in contrast to a previous study from the Mayo Clinic (Abdel et al. Citation2016).
The cemented Lubinus SPII stem (Waldemar Link, Hamburg, Germany) is a shape-closed, CoCrMo, tapered, and anatomically s-shaped stem, with a collar, a matte finish, and a 19° built-in anteversion of the femoral neck. Its shape allows neutral positioning in the femoral canal and resists rotational forces (Sesselmann et al. Citation2017), while the collar is claimed to restrict the distal migration of the stem (Catani et al. Citation2005). The anatomical shape of this stem probably facilitates an adequate cement mantle (Broden et al. Citation2015). The cemented Exeter stem (Stryker Howmedica, Mahwah, NJ, US) is a force-closed, straight, collarless, double-wedge tapered, highly polished stem. It does not bond to the cement and is designed to subside into the cement mantle as a wedge (Palan et al. Citation2016). Both stems are well documented with excellent outcomes in the short and long term (Murray et al. Citation2013, Prins et al. Citation2014, Sesselmann et al. Citation2017, Westerman et al. Citation2018). It is postulated that the subsidence of the Exeter stem into the cement mantle will create an axial loading effect within the cement mantle, resulting in hoop stresses in the adjacent bone, which might increase the risk of sustaining a PPFF. As soon as a periprosthetic fracture occurs close to an Exeter stem, the stem is by definition loose (Broden et al. Citation2015). The reason why force-closed cemented stems have a higher risk for periprosthetic fractures has been reported previously (Broden et al. Citation2015, Palan et al. Citation2016). The higher percentage of type C fractures within Lubinus SPII stems possibly has to do with the relative lower risk for fractures close to it (type B). We assume that these fractures are, rather, secondary to an osteoporotic femur (elderly, women, inflammatory arthritis, and previous history of hip fracture), than secondary to the stem’s design.
Previous comparisons between the posterior and the lateral approach showed superior results for the former regarding the thickness of the cement mantle (Hank et al. Citation2010), the alignment of the stem (Vaughan et al. Citation2007, Broden et al. Citation2015), and revision risk due to aseptic loosening of the stem (Lindgren et al. Citation2012). Femurs with a loose stem are more prone to suffer a periprosthetic fracture (Lindahl et al. Citation2005). Thus, the posterior surgical approach should be beneficial regarding the risk for aseptic loosening and, hence, the risk for type B fractures around a loose stem. We are not aware of any publication where the surgical approach is studied as a risk factor for postoperative periprosthetic femoral fractures, secondary to a primary cemented THR. Berend et al. (Citation2006) found that an anterolateral approach was associated with intraoperative fracture of the proximal femur, in both cemented and uncemented stems. A more recent study showed that patients older than 85 years, with hemiarthroplasty, had 2 times higher risk for postoperative PPFF if operated with a posterior approach, compared with those operated via a direct lateral approach (Rogmark et al. Citation2014), but this observation might have been confounded by inclusion of both cemented and uncemented stems of various designs.
Our finding, that use of a posterior approach is associated with a higher risk for PPFF, is difficult to explain. A radiostereometric study (Glyn-Jones et al. Citation2006) observed slightly increased retrotorsion of the Exeter stem if inserted through a posterior compared with an anterolateral approach, suggesting a less secure stem fixation in the former group. Gore et al. (Citation1982) showed less prosthetic femoral anteversion and more inward rotation of the operated hip with the posterior approach. A Cochrane review (Jolles and Bogoch Citation2006) also reported increased internal rotation of the hip joint in extension with use of the posterior approach, suggesting that implant loading might differ depending on the approach used.
The influence of potential risk factors for PPFF such as age, sex, and diagnosis at the time of primary THR vary depending on the type of the stem (cemented/uncemented, primary/secondary), the outcome measure (revision, reoperation, nonoperative treatment), and whether the fracture is intra- or postoperative (Berend et al. Citation2006, Cook et al. Citation2008, Meek et al. Citation2011, Abdel et al. Citation2016). We studied risk factors in patients with cemented Lubinus or Exeter stems and only those suffering a postoperative PPFF on the same side, and without any history of previous reoperation. Therefore, a generalization of our results for the whole population of patients with THR would be unreliable. High age, as well as the diagnosis of hip fracture or idiopathic femoral head necrosis, implied an increased risk for both type B and C fracture. Men had a higher risk for type B fractures, probably because of younger age with increased daily activity level (Witte et al. Citation2009) and higher risk for aseptic loosening than women (Hailer et al. Citation2010). Conversely, women, with more osteoporotic femoral bone and higher mean age at the time of primary THR, more frequently suffered type C fractures.
The year of index operation influenced the risk for type B and not for type C fractures. This is probably the result of the increasing mean age at the index operation during the study period, from 71 years in 2001 to 72 years in 2009. Another reason could, theoretically, be a trend toward a decrease in postoperative clinical and radiological controls after primary THR. This could lead to more cases with “unknown stem loosening,” and thus an increased risk for Vancouver type B fractures. The addition of the surgical approach in the subgroup analysis did not alter the relation of the other risk factors (age, sex, stem type, and year of primary THR). Inflammatory arthritis did not have a higher risk for fractures around the stem when compared with primary OA. This finding is in line with a previous report (Thien et al. Citation2014). On the other hand, femurs with inflammatory arthritis run a 6-times higher risk for distal femoral fractures. This is in accordance with a previous publication that reported a higher risk for osteoporotic fractures (Yamamoto et al. Citation2015) in patients with rheumatoid arthritis.
There are limitations to our study. The linkage between the SHAR and the NPR included only reoperations due to periprosthetic fracture and not all other reasons for reoperation (aseptic loosening, infection, dislocation, other). These reoperations are recorded in the SHAR, but could be underreported, especially those performed owing to infection (Lindgren et al. Citation2014). Therefore, the real number of all reoperations could be slightly higher than found by us. Reoperations that took place before the PPFF were detected when the case records were scrutinized. All other reoperations not reported to the SHAR could most probably be expected to be equally distributed between the 2 groups studied. Another limitation, however, is that we did not include the presence of a total knee replacement (TKR) as a risk factor. Total hip replacements with an ipsilateral TKR have a higher risk for proximal femoral fracture (Katz et al. Citation2014), and total knee replacement is associated with distal femoral fracture (McGraw and Kumar Citation2010). We do not, however, think that the relative number of patients with TKR differs between those who have been operated with a Lubinus and those who have received an Exeter stem. Hips with primary osteoarthritis and inflammatory arthritis had almost the same share in the 2 groups. It is also important to underline that the classification process was based on reading of medical records. A better optimized way would be to define the fracture type based on information from both the medical records and the radiographs. In a previous validation of the classification process (Chatziagorou et al. Citation2018) we did, however, observe good agreement corresponding to previous validations of the Vancouver classification (Brady et al. Citation2000, Rayan et al. Citation2008). In addition, our analysis was based only on fractures classified as either B or C, without any further analyses of the sub-categories in the type B group.
The methodological strength of this study was the relatively good data quality of a large volume of material, and its high external validity regarding PPFFs in the Swedish population. The hip prostheses studied in our report have a long tradition in Sweden with excellent implant survival (Junnila et al. Citation2016). The volume of our data was big enough to analyze only stems of the same length (150 mm). A difference in stem length can potentially affect the risk of periprosthetic fracture and its classification into type B or C. We also excluded uncemented cups, since use of such implants was shown to result in a higher rate of femoral lysis when used with Exeter V40 stems (Westerman et al. Citation2018). Furthermore, we investigated all kind of reoperations due to PPFF, and not only revisions, which is the contemporary standard in other arthroplasty registries. This, in addition to the cross-matching with the NPR, gave us the unique opportunity to study an almost complete data set of fractures treated surgically with other methods such as ORIF and without concomitant revision of the stem (mostly type B1 and C fractures).
Overall, the Exeter stem had almost an 3.5-times increased risk to suffer a periprosthetic fracture and about 10 times increased risk to suffer a PPFF leading to revision, which for the patient usually is a more demanding procedure than operation with osteosynthesis. According to our findings and previous studies the difference in risk ratio will increase further with increasing age and in patients with secondary OA. Lindahl et al. reported 23% reoperation rate (235 of 1,002) in patients treated surgically for type B and C fractures (Lindahl et al. Citation2005). We therefore think that our findings have clinical relevance and especially in the older population with a high incidence of osteoporosis.
In summary, the Exeter Polished stem had a higher risk for postoperative periprosthetic femoral fractures of type B compared with the Lubinus SPII. As regards type C fractures there was no difference. The relative increased proportion of type C versus type B fractures in the Lubinus group might indicate that, after the insertion of a Lubinus stem, the distal femur will constitute the weakest part as long as the stem has not loosened. Our study suggested that the posterior approach may not be beneficial regarding the risk of PPFF in cemented THRs, but this observation needs to be studied further.
GC: Planning of the research, collection of the material, analysis of the material, manuscript. HL: Planning of the research, collection of the material, manuscript. JK: Planning of the research, analysis of the material, manuscript.
Acta thanks Søren Overgaard for help with peer review of this study.
- Abdel M P, Watts C D, Houdek M T, Lewallen D G, Berry D J. Epidemiology of periprosthetic fracture of the femur in 32 644 primary total hip arthroplasties: a 40-year experience. Bone Joint J 2016; 98-b(4): 461–7.
- Berend M E, Smith A, Meding J B, Ritter M A, Lynch T, Davis K. Long-term outcome and risk factors of proximal femoral fracture in uncemented and cemented total hip arthroplasty in 2551 hips. J Arthroplasty 2006; 21(6 Suppl 2): 53–9.
- Brady O H, Garbuz D S, Masri B A, Duncan C P. Classification of the hip. Orthop Clin North Am 1999; 30(2): 215–20.
- Brady O H, Garbuz D S, Masri B A, Duncan C P. The reliability and validity of the Vancouver classification of femoral fractures after hip replacement. J Arthroplasty 2000; 15(1): 59–62.
- Broden C, Mukka S, Muren O, Eisler T, Boden H, Stark A, Skoldenberg O. High risk of early periprosthetic fractures after primary hip arthroplasty in elderly patients using a cemented, tapered, polished stem. Acta Orthop 2015; 86(2): 169–74.
- Catani F, Ensini A, Leardini A, Bragonzoni L, Toksvig-Larsen S, Giannini S. Migration of cemented stem and restrictor after total hip arthroplasty: a radiostereometry study of 25 patients with Lubinus SP II stem. J Arthroplasty 2005; 20(2): 244–9.
- Chatziagorou G, Lindahl H, Garellick G, Karrholm J. Incidence and demographics of 1751 surgically treated periprosthetic femoral fractures around a primary hip prosthesis. Hip Int 2018; Jul 1: [Epub ahead of print].
- Cook R E, Jenkins P J, Walmsley P J, Patton J T, Robinson C M. Risk factors for periprosthetic fractures of the hip: a survivorship analysis. Clin Orthop Relat Res 2008; 466(7): 1652–6.
- Glyn-Jones S, Alfaro-Adrian J, Murray D W, Gill H S. The influence of surgical approach on cemented stem stability: an RSA study. Clin Orthop Relat Res 2006; 448: 87–91.
- Gore D R, Murray M P, Sepic S B, Gardner G M. Anterolateral compared to posterior approach in total hip arthroplasty: differences in component positioning, hip strength, and hip motion. Clin Orthop Relat Res 1982; 165: 180–7.
- Hailer N P, Garellick G, Karrholm J. Uncemented and cemented primary total hip arthroplasty in the Swedish Hip Arthroplasty Register. Acta Orthop 2010; 81(1): 34–41.
- Hank C, Schneider M, Achary C S, Smith L, Breusch S J. Anatomic stem design reduces risk of thin cement mantles in primary hip replacement. Arch Orthop Trauma Surg 2010; 130(1): 17–22.
- Jolles B M, Bogoch E R. Posterior versus lateral surgical approach for total hip arthroplasty in adults with osteoarthritis. Cochrane Database Syst Rev 2006; (3): Cd003828.
- Junnila M, Laaksonen I, Eskelinen A, Pulkkinen P, Havelin L I, Furnes O, Fenstad A M, Pedersen A B, Overgaard S, Karrholm J, Garellick G, Malchau H, Makela K T. Implant survival of the most common cemented total hip devices from the Nordic Arthroplasty Register Association database. Acta Orthop 2016; 87(6): 546–53.
- Katz J N, Wright E A, Polaris J J, Harris M B, Losina E. Prevalence and risk factors for periprosthetic fracture in older recipients of total hip replacement: a cohort study. BMC Musculoskelet Disord 2014; 15: 168.
- Karrholm J, Lindahl H, Malchau H, Mohaddes M, Nemes S, Rogmark C, Rolfson O. The Swedish Hip Arthroplasty Register 2017. Annual Report 2016.
- Lindahl H, Malchau H, Herberts P, Garellick G. Periprosthetic femoral fractures: classification and demographics of 1049 periprosthetic femoral fractures from the Swedish National Hip Arthroplasty Register. J Arthroplasty 2005; 20(7): 857–65.
- Lindgren V, Garellick G, Karrholm J, Wretenberg P. The type of surgical approach influences the risk of revision in total hip arthroplasty: a study from the Swedish Hip Arthroplasty Register of 90,662 total hip replacements with 3 different cemented prostheses. Acta Orthop 2012; 83(6): 559–65.
- Lindgren J V, Gordon M, Wretenberg P, Karrholm J, Garellick G. Validation of reoperations due to infection in the Swedish Hip Arthroplasty Register. BMC Musculoskelet Disord 2014; 15: 384.
- Lowenhielm G, Hansson L I, Karrholm J. Fracture of the lower extremity after total hip replacement. Arch Orthop Trauma Surg 1989; 108(3): 141–3.
- McGraw P, Kumar A. Periprosthetic fractures of the femur after total knee arthroplasty. J Orthop Traumatol 2010; 11(3): 135–41.
- Meek R M, Norwood T, Smith R, Brenkel I J, Howie CR. The risk of peri-prosthetic fracture after primary and revision total hip and knee replacement. J Bone Joint Surg Br 2011; 93(1): 96–101.
- Murray D W, Gulati A, Gill H S. Ten-year RSA-measured migration of the Exeter femoral stem. Bone Joint J 2013; 95-B(5): 605–8.
- Palan J, Smith M C, Gregg P, Mellon S, Kulkarni A, Tucker K, Blom A W, Murray D W, Pandit H. The influence of cemented femoral stem choice on the incidence of revision for periprosthetic fracture after primary total hip arthroplasty: an analysis of national joint registry data. Bone Joint J 2016; 98-B(10): 1347–54.
- Prins W, Meijer R, Kollen B J, Verheyen C C, Ettema H B. Excellent results with the cemented Lubinus SP II 130-mm femoral stem at 10 years of follow-up: 932 hips followed for 5–15 years. Acta Orthop 2014; 85(3): 276–9.
- Ranstam J, Karrholm J, Pulkkinen P, Makela K, Espehaug B, Pedersen A B, Mehnert F, Furnes O. Statistical analysis of arthroplasty data, II: Guidelines. Acta Orthop 2011; 82(3): 258–67.
- Rayan F, Dodd M, Haddad F S. European validation of the Vancouver classification of periprosthetic proximal femoral fractures. J Bone Joint Surg Br 2008; 90(12): 1576–9.
- Rogmark C, Fenstad A M, Leonardsson O, Engesaeter L B, Karrholm J, Furnes O, Garellick G, Gjertsen J E. Posterior approach and uncemented stems increases the risk of reoperation after hemiarthroplasties in elderly hip fracture patients. Acta Orthop 2014; 85(1): 18–25.
- Sesselmann S, Hong Y, Schlemmer F, Wiendieck K, Soder S, Hussnaetter I, Muller L A, Forst R, Wierer T. Migration measurement of the cemented Lubinus SP II hip stem: a 10-year follow-up using radiostereometric analysis. Biomed Tech (Berl) 2017; 62(3): 271–8.
- Söderman P, Malchau H, Herberts P, Johnell O. Are the findings in the Swedish National Total Hip Arthroplasty Register valid? J Arthroplasty 2000; 15(7): 884–9.
- Thien T M, Chatziagorou G, Garellick G, Furnes O, Havelin L I, Makela K, Overgaard S, Pedersen A, Eskelinen A, Pulkkinen P, Karrholm J. Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the Nordic Arthroplasty Register Association database. J Bone Joint Surg Am 2014; 96(19): e167.
- Vaughan P D, Singh P J, Teare R, Kucheria R, Singer G C. Femoral stem tip orientation and surgical approach in total hip arthroplasty. Hip Int 2007; 17(4): 212–17.
- Westerman R W, Whitehouse S L, Hubble M J W, Timperley A J, Howell J R, Wilson M J. The Exeter V40 cemented femoral component at a minimum 10-year follow-up. Bone Joint J 2018; 100-b(8): 1002–9.
- Witte D, Klimm M, Parsch D, Clarius M, Breusch S, Aldinger P R. Ten-year survival of the cemented MS-30 femoral stem: increased revision rate in male patients. Acta Orthop Belg 2009; 75(6): 767–75.
- Yamamoto Y, Turkiewicz A, Wingstrand H, Englund M. Fragility fractures in patients with rheumatoid arthritis and osteoarthritis compared with the general population. J Rheumatol 2015; 42(11): 2055–8.
