Abstract
Background and purpose — Collaborations between arthroplasty registries are important in order to create the possibility of detecting inferior implants early and improve our understanding of differences between nations in terms of indications and outcomes. In this registry study we compared patient and procedure characteristics, and revision rates in the Nordic Arthroplasty Register Association (NARA) database and the Dutch Arthroplasty Register (LROI).
Patients and methods — All total hip arthroplasties (THAs) performed in 2010–2016 were included from the LROI (n = 184,862) and the NARA database (n = 290,823), which contains data from Denmark, Norway, Sweden, and Finland. Descriptive statistics and Kaplan–Meier survival analyses based on all reasons for revision and stratified by fixation were performed and compared between countries.
Results — In the Netherlands, the proportion of patients aged < 55 years (9%) and male patients (34%) was lower than in Nordic countries (< 55 years 11–13%; males 35–43%); the proportion of osteoarthritis (OA) (87%) was higher compared with Sweden (81%), Norway (77%), and Denmark (81%) but comparable to Finland (86%). Uncemented fixation was used in 62% of patients in the Netherlands, in 70% of patients in Denmark and Finland, and in 28% and 19% in Norway and Sweden, respectively. The 5-year revision rate for THAs for OA was lower in Sweden (2.3%, 95% CI 2.1–2.5) than in the Netherlands (3.0%, CI 2.9–3.1), Norway (3.8%, CI 3.6–4.0), Denmark (4.6%, CI 4.4–4.8), and Finland (4.4%, CI 4.3–4.5). Revision rates in Denmark, Norway, and Finland were higher for all fixation groups.
Interpretation — Patient and THA procedure characteristics as well as revision rates evinced some differences between the Netherlands and the Nordic countries. The Netherlands compared best with Denmark in terms of patient and procedure characteristics, but resembled Sweden more in terms of short-term revision risk. Combining data from registries like LROI and the NARA collaboration is feasible and might possibly enable tracking of potential outlier implants.
Arthroplasty registries are used to evaluate patient, procedure, prosthesis, and hospital characteristics associated with revision surgery as well as to improve quality of care (Herberts and Malchau Citation2000, Graves Citation2010). Comparison of national arthroplasty registries is important to improve our understanding of national differences and similarities. Furthermore, combining data from arthroplasty registries from several countries is needed in order to increase numbers to create the possibility of detecting inferior implants as early as possible.
The Nordic Arthroplasty Register Association (NARA) was established in 2007 by representatives from arthroplasty registries in Sweden, Norway, and Denmark to improve the quality of total hip and total knee arthroplasty through a registries-based research collaboration. Finland joined the association in 2010. To date, NARA is the most developed multinational arthroplasty database worldwide (Mäkelä et al. Citation2019). The comparison of national demographics and results was one of the main initial aims of the NARA collaboration. Therefore, the NARA database contains only parameters that are included in all the individual registries (Havelin et al. Citation2011).
The first NARA publication in 2009 described the results of 280,201 total hip arthroplasties (THAs) performed in 1995–2006 in Sweden, Norway, and Denmark (Havelin et al. Citation2009). This research was updated in 2014 by Mäkelä et al. using NARA data from 1995–2011 including Finland (Mäkelä et al. Citation2014). Substantial differences were found in the patient populations receiving a THA in the Nordic countries and in the procedure characteristics such as surgical approach and fixation (Mäkelä et al. Citation2014). Furthermore, substantial differences in 10-year survival rates were found between the Nordic countries (Havelin et al. Citation2009). The Dutch Arthroplasty Register (LROI) contains data on THAs since 2007. We initiated this study to compare patient and treatment characteristics as well as survival rates between THAs in the Netherlands and Nordic countries.
Patients and methods
The NARA database consists of pooled data from the national hip arthroplasty registries of Denmark, Norway, Finland, and Sweden. Each register has validation routines based on national patient registries. A minimal NARA dataset was created that contains data that all registries could deliver, where personal identification numbers are deleted. The data were treated with full confidentiality, and identification of individual patients was not possible as a result of the anonymization of the NARA dataset (Havelin et al. Citation2009, Citation2011).
The degree of coverage and completeness of the Nordic registries is documented to be higher than 95% (DHAR, FAR, NAR, SHAR n.d.). Selection and transformation of the respective datasets and de-identification of the patients, including deletion of the national personal identity numbers, was performed within each national registry. Anonymous data was then merged into a common research database. Ethical approval of the study was obtained through each national registry.
The LROI is the nationwide population-based register that includes information on arthroplasties in the Netherlands since 2007. The LROI has coverage of 100% of Dutch hospitals and completeness of reporting of over 95% for primary THAs and 88% for revision arthroplasties (LROI n.d., van Steenbergen et al. Citation2015). The LROI database contains information on patient, procedure, and prosthesis characteristics recorded by registrars from each hospital. The LROI uses the opt-out system to require informed consent of patients.
For the present study we included all primary THAs in the period 2010–2016 registered in the NARA (n = 290,823) and the LROI (n = 184,862). Bilateral procedures were included in the study, since they do not introduce significant dependency problems in register studies (Ranstam et al. Citation2011). Resurfacing hip arthroplasties were excluded, though metal-on-metal total hip arthroplasties were included. Records with missing data were included.
Age was categorized into 4 groups (< 55, 55–64, 65–74, ≥ 75). The categories for diagnosis differed slightly between NARA and the LROI. We harmonized LROI variables to the NARA minimal dataset of variables, with the main harmonization for childhood diseases being developmental dysplasia of the hip, Perthes disease, and slipped capital femoral epiphysis and a combination of the latter two diagnoses in the NARA dataset compared with post-Perthes and dysplasia in the LROI (). Furthermore, surgical approach was divided into posterior and non-posterior.
Table 1. Harmonization of LROI variables to the NARA minimal dataset for diagnosis
Cause of revision was harmonized between the NARA and the LROI. In the LROI more than one cause of revision could be registered, which is not in line with the NARA where the main reason for revision is registered. Therefore, a hierarchical order of reasons for revision (similar to the order used on the Norwegian data: top to bottom; infection, aseptic loosening, periprosthetic fracture, dislocation, other, missing) was used for the LROI data. Loosening of the acetabular and femoral component without infection as available in the LROI were combined as aseptic loosening (). In the LROI for 211 records (11%) more than one reason for revision was registered within 1 year of follow-up and 296 (8%) within the entire study period. The study is reported according to the STROBE guidelines.
Table 2. Harmonization of LROI variables to the NARA minimal dataset for cause of revision
Statistics
Descriptive statistics of patient and procedure characteristics as well as THA incidence per year based on the population per country was calculated, according to country. Survival time was calculated as the time from primary procedure to first all-cause, any component revision, death of the patient, or end of the follow-up (January 1, 2017). Median follow-up was 3 years (interquartile range: 1.4–4.8 years). Kaplan–Meier survival analyses were performed to evaluate time to all-cause any component revision including 95% confidence intervals (CI) according to countries for OA THA patients. Stratified analyses were performed according to fixation and sex. Reasons for revision within 1 year and within 5 years’ follow-up time were described per country. For the 95% CIs, we assumed that the number of observed cases followed a Poisson distribution.
Ethics, registration, funding and potential conflicts of interests
The dataset was processed in compliance with the regulations of the LROI and NARA governing research on registry data. No external funding was received. No competing interests were declared.
Results
475,685 THAs were included in the NARA and LROI databases in the study period, with 39% of procedures from the Netherlands, 24% from Sweden, and around 12% each from Denmark, Norway, and Finland (). The volume of primary THAs increased each year in all 5 countries during the study period. The 2016 incidence rates of new THAs were around 170–175 per 100,000 inhabitants in NARA countries, and 150 in the Netherlands ().
Table 3. Primary total hip arthroplasty volume per country
Patient characteristics
In the Netherlands, the proportion of patients aged < 55 years was 9%, which was lower than that in the Nordic countries; in Finland 13% of THA patients were aged < 55 years. The proportion of patients aged ≥ 75 years was comparable between the Netherlands, Denmark, and Sweden with 31–32% each, while this proportion was lower in Finland and Norway (28–29%). The proportion of male patients was lowest in the Netherlands at 34% compared with any of the Nordic countries (35–43%). The proportion of THAs due to primary osteoarthritis (OA) was higher in the Netherlands (87%) than in Sweden, Norway, and Denmark, but comparable to Finland. The proportion of hip fractures was lower in the Netherlands compared with Denmark, Sweden, and to a lesser extent Norway. The proportion of inflammatory arthritis differed between the countries, from 0.9% in the Netherlands up to 2.5% in Finland. In Denmark and Sweden hip fracture as diagnosis for THA was almost twice as frequent as in the Netherlands and almost 3 times more frequent than in Finland ().
Table 4. Characteristics of the total hip arthroplasty patients and procedures registered in the NARA and LROI database, 2010–2016 (n = 475,685). Values are percentages unless otherwise specified
Procedure characteristics
Uncemented fixation of both components was used in 62% of patients in the Netherlands, in 70% of patients in Denmark and Finland, and in 28% and 19% in Norway and Sweden, respectively.
In the Netherlands, a posterior hip approach was used in 61% of the THA procedures, which was in between Sweden (52%) and Finland (67%), but lower than in Denmark (96%) and higher compared with Norway (40%) ().
Table 5. Procedure characteristics of the total hip arthroplasty patients and procedures registered in the NARA and LROI database, 2010–2016 (n = 475,685). Values are percentages unless otherwise specified
Revision
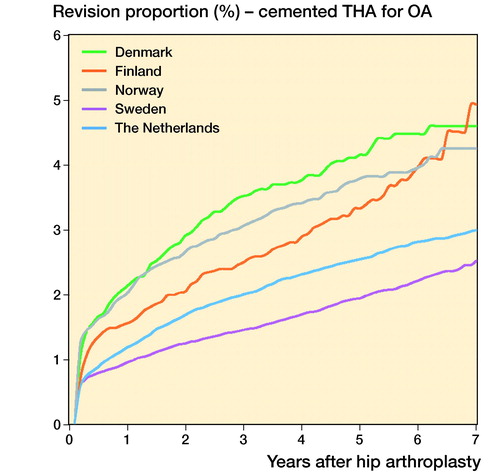
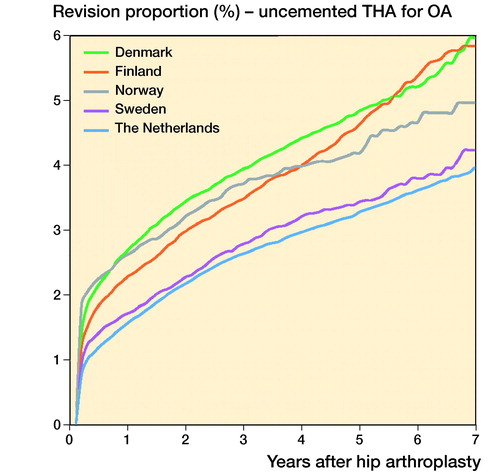
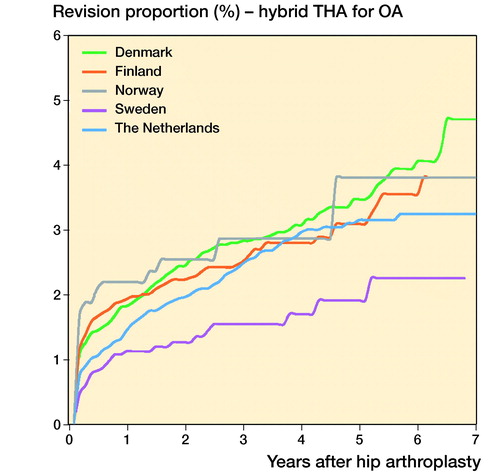
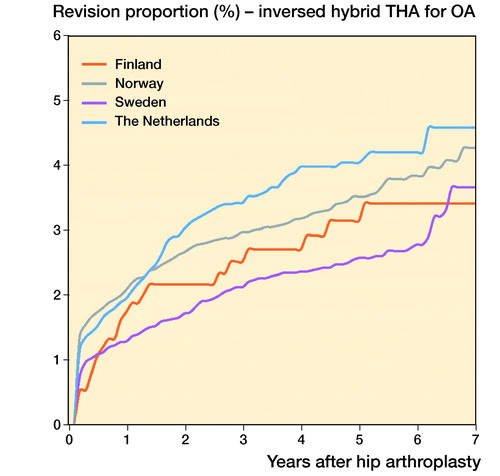
In THAs for primary OA the 1-, 3-, and 5-year overall revision rates were lowest in Sweden. The Netherlands had a higher revision rate (5-year revision rate: 3.0%, CI 2.9–3.1) compared with Sweden (2.3%, CI 2.1–2.5), but a lower revision rate compared with Denmark (4.6%, CI 4.4–4.8), Norway (3.8%, CI 3.6–4.0), and Finland (4.4%, CI 4.3–4.5) (, ). Stratified analyses showed lower revision rates for cemented THAs in Sweden and the Netherlands compared with Denmark, Norway, and Finland. Uncemented THAs had lower 3- and 5-year revision rates in the Netherlands and Sweden than in Norway, Denmark, and Finland. Hybrid (femur cemented) and reverse hybrid (cup cemented) THAs had lowest short-term revision rates in Sweden (, ). However, the number of cases with reverse hybrid THAs was small in Finland and too small in Denmark for meaningful analyses. Therefore the reverse hybrid cases from Denmark were excluded. Stratified analyses by sex showed comparable results for short-term overall revision rates examining differences between countries. Short-term overall revision rates were somewhat higher for males compared with females in all countries (data not shown). Analyses of the whole study population including cases with non-OA diagnoses gave the same results (data not shown).
Figure 1. Cumulative revision proportion (%) of THAs for OA according to country, all fixation methods.
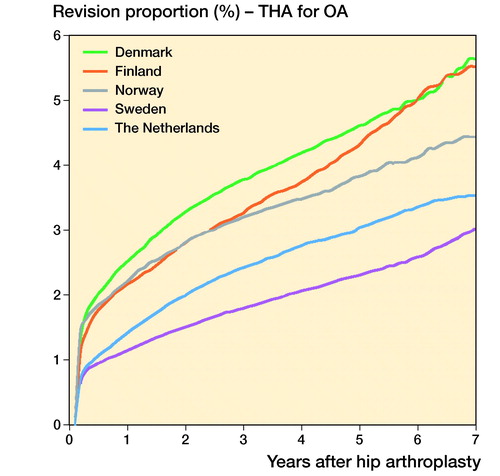
Figure 2. Cumulative revision proportion (%) of cemented THAs (a), uncemented THAs (b), hybrid THAs (c), and inverse hybrid THAs (d) for OA according to country.
Table 6. Kaplan–Meier revision rates (%) with 95% confidence intervals at 1, 3, and 5 years after primary total hip arthroplasties for osteoarthritis
Reason for revision
The most frequent reason for revision in the first year after primary THA differed between countries; dislocation was the most frequently registered reason for revision within the first year for Denmark and the Netherlands. For Norway, Sweden, and Finland deep infection was the most frequent reason for revision (). After up to 5 years of follow-up, dislocation and infection were the most common reasons for revision in the Nordic countries, while aseptic loosening was the most frequently registered reason for revision within 5 years of follow-up in the Netherlands.
Table 7. Reasons for revision (%) within 1 year and up to 5-year follow-up of total hip arthroplasties for osteoarthritis registered in the NARA and LROI database
Discussion
This study provides the first comparison between the NARA countries (Denmark, Finland, Norway, and Sweden) and the Netherlands for primary THA procedures. Combining data from different national arthroplasty registries like NARA and LROI is possible for patient and procedure characteristics as well as for revision rates and reasons for revision. When combining datasets some requirements are necessary such as harmonizing categories of diagnosis and reasons for revision.
Patient and procedure characteristics
Our findings concerning patient and procedure characteristics of the NARA countries are in line with previously reported results. However, the proportion of male patients is somewhat higher in all NARA countries, especially in Norway compared with earlier NARA results (Mäkelä et al. Citation2014). Dutch patients who received a THA were generally somewhat older than THA patients in NARA countries, with Finland having a known younger THA population (Mäkelä et al. Citation2014). Furthermore, the proportion of OA as the diagnosis for primary THA was higher in the Netherlands compared with the Nordic countries, whereas the proportion of hip fractures was lower in the Netherlands compared with Denmark, Norway, and Sweden. This might be the result of the varying indications for use of THA for fracture patients in the Nordic countries and the Netherlands. The incidence of THA is in line with reported international THA incidence rates (Merx et al. Citation2003, Paxton et al. Citation2019), but seems to be somewhat lower in the Netherlands compared with the Nordic countries. This may reflect differences in demography, prevalence of various hip diseases, indications for surgical treatment, and/or healthcare policy between countries.
Apart from the differences in patient population, procedure characteristics also differed between the Netherlands and the Nordic countries. The Netherlands was most comparable to Denmark and Finland concerning THA fixation technique. These countries had a high proportion of uncemented fixation, while Norway and Sweden had a low proportion of uncemented fixation. Good results of cemented THA and inferior results of some uncemented THAs in the Swedish and Norwegian registries have encouraged the continued use of cemented THA in these countries (Havelin et al. Citation2009). However, uncemented fixation as well as reverse hybrid fixation increased in both Norway and Sweden during the study period.
Revision
There were differences in short-term revision rates between NARA countries and the Netherlands for all evaluated hip stem and acetabular fixation group combinations. Although differences were small, revision risk at short-term follow-up was lowest in Sweden for cemented THAs. The Swedish Hip Arthroplasty Register (SHAR) has provided feedback and advice to the orthopedic surgeons for over 40 years (SHAR n.d.). However, Dutch results showed comparable low short-term revision rates as well. The higher short-term revision rates for THAs in Denmark and Finland might be explained by more dislocations due to the posterior approach (Zijlstra et al. Citation2017), which is frequently used in these countries. However, the posterior approach has been shown to give better patient-reported outcomes (Amlie et al. Citation2014, Rosenlund et al. Citation2017).
Results of large femoral head metal-on-metal THAs have been poor (Seppanen et al. Citation2018), which may be an important factor in the explanation for the higher revision rates in uncemented THAs in Denmark and Finland where the proportion of these THAs was high. However, in the Netherlands these large femoral head metal-on metal THAs were also used in substantial numbers (LROI n.d.). Unfortunately we were not able to exclude these big head metal-on-metal cases from our analyses because we did not include femoral head size or articulating materials in this data set. Furthermore, patient characteristics are likely to play a role in the revision rates of THAs, with Finland having a younger patient population that might partly explain their higher short-term revision rate (FAR, LROI n.d.).
Reverse hybrid and hybrid THAs had the lowest short-term revision rates in Sweden, being lower than in the Netherlands. It has been stated previously based on NARA data, however, that reverse hybrid THA has a higher revision rate than cemented THA, mainly due to periprosthetic fractures (Wangen et al. Citation2017). The number of reverse THAs in the Nordic countries has decreased in recent years, after the period of the current study (2010–2016).
Cause of revision differed between countries, with dislocation being the most frequent reason for revision in the Netherlands and Denmark. This is probably related to a higher proportion of the THAs done with a posterior approach. Infection represents a major share of the short-term revisions, which might substantially influence the short-term revision rate. However, infection as a reason for revision should be considered carefully, since the capture rate in arthroplasty registries is known to be suboptimal, with up to 40% of revision procedures with proven infections missing (Gundtoft et al. Citation2015). This might be different between countries, which most likely biases the results. Validity of revision for infection largely depends on the possibility to validate registry data with other datasets from, e.g., microbiology. Currently, a study is being performed in the Netherlands to examine the proportion of revisions for infections not registered in the LROI, which is expected to be comparable to the study by Gundtoft et al. The proportion of unknown reasons for revision differed substantially between countries, which also might bias the short-term results.
Strengths and weaknesses
The strength of this study is the large population-based registry dataset from 5 countries with high-quality data and minimal loss to follow-up from each national register. Completeness of data in the included registries is documented to be higher than 95% (DHAR, FAR, LROI, NAR, SHAR n.d.). Furthermore, registries provide real-world data with high generalizability and external validity. This gives us the opportunity to describe trends and differences between countries. On the other hand, our registry data are observational and can be subject to bias that we cannot account for, i.e., selection bias and confounding by indication by surgeon. Therefore, causality cannot be inferred. Data used for this project is limited by being common to all 5 registries, and hence we lack information on some factors that affect the outcomes. In this first study comparing LROI and NARA data we did not merge the datasets, hampering the possibility to perform adjusted analyses.
In this study we examined and compared NARA and LROI data from a relatively recent period, resulting in a limited follow-up of THA procedures with a maximum of 7 years. Furthermore, we did not include femoral head size or type of articulation, which are known factors influencing revision rates. Moreover, we were not able to exclude metal-on-metal THAs, which have a known high revision rate (Smith et al. Citation2012).
In addition, we evaluated overall revision, which contains a variety of revision procedures ranging from small revision procedures like femoral head exchange to major revision procedures such as complete exchange or extraction of all components. The type of revision procedure performed might differ between countries, resulting in differences in revision rates. Moreover, the threshold for performing revision procedures may vary between countries, which influences revision rates.
Demographics of the Nordic countries and the Netherlands are comparable, although there are substantial differences in travel distance to the nearest (revision) hospital between the Netherlands and, e.g., the rural areas of the Nordic countries. Furthermore, the Nordic countries as well as the Netherlands have a solid healthcare system. However, while the health expenditure of the Nordic countries is mainly paid by the government, the health expenditure of the Netherlands is mainly covered by compulsory health insurance (OECD n.d., OECD Citation2019).
Conclusion
Patient and THA procedure characteristics as well as revision rates evinced some differences between the Netherlands and the Nordic countries, although the magnitude of differences was small. The Netherlands seemed to compare best to Denmark in terms of patient and procedure characteristics, but was most comparable to Sweden in terms of short-term revision risk for both cemented and uncemented THAs. The observed absolute differences in revision risk were small and might not be clinically relevant, since they most likely are a reflection of variations in demographics, patient selection, procedure characteristics, or indications for revision. However, most of these factors cannot be studied based on the common data available. Combining data from registries like LROI and those included in the NARA collaboration is feasible. This might possibly enable tracking of potential outlier implants, specific patient groups, or events with a relatively low occurrence. Further research is warranted to merge datasets and look at more details concerning THA, creating the opportunity to perform patient-, procedure-, and prosthesis-adjusted analyses.
All authors made a substantial contribution to the study. RN, BS, and LS contributed to the conception of the study. JK created the dataset with the NARA study group. LS conducted the statistical analyses and prepared the manuscript. KM, JK, OR, SO, OV, AP, AE, GH, BS, and RN participated in the data collection and revision of the manuscript.
The authors would like to thank the technical support team at the SHAR for their help.
- Amlie E , Havelin L I , Furnes O , Baste V , Nordsletten L , Hovik O , Dimmen S . Worse patient-reported outcome after lateral approach than after anterior and posterolateral approach in primary hip arthroplasty: a cross-sectional questionnaire study of 1,476 patients 1–3 years after surgery. Acta Orthop 2014; 85(5): 463–9.
- DHAR . www.dhr.dk.
- FAR . www.thl.fi/far.
- Graves S E . The value of arthroplasty registry data. Acta Orthop 2010; 81(1): 8–9.
- Gundtoft P H , Overgaard S , Schonheyder H C , Moller J K , Kjaersgaard-Andersen P , Pedersen A B . The “true” incidence of surgically treated deep prosthetic joint infection after 32,896 primary total hip arthroplasties: a prospective cohort study. Acta Orthop 2015; 86(3): 326–34.
- Havelin L I , Fenstad A M , Salomonsson R , Mehnert F , Furnes O , Overgaard S , Pedersen A B , Herberts P , Kärrholm J , Garellick G . The Nordic Arthroplasty Register Association: a unique collaboration between 3 national hip arthroplasty registries with 280,201 THRs. Acta Orthop 2009; 80(4): 393–401.
- Havelin L I , Robertsson O , Fenstad A M , Overgaard S , Garellick G , Furnes O . A Scandinavian experience of register collaboration: the Nordic Arthroplasty Register Association (NARA). J Bone Joint Surg Am 2011; 93(Suppl. 3): 13–19.
- Herberts P , Malchau H . Long-term registration has improved the quality of hip replacement: a review of the Swedish THR Register comparing 160,000 cases. Acta Orthop Scand 2000; 71(2): 111–21.
- LROI . www.lroi-report.nl.
- Mäkelä K T , Matilainen M , Pulkkinen P , Fenstad A M , Havelin L I , Engesaeter L , Furnes O , Overgaard S , Pedersen A B , Kärrholm J , Malchau H , Garellick G , Ranstam J , Eskelinen A . Countrywise results of total hip replacement: an analysis of 438,733 hips based on the Nordic Arthroplasty Register Association database. Acta Orthop 2014; 85(2): 107–16.
- Mäkelä K T , Furnes O , Hallan G , Fenstad A M , Rolfson O , Kärrholm J , Rogmark C , Pedersen A B , Robertsson O , A W D, Eskelinen A, Schroder H M, Aarimaa V, Rasmussen J V, Salomonsson B, Hole R, Overgaard S. The benefits of collaboration: the Nordic Arthroplasty Register Association. EFORT Open Rev 2019; 4(6): 391–400.
- Merx H , Dreinhofer K , Schrader P , Sturmer T , Puhl W , Gunther K P , Brenner H . International variation in hip replacement rates. Ann Rheum Dis 2003; 62(3): 222–6.
- NAR . http://nrlweb.ihelse.net/eng/Rapporter/Report2019_english.pdf.
- OECD . Health at a glance 2019, Paris: OECD; 2019.
- OECD . https://ec.europa.eu/health/sites/health/files/state/docs/chp_sv_english.pdf.
- Paxton E W , Cafri G , Nemes S , Lorimer M , Kärrholm J , Malchau H , Graves S E , Namba R S , Rolfson O . An international comparison of THA patients, implants, techniques, and survivorship in Sweden, Australia, and the United States. Acta Orthop 2019; 90(2): 148–52.
- Ranstam J , Kärrholm J , Pulkkinen P , Makela K , Espehaug B , Pedersen A B , Mehnert F , Furnes O , group Ns . Statistical analysis of arthroplasty data, I: Introduction and background. Acta Orthop 2011; 82(3): 253–7.
- Rosenlund S , Broeng L , Holsgaard-Larsen A , Jensen C , Overgaard S . Patient-reported outcome after total hip arthroplasty: comparison between lateral and posterior approach. Acta Orthop 2017; 88(3): 239–47.
- Seppanen M , Laaksonen I , Pulkkinen P , Eskelinen A , Puhto A P , Kettunen J , Leskinen J , Manninen M , Mäkelä K . High revision rate for large-head metal-on-metal THA at a mean of 7.1 years: a registry study. Clin Orthop Relat Res 2018; 476(6): 1223–30.
- SHAR . https://registercentrum.blob.core.windows.net/shpr/r/Arsrapport_2018 _Hoftprotes_ENG_26mars_Final-rJepCXNsLI.pdf.
- Smith A J , Dieppe P , Vernon K , Porter M , Blom A W , National Joint Registry of England and Wales. Failure rates of stemmed metal-on-metal hip replacements: analysis of data from the National Joint Registry of England and Wales. Lancet 2012; 379(9822): 1199–204.
- van Steenbergen L N , Denissen G A , Spooren A , van Rooden S M , van Oosterhout F J , Morrenhof J W , Nelissen R G . More than 95% completeness of reported procedures in the population-based Dutch Arthroplasty Register. Acta Orthop 2015; 86(4): 498–505.
- Wangen H , Havelin L I , Fenstad A M , Hallan G , Furnes O , Pedersen A B , Overgaard S , Kärrholm J , Garellick G , Mäkelä K , Eskelinen A , Nordsletten L . Reverse hybrid total hip arthroplasty. Acta Orthop 2017; 88(3): 248–54.
- Zijlstra W P , De Hartog B , Van Steenbergen L N , Scheurs B W , Nelissen R . Effect of femoral head size and surgical approach on risk of revision for dislocation after total hip arthroplasty. Acta Orthop 2017; 88(4): 395–401.