Antibiotics have been suggested as treatment for selected patients with chronic back pain, with or without leg pain, and in association with Modic changes type 1 (MC1) on MRI (Modic et al. Citation1988, Albert et al. Citation2013a).
The hypothesis is that various bacteria, but above all the common skin bacterium Cutibacterium acnes (formerly Propionibacterium acnes), would spread hematogenously to degenerated discs, where a “low-grade subclinical infection” would trigger an inflammatory reaction and cause MC1 (Albert et al. Citation2013a), irritate nociceptive nerve endings, and induce pain. Other studies have not found this connection, or have been cautious in their conclusions (Birkenmaier Citation2013, Urquhart et al. Citation2015) but have not had the same public impact.
Since back/leg pain is common, and Modic changes occur in people with or without back/leg pain (Wang et al. Citation2012), and as antibiotic resistance is a major health threat (Carlsson et al. Citation2019), the suggestion of treating chronic back/leg pain with antibiotics must be thoroughly investigated.
Research groups in Sweden, Denmark, and Norway have independently conducted studies from 3 different perspectives, but with a focus on the same basic questions: is there a causative link between Modic changes, back pain, and bacteria. The studies, all published during 2019, conclude that antibiotics should not be used for back/leg pain, unless there is a clinically relevant infection in the disc/vertebra (discitis/spondylitis).
Bacteria and discs, Fritzell et al. (Citation2019)
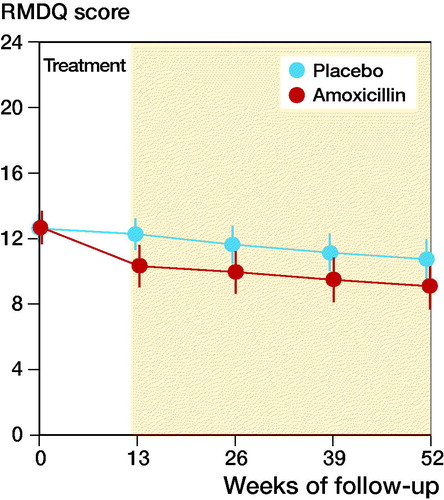
In this Swedish multicenter study, the presence of bacteria in discs/vertebrae was evaluated in 2 patient groups from 7 hospitals (). Samples from degenerated discs in 40 patients operated on for lumbar disc herniation (median age 43 years) were compared with samples from non-degenerated discs in young patients operated on for scoliosis, who did not have back pain or disc herniation (median age 17 years). The samples were analyzed using culture and DNA technology at 2 independent university laboratories in Gothenburg and Uppsala.
Figure 1. Data from Fritzell et al. Citation2019. LDH = lumbar disc herniation.
The study found no statistically significant difference in bacterial presence between the 2 groups. No association was seen between Modic changes and findings of bacteria or between back/leg pain and findings of bacteria or Modic changes.
Conclusion
Findings of bacteria, or traces of bacteria, as described in previous studies, are most likely a result of contamination during the surgical procedure.
Modic changes and back pain, Udby et al. (Citation2019)
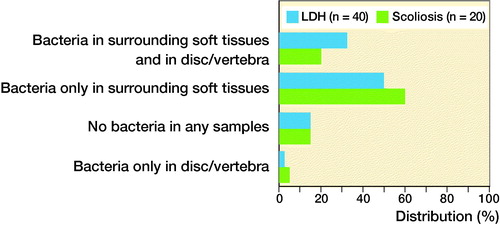
In Denmark, the clinical relevance of Modic changes for back pain and function was evaluated in a cohort study with a 13-year follow-up period (). In all, 204 patients were stratified to a group with or without Modic changes. The relationship between Modic changes at study start and impaired physical function, measured with the RMDQ (Roland Morris Disability Questionnaire, 0 = best, 23 = worst possible function) (Roland et al. 1983), back pain, and sick leave at follow-up was evaluated.
Figure 2. Data from Udby et al. Citation2019.
The study found no statistically significant differences in demographic data, BMI, smoking, back and leg pain at the start of the study, or at follow-up. Physical function measured with RMDQ was initially equal between the 2 groups, but statistically significantly better (without clinical relevance) at the follow-up in patients with Modic changes at the start of the study, 7.4 versus 9.6 (p = 0.02). Patients with Modic changes at the start of the study also had fewer sick days due to back pain during the study period, 9 versus 23.
Conclusion
Modic changes on MRI in patients with back pain at study start were not negatively associated with back pain or functional level after 13 years.
Antibiotics and back pain, Bråten et al. (2019)
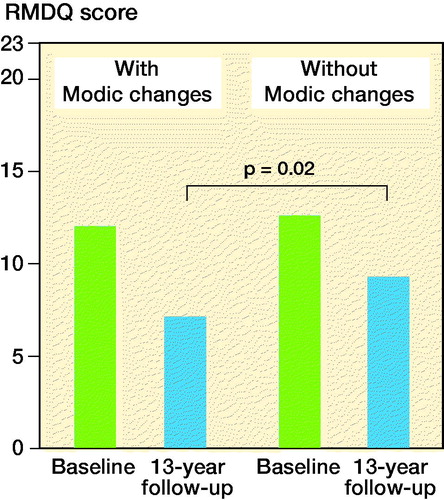
In Norway, the Danish study by Albert et al. (Citation2013b) was largely reproduced to evaluate the effect of antibiotic treatment in patients with chronic back pain (). The research group conducted a randomized placebo-controlled double-blind multicenter study at 6 hospitals (the Albert et al. study was a single-center study). The Norwegian study included 180 patients with back pain and Modic change type 1 or type 2. The participants were randomized to 3 months of treatment with either amoxicillin 3 × 750 mg or placebo, and follow-up was done according to “intention to treat” after 1 year. The outcome, measured with RMDQ, was similar in the 2 groups.
Conclusion
3 months of treatment with amoxicillin showed no relevant clinical effect after 1 year in patients with chronic back pain and Modic changes.
Summary
Based on current scientific evidence, where the 3 Nordic studies supply complementary findings, antibiotic treatment for back/leg pain with no signs of serious infection (discitis/spondylitis) cannot be recommended. It is important to counteract the development of antibiotic resistance in society due to antibiotic use without scientific evidence.
This article has also been published in the Swedish Läkartidningen; 2020; 117: 20067.
No author has any conflict of interest.
- Albert H B , Lambert P , Rollason J , Solgaard Sorensen J , Worthington T , Bach Pedersen M , Schack Nørgaard H , Vernallis A , Busch F , Manniche C , Elliott T. Does nuclear tissue infected with bacteria following disc herniations lead to Modic changes in the adjacent vertebrae? Eur Spine J 2013a; 22(4): 690–6.
- Albert H B , Sorensen J S , Schiott Christensen B , Manniche C. Antibiotic treatment in patients with chronic low back pain and vertebral bone oedema (Modic type 1 changes): a double-blind randomized clinical controlled trial of efficacy. Eur Spine J 2013b; 22(4): 697–707.
- Birkenmaier C. Should we start treating chronic low back pain with antibiotics rather than with pain medications? Korean J Pain 2013; 26(4): 327–35.
- Bråten L C H , Rolfsen M P , Espeland A , Wigemyr M , Aßmus J , Froholdt A , Haugen A J , Marchand G H , Kristoffersen P M , Lutro O , Randen S , Wilhelmsen M , Winsvold B S , Kadar T I , Holmgard T E , Vigeland M D , Vetti N , Nygaard Ø P , Lie B A , Hellum C , Anke A , Grotle M , Schistad E I , Skouen J S , Grøvle L , Brox J I , Zwart J A , Storheim K ; AIM study group. Efficacy of antibiotic treatment in patients with chronic low back pain and Modic changes (the AIM study): double blind, randomised, placebo controlled, multicentre trial. BMJ 2019; 367: 15654.
- Carlsson F , Jacobsson G , Jagers S C , Lampi E , Robertson F , Rönnerstrand B. Who is willing to stay sick for the collective? Individual characteristics, experience, and trust. Göteborg: Göteborgs universitet, institutionen för samhällsekonomi med statistik; 2019. SSM Popul Health 2019; 9: 100499.
- Fritzell P , Welinder-Olsson C , Jönsson B , Melhus Å , Andersson S G E , Bergström T , Tropp H , Gerdhem P , Hägg O , Laestande H , Knutsson B , Lundin A , Ekman P , Rydman E , Skorpil M. Bacteria: back pain, leg pain and Modic sign—a surgical multicentre comparative study. Eur Spine J 2019; 28(12): 2981–9.
- Modic M T , Steinberg P M , Ross J S , Masaryk T J , Carter J R. Degenerative disk disease: assessment of changes in vertebral body marrow with MR imaging. Radiology 1988; 166(1, Pt 1): 193–9.
- Roland M O , Morris R W. A study of the natural history of back pain. Part 1: Development of a reliable and sensitive measure of disability in low back pain. Spine (Phila Pa 1976) 1983; 8(2): 141–4.
- Udby P M , Bendix T , Ohrt-Nissen S , Lassen M R , Sørensen J S , Brorson S , Carreon L Y , Andersen M Ø. Modic changes are not associated with long-term pain and disability: a cohort study with 13-year follow-up. Spine (Phila Pa 1976) 2019; 44(17): 1186–92.
- Urquhart D M , Zheng Y , Cheng A C , Rosenfeld J V , Chan P , Liew S , Monira Hussain S , Cicuttini F M. Could low grade bacterial infection contribute to low back pain? A systematic review. BMC Med 2015; 13: 13.
- Wang Y , Videman T , Battié M C. Modic changes: prevalence, distribution patterns and association with age in white men. Spine J 2012; 12(5): 411–16.