Abstract
Background and purpose — The trochanteric stabilizing plate (TSP) may be used as an adjunct to a sliding hip screw (SHS) in the treatment of trochanteric fractures to increase construct stability. We performed a scoping review of the literature to clarify when and how the TSP may be useful.
Methods — A systematic search was performed in 5 databases and followed by a backwards-and-forwards citation search of the identified papers. 24 studies were included.
Results — 6 biomechanical studies and 18 clinical studies were included in the review. The studies presented mainly low-level evidence. All studies were on unstable trochanteric fractures or fracture models. Due to the heterogeneity of methods and reporting, we were not able to perform a meta-analysis. In the biomechanical trials, the TSP appeared to increase stability compared with SHS alone, up to a level comparable with intramedullary nails (IMNs). We identified 1,091 clinical cases in the literature where a TSP had been used. There were 82 (8%) reoperations. The rate of complications and reoperations for SHS plus TSP was similar to previous reports on SHS alone and IMN. It was not possible to conclude whether the TSP gave better clinical results, when compared with either SHS alone or with IMN.
Interpretation — The heterogeneity of methods and reporting precluded any clear recommendations on when to use the TSP, or if it should be used at all.
Internal fixation of trochanteric femoral fractures is usually performed with a plate or nail with a lag screw allowing axial compression to enhance fracture healing. The agreement between surgeons on implant choice is fair (Mellema et al. Citation2021). While a sliding hip screw (SHS) seems sufficient in stable trochanteric fractures (Parker and Handoll 2010), several guidelines recommend the use of intramedullary nails (IMNs) in more unstable fracture patterns (NICE Citation2011, Roberts and Brox Citation2015). Fixation without a lag screw is not recommended (Parker and Handoll 2010, Parker et al. Citation2018). Fractures involving the lateral wall, or with posteromedial comminution, are considered as unstable. This might cause excessive medialization of the femoral shaft, malunion, poor functional results, and even fixation failure (Parker Citation1996, Bretherton and Parker Citation2016). In addition, a thin lateral wall or a concomitant fracture through the greater trochanter increases the risk for an intra- or postoperative lateral wall fracture (Palm et al. Citation2007, Hsu et al. Citation2013). Under these circumstances, with a compromised lateral buttress, implant-preventing secondary displacement is required.
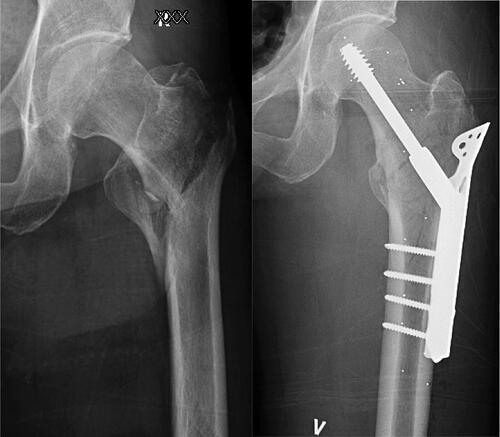
The trochanteric stabilizing plate (TSP) was introduced in the early 1990s as an adjunct to the sliding hip screw. The plate acts by buttressing the lateral trochanteric wall and is intended to prevent medialization of the femoral shaft (). Despite being sparsely discussed in the literature, an SHS with an additional TSP has been widely used in some countries and regions for decades (Lunsjö et al. Citation2001, Bong et al. Citation2004, Gupta et al. Citation2010, Knobe et al. Citation2013, Hsu et al. Citation2015, Alm et al. Citation2021). We reviewed the literature on TSP to clarify existing evidence and aid in the decision-making on when to use a TSP.
Figure 1. Pre- and postoperative images of a AO/OTA 31-A2 fracture operated on with a sliding hip screw with trochanteric stabilizing plate (TSP). The TSP should prevent excessive medialization of the femoral shaft by buttressing the lateral trochanteric wall. In this case, a loss of medial buttress with a large lesser trochanter fragment and a thin lateral wall would strengthen the traditional indication for a TSP.
Method
We applied the recommendations from the Cochrane collaboration (Higgins et al. Citation2020) and the methodological framework for scoping reviews as proposed by Arksey and O’Malley (Citation2005).
Research questions
What are the mechanical properties of the SHS plus TSP compared with SHS alone or intramedullary implants?
Does the TSP lead to an improved clinical outcome compared with SHS alone or IMN?
How does the TSP function in terms of non-union, mechanical failure, and reoperations?
Is it possible to establish guidelines for TSP use based on the existing evidence?
Eligibility criteria
All papers, both clinical and biomechanical, reporting outcomes related to TSP use in trochanteric fracture treatment were included in the review. We excluded studies reporting 3 cases or less, or where the TSP was used for indications other than acute trochanteric fractures.
Information sources
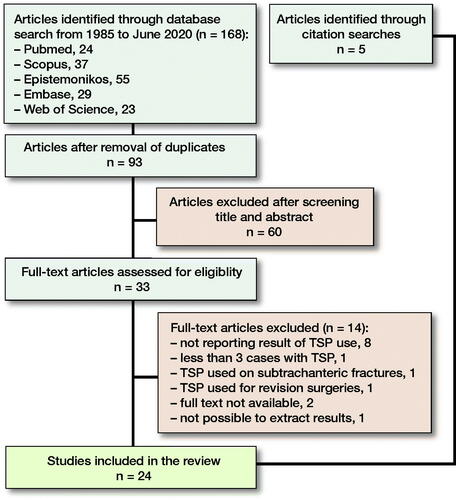
A systematic search through PubMed, Scopus, Web of Science, Embase, and Epistemonikos was performed and last updated on June 25, 2020 by the 1st author (CEA). The complete search strategy is shown in the legend to . In addition, we did a backwards search of all references of the papers identified and a forward search of papers citing the identified publications. We also manually searched the reference lists of review papers, meta-analyses, and guidelines until no new papers turned up.
Figure 2. Flow chart of papers in the review. The papers identified were from Norway, Sweden, Switzerland, Germany, Taiwan, India, United States, Canada, Northern Ireland, South Korea, and Egypt. Search strategy: Languages: All. Search terms/-strings: Title/Abstract (“trochanteric stabilising plate” OR “trochanteric stabilizing plate” OR “trochanteric stabilisation plate” OR “trochanteric stabilization plate” OR “lateral support plate” OR “trochanter stabilising plate” OR “trochanter stabilizing plate” OR “trochanter stabilization plate” OR “trochanter stabilisation plate”).
Study selection
Irrelevant studies were excluded based on title and abstract screening. Full text versions of the remaining studies were screened for eligibility by CEA and FF.
Funding and potential conflicts of interest
No funding was received. The authors declare no conflicts of interest.
Results
Study selection
After removal of duplicates, 93 unique papers were identified for further analysis (). Based on screening of title and/or abstract, 60 records were excluded, leaving 33 studies for full text evaluation. Of these 33 studies, 14 were excluded for various reasons (). The citation searches identified 5 additional papers (Babst et al. Citation1993, David et al. Citation1996, Friedl and Clausen Citation2001, Klinger et al. Citation2005, Bonnaire et al. Citation2007).
Summary of the literature
6 biomechanical studies (, see Supplementary data) and 18 clinical studies ( and , see Supplementary data) were identified. The clinical studies all reported surgical outcomes, and all but 2 reported at least 1 relevant clinical outcome. All papers studied unstable trochanteric fractures or fracture models.
Table 1. Included biomechanical studies reporting on sliding hip screw (SHS) with trochanteric support plate (TSP), compared to either intramedullary nail (IMN, 5 studies) or SHS alone (1 study), and 95° angled blade plate (1 study)
Table 2. Methods of the clinical studies included reporting on the use of sliding hip screw (SHS) with trochanteric support plate (TSP), without comparator (8 studies) or comparing with intramedullary nail (IMN, 6 studies), SHS alone (5 studies), proximal femur locking plate (PFLP, 1 study), Medoff sliding plate (MSP, 1 study) and dynamic condylar screw (DCS, 1 study). In one study an anti-rotation screw (ARS) was used as an addition to SHS
Table 3. Results of the clinical studies included reporting on the use of sliding hip screw (SHS) with trochanteric support plate (TSP), without comparator (8 studies) or comparing with intramedullary nail (IMN, 6 studies), SHS alone (5 studies), proximal femur locking plate (PFLP, 1 study), or other extramedullary implants (1 study)
16 studies compared SHS plus TSP (SHS/TSP) with other implants. In 3 studies the comparator was SHS without TSP (Su et al. Citation2003, Hsu et al. Citation2015, Haddon et al. Citation2019). In 8 studies SHS/TSP was compared with IMN (Götze et al. Citation1998, Friedl and Clausen Citation2001, Nuber et al. Citation2003, Bong et al. Citation2004, Klinger et al. Citation2005, Bonnaire et al. Citation2007, Walmsley et al. Citation2016, Fu et al. Citation2020), and in 3 studies SHS/TSP were compared with both SHS and IMN (Madsen et al. Citation1998, Tucker et al. Citation2018, Müller et al. Citation2020). In addition, SHS/TSP was compared with other extramedullary implants in 2 papers (Lunsjö et al Citation2001, Selim et al. Citation2020). The lack of standardized methods and reporting of outcomes made a meta-analysis infeasible.
We identified 1,091 clinical cases in the literature where a TSP had been used as an adjunct to the SHS. Overall, 46 cases (4%) of mechanical failures and non-unions were reported. The number of reoperations was 82 (8%), including 19 routine removals of implants. The 10 prospective trials reported 15 reoperations (4%), while 67 (10%) reoperations were reported in the retrospective trials.
Biomechanical studies
SHS/TSP versus SHS (, see Supplementary data)
Su et al. (Citation2003) studied unstable trochanteric fracture models in 10 matched pairs of embalmed femora instrumented with an SHS with or without a TSP. The addition of the TSP to the SHS led to decreased displacement of the head fragment after cyclic loading at 750N.
SHS/TSP versus IMN (, see Supplementary data)
2 studies compared SHS/TSP with an IMN in both cadaveric and synthetic femora using various osteotomies. Friedl and Clausen (Citation2001) concluded that the IMN was more resistant to deformation on cyclic loading than SHS with TSP. Götze et al. (Citation1998) reported a higher load to failure with IMN than SHS with TSP. To compare the biomechanical properties of the SHS plus a TSP with an IMN, unstable, 4-part trochanteric fractures were created in 6 pairs of cadaveric human femora, matched by bone mineral density (BMD), by Bong et al. (Citation2004). In their study the SHS plus TSP provided equal stability and similar ability to resist femoral shaft medialization as the IMN at 250–750 N loading. Walmsley et al. (Citation2016) created unstable intertrochanteric fractures in 24 artificial femora showing similar stiffness but lower axial compression strength when SHS/TSP was compared with an IMN. Bonnaire et al. (Citation2007) studied the influence of BMD on the risk of lag screw cut out in a trochanteric fracture model. They compared fixation with SHS/TSP with 2 types of IMN using cyclic loading at 2000N and found that if BMD was above 0.6 g/cm3 all implants provided sufficient stability to avoid fixation failure.
Clinical studies
Studies reporting SHS/TSP without comparator ( and , see Supplementary data)
We identified 8 patient series without comparator including from 17 to 46 patients, 234 in total. The TSP was mainly used in unstable fractures ( and 4) (Babst et al. Citation1993, Hoffmann et al. Citation1994, David et al. Citation1996, Babst et al. Citation1998, Gupta et al. Citation2010, Cho et al. Citation2011, Prabhakar and Singh Citation2016, Shetty et al. Citation2016). The reporting of surgical and clinical results varied. All papers reported number of reoperations, and at least 1 radiographic and functional outcome. 4 papers reported results of a functional outcome score. All concluded that SHS plus TSP was a viable treatment option.
Studies comparing SHS plus TSP with SHS alone or with other extramedullary implants (, see Supplementary data)
SHS plus TSP was compared with SHS alone in 2 studies and with other extramedullary implants in 2 studies. In the only randomized trial in this review, 100 patients with unstable trochanteric fractures were randomized to SHS with or without a TSP. No clinically relevant differences between the groups were found, either in complications, secondary fracture displacement, or functional results (Haddon et al. Citation2019). Hsu et al. (Citation2015) reported on 252 patients with AO/OTA 31 A2 trochanteric fractures. 205 patients were operated on with an SHS alone and 47 with SHS plus TSP. They performed a risk analysis for postoperative lateral wall fracture (LWF) and found that a lateral wall thickness (LWT) of less than 22 mm strongly predicted a postoperative fracture of the lateral wall. Further, they compared SHS alone (n = 125) and SHS plus TSP (n = 46) as treatment of fractures with a LWT < 22 mm and found that the TSP decreased lag screw sliding and reoperation rate. Lunsjö et al. (Citation2001) performed a secondary analysis of a randomized trial with 569 patients with unstable trochanteric fractures. At the surgeon’s discretion 49 patients were operated on with an SHS and a TSP. No important difference was found between patients operated on with SHS and a TSP compared with patients operated with a Medoff plate or SHS without TSP. Selim et al. (Citation2020) compared SHS plus TSP with a proximal femoral locking plate. The authors found better functional outcome, shorter time to union, and a lower failure rate in the SHS group.
Studies comparing SHS plus TSP with IMN (, see Supplementary data)
Nuber et al. (Citation2003) compared SHS plus TSP with IMN in unstable trochanteric and subtrochanteric fractures and reported slightly better functional results and less pain in patients treated with an IMN. Complication rates and patient satisfaction were similar between the groups. Klinger et al. (Citation2005) compared 51 patients treated with SHS/TSP with 122 patients treated with IMN. They found shorter operating time and hospital stay and fewer complications in the IMN group, but no differences in functional results. In the largest study (n = 234) included in the review, Fu et al. (Citation2020) found no difference in functional scores, fracture healing, failure rate, or rate of reoperation when comparing SHS plus TSP with IMN in both AO type A2 and A3 fractures
Studies comparing SHS plus TSP with both SHS alone and with IMN (, see Supplementary data)
Madsen et al. (Citation1998) compared a consecutive series of 85 patients with unstable trochanteric fractures treated with SHS plus TSP with 170 patients randomized to either an IMN or an SHS. They found a trend towards better functional results and less lag screw sliding in the TSP group, but an even distribution of complications. In a register-based study by Tucker et al. (Citation2018) reporting on more than 3,000 fractures with IMN (598), SHS (2,474), and SHS plus TSP (158), a tendency towards fewer reoperations and better clinical results with IMN was found. Another retrospective cohort compared SHS with or without TSP and IMN (AO/OTA A2 fractures only) and reported a non-significant tendency toward fewer reoperations after IMN (Müller et al. Citation2020).
Discussion
The identified studies presented mainly low-level evidence with only 1 prospective comparison and 1 relatively small randomized controlled trial. All studies reported on unstable fractures or fracture models. A meta-analysis was not possible due to the heterogeneity of the studies.
Research question 1. What are the mechanical properties of the SHS plus TSP compared with SHS alone or with IMN?
The testing circumstances in the trials varied. 3 trials (Götze et al. Citation1998, Friedl and Clausen Citation2001, Walmsley et al. Citation2016) used supraphysiological loads, while in 2 trials (Su et al. Citation2003, Bong et al. Citation2004) the load applied was below normal loading associated with gait (Duda et al. Citation1997). In addition, the fracture models were simple, and thus not comparable to the comminution frequently seen in clinical practice. This complicates the interpretation of the results and limits the clinical value.
In 3 trials (Götze et al. Citation1998, Friedl and Clausen Citation2001, Walmsley et al. Citation2016) composite bones were used alone, or in combination with cadaver specimens. Synthetic bone is probably not adequate when testing a typically osteoporotic fracture model and the results may be of limited value, as the model does not mimic the bone loss predominant in hip fracture patients (Basso et al. Citation2014).
1 trial using cadaveric specimens found that SHS plus TSP provided sufficient stability within a clinical bone density range (Bonnaire et al. Citation2007).
The biomechanical studies using IMN as a comparator all showed that the TSP provided comparable stability to intramedullary nails (). The only biomechanical study comparing SHS with and without TSP (Su et al. Citation2003) used a highly unstable fracture model (AO/OTA A3) and found less displacement with an additional TSP. In comparison, the SHS alone has been reported to have less ability to withstand deformation after cyclic loading than IMN (Kaiser et al. Citation1997, Sommers et al. Citation2004).
Thus, the TSP appears to add stability to the osteosynthesis up to a level comparable with IMN.
Research question 2. Does the TSP lead to an improved clinical outcome compared with SHS alone or with IMN?
The only randomized trial comparing SHS plus TSP with SHS alone was powered to detect a difference in lag screw sliding of 4 millimeters between SHS with and without TSP (Haddon et al. Citation2019). At 1-year follow-up a difference in lag screw sliding of less than 1 mm was found between the groups. With a broken lateral wall (n = 44) the difference was 3 mm in favor of the TSP group (not statistically significant). In the main clinical outcome measure in the trial, the Merle d’Aubigne-Postel score, a statistically non-significant 0.7 difference in favor of the group treated with SHS alone was found. The trial was not powered for subgroup analyses, but even with a larger number of patients included it is improbable that a meaningful clinical difference would have occurred.
A thin or fractured lateral wall may, however, be a predictor of mechanical failure (Palm et al. Citation2007, Hsu et al. Citation2015) and the TSP may have a beneficial effect under these circumstances as reported by Hsu et al. (Citation2015).
A few studies (Madsen et al. Citation1998, Nuber et al. Citation2003, Klinger et al. Citation2005, Tucker et al. Citation2018, Müller et al. Citation2020) included in this review compared SHS plus TSP indirectly with IMN or SHS without TSP. From these studies it may be argued that the TSP protected against secondary fracture displacement. Madsen et al. observed a trend towards better functional results in the TSP group while the other publications failed to show any functional benefit of the TSP compared with IMN.
The findings above may be seen in light of 2 RCTs comparing SHS without TSP with IMN. Parker et al. (2017) included both stable and unstable fractures in a large trial. The authors reported slightly better regain of mobility in patients operated on with an IMN. Hardy et al. (Citation1998) reported similar results in a randomized study of 100 patients. They explained their findings, at least in part, by the significantly larger lag screw sliding distance and subsequent limb shortening in the SHS group.
Based on the existing evidence it is not possible to conclude whether the TSP offers better clinical results than SHS alone, or when SHS plus TSP was compared with IMN for unstable trochanteric fractures.
Research question 3. How does the TSP function in terms of non-union, mechanical failure, and reoperations?
A total of 1,091 SHS plus TSP were reported with 46 (4%) cases of healing problems and 82 (8%) reoperations for any cause. The 2010 Cochrane review (Parker and Handoll 2010), also including a high number of stable fractures, reported a (4%) reoperation rate and 3–4% healing complications and failures after SHS. In the same review the authors found an increased relative risk of cutout with the IMN, but a reduced risk of non-union (both statistically non-significant).
A study from the Norwegian Hip Fracture Register (Matre et al. Citation2013a) reported 10% reoperations at 3 years after AO/OTA A3 fractures and subtrochanteric fractures treated with SHS with or without TSP compared with 7% in the IMN group. This contrasts the findings in a randomized trial (Matre et al. Citation2013b) comparing IMN to SHS with or without TSP where a similar reoperation rate of 8% was reported after 12 months.
10 of the 19 included clinical trials were retrospective cohorts and chart reviews vulnerable to an under-reporting of serious complications and reoperations, as the patients may have sought advice elsewhere, or not at all (). 1 trial was from a register, equally prone to reporting minimum numbers of revision surgeries (Tucker et al. Citation2018). There was, however, no tendency to more reoperations in the prospective trials compared with the retrospective trials in our material.
The rate of complications and reoperations for SHS plus TSP was comparable to previous reports on trochanteric fractures treated with SHS alone or IMN.
Research question 4. Is it possible to work out guidelines for TSP use based on the existing evidence?
All reports included in the review were on unstable fracture models or fractures. This implies that no authors believe that the TSP has a role in stable fractures (AO/OTA 31 A1 and Evans Jensen I–II). The results of the randomized trial comparing SHS with or without TSP suggest that the TSP has at best a limited role (Haddon et al. Citation2019). Some papers report, however, that the TSP increases stability compared with SHS alone (Su et al. Citation2003, Hsu et al. Citation2015) and with a similar stability to IMN (Madsen et al. Citation1998, Bong et al. Citation2004).
The limited literature identified, and the heterogeneity of methods and results, precludes any clear recommendations on when to use the TSP, or if it should be used at all. However, it might be argued that in practices where IMN is not available the TSP might be beneficial when treating trochanteric fractures with a thin or compromised lateral wall.
Strengths and limitations
We believe that our literature search is exhaustive, and we have included both biomechanical and clinical trials. Some papers were not included due to insufficient reporting or failure to obtain a translation. A synthesis of functional results was not possible.
Conclusion
This review did not identify literature clearly advising when to use a TSP. The findings indicated, however, that the TSP may provide a more stable construct, reducing lag screw sliding and medialization of the femoral shaft, than the SHS alone in unstable trochanteric fractures. Whether this translates into improved clinical outcomes compared with SHS alone or with IMN remains unclear. There is a need for high-quality, well-powered clinical trials with relevant outcome measures to clarify any role of the TSP in the treatment of trochanteric fractures.
Supplemental Material
Download PDF (440.2 KB)All authors contributed to study planning. CEA and FF selected the studies and extracted data. CEA wrote the 1st draft and all authors revised the manuscript.
Acta thanks Micha Holla and Olof Wolf for help with peer review of this study.
Supplementary data
Tables 1–3 are available as supplementary data in the online version of this article, http://dx.doi.org/10.1080/17453674.2021.1954305
- Alm C E, Frihagen F, Dybvik E, Matre K, Madsen J E, Gjertsen J-E. Implants for trochanteric fractures in Norway: the role of the trochanteric stabilizing plate—a study on 20,902 fractures from the Norwegian hip fracture register 2011–2017. J Orthop Surg Res 2021; 16(1): 26.
- Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005; 8(1): 19–32.
- Babst R, Martinet O, Renner N, Rosso R, Bodoky A, Heberer M, Regazzoni P. The dynamic hip screw support plate for management of unstable proximal femoral fractures. Helv Chir Acta 1993; 59(4): 521–5.
- Babst R, Renner N, Biedermann M, Rosso R, Heberer M, Harder F, Regazzoni P. Clinical results using the trochanter stabilizing plate (TSP): the modular extension of the dynamic hip screw (DHS) for internal fixation of selected unstable intertrochanteric fractures. J Orthop Trauma 1998; 12(6): 392–9.
- Basso T, Klaksvik J, Syversen U, Foss O A. A biomechanical comparison of composite femurs and cadaver femurs used in experiments on operated hip fractures. J Biomech 2014; 47(16): 3898–902.
- Bong M R, Patel V, Iesaka K, Egol K A, Kummer F J, Koval K J. Comparison of a sliding hip screw with a trochanteric lateral support plate to an intramedullary hip screw for fixation of unstable intertrochanteric hip fractures: a cadaver study. J Trauma 2004; 56(4): 791–4.
- Bonnaire F, Weber A, Bösl O, Eckhardt C, Schwieger K, Linke B. [“Cutting out” in pertrochanteric fractures—problem of osteoporosis?]. Unfallchirurg 2007; 110(5): 425–32.
- Bretherton C P, Parker M J. Femoral medialization, fixation failures, and functional outcome in trochanteric hip fractures treated with either a sliding hip screw or an intramedullary nail from within a randomized trial. J Orthop Trauma 2016; 30(12): 642–6.
- Cho S H, Lee S H, Cho H L, Ku J H, Choi J H, Lee A J. Additional fixations for sliding hip screws in treating unstable pertrochanteric femoral fractures (AO Type 31-A2): short-term clinical results. Clin Orthop Surg 2011; 3(2): 107–13.
- David A, Hufner T, Lewandrowski K U, Pape D, Muhr G. [The dynamic hip screw with support plate—a reliable osteosynthesis for highly unstable “reverse” trochanteric fractures?]. Chirurg 1996; 67(11): 1166–73.
- Duda G N, Schneider E, Chao E Y. Internal forces and moments in the femur during walking. J Biomech 1997; 30(9): 933–41.
- Friedl W, Clausen J. Experimental examination for optimized stabilisation of trochanteric femur fractures: intra- or extramedullary implant localisation and influence of femur neck component profile on cut-out risk. Chirurg 2001; 72(11): 1344–52.
- Fu C W, Chen J Y, Liu Y C, Liao K W, Lu Y C. Dynamic hip screw with trochanter-stabilizing plate compared with proximal femoral nail antirotation as a treatment for unstable AO/OTA 31-A2 and 31-A3 intertrochanteric fractures. Biomed Res Int 2020; 2020: 1896935.
- Götze B, Bonnaire F, Weise K, Friedl H P. Loadability of osteosynthesis of unstable per- and subtrochanteric fractures: an experimental study testing the proximal femoral nail (PFN), the Gamma-nail, the DHS/trochanteric stabilization plate, the 95°angled blade plate and the UFN/spiral blade. Aktuelle Traumatol 1998; 28(5): 197–204.
- Gupta R K, Sangwan K, Kamboj P, Punia S S, Walecha P. Unstable trochanteric fractures: the role of lateral wall reconstruction. Int Orthop 2010; 34(1): 125–9.
- Haddon J, Buciuto R, Johnsen L G. A prospective randomized trial of 100 patients using trochanteric support plates; worth their mettle? Injury 2019; 50(3): 733–7.
- Hardy D C, Descamps P Y, Krallis P, Fabeck L, Smets P, Bertens C L, Delince P E. Use of an intramedullary hip-screw compared with a compression hip-screw with a plate for intertrochanteric femoral fractures: a prospective, randomized study of one hundred patients. J Bone Joint Surg Am 1998; 80(5): 618–30.
- Higgins J, Thomas J, Chandler J, Cumpston M, Li T, Page M J, Welch V A. Cochrane handbook for systematic reviews of interventions version 6.1. Cochrane 2020. Available from: https://www.cochranelibrary.com/.
- Hoffmann T F, Berteloot F, Renneker D. The DHS-trochanter-stabilising-plate: first results after implantation in 20 patients. Aktuelle Traumatol 1994; 24(8): 295–300.
- Hsu C E, Shih C M, Wang C C, Huang K C. Lateral femoral wall thickness: a reliable predictor of post-operative lateral wall fracture in intertrochanteric fractures. Bone Joint J 2013; 95-b(8): 1134–8.
- Hsu C E, Chiu Y C, Tsai S H, Lin T C, Lee M H, Huang K C. Trochanter stabilising plate improves treatment outcomes in AO/OTA 31-A2 intertrochanteric fractures with critical thin femoral lateral walls. Injury 2015; 46(6): 1047–53.
- Kaiser W, Burmester J, Hausmann H, Gulielmos V, Hätzel M, Merker H J. [Comparative stability evaluation of dynamic hip screw and gamma-nail osteosyntheses in unstable pertrochanteric femoral osteotomies]. Langenbecks Arch Chir 1997; 382(2): 100–6.
- Klinger H M, Baums M H, Eckert M, Neugebauer R. Eine vergleichende Untersuchung der Versorgung instabiler per- und intertrochantärer Femurfrakturen mittels DHS-Osteosynthese unter Verwendung der Trochanterabstützplatte und dem Proximalen Femurnagel (PFN) [A comparative study of unstable per- and intertrochanteric femoral fractures treated with dynamic hip screw (DHS) and trochanteric butt-press plate vs. proximal femoral nail (PFN)]. Zentralbl Chir 2005; 130(4): 301–6.
- Knobe M, Gradl G, Ladenburger A, Tarkin I S, Pape H C. Unstable intertrochanteric femur fractures: is there a consensus on definition and treatment in Germany? Clin Orthop Relat Res 2013; 471(9): 2831–40.
- Lunsjö K, Ceder L, Thorngren K G, Skytting B, Tidermark J, Berntson P O, Allvin I, Norberg S, Hjalmars K, Larsson S, Knebel R, Hauggaard A, Stigsson L. Extramedullary fixation of 569 unstable intertrochanteric fractures: a randomized multicenter trial of the Medoff sliding plate versus three other screw-plate systems. Acta Orthop 2001; 72(2): 133–40.
- Madsen J E, Naess L, Aune A K, Alho A, Ekeland A, Stromsoe K. Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screw. J Orthop Trauma 1998; 12(4): 241–8.
- Matre K, Havelin L I, Gjertsen J E, Vinje T, Espehaug B, Fevang J M. Sliding hip screw versus IM nail in reverse oblique trochanteric and subtrochanteric fractures: a study of 2716 patients in the Norwegian Hip Fracture Register. Injury 2013a; 44(6): 735–42.
- Matre K, Vinje T, Havelin L I, Gjertsen J E, Furnes O, Espehaug B, Kjellevold S H, Fevang J M. TRIGEN INTERTAN intramedullary nail versus sliding hip screw: a prospective, randomized multicenter study on pain, function, and complications in 684 patients with an intertrochanteric or subtrochanteric fracture and one year of follow-up. J Bone Joint Surg Am 2013b; 95(3): 200–8.
- Mellema J J, Janssen S, Schouten T, Haverkamp D, van den Bekerom M P J, Ring D, Doornberg J N. Intramedullary nailing versus sliding hip screw for A1 and A2 trochanteric hip fractures. Bone Joint J 2021; 103-b(4): 775–81.
- Müller F, Doblinger M, Kottmann T, Füchtmeier B. PFNA and DHS for AO/OTA 31-A2 fractures: radiographic measurements, morbidity and mortality. Eur J Trauma Emerg Surg 2020; 46(5): 947–953.
- NICE. The management of hip fracture in adults. Available from: https://www.nice.org.uk/guidance/cg124. Retrieved May 2020. London: National Clinical Guideline Centre; 2011.
- Nuber S, Schonweiss T, Ruter A. [Stabilisation of unstable trochanteric femoral fractures. Dynamic hip screw (DHS) with trochanteric stabilisation plate vs. proximal femur nail (PFN)]. Der Unfallchirurg 2003; 106(1): 39–47.
- Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P. Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperation. J Bone Joint Surg Am 2007; 89(3): 470–5.
- Parker M J. Trochanteric hip fractures: fixation failure commoner with femoral medialization, a comparison of 101 cases. Acta Orthop 1996; 67(4): 329–32.
- Parker M J. Sliding hip screw versus intramedullary nail for trochanteric hip fractures: a randomised trial of 1000 patients with presentation of results related to fracture stability. Injury 2017; 48(12): 2762–7.
- Parker M J, Handoll H H. Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev 2010(9): CD000093.
- Parker M, Raval P, Gjertsen J E. Nail or plate fixation for A3 trochanteric hip fractures: a systematic review of randomised controlled trials. Injury 2018; 49(7): 1319–23.
- Prabhakar S, Singh R P. Does modular extension of DHS fix the unstable trochanteric fractures. J Evol Med Dent Sci 2016; 5(54): 3683–92.
- Roberts K C, Brox W T. AAOS clinical practice guideline: management of hip fractures in the elderly. J Am Acad Orthop Surg 2015; 23(2): 138–40.
- Selim A A H A, Beder F K, Algeaidy I T, Farhat A S, Diab N M, Barakat A S. Management of unstable pertrochanteric fractures, evaluation of forgotten treatment options. SICOT-J 2020; 6: 21.
- Shetty A, Ballal A, Sadasivan A K, Hegde A. Dynamic hip screw with trochanteric stablization plate fixation of unstable inter-trochanteric fractures: a prospective study of functional and radiological outcomes. J Clin Diagn Res 2016; 10(9): RC06–RC8.
- Sommers M B, Roth C, Hall H, Kam B C, Ehmke L W, Krieg J C, Madey S M, Bottlang M. A laboratory model to evaluate cutout resistance of implants for pertrochanteric fracture fixation. J Orthop Trauma 2004; 18(6): 361–8.
- Su E T, DeWal H, Kummer F J, Koval K J. The effect of an attachable lateral support plate on the stability of intertrochanteric fracture fixation with a sliding hip screw. J Trauma 2003; 55(3): 504–8.
- Tucker A, Donnelly K J, Rowan C, McDonald S, Foster A P. Is the best plate a nail? A review of 3230 unstable intertrochanteric fractures of the proximal femur. J Orthop Trauma 2018; 32(2): 53–60.
- Walmsley D, Nicayenzi B, Kuzyk P R, Machin A, Bougherara H, Schemitsch E H, Zdero R. Biomechanical analysis of the cephalomedullary nail versus the trochanteric stabilizing plate for unstable intertrochanteric femur fractures. Proc Inst Mech Eng H 2016; 230(12): 1133–40.
