1. Introduction and methodology
Mobility measurement is an important part in terms of diagnostics as well as therapeutics in many musculoskeletal conditions. In former days, clinical examination and radiographic measurement of the joints were sufficient. New technologies and improved treatment created an urge for more precise mobility measurement. This development may be exemplified by determining the movement between bone, cement and prosthesis in joint arthroplasty (Mjöberg et al. Citation1984, Snorrason and Kärrholm Citation1990), growth disturbances in childhood (Kärrholm et al. Citation1982, Bylander et al. Citation1983) and, subsequently, healing determination after spinal fusion (Olsson et al. Citation1976a, Johnsson et al. Citation1990). Roentgen stereophotogrammetric analysis (RSA), or radiostereometry which will be the nomenclature used onwards, was primarily introduced by Göran Selvik (Citation1976) and proved to be a new technique for studying the musculoskeletal system with an increased precision. It is a refinement and completion of previous attempts to study the kinematics of rigid bodies applied on skeletal segments and proved to be such a landmark in the study of skeletal kinematics that it was repeatedly published in 1989 (Selvik Citation1989). It has been applied to normal and abnormal growth in childhood (Bylander et al. Citation1983, Hägglund et al. Citation1986), maxillofacial problems (Rune et al. Citation1980, Citation1986), hip arthroplasty (Baldursson et al. Citation1980, Mjöberg et al. Citation1985), knee arthroplasty (Albrektsson et al. Citation1990, Nilsson et al. Citation1990, Ryd et al. Citation1995), osteotomy in gonarthrosis (Tjörnstrand et al. Citation1981, Magyar et al. Citation1999), and in a multitude of other parts of the skeleton such as the sacroiliac joint and the symphysis (Egund et al. Citation1978, Walheim and Selvik Citation1984, Sturesson et al. Citation2000).
In our laboratory we started applying radiostereometry to the lower lumbar spine in the mid 1980s, inspired by the early work by Olsson et al. (Citation1976a, Citationb, Citation1977). Through more than 15 years it has been our aim to study lumbosacral kinematics in various lumbar spine disorders, and in relation to surgical procedures and external fixation. This presentation is an overview of the technique and applications, and a summary of results when applying radiostereometry to the lumbosacral spine.
Lumbar spine mobility
Spinal mobility occurs over the disc and the two facet joints on a segmental level and can be recorded exteriorly as mobility over single or multiple segmental levels. The vast majority of painful disorders in the lumbar spine are related to movement and loading, which makes it highly interesting to measure spinal mobility in health and in pathological conditions. Thus, it is very logical that many attempts to determine spinal movements exteriorly have been made during the last century (Schober Citation1937, Öhlén et al. Citation1989). Flexion extension is the most studied plane of movement but also movement around the other two axes is of interest. Steinmann pins inserted into the spinous processes have been used to refine the external measurings (Lumsden et al. Citation1968, Pope et al. Citation1977). Results reported have been in part contradictory and the interest has instead focused on radiographic techniques. Multiple studies have shown the accuracy of measuring lumbar spine mobility from flexion extension radiographs to be imprecise with measurement errors from 2–8 mm (Danielsson et al. Citation1988). Biplanar radiographic techniques seem to be able to improve measurement precision but have hitherto mostly been applied for research purposes and not for clinical routine use (Pearcy Citation1985).
Intervertebral discs gradually lose their hydration with ageing and facet joints also degenerate to a high extent. Thus, normal values of mobility should be expected to decrease over the years. The degenerative process has been described in a theoretical model by Kirkaldy-Willis and Farfan (Citation1982) who postulated three stages of degeneration where the middle phase in the degenerative cascade is characterized by instability and the last phase by spontaneous stabilization. This model, however, is mainly theoretically constructed and has not been possible to reproduce in humans. Many patients with degenerative changes of the lumbar spine experience instability-like symptoms which seem to support the theory. Instability has been a clinical description, the radiographic correlation however being hard to verify. In one study (Friberg Citation1987), loading of the spine is claimed to induce abnormal mobility correlating with pain in patients with isthmic spondylolisthesis but generally the characteristics of instability are based on a clinical picture with pain on movement, instability catch, giving away and locking phenomena.
Surgical treatment for low back pain based on disc degeneration traditionally means spinal fusion. A fusion procedure would be expected to alter the kinematics of the lumbar spine with increasing strain on adjacent segments, a theory which has evidence and counter-evidence in the literature (Hunter et al. Citation1980, Dekutoski et al. Citation1994, Schlegel et al. Citation1996, Hambly et al. Citation1998). Today much focus is given to disc prostheses and one of the rationales for this technique would be the less strain put on the adjacent segment by a mobile disc implant compared to fusion.
Another focus for lumbar spine kinematic studies is to identify unintended residual mobility after fusion procedures. Fusion healing is difficult to determine with conventional methods such as plain radiography, flexion extension radiography and computed tomography. This is to a great extent depending on the lack of accuracy of the measurement. Spinal fusion is not a uniformly successful procedure. Whether transpedicular implants, used increasingly in lumbar spine fusion, improve the outcome of fusion is debated (Zdeblick Citation1993, Thomsen et al. Citation1997, Möller and Hedlund Citation2000, Fritzell et al. Citation2002, Ekman et al. Citation2005). The varying outcomes reported may reflect our inability to adequately establish whether movement over the fused segments is abolished (in addition to the well-recognized difficulty in selecting the right patient).
These are only some examples of the need for precise mobility measurements of the lumbar spine in addition to the need for increased knowledge of normal and pathological motion patterns.
Mobility measurements
External measurements of spinal mobility mainly have focused on sagittal mobility, i.e. flexion and extension as these are the motions most accessible for measurement. Schober (Citation1937) introduced the method of measuring skin distraction over the spine on forward flexion. This and the fingertip to floor method of measuring spinal flexion have been the most frequently used previously. The kyphometer introduced by Debrunner (Citation1972) and further elaborated by Öhlén (Citation1989) seems to give a reproducible measure of spinal flexion in a simple way. These techniques however only study mobility in one plane whereas the segmental mobility is three-dimen-sional. Also, movements of the lumbar spine are to a great extent coupled (Lund et al. Citation2002). Flexion extension radiography (Knutsson Citation1944, Hanley et al. Citation1976) is a more precise way to determine movements of the lumbar spine in the sagittal plane. For clinical purpose, mobility in this plane seems to be the most interesting one but measurement errors are considerable. Assessing the degree of spondylolisthesis on lateral radiographs, these measurement errors are shown to be as high as 20% of the sagittal length of the vertebra (= 8 mm) (Danielsson et al. Citation1988). Friberg (Citation1987), using axial compression and traction, claimed that sagittal translations exceeding 5 mm in isthmic spondylolisthesis correlate to low back pain whereas correlation between pain and increased mobility otherwise has been difficult or impossible to demonstrate.
A precise method of measuring lumbar spine mobility was introduced by Pearcy (Citation1985) using biplanar radiography and in models achieving measurement errors along the three axes between 0.20 and 0.31 mm. The technique has been further developed by Frobin et al. (Citation1996, Citation1997) and Leivseth et al. (Citation1998). This might enable future measurements of spinal mobility with improved precision without invasive marker insertion.
However, today, precise mobility measurements of the lumbar spine in relation to clinical disorders and surgical treatments have been mainly produced by means of radiostereometry. Introduced by Selvik (Citation1976), it was applied to the lumbar spine for the study of fusion healing by Olsson et al. (Citation1977). Spinal movements can be studied in three planes measuring translatory movements along the x-, y- and z-axes or angular movements around the same axes. The technique can determine in vivo skeletal kinematics with high accuracy and was introduced in our department for the study of fusion healing in the late 1980s (Johnsson et al. Citation1990). In contrast to most previous measurement techniques, the aim is to study standardized movements to avoid the influence of the degree of patient collaboration and the degree of pain.
Aim of radiostereometry
The aim of this presentation is to describe the techniques of performing radiostereometry from marker insertion to evaluation and to present its clinical applications in studies performed at our institution. It also includes a description of a standardized provocation technique. Applications presented are studies of mobility in normal and degenerative lumbar segments, and in spinal segments with mobility restriction by orthosis or by an external fixator. Further, the postoperative course after fusion procedures using instrumented and noninstrumented, posterior and anterior techniques as well as BMP enhancement has been delineated. Conclusions regarding clinical implications of results are presented.
Radiostereometry method
Marker insertion
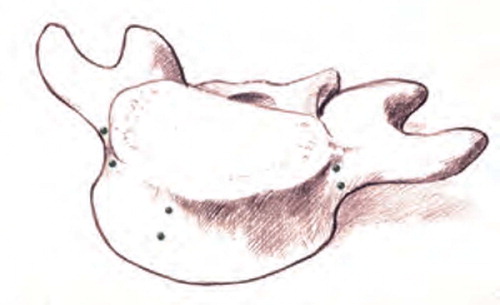
A prerequisite for radiostereometry is the insertion of skeletal tantalum markers. Specially designed insertion instruments exist () and insertion can be performed under local anesthesia but this is cumbersome and mainly our investigations have been performed on patients where the markers have been inserted during a surgical procedure. In order to achieve the highest degree of measurement accuracy, the tantalum markers should be spread three-dimensionally throughout the vertebra. When inserted in posterior procedures, the markers are placed in the transverse processes bilaterally and in the spinous process (). In anterior procedures the markers are placed at predefined locations in the vertebral body (). Two markers are placed on each location.
Figure 1:2 Posterior placing of tantalum indicators in the two transverse processes and in the spinous process to create a three-dimensional rigid body for radiostereometry.
Figure 1:3 Additional tantalum indicators applied in the ventral parts of the vertebra during anterior fusion in order to enlarge the rigid body for radiostereometry.
Ethics committee approval has been achieved for RSA and no complications from marker insertion have been reported in the literature or experienced in our studies.
Radiographic investigation
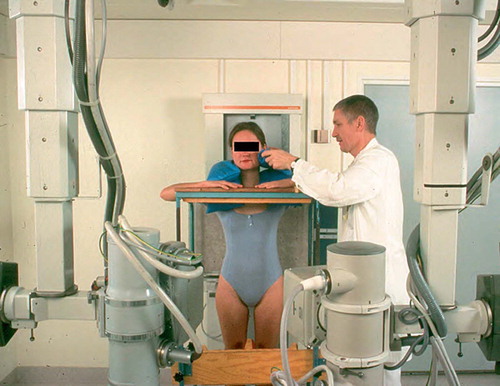
A standard radiographic laboratory can be utilized but some modifications are required. The basic principle is that two simultaneous radiographs with angulation between the radiographic tubes have to be obtained. This requires a set-up with double radiographic tubes (). Further, a calibration cage has to be developed and placed between the patient and the radiographic films. For the simultaneous radiographs, double films have to be used in every investigation. The calibration cage has to be suited to the organ to be investigated and the cage serves both reference and calibration purpose. At each investigation great care must be taken to confirm that all implanted radiographic tantalum markers can be visualized on the radiographic films. The radiographic investigations are performed at predetermined follow-up times after surgery in the investigations where fusion healing was determined. The patient positioning in the investigations are described in the chapter on standardization of provocation below.
Digitization
The individual tantalum markers in the skeleton are identified on both radiographs. This was performed on analogue radiographic pictures for most parts of the study but, after the digitization of the radiographic department, it was performed on monitors. Information on the individual tantalum markers, identified by numbers, are fed into a computer using the Kinema software (RSA Biomedical Innovations AB, Umeå Sweden) where the two dimensional distances between the images of the metallic markers formed the input data for conversion to a three-dimensional co-ordinate system.
Evaluation
A built-in system for identification of stability/ instability of the markers has been developed (Kärrholm Citation1989) by means of determining rigid body deformation. This excluded, the Kinema program can determine mobility for lumbar spine segments along transverse (x), longitudinal (y) and sagittal (z) axes or rotations around x-, y- and z-axes. Depending on type of study, either movements between skeletal parts or skeletal parts and implants can be determined, or changes between tantalum markers recorded over time.
Standardization of provocation
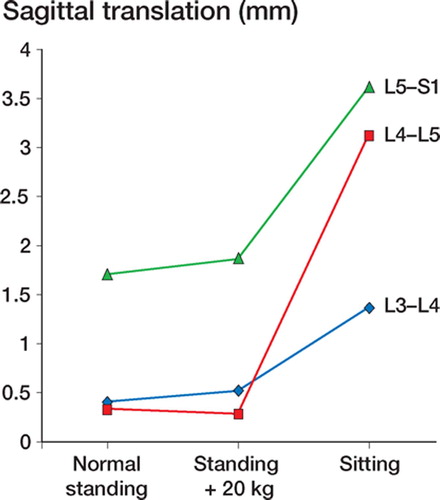
Mobility of the lumbar spine, especially active flexion/extension, is to a high extent dependent on pain level of the patient, cooperation of the patient and understanding of the procedure. This means that a patient can show very different mobility patterns from one day to another. Therefore, for RSA investigations it has been judged mandatory to standardize the mobility provocations. In early studies, we restricted mobility provocation to comparing mobility from supine to standing position. In some situations, for example in the early postoperative phase, this might be the only provocation biomechanically acceptable. However, more powerful provocation seems desirable. The mobility response provided when the patient changed from supine () to three different standardized positions, i.e. standing position (), sitting with semiflexed hips () and standing with axial load applied on the shoulders (), were compared (Axelsson and Karlsson Citation2005). This investigation showed clearly that axial loading did not give additional information as compared to normal standing whereas the sitting position increased the mobility significantly (, ). Due to these facts, we preferably provide standardized provocation of lumbar mobility by the positional change from supine to the sitting position if such provocation is not contradicted by postoperative restrictions.
Figure 1:4B RSA in normal standing position in a stabilizing frame with no weightsharing on the arms. (Reproduced with permission from Spine).

Figure 1:4C RSA in sitting position on a chair with standardized lowering of the knees allowing free passage of the x-rays above the femoral shafts to the lumbosacral spine. (Reproduced with permission from Spine).

Figure 1:4D RSA in standing position with sandbags weighing in total 20 kilograms equally distributed on both shoulders. (Reproduced with permission from Spine).
Accuracy measurements
Accuracy of the average stereometry applied to the lumbar spine was initially determined by double examinations of 8 patients with good osseous fusion radiographically in an early patient series (Johnsson et al. Citation1990). Standard deviations for the error of measurement in this study were found to be 0.08, 0.17 and 0.22 mm for the transverse (x), vertical (y) and sagittal (z) axes, respectively. The corresponding minimally significant (p < 0.01) translations are 0.22, 0.49 and 0.64 mm, respectively. Translations lower than these values are considered insignificant. In a later study, including the sitting position (Johnsson et al. Citation2002), significant mobilities along the respective axes using 99 % confidence intervals were 0.41, 0.42 and 0.60 mm and the corresponding rotations were 1.89°, 0.43° and 0.78°.
2. Lumbar segmental mobility – normal and pathologic
Normal lumbar segments
To define normal spinal intervertebral mobility would have a certain value as a baseline and a comparison for the radiostereometric studies of pathological conditions. Since the method includes the invasive implantation of skeletal markers, it had not been applicable to the asymptomatic individual without pathologic disc morphology required for assessment of normal mobility.
With the original aim to analyze intervertebral mobility in defined stages of disc degeneration (Axelsson and Karlsson Citation2004), we applied radiostereometry (Selvik Citation1989) in 18 patients. Apart from the degenerated level, a normal disc was identified at the L3-L4 level in 14 of these patients, at L4-L5 in 5 patients and at L5-S1 in 6 patients. The mobility response over these non degenerated discs induced by the patient changing from supine, as the baseline position, to a standardized sitting position (Axelsson and Karlsson Citation2005) are given in .
Table 2 :1. Intervertebral translations (mm) over 25 normal discs
For the lumbosacral level, the most pronounced sagittal mobility was 5.9 mm seen in patient number 2. The least mobility with the same provocation was 1.4 mm seen in patient number 17. The corresponding maximum and minimum values for vertical translation were 4.2 mm (patient number 7) and 0.1 mm (patient number 11).
At the L4–L5 level, maximum sagittal mobility response was 4.5 mm measured in patient number 14. The minimum value provided along the same axis was 0.8 mm seen in patient number 18. Vertically the extreme values were 3.9 mm and 0.8 mm in patient number 14 and 15, respectively.
For the L3–L4 level, maximum and minimum sagittal translations were 3.5 mm in patient number 7 and 0.1 mm in patient number 18. The vertical mobility was most pronounced in patient number 2 measuring 5.1 mm and the lowest vertical value was 0.1 mm for patient number 5.
The fact that several normal segments in these studies had adjacent segments being degenerated brings certain limitation when making conclusions about normal lumbar intervertebral mobility based on the current information. Anyhow, it is an interesting fact that the sagittal and vertical translation for one vertebra relative to the adjacent distal vertebra can differ from no translation at all up to 6 mm at the extreme for individuals with the same normal disc status and when the provocation is standardized without active movements in flexionextension. These pronounced interindividual differences implies that the RSA study bringing the strongest evidence compares the same individual over time for example through a postoperative course or when changing external factors such as with and without orthosis or locking/unlocking an external fixator.
Degenerated lumbar segments
The progressive course of the degenerative process was described by Kirkaldy-Willis and Farfan (Citation1982) who claimed three separate stages defined by differing characteristics of segmental mobility and stability. An early stage of temporary dysfunction is subsequently transformed into a stage of segmental instability which is evidenced by a resulting deformity. With the deformity, the third and last stage of definitive stabilization is reached caused by osteoligamentary repair mechanisms. Such a three stage course would have certain clinical implications. According to Kirkaldy-Willis and Farfan (Citation1982), a stenotic segment with a degenerative slip that has reached the fixed stage of stabilization could be treated with decompression only, while a patient in the unstable second stage rather needs a supplementary fusion. The three stage theory also claims that the stability characteristics of a segment can be deduced from the current degenerative radiographic findings which would bring a possibility to select the individual patient for the appropriate treatment. Radiostereometry can not be used in routine clinical practice for this purpose but has the adequate measurement accuracy to test the hypothesis concerning instability and whether certain radiographic degenerative findings are connected to a specific mobility status.
Eighteen patients were considered for a lumbar fusion due to long standing low back pain on disc degenerative basis (Axelsson and Karlsson Citation2004). The status of the L4–L5 and L5–S1 discs were assessed semiquantitatively by conventional radiography and a T1, T2 weighted MRI. Five categories were defined based on a modification from Saraste et al. (Citation1985); normal disc height without dehydration (I A), normal disc height with dehydration (I B), disc height decreased by less than 50 percent (II), disc height decreased by at least 50 percent (III) and disc height obliterated (IV).
An external pedicular fixation test (Magerl Citation1984) was included for each patient to prognostify the result of a definitive stabilization by fusion (Olerud et al. Citation1986). The insertion of the pedicular Schanz screws required general anesthesia and the tantalum indicators for RSA were implanted percutaneously during the same procedure. Two months after extraction of the temporary Schanz screws, the influence of the external fixation was considered minimal with the soft tissues fully healed and the usual lumbar mobility restored. RSA was performed under these conditions with the patients in supine and sitting positions (Axelsson and Karlsson Citation2005). The intervertebral mobility provided when the patient changed position from supine to sitting was calculated for L4 relative to L5 and for L5 relative to the sacrum.
Eleven discs were unaffected by degeneration, category IA (). Dehydration without disc height reduction, category IB, was seen in 7 discs. Category II with the disc height decreased less than 50 percent and category III with a disc height reduction of at least 50 percent included 10 and 8 discs, respectively. No discs were obliterated, classified as category IV.
Table 2 :2. Intervertebral translations (mm) over 36 discs ordered according to the grade of degeneration
Mean intervertebral mobility was compared for the four disc categories found. Changing position from supine to sitting induced a mean vertical translation of 2.0 mm over the 11 discs categorized as IA (). A small increase in mobility with progressive loss of disc height through the degenerative stages IB (7 discs) and II (10 discs) to 2.2 mm and 2.6 mm was not significant according to the confidence intervals given in . Further degeneration to grade III seen for 8 discs meant a significant mean vertical mobility reduction to 0.8 mm (p=0.01, Student t test). The corresponding values for sagittal translations were 3.0 mm, 3.1 mm, 3.6 mm and 1.7 mm for the four disc categories found (). These alterations were not statistically significant.
Figure 2:1 Mean vertical intervertebral mobility with confidence intervals given for 36 discs categorized according to the grade of degeneration. (Reproduced with permission from Eur Spine J).
Figure 2:2 Mean sagittal intervertebral mobility with confidence intervals given for 36 discs categorized according to the grade of degeneration. (Reproduced with permission from Eur Spine J).
Our result brings support for a late stage of stabilization within the degenerative course as proposed by Kirkaldy-Willis and Farfan (Citation1982). This stage begins when the disc height is reduced by at least 50 percent. For the clinical situation, the stability can however not be deduced from the radiographic degenerative findings since the interindividual differences in mobility were considerable for discs with the same stage of degeneration (). For the same reason, a fully stable situation can not be taken for granted even when the disc height is reduced by 50 percent. An unstable phase preceding the stage of stabilization, also claimed by Kirkaldy-Willis and Farfan (Citation1982) in their three stage theory for the degenerative course, is in clinical practice supported by the resulting deformity but could not be verified as hypermobility in the limited patient cohort examined here.
Spondylolytic lumbar segments
In the growing adolescent spine, a spondylolytic defect in pars interarticularis can cause instability as evidenced by the resulting forward slip of the affected vertebra. In the adult spine, the question about instability is more controversial since a progressive deformity with increased slip is seldom seen. In this category, the course rather has degenerative characteristics with low back pain appearing first in the middle age. We applied RSA to compare the mobility of a spondylolytic vertebra in the adult with the mobility of a vertebra without spondylolysis (Axelsson et al. )
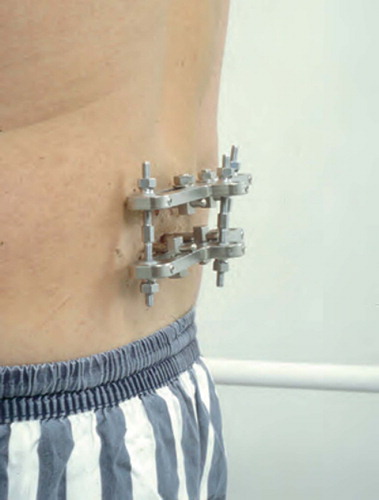
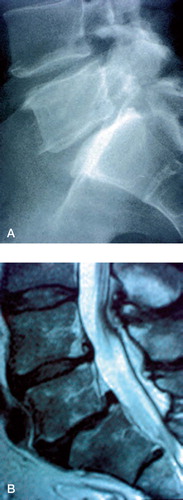
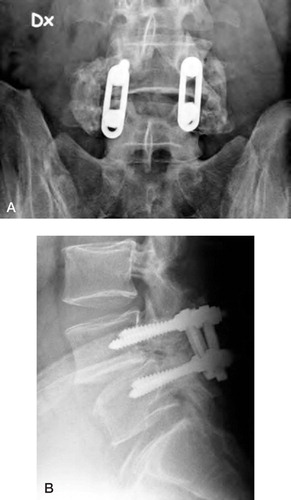
Eight patients with low back pain, spondylolysis of L5 and a spondylolisthesis grade 1-2 (, ) had an external fixation test (Magerl Citation1984)) as part of the prognostication for a sub sequent fusion (Olerud et al. Citation1986). Pedicular screws for fixation and tantalum indicators for RSA were inserted with percutaneous technique in the same procedure using general anesthesia. Two months after terminating the external fixation test by extracting the pedicular screws, the soft tissues were healed and RSA was, in this study, done with the patient in supine and standing positions (Johnsson et al. Citation1990). The intervertebral mobility of the spondylolytic vertebra relative to the sacrum, induced by this change in position, was calculated. For comparison, eight patients without spondylolysis/olisthesis but with lumbar pain presumably on degenerative basis were examined in exactly the same manner. The patients from the two groups were matched in pairs according to sex, affected lumbar segment and grade of disc degeneration.
Figure 2:3 A. Spondylolysis and grade I olisthesis in a 46-year-old man having low back pain for one year. B. MRI reveals degenerative findings of the disc under the slipped vertebra with disc height reduction, dehydration and endplate reaction.
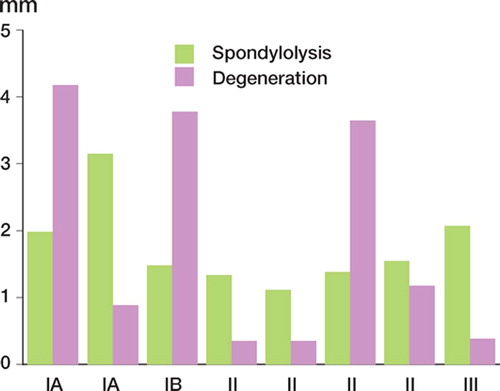
The mean vertical intervertebral translation was 0.7 (0 to 1.6) mm in the spondylolytic group and 0.8 (0.1 to 2.5) mm in the degenerative group. The corresponding figures for the sagittal translations were 1.8 (1.1 to 3.1) mm and 1.8 (0.3 to 4.2) mm, respectively. A Wilcoxon signed-rank test comparing intervertebral mobility for matched pairs in the two groups revealed no significant differences neither along the vertical axis (p=1) nor the sagittal axis (p=0.8). The mobility response along the sagittal axis is given in with the patients paired according to sex and disc status. The mobility of the degenerative group tended to vary irrespective of the grade of disc degeneration while the mobility for the spondylolytic group was more homogenous through the degenerative stages.
Figure 2:4 Lumbosacral sagittal mobility in eight patients with spondylolysis and low back pain compared in matched pairs with the mobility of patients without spondylolysis having low back pain on degenerative basis. The grade of disc degeneration is categorized and given on the x-axis for each pair. (Reproduced with permission from Spine).
According to this study, the spondylolytic defect in pars interarticularis does not induce a situation of permanent instability that can be detected in the adult patient with low back pain and low-grade spondylolisthesis. The prevalence of progressive disc degeneration is increased below a spondylolytic vertebra (Szypryt et al. Citation1989) and, in clinical practice, the patient with a low-grade olisthesis often presents a low back problem in the middle age after a long asymptomatic youth. Considering these three facts, the low back pain in the adult patient with a lytic low-grade spondylolisthesis seems rather to have degenerative reasons than being a manifestation of instability.
3. External pedicular fixation
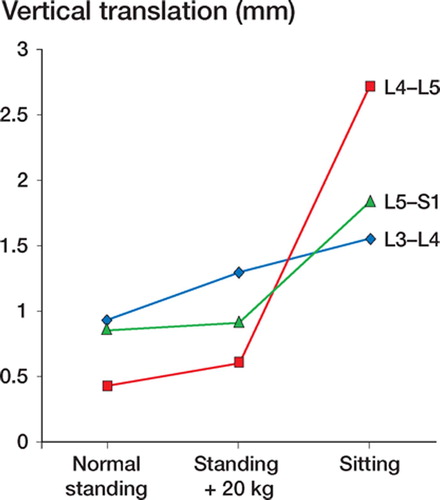
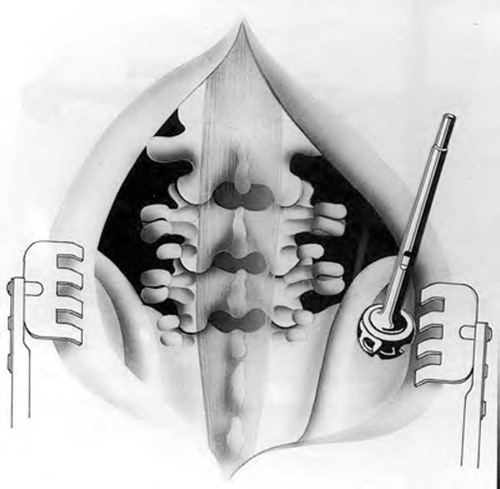
The pain relief induced by spinal fusion is ascribed the abolishment of painful intervertebral mobility. If we accept this as a rationale for treating low back pain (Frymoyer and Selby Citation1985), then a method providing the locking effect temporarily during test conditions would have a certain value for prognostifying the outcome of the definitive fusion. External pedicular fixation () was originally introduced for treating vertebral fractures (Magerl Citation1984) but later applied to the problem of patient selection in lumbar fusion (Olerud et al. Citation1986). We have used radiostereometry (Selvik Citation1989) to study the mechanical properties of the external frame used for fixation. The aim was to assess the grade of stabilization when the frame is in the locked position but also whether unlocking means restitution of intervertebral mobility in spite of the pedicular Schanz screws passing through the soft tissues and in close relation to the facet joints. Such dynamics would be a prerequisite to provide the adequate mechanical basis for the prognostic test fixation.
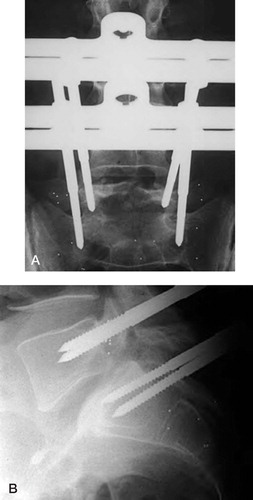
Ten patients with spondylolysis-olisthesis grade 1–2 and no prior spinal surgery had an external fixation of the olisthetic lumbosacral segment (Axelsson et al. Citation1996). Both Schanz screws for the external fixator and tantalum skeletal markers for RSA were inserted during general anaesthesia and by percutaneous technique at standardized anatomical landmarks (). The external frame was fixed with the grade of lordosis chosen by the patient to be the most comfortable and active distraction/ compression was not intended. The time for test fixation was seven days during which the patients were encouraged to perform the activities that usually provoked lumbar pain in order to facilitate the evaluation of any possible pain relieving effect.
Figure 3:2 Tantalum indicators for radiostereometry implanted into the bases of the two transverse processes of the spondylolytic fifth vertebra and in the lateral masses and the central portion of the sacrum. Two pedicular screws are placed on each level. A. Anteroposterior view. B. Lateral vew. (Reproduced with permission from Spine).
In three patients the external frame covered too many of the tantalum indicators to permit RSA and the number of patients evaluated was therefore reduced to seven. Each patient had three separate examinations. On the seventh day after screw application the screw related pain was considered minimal and RSA performed both with the external frame fixed and with the frame loosened. The third examination was done six weeks after fulfilling the test fixation with the Schanz screws removed, the soft tissues fully healed and the usual lumbar mobility regained. Each RSA included examination in standardized supine and erect positions (Johnsson et al. Citation1990). The translatory movements of the olisthetic fifth vertebra in relation to the sacrum induced by this positional change were calculated along the three axes; transverse, vertical and sagittal.
In the seven patients included, the mean sagittal translation was significantly reduced with the external frame fixed (p=0.01, Student t test). The mean sagittal translation of L5 was 1.9 mm without the external frame, 2.1 mm with the frame loosened and 0.7 mm with the frame fixed. By fixing the frame, the sagittal mobility was significantly reduced in six patients compared to the mobility without frame or with the frame loosened (). In three of these, cases 2, 3 and 5 (), the fixation reduced the translation to a level beneath the measurement accuracy (). In the seventh patient, case number 4, the sagittal translations were small in all three situations and a clear stabilizing effect was not verified.
Figure 3:3 Sagittal intervertebral translations for seven patients measured both with the external frame loosened and with the frame fixed. The dotted line indicates the accuracy for sagittal translation, 0.7 mm. (Reproduced with permission from Spine).
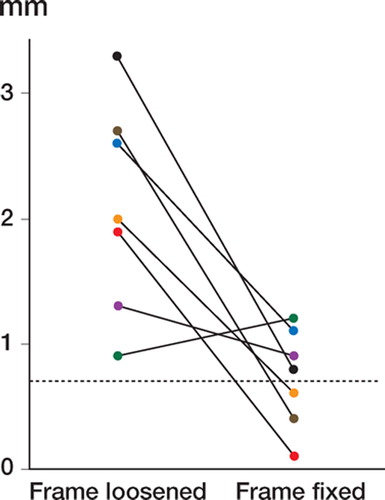
Table 3 :1. Clinical data and RSA intervertebral translations in 7 patients without fixator (left columns), with external fixator fixed (middle columns) and loosened (right columns)
For the mean vertical translations, the immobilizing effect induced by the fixed frame was not as consistent (p=0.15, Student t test) as in the sagittal plane. The mean vertical translation was 1.0 mm without frame, 0.7 mm with the frame loosened and 0.4 mm with the frame fixed. The most pronounced mobility vertically seen in cases 1, 3 and 7 were however all fully stabilized when the external frame was fixed. The transverse translations were mostly negligible in all three situations.
Loosening of the frame yielded regained mobility in all except one patient, case number 1, who regained mobility first when the frame and the screws were fully extracted ().
Several studies claim a prognostic value of the external fixation test in selecting patients for a subsequent fusion (Esses et al. Citation1989, Soini et al. Citation1993, Jeanneret et al. Citation1994, Bednar and Raducan Citation1996, Axelsson et al. Citation2003). Divergent results from in vitro studies (Schläpfer et al. Citation1982, Lund et al. Citation1999) have however questioned the mechanical capacity for achieving the requisite stabilization by using the external fixator. Studied here in vivo and by radiostereometry, the fixator does reduce and in most cases fully abolish the intervertebral mobility of a single spinal segment. Loosening the frame can reproduce the pain by the immediate restitution of the mobility over the segment even though the pedicular screws run through the soft tissues and in close relation to the facet joints. We conclude that the external fixator designed by Magerl has the stabilizing properties and dynamics to provide the adequate mechanical basis for the external fixation test as prognostic instrument in lumbar fusion.
4. Posterolateral uninstrumented fusion, stabilization schedule
The posterolateral uninstrumented fusion () includes decortication of transverse processes, lateral aspects of the articular processes and, when the sacrum is involved, the lateral masses of the sacrum. Bone grafting is performed from the posterior iliac crest (). This procedure is carried out since the 1940s but its use has decreased during later decades partly because of a nonunion rate of 15–35%, and partly because of a belief that the disc is the most common pain generator in disc degenerative disease and should be removed. The posterolateral fusion has been supplemented with transpedicular fixation and alternative interbody fusion techniques such as ALIF, PLIF and TLIF have been developed. Recent large multicenter prospective studies on lumbar spinal fusion do however not demonstrate a beneficial effect in terms of patient outcome using these methods while both costs and complication rates are increased. Therefore, the uninstrumented, posterolateral technique still seems a valid alternative in lumbar spine fusion.
Figure 4:1 Uninstrumented fusion with solid bony bridging between the transverse processes of the L4 and L5 vertebra. A. Anteroposterior view. B. Lateral view.
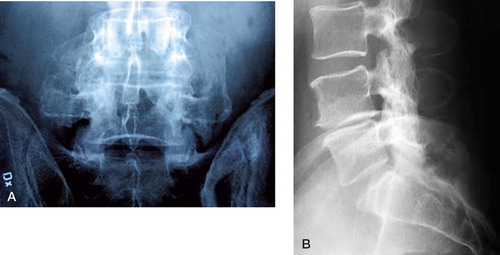
Figure 4:2 Schematic drawing of posterolateral uninstrumented fusion after decortication but before bone harvesting with a reamer.
For these reasons and due to the need for planning the after-treatment after surgery, the stabilization schedule after uninstrumented fusion is of great interest. In 11 patients, aged 33 (21–59) years with either spondylolysis/olisthesis grade 1–2 or disc degenerative disease in the lower lumbar spine, tantalum marker insertion was performed at the time of uninstrumented fusion which in 4 cases was performed between L5 and S1 and 7 between L4 and S1 (Johnsson et al. Citation1990). The surgical procedure was strictly standardized using autogenic bone graft from one or both iliac crests and decortication of the transverse processes and the lateral masses of the sacrum. The postoperative treatment included a soft orthosis for 5 months.
Monthly radiostereometric investigations comparing the supine to the standing positions were performed up to 6 months after surgery and with a final investigation after 12 months. Minimum significant translations (accuracies) in this setting were determined to be 0.3, 0.6 and 0.7 mm along the transverse, vertical and sagittal axes.
Eight of the 11 fusions healed radiographically. The sagittal and vertical translations over time for these patients are demonstrated in , and in showing a decrease in translation gradually over time. The majority of patients were fully stable first 12 months after surgery. For the group of patients obtaining fusion, mean vertical translation was 0.5 mm at 6 months and 0.3 mm at 12 months, as compared to the nonfusing patients displaying mean 0.9 mm at 6 months and 1.2 mm at 12 months. Corresponding figures along the sagittal axis were for the fusing patients mean 1.1 mm at 6 months and 0.7 mm at 12 months while the non-unions showed mean 6.1 mm at 6 months and 5.9 mm at 12 months. Clinically, one of the fused patients had persisting bilateral sciatic pain and two of three non-unions were painless.
Figure 4:3 Mean sagittal translation determined by radiostereometry in 8 solidly healing uninstrumented fusions. The dotted line indicates the accuracy for sagittal translation, 0.7 mm.
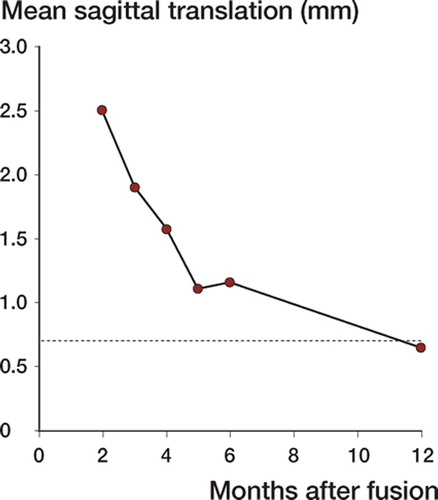
Figure 4:4 Mean vertical translation determined by radiostereometry in 8 solidly healing uninstrumented fusions. The dotted line indicates the accuracy for vertical translation, 0.6 mm.
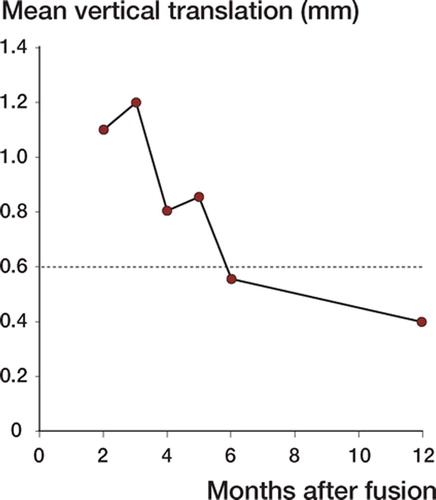
Table 4 :1 Mobility schedule over time for 11 patients with uninstrumented fusion
This investigation was designed to determine the timetable for intervertebral stabilization after uninstrumented posterolateral fusion in the lower lumbar spine. In conclusion, stabilization schedule is slow and remaining mobility is a frequent finding even 6 months postoperatively in patients ending up with a stable fusion one year after surgery.
5. Instrumented fusion, stabilization schedule
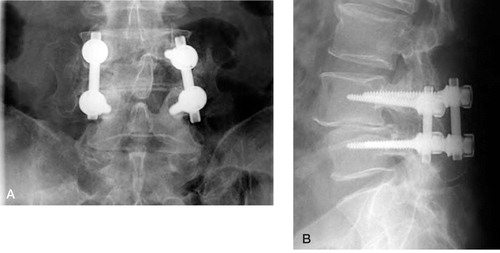
Posterior transpedicular fixation of lumbar spinal fusions () has become increasingly popular, although some debate over the need for supplementary fixation exists, and the complication rate has been shown to be higher when instrumentation is used (Thomsen et al. Citation1997, Fritzell et al. Citation2003). The following investigation was carried out in analogy to the study of the stabilization schedule for posterolateral uninstrumented fusion (Johnsson et al. Citation1990), with the main aim to see whether transpedicular instrumentation gave immediate and persistent stability to the segments aimed for fusion.
Figure 5:1 Instrumented fusion L4–L5 with bridging trabecular bone between transverse processes lateral to VSP implants. A. Anteroposterior view. B. Lateral vew.
The schedule for stabilization according to RSA, thus, was evaluated after instrumented posterolateral fusion in 12 patients (Johnsson et al. Citation1999b). Patient age was 39 (20–56) years. The indications for surgery were spondylolysis/olisthesis in three cases (slips grade 1, 2 and 3), instability after facetectomy in two cases and disc degenerative back pain in the remainder. All patients wore a soft brace during daytime for 4 months postoperatively. RSA investigations, supine to standing provocation, were performed at one, 6 and 12 months after surgery.
Two patients with pronounced olisthesis at the L5 had a wide decompression at that level and fixation between the L4 and S1 vertebrae only. These patients showed a postoperative course differing significantly from the remaining 10. Both patients had persisting mobility along the sagittal axes at one year postoperatively. In one of the patients there was a sacral screw loosening but extended follow-up until two years postoperatively showed healing of the fusion ultimately.
For the remaining 10 patients with one-level fusions in 8 cases and two-level fusions in two cases, the latter with screw fixation in all three vertebrae, the postoperative RSA course was uneventful. In the two two-level fusions and in one onelevel fusion, sagittal translations less than 1.3 mm but exceeding the accuracy of the method persisted at 6 months but had disappeared at the 12 months follow-up.
The conclusion of this study is that posterior transpedicular fixation of the inherently stable lumbar spine, even in the case of previous facetectomy, gives immediate and persistent stability. In the cases with wide decompression and lack of fixation of the intermediate vertebrae, prolonged immobilization, or, preferably anterior supplementing fusion must be considered.
6. Posterior transpedicular stabilization techniques
Biomechanical testing of spinal implants of transpedicular type has been most abundant but the step from the test situation to real life is not always obvious. Radiostereometry yields the possibility to complement the biomechanical testings with studies of the in vivo kinematics of transpedicular implants. More or less all fusions enhanced by transpedicular systems include autogenic or allogenic bone transplantation as the implants would be expected to sustain fatigue fractures in the long run. However, as demonstrated in the chapter on posterolateral uninstrumented fusion above, stabilization occurs slowly (Johnsson et al. Citation1990). At 4 weeks after an instrumented fusion, the auto- or allogenic bone cannot be assumed to contribute to stability of the segment which, thus, is more or less totally dependent on the transpedicular implant. This time point is therefore very well suited for studying the stabilizing effect of inserted implants.
The aim of this study (Gunnarsson et al. Citation2000) was to determine the radiostereometric mobility at 4 weeks after instrumented posterolateral lumbar fusion using two types of implant, the VSP plate and screw system () and the Diapason rod and screw system (). In all, 14 patients with age 45 (33–56) years, were operated using one of the two systems and matched regarding gender and number of levels fused. One of the patients had spondylolysis with low grade slipping, the remaining patients either had degenerative disc disease (n = 8) or pain after previous disc or decompressive surgery (n = 5). In three of the cases concomitant nerve root decompression was performed with facet joint preserving technique. Standard surgical technique with posterolateral decortication and autogenic bone + instrumentation with either system was performed using an image intensifier.
Figure 6:1 Instrumented fusion L4–L5 with bridging trabecular bone between transverse processes lateral to Diapason implants. A. Anteroposterior view. B. Lateral vew.
At 4 weeks after surgery, when soft tissues were judged to have healed and postoperative pain subsided but no stabilizing effect of bone transplant had occurred, radiostereometry was performed in supine and standing position.
The results () show that no mobility along any axes were seen for any of the patients except R4, a patient with rods and screws from L5 to S1, with a sagittal mobility exceeding the accuracy of the method. At later follow-up, this mobility disappeared and the fusion healed uneventfully.
Table 6. 1. Intervertebral translations (mm) 4 weeks after fusion for all operated segments
The significance of this study is in our opinion that posterior stabilization with transpedicular techniques in the inherently stable spine gives a very good immediate stability, and, also, that the study set-up described may be used for comparing implants of different locations and types in the future. An unpublished series of patients operated on with the CCD technique and another with the Ultium plates and screws, both also posterior transpedicular implants, have given similar outcome.
7. Transarticular fixation of facet joints with biode gradable rods
Biodegradable rods (Biofix, Bioscience, Tampere) consist of self-reinforced polyglycolic acid composite material (Vainionpää et al. Citation1987). They degrade postoperatively, losing the major part of their mechanical strength within a month and disintegrating entirely within 6–12 months. Theoretically, biodegradable rod fixation of facet joints would yield increased immediate stability after uninstrumented fusions but avoid the risk for implant related complications and the sometimes occurring need for implant removal after fusion healing.
On this subject, a fusion series was performed (Johnsson et al. Citation1997) with conventional posterolateral technique supplemented by filling the facet joints with autogenous bone. Further, perpendicular to the joint line of each facet joint, a canal was drilled with a width of either 2 or 3.2 mm depending on the size of the facet joint. These canals were filled with biodegradable rods which by absorbing fluid in the body expanded rapidly and became fixed in the canal within a few minutes from insertion. The rod length used in our study was 3 cm and the diameter 2 or 3.2 mm. These rods have been demonstrated to have an initial shear strength of 180–200 MPa and a bending strength of 300–350 MPa, thus, values at least 20 times higher than the strength of cancellous bone.
In total, 11 consecutive patients with mean age 46 (39–59) years were enrolled. All patients had longstanding segmental type of back pain refractory to non-surgical treatment and emanating from disc/facet joint degeneration. Decompression was in no case part of the procedure and no patient had previous spinal surgery. Seven patients had L5–S1 fusions and the remaining four had L4–S1 fusions.
The follow-up schedule was similar to the one presented for the posterolateral instrumented fusions above (Johnsson et al. Citation1999b), i.e. monthly investigations up to 6 months and a final investigation at 12 months, including RSA, clinical investigation and plain radiography. For the RSA, supine to standing provocation was used.
All 7 patients with L5–S1 fusions healed radiographically and became rigid according to radiostereometry. Three of the fusions were stable at the first postoperative investigation and remained so, one from the 3 month investigation onwards, two from the 5 month investigation onwards and the final patient not until 12 months after surgery. Contrarily, none of the 4 patients with L4–S1 fusions healed. One of the patients had to be excluded because of inadequate placement of the tantalum markers. In the three remaining cases 1–3 mm sagittal translations persisted at 12 months after surgery and plain radiography only showed partial osseous fusion. No implant-related complications, such as nerve root pain or radiographic signs of osteolysis around the biodegradable rods occurred.
In conclusion, biodegradable rods inserted into the facet joints as part of the fusion procedure do not provide a full immediate stabilization to be relied on during the postoperative period of fusion consolidation. A clear positive effect on fusion healing was not verified for the current patient series.
8. Anterior stabilization
The stabilizing effect of interbody cages in lumbar spine fusion is questioned. Supplementary ante-rior/posterior instrumentation is a frequent surgical recommendation based on in vitro results of human cadaveric studies. The mobility reduction in flexion is around 40 percent both for the anterior (ALIF) and posterior (PLIF) approach when testing the three-dimensional mobility response putting standardized well-defined load on a specimen with interbody cage implants (Oxland and Lund Citation2000). No stabilizing effect is seen in extension. Some but inadequate reduction is also registered for the axial rotation and lateral bending both by the ALIF and PLIF with some advantage for the anterior technique. Other authors report inconsistent mechanical effects with even increased segmental mobility over the disc space with cage implants, which could be a consequence of the resection of the anterior longitudinal ligament included in the ALIF and of the medial facetectomy required for the PLIF (Vishteh et al. Citation2005). Such surgical destabilization, if confirmed in vivo, would be a certain reason to limit the use of the interbody cage fusion technique instead favouring alternative procedures to provide immediate postoperative stability.
In a previous RSA based study, intervertebral mobility before surgical intervention was measured in 18 patients with degenerative disc disease (Axelsson and Karlsson Citation2004). Tantalum indicators for this RSA assessment were implanted percutaneously from behind in connection with the application of pedicle screws for an external fixation test (Magerl Citation1984, Olerud et al. Citation1986). The spinal RSA was performed two months after finishing the test fixation in order to avoid any influence on lumbar range of motion caused by the test procedure. The mobility response induced by the patient changing from supine to a standardized sitting position (Axelsson and Karlsson Citation2005) was thereby measured for the L4–L5 and L5–S1 levels.
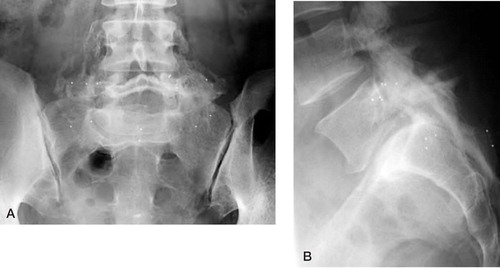
Among these patients having defined ranges of preoperative intervertebral mobility, 4 patients were recommended to undergo a subsequent anterior lumbar interbody fusion (Johnsson et al. Citation1999a). This recommendation was based on a positive outcome at temporary fixation. Two threaded, cylindrical cages were used as a stand alone procedure via a retroperitoneal approach (). One patient was operated on two lumbar levels, L4–L5 and L5–S1. The other 3 patients all had an isolated lumbosacral fusion. At surgery, additional tantalum indicators were applied in the ventral aspects of the vertebrae to be fused (), in order to improve the basis for the postoperative radiostereometric evaluation.
Figure 8:1 Patient number 1. Conventional radiography showing no reaction around the implant at one year follow-up. Tantalum indicators both in the ventral and dorsal parts of the vertebrae fused. A. Anteroposterior view. B. Lateral view.
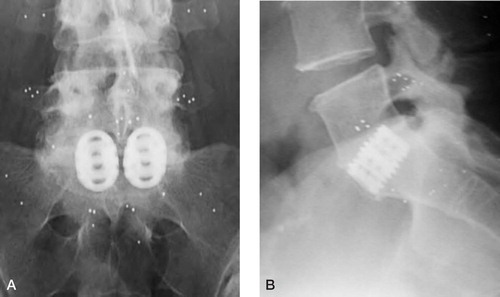
In addition to the preoperative RSA described above, each patient had 3 separate postoperative examinations 1 month, 6 months and one year after surgery. The RSA set-up was identical at all 4 occasions with the patients examined in standardized positions (Axelsson and Karlsson Citation2005). The translatory movements of the vertebra proximal to the cage relative to the vertebra distal to the cage were calculated for this positional change from supine to sitting.
The intervertebral mobility along the x-, y- and z-axis from preoperatively throughout the postoperative course is given in . An immediate stabilization was seen for all five segments as a mobility reduction 1 month after surgery. Minor remaining translations along the z-axis were demonstrated on the L5–S1 level for patient number 2 and 3. One year after surgery, 4 fused levels were fully stable and the only significant mobility registered was a minor sagittal translation, again for patient number 3.
Table 8 :1. Intervertebral mobility (mm) before and through the postoperative course after anterior fusion
This study does not verify a risk of initial destabilization by the anterior interbody fusion as previously described from cadaveric in vitro data. Even though the patient number was small and the loading provocation at RSA was limited, instead favouring standardization, we conclude that the biomechanical effects by the anterior interbody cage stabilization are adequate and a general recommendation to use a supplementary anterior/posterior instrumentation is not relevant. Reported high pseudarthrosis rates (Nilsson et al. Citation2001) and specific complications as postopera-be further clarified in order to evaluate the antetive sexual dysfunction for the anterior procedure rior cage stabilization as instrument in lumbar (Hägg et al. Citation2003) are clinical aspects that must fusion.
9. BMP in lumbar fusion, a comparative randomized study
As stated previously, some advantages with uninstrumented posterolateral fusion can be identified such as lower costs and risks due to the absence of transpedicular implants. Quite a few literature studies demonstrate likeworthy results with instrumented fusions as with uninstrumented (Thomsen et al. Citation1997, Fritzell et al. Citation2002). Drawbacks are a nonunion rate of 10–30% (Seitsalo Citation1990, Frennered et al. Citation1991, Axelsson et al. Citation1994) and as with all bone grafting, the variably occurring problem of donor site pain (Summers and Eisenstein Citation1989, Strömqvist Citation1993). Recently, the characterization and production of osteoinductive proteins has attained significant interest. Animal studies in the 1990s applied to the spine showed very promising results (Cook et al. Citation1994, Boden et al. Citation1995) and some bone morphogenic proteins, such as BMP-1 and BMP-7 were used in pilot studies.
A human RCT comparing the effects of BMP-7 (OP-1, Stryker Biotech, Hopkinton, MA), and conventional autograft was initiated as an efficacy trial for lumbosacral uninstrumented fusion (Johnsson et al. Citation2002). The outcome was evaluated by radiostereometry. The study hypothesis was that the OP1 implant would give faster and better formation of bridging bone than autograft.
In order to standardize the patient material, only patients with symptomatic isthmic spondylolisthesis of the L5, grade 1 and 2, in patients aged more than 20 years were included. The study was approved by the ethics committee and 20 patients were operated on by two experienced spine surgeons. The procedures were identical up to the stage where decortication was performed. At this stage, according to randomization, patients either had conventional autograft harvested through the same incision from the posterior iliac crest or BMP-7. The latter preparation included 3.5 mg of rhOP-1 reconstituted with a carrier consisting of 1 g of type 1 bone collagen and this powder was mixed with 2.5 ml of saline. Two such preparations were made, one for the right and one for the left side, and placed into the same location where the autograft was placed in the control patients. Conventional application of tantalum markers and postoperative treatment with a soft lumbosacral brace for 5 months was instituted. RSA was performed monthly during the first half year and 12 months after surgery. Repeat RSA was performed 5 years later in order to determine the consistency of the fusion. Conventional radiography and clinical assessment also was performed. Accuracy measurement determined similar values as previously.
The velocity of fusion healing did not differ between the two groups according to RSA. At one year after surgery the number of cases showing L5 stabilization relative to the sacrum was similar in the two groups according to the translations along the sagittal axis and for the rotations around the transverse axis. The number of cases with stabilization of the L5 translations along the vertical axis was higher in the autograft group (p = 0.03, Fish-er’s exact test). Two re-operations were performed in the OP-1 group and one in the autograft group. In total 15 of the 20 patients experienced minor or no back pain at one-year follow-up.
At a 5-year RSA follow-up, it was demonstrated that stabilization achieved at one year postoperatively was retained over time.
This study demonstrates that using BMP-7 in the form described above as a substitute for autograft in posterolateral fusion can yield fusion healing () but not to a higher extent than autograft. The preparation has been improved today and is delivered as a putty where improved results have been shown (Vaccaro et al. Citation2005a, b). Mixing of BMP-7 with autograft as well as using bisphosphonates might be ways to improve fusion rates in the future.
10. Orthoses in lumbar fusion
The need for postoperative spinal immobilization to achieve bony consolidation of a lumbar fusion is questioned (Connolly et al. Citation1998). On one hand, support can be found in the literature for the use of a rigid plaster body cast (Stauffer and Coventry Citation1972). On the other hand, bony fusion healing is shown in a high rate even with free postoperative mobilization after posterolateral fusion without internal fixation (Jackson et al. Citation1985).
To determine the influence of spinal immobilization on the consolidation of a lumbar fusion, we compared two consecutive patient series including 11 patients each (Johnsson et al. Citation1992). The diagnosis was spondylolysis with low grade olisthesis in 19 patients and degenerative disc or facet joint disorder in 3 patients. All patients suffered from long-standing low back and/or radiating pain. Posterolateral fusion without internal fixation was performed on the L5–S1 level in 11 cases and on the L4–S1 level in the other 11. This procedure included implantation of tantalum indicators for radiostereometry (RSA) (Selvik Citation1989). The two patient series differed by the postoperative regimen. Patients in Series 1 were treated with a molded, rigid thoracolumbosacral orthosis of TLSO type (Nachemson Citation1987) () for 5 months and were instructed to keep the trunk straight and to avoid all active spinal motions during the same period. Patients in Series 2 used the same orthosis and had the same instructions regarding spinal immobilization but instead for a period of 3 months after surgery. RSA was performed monthly 2-6 months postoperatively and then one year after surgery. The patients were examined without orthosis in a standardized way in supine and erect positions (Johnsson et al. Citation1990). The translatory movements of the most proximal vertebra in the fusion in relation to the sacrum were calculated for this positional change. Fusion consolidation was also assessed by conventional radiography 6 months and one year after surgery.
Figure 10:1 Molded, rigid lumbar orthosis made of light weight material. A. Anteroposterior view. B. Lateral view. (Reproduced with permission from J Spinal Disord).
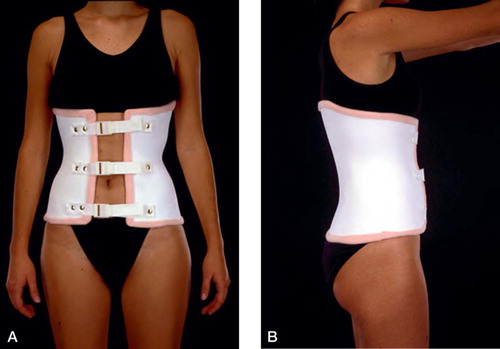
In Series 1, eight patients had osseous fusion healing according to radiography and the stabilizing effect was confirmed by RSA showing decreasing intervertebral translations less than 1 mm 1 year after surgery. For Series 2, a corresponding outcome consistent with a healed fusion was seen only in 2 patients. Definitive pseudarthrosis based on both radiography and RSA was assessed for 3 patients in Series 1 and seven patients in Series 2. In two patients in the latter series, the radiographic and radiostereometric findings were inconclusive and the fusions were classified as doubtful. With these two patients excluded, the healing rate was significantly higher (p<0.05, Fisher exact test) in Series 1 (8 of 11 cases) than in Series 2 (2 of 9 cases).
It seems, for the non-instrumented lumbar fusion, that a postoperative period of 5 months with lumbar immobilization using orthosis is superior in terms of a higher fusion rate compared to the same regimen used only for 3 months. The role of the orthosis in this context is unclear. The orthotic mobility restriction could have two possible effects; restriction of gross body motions reducing the moment load caused by trunk flexion, extension and side bending (Lantz and Schultz Citation1986) and/or restriction of intervertebral segmental mobility. Any such orthotic effect on the segmental mobility, provided by small intervertebral translations, has prior been difficult to assess requiring a measuring method with a very high accuracy. Attempts include the use of Kirschner wires as measuring marks inserted into the spinous processes (Norton and Brown Citation1957, Lumsden and Morris Citation1968). The results indicated very small effects on intersegmental movements using orthosis and a paradoxical increase in lumbosacral mobility was described in some cases (Lumsden and Morris Citation1968). The results were however questioned due to the potential confounding effect of the Kirschner wires passing through the soft tissues, potentially reducing the muscular range of motion.
We applied RSA to determine whether different types of lumbar orthoses affect the intervertebral mobility in the lower spine (Axelsson et al. Citation1992). Seven patients operated on with a non-instrumented lumbar fusion for isthmic spondylolisthesis grade I-II had tantalum markers inserted at the time of fusion. Four fusions were performed between L5 and S1 and three between L4 and S1. One month after surgery, radiostereometry was performed when soft tissue healing was judged to be completed, pain by surgery abolished but stabilization by fusion still not provided. Each patient was examined in three separate situations: 1) without external lumbar support; 2) with a molded, rigid orthosis of TLSO type (Nachemson Citation1987) made of a light weight thermoplastic material (); and 3) with a canvas corset splinted with thin metal ribbons and with a molded posterior plastic reinforcement (). The RSA set-up was identical with the first study on orthoses referred above (Johnsson et al. Citation1992). Thus, each RSA was performed with the patient in supine and erect positions avoiding active spinal movements. The intervertebral translations provided by this positional change were calculated for the most proximal vertebra in the intended fusion relative to sacrum.
Figure 10:2 Lumbar canvas corset with molded plastic posterior support. A. Anteroposterior view. B. Lateral vew. (Reproduced with permission from J Spinal Disord).
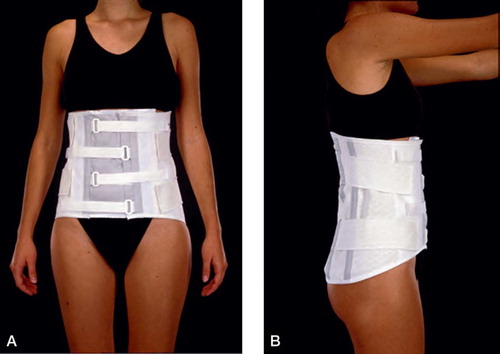
In the seven patients examined neither of the two types of lumbar support had any stabilizing effect on the sagittal or vertical intervertebral translations (). Instead the orthoses, both rigid and soft, tended to increase the translations in six of the patients examined. The mean sagittal translation was 3.8 mm without support, 4.7 mm with the molded rigid orthosis and 5.1 mm with the canvas corset. The corresponding values for vertical translations were 2.3 mm, 2.7 mm and 2.7 mm, respectively. The transverse translations were negligible in all three situations.
Table 10 :1. Clinical data and RSA intervertebral translations of 7 patients with different lumbar support
This paradoxical tendency towards an increase in mobility with orthosis has been previously described (Lumsden and Morris Citation1968) and is assumed to be an unfavourable effect of inadequate pelvic fixation. In a following radiostereometric study (Axelsson et al. Citation1993), a similar comparison as with rigid and soft orthoses was performed but instead in patients wearing an orthosis with a unilateral hip immobilization (). Ten patients with the same diagnosis, spondylolysis/ spondylolisthesis grade 1–2, were included but the placement of the tantalum indicators was suboptimal in one case. Thus, nine patients could be assessed by radiostereometry with and without an orthosis with an extension to one thigh.
Figure 10:3 Molded, rigid lumbar orthosis made of light weight material extended to one thigh immobilizing one hip. A. Anteroposterior view. B. Lateral vew. (Reproduced with permission from Spine).
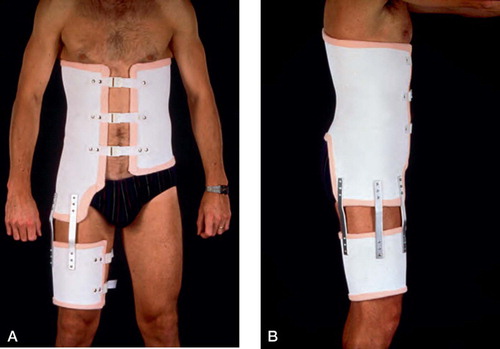
No significant immobilizing effect was registered for the sagittal or vertical intervertebral translations using the orthosis with unilateral hip immobilization (). The tendency towards increased mobility seen for the conventional two orthoses did however disappear. The mean sagittal translation was 2.7 mm with orthosis and 3.5 mm without. The mean vertical translation was 1.5 mm with and without support. Again, the transverse translations were minor and insignificant in both situations measured.
Table 10 :2. Clinical data and RSA intervertebral translations of 9 patients with and without orthosis with unilateral hip immobilization
According to the radiostereometric results, the small intervertebral translations between segments cannot be eliminated or significantly reduced by an external orthosis (Axelsson et al. Citation1992). Hip flexion does provide a great mobility provocation in the lower lumbar spine (Axelsson and Karlsson Citation2005) but an attempt to reduce pelvic motions by extending the orthosis to one thigh did not reduce the translations to an extent justifying the use of such unilateral hip immobilization (Axelsson et al. Citation1993). The positive influence of spinal immobilization on the consolidation of lumbar fusion (Johnsson et al. Citation1992) is thus rather a consequence of reduced gross body motions. We have put that into practice during the postoperative period after uninstrumented fusion and all patients are recommended to avoid active movements of the spine keeping the trunk straight and also avoiding the sitting position with the hips in flexion. A soft orthosis is used as a reminder of this regimen but is not ascribed any stabilizing capacity.
11. Lumbar segmental mobility adjacent to fusion
Progressive disc degeneration, facet joint hypertrophy, spinal stenosis and even acquired spondylolysis are radiographic long term findings () implying an increased load on the spinal segment adjacent to a lumbar fusion (Harris and Wiley Citation1963, Lee Citation1988). The characteristic clinical picture includes a long asymptomatic period after fusion before presenting with recurrent pain (Lee Citation1988, Schlegel et al. Citation1996). It is not fully clarified how often such an unfavourable course is seen for the juxta-fused segment. Treatment by extended fusion is proposed but controversial due to poor clinical outcome and complications (Whitecloud et al. Citation1994).
Figure 11:1 A. Computerized tomography in a patient with relapsing leg pain 12 years after decompression and fusion L4–S1. B. MRI of the same patient reveals a significant spinal stenosis of the segment proximal, adjacent to fusion with a small anterior slip of L3.
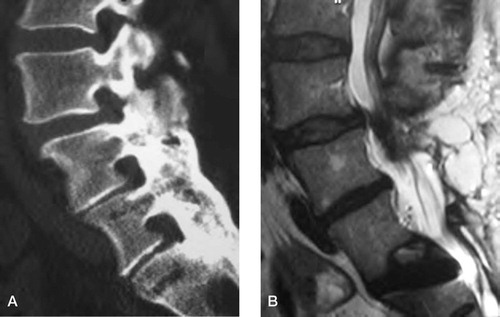
These clinical observations have initiated several biomechanical studies reporting on the loading effects and altered kinematics induced on the juxta-fused segment. In vitro, the intradiscal pressure above a segment fixed by instrumentation is increased in flexion (Weinhoffer et al. Citation1995). Considering kinematics, the center of rotation in flexion was shifted cranially in a study of human cadavers with one lumbar segment stabilized (Lee and Langrana Citation1984).
Radiostereometry (RSA) (Selvik Citation1989) has brought the possibility to study the mobility effects on the segment adjacent to fusion in vivo and over time from preoperatively through the course of fusion consolidation (Axelsson et al. Citation1997). Six patients with spondylolysis of L5, a low grade spondylolisthesis and intractable low back pain with a mean duration of two years had an external test fixation of the lumbosacral segment (Magerl Citation1984, Olerud et al. Citation1986). The diagnosis was based on conventional radiography and no sign of degeneration was seen for the disc above the olisthetic level on preoperative radiographs. The pedicular Schanz screws used for the external fixator and the tantalum skeletal indicators required for radiostereometry were applied with percutaneous technique and under general anesthesia. The tantalum indicators were placed in the spondylolytic L5 vertebra, in the adjacent proximal L4 vertebra and distally in the sacrum using standardized anatomical landmarks (Johnsson et al. Citation1990).
Due to a positive outcome regarding pain relief during temporary fixation, all six patients were scheduled for a fusion of the olisthetic segment. At surgery, the posterolateral parts of L5 and S1 were exposed, decorticated and covered with a cancellous autogenic bone graft from the iliac crest. No internal fixation and no laminectomy was performed. After surgery, all patients were instructed to keep the trunk straight avoiding all movements of the lumbar spine for a period of 5 months. A canvas corset was used for the same period to remind the patient about this regimen.
Each patient had four separate radiostereometric examinations. The first was performed before the fusion but 2 months after completion of the external fixation test. The soft tissues were fully healed at that time and the patients were assumed to have regained their usual lumbar mobility. The three remaining examinations were carried out during the period of fusion consolidation 3, 6 and 12 months after surgery. To be consistent with the postoperative advice to avoid active and passive lumbar movements, the patients were examined in supine and erect positions without active mobility provocation. The translatory movements of the L4 in relation to L5 and L5 in relation to sacrum induced by this positional change, supine to erect, were calculated.
The mean intervertebral translations for the juxta-fused L4–L5 level did not alter throughout the period of fusion consolidation () However, studying individual mobility in the six patients included, three separate patterns were identified. Transformation of preoperative lumbosacral mobility to the L4–L5 segment during fusion consolidation was verified in two patients (cases 2 and 5) (). This pattern is illustrated by the sagittal translations plotted over time for case 2 in . In two patients (cases 3 and 4), the mobility of the segment adjacent to fusion decreased and had almost disappeared up to one year after surgery. This second pattern is exemplified by the sagittal translations of case 4 in For the remaining two patients (cases 1 and 6), the translations of the L4–L5 level were small preoperatively and were not significantly affected by the fusion procedure.
Figure 11:2 Mobility of the L4–L5 and L5–S1 segments for one patient (case 2) representing the pattern with increased mobility of the adjacent segment after fusion. (Reproduced with permission from Spine).
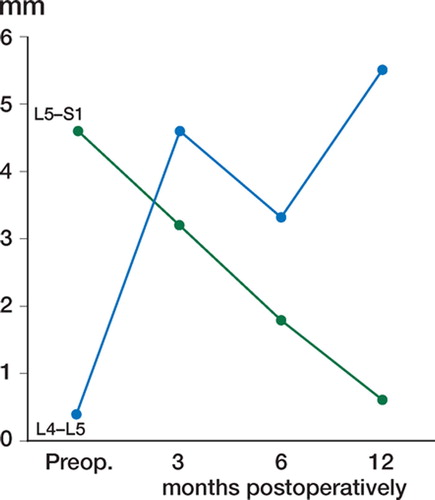
Figure 11:3 Mobility of the L4–L5 and L5–S1 segments for one patient (case 4) representing the pattern with decreased mobility of the adjacent segment after fusion. (Reproduced with permission from Spine).
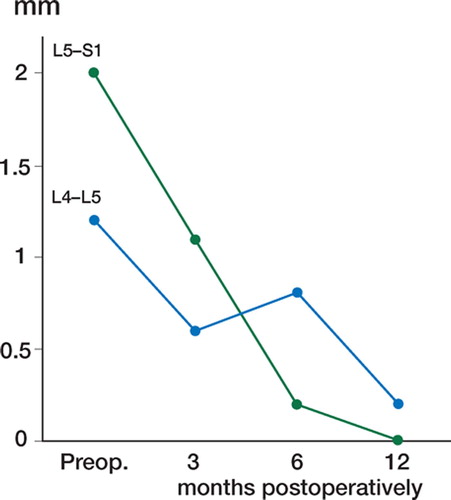
Table 11 :1. RSA intervertebral translations in the adjacent L4–L5 segment for six patients before and after posterolateral lumbosacral fusion
These radiostereometric results confirm the clinical impression that stabilizing one lumbar segment can, although this is not a general phenomenon, increase the load on the adjacent segment by altering the kinematics redistributing the mobility towards a situation of relative hypermohand, decreased mobility of the segment adjacent to fusion was also identified as a mobility pattern during the postoperative course. This stabilizing effect might be explained by the fact that the fusion procedure with decortication of the superior articular process is performed in close relation to the L4–L5 facet joint. The clinical consequence of this second mobility pattern might instead be an overload for the segment adjacent to the juxta-fused segment. It is an interesting fact that degeneration is seen equally often for these two segments in clinical practice (Schlegel et al. Citation1996). With a protracted radiostereometric follow-up in extended patient series we hope to clarify whether the different mobility patterns identified here affect the long term complications described for the segments adjacent to fusion.
12. Discussion
Disregarding tumors, fractures and infections, the incidence of lumbar spine disorders has probably not increased over the years whereas disability due to these disorders is much more prevalent. These disorders, generally described as degenerative, are the focus of immense research activities today and our knowledge on etiology, for example inflammatory aspects (disc herniation, arthritic conditions) and genetic aspects (congenital stenosis, disc degeneration) are significant. Further, psychological and psychosocial aspects as well as coping strategies affect the disability resulting from lumbar spine disorders to a high extent. Still, lumbar spine symptoms relate to lumbar spine kinematics and significant efforts have been put into the study of spinal mobility in normal and pathological conditions described in the introduction. The complexity of demands on the spine combining flexibility and stability, and the very high loads noted in different positions of off-center mobility, are most likely the explanations for pain emanating from the spine. This is even more evident in the limited number of lumbar spine disorders treated surgically.
Radiostereometry (RSA) as described by Selvik (Citation1976, Citation1989) is a technique of studying skeletal kinematics in different body positions or over time with a high accuracy. Among many applications for the method, the studies of prosthetic fixation in the hip and knee have provided significant contributions to orthopedics. In the lumbar spine, mobility measurement with external devices or using radiography have been demonstrated to be very imprecise. Therefore the potential of RSA is obvious and was explored for the first time by Olsson et al. (Citation1976a, Citationb). This work inspired us to use the technique in the multiple clinical situations described in this supplementum. The main fields of study have concerned the mobility of normal and abnormal lumbar segments, the effects of temporary spine fixation (orthosis and external pedicular fixation), the kinematics of different types of spinal fusion and the effect of fusion on the adjacent segment.
Kinematics in normal and degenerative lumbar segments as well as spondylolisthetic segments have been studied after acceptance of the individual patients and the ethical committee of our university. The mobility pattern related to the degree of disc degeneration showed that a stage of stabilization with decreased mobility is seen for spinal segments with disc height reduced by at least 50 % (Axelsson and Karlsson Citation2004). An intermediate stage of instability/hyper mobility such as proposed by Kirkaldy-Willis and Farfan (Citation1982) could not be verified. The same was true for segments with isthmic spondylolisthesis, i.e. no hypermobility could be demonstrated in adult symptomatic patients with a low-grade slip (Axelsson et al. Citation2000). Instead, very pronounced interindividual differences were seen regarding mobility of normal as well as degenerated segments. According to our findings, patients who experience symptoms mimicking instability such as the instability catch, sudden stabbing pain or giving away on weight bearing do not suffer segmental instability. Instead these patients probably express painful mobility as part of the degenerative process and why this occurs in some cases, whereas the majority of humans undergoing disc degeneration over life are asymptomatic, remains unclear.
Fusion of the lumbar spine accounts for a rather small fraction of the total number of surgical procedures for degenerative disorders (Strömqvist et al. Citation2005) but the debate over indications and type of fusion to be performed is intense especially in degenerative disc disease, DDD. Non-instru-mented lumbar fusion has been performed since the beginning of the last century but with gradually improved technique. The appearance of transpedicular implant systems gave a more immediate stability to the segment but at the cost of an increased complication rate and also an economical cost. Interbody fusions with and without implants, stand alone or combined with posterior instrumentation, are used today and no consensus exists on which method is the best. In some recent studies on fusion for DDD (Fischgrund et al. Citation1997, Thomsen et al. Citation1997, Fritzell et al. Citation2002), benefits of adding instrumentation to the fusion procedure have not been possible to demonstrate. The debate goes on and the recent introduction of disc arthroplasty as a treatment modality for this patient group further alters the situation. Possibly, individual, patient related factors should be taken into consideration when choosing type of surgery.
Posterolateral uninstrumented fusion for isthmic spondylolisthesis or DDD is, according to radiostereometry, a very slowly stabilizing process with the majority of patients going on to fusion still having some degree of mobility persisting even 6 months after surgery. This has to be considered when selecting the adequate aftertreatment. Instrumented posterolateral fusion seems to give immediate stabilization of the spinal segment in the inherently stable spine. The healing time for an instrumented fusion in a more unstable situation is long and additional anterior stabilization can be justified in such cases. The possibility of the disc as a pain generator in a solid fusion has been proposed but this indication for concomitant interbody fusion so far remains to be proven and must be questioned.
Interbody fusions can be performed as bone graft procedures only, or supplemented with cages or ramps. The surgical approach can be retroperitoneal and anterior (ALIF) or from the posterior route (PLIF or TLIF). These procedures normally give immediate stability at the cost of an increased complication rate. Whether this is reflected in a higher fusion rate or not is debated. ALIF with and without titanium cages has been demonstrated to be afflicted with a risk for non-union and also for some subsidence during the healing procedure. Our material of ALIF, supplemented with BAK-cages, confirms immediate stability in most cases and the technique seems to be a valid treatment alternative in patients with good bone quality, especially in females.
Fusion promoters have been described in an increasing number during the last 10 years and hopefully will increase our ability to achieve a high fusion rate. In the RSA study presented, a fusion rate of uninstrumented fusion could be obtained with BMP-7 only that was fully comparable to conventional uninstrumented fusion with bone graft from the iliac crest. A long-term followup of this patient group shows that the stability achieved does not deteriorate over time. However, non-unions are seen in the patient material. In the event of forming stable bridging bone in a bone transplant, different bone morphogenetic proteins are active in different time periods in a cascade reaction and perhaps other preparations (Barnes et al. Citation2005, Vaccaro et al. Citation2005a, Citationb) and other bone formation promoters (Boden et al. Citation2002) can bring further improvement.
Whether or not the use of an orthosis after fusion surgery is beneficial is not obvious (Jackson et al. Citation1985, Connolly et al. Citation1998) and clinical practice concerning the use, type and timing of orthosis wearing is most variable over the world. The stabilizing ability of an orthosis, whether soft, rigid or supplemented with hip immobilization, is minor or even absent when assessed as intervertebral mobility reduction. In non-instrumented lumbosacral fusion, however, postoperative corset wearing for 5 months yielded a lower non-union rate than orthosis wearing for 3 months. In spite of the inability of the orthosis to immobilize lumbar segments, uninstrumented fusions probably should be treated with bracing for 5 months instead of 3. This effect is then rather induced by restricting gross body motions and making the patient aware of keeping the spine straight during the healing process. Whether a postoperative orthosis is beneficial in instrumented fusion has not been studied.
The indication for fusion of disc degenerative disease, DDD, is questioned. Degenerated discs on plain radiographs or MRI are present in most people after 40 years of age and are frequent in asymptomatics also during the preceding decades. However, there seems to be a clear clinical picture of segmental pain from degenerated discs and recent studies on inflammatory reactions seem to corroborate this hypothesis (Schwarzer et al. Citation1995, Peng et al. Citation2006). Therefore, the identification of painful segments in patients with long-lasting low back pain expected to improve by segmental fusion, is focus of broad clinical research. Recent RCTs have shown conflicting results. In a Swedish multicenter study, the 2-year outcome of fused patients was significantly better than in patients treated with nonspecific physiotherapy (Fritzell et al. Citation2001) with a patient satisfaction rate at two years of 63% and 29%, respectively. Similar studies comparing fusion to cognitive therapy show more questionable results (Brox et al. Citation2003, Fairbank et al. Citation2005). The basic idea, to identify the symptomatic segment and to prognosticate the outcome of fusion, has been pursued by clinical examination, facet joint blocks, disc blocks and also by the external test fixation as described by Magerl (Citation1984). The external fixator theoretically mimics the fusion procedure giving the patient a possibility to anticipate what the outcome of a fusion will be. The method requires the insertion of pedicular screws which is an invasive procedure and complications are reported. Therefore it is important to assess whether the mechanical basis is adequate in the form of stabilization to the segment with the external frame placed outside the body. The RSA study showed good reduction of segmental motion and on removal of the frame, retaining the screws in place, mobility was regained. The dynamics of the external fixator thereby provides an adequate mechanical basis for the prognostication of a definitive bony fusion. In a subsequent uncontrolled clinical study (Axelsson et al. Citation2003), the satisfaction rate after fusion was 75% in patients all having a positive outcome at preoperative test fixation. The ideal study, to perform the external test fixation and then, irrespective of test result, continue with fusion relating the outcome of fusion to the outcome of test fixation, cannot for ethical reasons be justified.
Potential negative effects of a lumbar fusion on the adjacent spinal segment has been a focus of many studies, taking into consideration the alteration of kinematics induced for the juxta-fused segment. Recurrent symptoms after a painfree period are often ascribed to progressive degeneration of the juxta-fused segment but whether this finding is elicited by the fusion as such or if the patient is predisposed to degeneration generally, which is a reasonable presumption, is not clear. In two of the patients in the RSA study, an obvious increase in mobility of the L4–L5 segment was verified seen at three months postoperatively and persisting after fusion healing. This corroborates with the cadaver study of Lee and Langrana (Citation1984) demonstrating that the center of rotation in flexion shifts cranially with the stabilization of one lumbar segment. It is plausible to postulate that this is more likely to occur in the subgroup of patients with pronounced lumbar segmental mobility such as demonstrated in the first study of normal segments. Whether juxtafused hypermobility, verified by RSA, predisposes for late adjacent segment degeneration will be one of many future issues in which radiostereometry can contribute in spinal research.
Other radiostereometric applications in the lumbar (Halldin et al. Citation2005) and cervical (Zoega et al. Citation2003) spine have been explored and, in the probably upcoming era of disc arthroplasty, RSA will be a useful means to demonstrate in vivo kinematics.
13. Conclusions
Radiostereometry can demonstrate lumbar spine kinematics with a high accuracy, 0.2–0.7 mm, along the three axes of movement or 0.5–2,0° along the axes of rotation.
Radiostereometry is invasive, time consuming and expensive and suitable for focused studies.
The range of intervertebral mobility over normal, non-degenerated discs differs widely between individuals.
In the progressive degenerative process, a stage of stabilization begins when the disc height is reduced by at least 50 % but, in the clinical situation, stability cannot be taken for granted even with such disc height reduction.
The spondylolytic segment is not hypermobile/ unstable in the adult, symptomatic patient with a low-grade olisthesis. The back pain is rather a manifestation of degeneration of the disc below the slipped vertebra.
The external pedicular fixator can immobilize a lumbar spine segment more or less totally and mobility is regained immediately when the frame is unlocked with the pedicular Schanz screws retained.
The uninstrumented lumbar fusion stabilizes the segment very slowly and some mobility often remains after 6 months in fusions stable at 12 months.
By adding posterior instrumentation to a postero lateral fusion in DDD or spondylolysis/olisthe-sis, immediate stabilization is provided except when the surgery includes broad decompression with facet joint resection.
Transarticular fixation of facet joints with biodegradable rods is not a valid method in terms of stabilization and has no consistent influence on the consolidation of a posterolateral fusion.
Anterior interbody fusion with cages as a standalone procedure may provide an immediate segmental stabilization and a general recommendation to use a supplementary instrumentation is not motivated.
BMP-7 can give as high a fusion rate as autogenic iliac crest graft.
Neither a soft, stiff or hip joint immobilizing orthosis provides lumbar spine stabilization assessed as reduction of intervertebral segmental mobility.
A postoperative period of 5 months in orthosis after non-instrumented fusion is superior in terms of a higher fusion rate compared to the same regimen for 3 months, which most likely is an effect of the restricted gross body motions during the period.
Fusion of one lumbar segment may, although this is not a general phenomenon, alter the kinematics of the juxta-fused segment into a situation of relative hypermobility.
14. Acknowledgements
We wish to express our sincere gratitude to Håkan Leijon, engineer and RSA technician, for data processing the RSA material in all the studies from our department referred to in this text book. The secretarial work by Lena Oreby is highly appeciated. Economic support was given by Stiftelsen för bistånd åt rörelsehindrade i Skåne, Medical Faculty, Lund University and Swedish Research Council – Medicine (09509).
References
- Albrektsson B E, Ryd L, Carlsson L V, Freeman M A, Herberts P, Regner L, Selvik G. The effect of a stem on the tibial component of knee arthroplasty. A roentgen stereophotogrammetric study of uncemented tibial components in the Freeman-Samuelson knee arthroplasty. J Bone Joint Surg (Br) 1990; 72: 252–8
- Axelsson P, Johnsson R, Strömqvist B. Effect of lumbar orthosis on intervertebral mobility. A roentgen stereophotogrammetric analysis. Spine 1992; 17: 678–81
- Axelsson P, Johnsson R, Strömqvist B. Lumbar orthosis with unilateral hip immobilization. Effect on intervertebral mobility determined by roentgen stereophotogrammetric analysis. Spine 1993; 18: 876–9
- Axelsson P, Johnsson R, Strömqvist B. Mechanics of the external fixation test in the lumbar spine. A roentgen stereophotogrammetric analysis. Spine 1996; 21: 330–3
- Axelsson P, Johnsson R, Strömqvist B. The spondylolytic vertebra and its adjacent segment. Mobility measured before and after posterolateral fusion. Spine 1997; 22: 414–7
- Axelsson P, Johnsson R, Strömqvist B. Is there increased intervertebral mobility in isthmic adult spondylolisthesis? A matched comparative study using roentgen stereophotogrammetry. Spine 2000; 25: 1701–3
- Axelsson P, Johnsson R, Strömqvist B, Andréasson H. Temporary external pedicular fixation versus definitive bony fusion: a prospective comparative study on pain relief and function. Eur Spine J 2003; 12: 41–7
- Axelsson P, Johnsson R, Strömqvist B, Arvidsson M, Herrlin K. Posterolateral lumbar fusion. Outcome of 71 consecutive operations after 4 (2–7) years. Acta Orthop Scand 1994; 65: 309–14
- Axelsson P, Karlsson B S. Intervertebral mobility in the progressive degenerative process. A radiostereometric analysis. Eur Spine J 2004; 13: 567–72
- Axelsson P, Karlsson B S. Standardized provocation of lumbar spine mobility. Three methods compared by radiostereometric analysis. Spine 2005; 30: 792–7
- Baldursson H, Hansson L I, Olsson T H, Selvik G. Migration of the acetabular socket after total hip replacement determined by roentgen-stereophotogrammetry. Acta Orthop Scand 1980; 51: 535–40
- Barnes B, Boden S D, Louis-Ugbo J, Tomak P R, Park J S, Park M S, Minamide A. Lower dose of rhBMP-2 achieves spine fusion when combined with an osteoconductive bulking agent in non-human primates. Spine 2005; 30: 1127–33
- Bednar D A, Raducan V. External spinal skeletal fixation in the management of back pain. Clin Orthop. 1996; 322: 131–9
- Boden S D, Schimandle J H, Hutton W C. Lumbar intertrans-verse-process spinal arthrodesis with use of a bovine bone-derivated osteoinductive protein. A preliminary report. J Bone Joint Surg (Am) 1995; 77A: 1404–17
- Boden S D, Kang J, Sandhu H, Heller J G. Use of recombinant human bone morphogenetic protein-2 to achieve posterolateral lumbar spine fusion in humans: a prospective, randomized clinical pilot trial: 2002 Volvo Award in clinical studies. Spine 2002; 27: 2662–73
- Brox J I, Sorensen R, Friis A, Nygaard O, Indahl A, Keller A, Ingebrigtsen T, Eriksen H R, Holm I, Koller A K, Riise R, Reikeras O. Randomized clinical trial of lumbar instrumented fusion and cognitive intervention and exercises in patients with chronic low back pain and disc degeneration. Spine 2003; 28: 1913–21
- Bylander B, Hansson L I, Selvik G. Pattern of growth retardation after Blount stapling: a roentgen stereophotogrammetric analysis. J Pediatr Orthop. 1983; 3: 63–72
- Connolly P J, Grob D. Controversy. Bracing of patients after fusion for degenerative problems of the lumbar spine – yes or no?. Spine 1998; 23: 1426–8
- Cook S D, Baffes G C, Wolfe M W, Sampath T K, Rueger D C, Whitecloud TS III. The effect of recombinant human osteogenic protein-1 on healing of large segmental bone defects. J Bone Joint Surg (Am) 1994; 76A: 827–38
- Danielsson B, Frennered K, Irstam L. Roentgenologic assessment of spondylolisthesis. I. A study of measurement variations. Acta Radiol 1988; 29: 345–51
- Debrunner H U. Das Kyphometer. Z Orthop 1972; 110: 389–92
- Dekutoski M B, Schemdel M J, Ogilvie J W, Olsewski J M, Wallace L J, Lewis J L. Comparison of in vivo and in vitro adjacent segment motion after lumbar fusion. Spine 1994; 19: 1745–51
- Egund N, Olsson T H, Scmid H, Selvik G. Movements in the sacroiliac joints demonstrated with roentgen-stereo-photogrammetry. Acta Radiol (Diagn) (Stockh) 1978; 19: 833–46
- Ekman P, Möller H, Hedlund R. The long-term effect of posterolateral fusion in adult isthmic spondylolisthesis: a randomized controlled study. Spine J 2005; 5: 36–44
- Esses S I, Botsford D J, Kostuik J P. The role of external spinal skeletal fixation in the assessment of low-back disorders. Spine 1989; 14: 594–601
- Fairbank J, Frost H, Wilson-MacDonald J, Yu L M, Barker K, Collins R;. Spine Stabilisation Trial Group. Randomised controlled trial to compare surgical stabilisation of the lumbar spine with an intensive rehabilitation programme for patients with chronic low back pain: the MRC spine stabilisation trial. BMJ 2005; 330: 1233, Epub May 23
- Fischgrund J S, Mackay M, Herkowitz H N, Brower R, Montgomery D M, Kurz L T. 1997 Volvo Award winner in clinical studies. Degenerative lumbar spondylolisthesis with spinal stenosis: a prospective, randomized study comparing decompressive laminectomy and arthrodesis with and without spinal instrumentation. Spine 1997; 22: 2807–12
- Frennered A K, Danielson B I, Nachemson A L, Nordwall A B. Midterm follow-up of young patients fused in situ for spondylolisthesis. Spine 1991; 16: 409–16
- Friberg O. Lumbar instability: A dynamic approach by traction-compression radiography. Spine 1987; 12: 119–29
- Fritzell P, Hägg O, Nordwall A. Complications in lumbar fusion surgery for chronic low back pain: comparison of three surgical techniques used in a prospective randomized study. A report from the Swedish Lumbar Spine Study Group. Eur Spine J 2003; 12: 178–89
- Fritzell P, Hägg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish Lumbar Spine Study Group. Spine 2002; 27: 1131–41
- Fritzell P, Hägg O, Wessberg P, Nordwall A. 2001 Volvo Award winner in clinical studies. Lumbar fusion versus nonsurgical treatment for chronic low back pain: a multicenter randomized controlled trial from the Swedish Lumbar Spine Study Group. Spine 2001; 26: 2521–32
- Frobin W, Brinckmann P, Biggemann M, Tillotson M, Burton K. Precision measurement of disc height, vertebral height and sagittal plane displacement from lateral radiographic views of the lumbar spine. Clin Biomech 1997; 12(Suppl)S1–63
- Frobin W, Brinckmann P, Leivseth G, Biggemann M, Reikerås O. Precision measurement of segmental motion from flexion-extension radiographs of the lumbar spine. Clin Biomech 1996; 11: 457–65
- Frymoyer J W, Selby D K. Segmental instability. Rationale for treatment. Spine 1985; 10: 280–6
- Gunnarsson G, Axelsson P, Johnsson R, Strömqvist B. A method to evaluate the in vivo behaviour of lumbar spine implants. Eur Spine J 2000; 9: 230–4
- Halldin K, Zoega B, Nyberg P, Kärrholm J, Lind BI. The effect of standard lumbar discectomy on segmental motion: 5-year follow-up using radiostereometry. Int Orthop 2005; 29: 83–7
- Hambly M F, Wiltse L L, Raghavan N, Schneiderman G, Koenig C. The transition zone above a lumbosacral fusion. Spine 1998; 23: 1785–92
- Hanley E N, Matteri R E, Frymoyer J W. Accurate roentgenographic determination of lumbar flexion-extension. Clin Orthop Relat Res 1976, 115: 145–56
- Harris R I, Wiley J J. Acquired spondylolysis as a sequel to spine fusion. J Bone Joint Surg (Am) 1963; 45: 1159–70
- Hunter L Y, Braunstein E M, Bailey R W. Radiographic changes following anterior cervical fusion. Spine 1980; 5: 399–401
- Hägg O, Fritzell P. Nordwall A and the Swedish Lumbar Spine Study Group. Sexual function after surgery for chronic low back pain. Eur Spine J 2003; 12(Suppl 1)S17–S18
- Hägglund G, Bylander B, Hansson L I, Kärrholm J, Selvik G, Svensson K. Longitudinal growth of the distal fibula in children with slipped capital femoral epiphysis. J Pediatr Orthop 1986; 6: 274–7
- Jackson R K, Boston D A, Edge A J. Lateral mass fusion: A prospective study of a consecutive series with long-term follow-up. Spine 1985; 10: 828–32
- Jeanneret B, Jovanovic M, Magerl F. Percutaneous diagnostic stabilization for low back pain. Correlation with results after fusion operations. Clin Orthop. 1994; 304: 130–8
- Johnsson R, Axelsson P, Branth B, Jönsson B, Strömqvist B, Tullberg T. Interbody stability following anterior lumbar fusion with BAK cages evaluated by RSA. Read at the 26th Annual Meeting of the International Society for the Study of the Lumbar Spine, Kona, Hawaii, 1999a
- Johnsson R, Axelsson P, Gunnarsson G, Strömqvist B. Stability of lumbar fusion with transpedicular fixation determined by roentgen stereophotogrammetric analysis. Spine 1999b; 24: 687–90
- Johnsson R, Axelsson P, Strömqvist B. Posterolateral lumbar fusion using facet joint fixation with biodegradable rods: a pilot study. Eur Spine J 1997; 6: 144–8
- Johnsson R, Selvik G, Strömqvist B, Sundén G. Mobility of the lower lumbar spine after posterolateral fusion determined by roentgen stereophotogrammetric analysis. Spine 1990; 15: 347–50
- Johnsson R, Strömqvist B, Aspenberg P. Randomized radiostereometric study comparing osteogenic protein-1 (BMP-7) and autograft bone in human noninstrumented posterolateral lumbar fusion. Spine 2002; 27: 2654–61
- Johnsson R, Strömqvist B, Axelsson P, Selvik G. Influence of spinal immobilization on consolidation of posterolateral lumbosacral fusion. A roentgen stereophotogrammetric and radiographic analysis. Spine 1992; 17: 16–21
- Kirkaldy-Willis W H, Farfan H F. Instability of the lumbar spine. Clin Orthop 1982; 165: 110–23
- Knutsson F. The instability associated with disk degeneration in the lumbar spine. Acta Radiol 1944; 25: 593–609
- Kärrholm J. Roentgen stereophotogrammetry. Review of orthopaedic applications. Acta Orthop Scand 1989; 60: 491–503
- Kärrholm J, Hansson L I, Selvik G. Roentgen stereophotogrammetric analysis of growth pattern after supinationadduction ankle injuries in children. J Pediatr Orthop 1982; 2: 271–9
- Lantz S A, Schultz A B. Lumbar spine orthosis wearing. 1. Restriction of gross body motions. Spine 1986; 11: 834–7
- Lee C K. Accelerated degeneration of the segment adjacent to a lumbar fusion. Spine 1988; 13: 375–7
- Lee C K, Langrana N A. Lumbosacral spinal fusion. A biomechanical study. Spine 1984; 9: 574–81
- Leivseth G, Brinckmann P, Frobin W, Johnsson R, Strömqvist B. Assessment of sagittal plane segmental motion in the lumbar spine. A comparison between distortion-com-pensated and stereophotogrammetric Roentgen analysis. Spine 1998; 23: 2648–55
- Lumsden R M, Morris J M. An in vivo study of axial rotation and immobilization at the lumbosacral joint. J Bone Joint Surg 1968; 50A: 1591–1602
- Lund T, Nydegger Schlenzka D, Oxland T R. Three-dimensional motion patterns during active bending in patients with chronic low back pain. Spine 2002; 27: 1865–74
- Lund T, Rathonyi G, Schlenzka D, Oxland T R. The external spinal fixator does not reduce anterior column motion under axial compressive loads. A mechanical in vitro study. Acta Orthop Scand 1999; 70: 37–41
- Magerl F P. Stabilization of the lower thoracic and lumbar spine with external skeletal fixation. Clin Orthop 1984; 189: 125–41
- Magyar G, Toksvig-Larsen S, Lindstrand A. Changes in osseous correction after proximal tibial osteotomy: radiostereometry of closed- and open-wedge osteotomy in 33 patients. Acta Orthop Scand 1999; 70: 473–7
- Mjöberg B, Brismar J, Hansson L I, Pettersson H, Selvik G, Önnerfält R. Definition of endoprosthetic loosening. Comparison of arthrography, scintigraphy and roentgenstereophotogrammetry in prosthetic hips. Acta Orthop Scand 1985; 56: 469–73
- Mjöberg B, Hansson L I, Selvik G. Instability, migration and laxity of total hip prostheses. A roentgen stereophotogrammetric study. Acta Orthop Scand 1984; 55: 141–5
- Möller H, Hedlund R. Instrumented and noninstrumented posterolateral fusion in adult spondylolisthesis. A prospective randomized study: part 2. Spine 2000; 25: 1716–21
- Nachemson A L. Orthotic treatment for injuries and diseases of the spinal column. Physical Medicine and Rehabilitation 1987; 1: 11–24
- Nilsson K G, Kärrholm J, Ekelund L. Knee motion in total knee arthroplasty. A roentgen stereophotogrammetric analysis of the kinematics of the Tricon-M knee prosthesis. Clin Orthop Rel Res 1990, 256: 147–61
- Nilsson L T, Geijer M, Neumann P, Lind B. The Brantigan anterior lumbar I/F cage. Two years radiological results. Eur Spine J 2001; 10(Suppl 1)S26
- Norton P L, Brown T. The immobilizing efficiency of back braces. Their effect on the posture and motion of the lumbosacral spine. J Bone Joint Surg (Am) 1957; 39: 111–39
- Olerud S, Sjöström L, Karlström G, Hamberg M. Spontaneous effect of increased stability of the lower lumbar spine in cases of severe chronic back pain. The answer of an external transpeduncular fixation test. Clin Orthop 1986; 203: 67–74
- Olsson T H, Selvik G, Willner S. Kinematic analysis of posterolateral fusion in the lumbosacral spine. Acta Radiol (Diagn) (Stockh) 1976a; 17: 519–30
- Olsson T H, Selvik G, Willner S. Vertebral motion in spondylolisthesis. Acta Radiol (Diagn) (Stockh) 1976b; 17: 861–8
- Olsson T H, Selvik G, Willner S. Postoperative kinematics in structural scoliosis. Acta Radiol (Diagn) (Stockh) 1977; 18: 75–86
- Oxland T R, Lund T. Biomechanics of stand-alone cages and cages in combination with posterior fixation: a literature review. Eur Spine J 2000; 9(Suppl 1)S95–S101
- Pearcy M J. Stereo radiography of lumbar spine motion. Acta Orthop Scand 1985; 56(Suppl 212)1–45
- Peng B, Hao J, Hou S, Wu W, Jiang D, Fu X, Yang Y. Possible pathogenesis of painful intervertebral disc degeneration. Spine 2006; 31: 560–6
- Pope M H, Hanley E N, Matteri R E, Wilder D G, Frymoyer J W. Measurement of intervertebral disc space height. Spine 1977; 2: 282–6
- Rune B, Sarnäs KV, Selvik G, Jacobsson S. Movement of the cleft maxilla in infants relative to the frontal bone. A roentgen-stereophotogrammetric study with the aid of metallic implants. Cleft Palate J 1980; 17: 155–74
- Rune B, Sarnäs KV, Selvik G, Jacobsson S. Roentgen-ste-reometry in the study of craniofacial anomalies –the state of the art in Sweden. Br J Orthod 1986; 13: 151–7
- Ryd L, Albrektsson B E, Carlsson L, Dansgård F, Herberts P, Lindstrand A, Regner L, Toksvig-Larsen S. Roentgen stereophotogrammetric analysis as a predictor of mechanical loosening of knee prostheses. J Bone Joint Surg (Br) 1995; 77: 377–83
- Saraste H, Broström LA, Aparisi T, Axdorph G. Radiographic measurement of the lumbar spine. A clinical and experimental study in man. Spine 1985; 10: 236–41
- Schlegel J D, Smith J A, Schleusener R L. Lumbar motion segment pathology adjacent to thoracolumbar, lumbar, and lumbosacral fusions. Spine 1996; 21: 970–81
- Schläpfer F, Wörsdörfer O, Magerl F, Perren S M. Stabilization of the lower thoracic and lumbar spine: Comparative in vitro investigation of an external skeletal and various internal fixation devices. Uhthoff HK. Springer Verlag, Berlin 1982; 367–80, Current concepts of external fixation of fractures
- Schober P. Lendenwirbelsäule und Kreuzschmerzen. Münch Med Wschr 1937; 84: 336–8
- Schwarzer A C, Aprill C N, Derby R, Fortin J, Kine G, Bogduk N. The prevalence and clinical features of internal disc disruption in patients with chronic low back pain. Spine 1995; 20: 1878–83
- Seitsalo S. Operative and conservative treatment of moderate spondylolisthesis in young patients. J Bone Joint Surg (Br) 1990; 72B: 908–13
- Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. Acta Orthop Scand 1989; 60(Suppl 232)1–51
- Selvik G. Roentgen stereophotogrammetry. A method for the study of the kinematics of the skeletal system. University of Lund. 1976, Thesis
- Snorrason F, Kärrholm J. Primary migration of fully-threaded acetabular prostheses. A roentgen stereophotogrammetric analysis. J Bone Joint Surg (Br) 1990; 72: 647–52
- Soini J, Slätis P, Kannisto M, Sandelin J. External transpedicular fixation test of the lumbar spine correlates with the outcome of subsequent lumbar fusion. Clin Orthop 1993; 293: 89–96
- Stauffer R N, Coventry M B. Posterolateral lumbar-spine fusion: Analysis of Mayo clinic series. J Bone Joint Surg 1972; 54A: 1195–1204
- Strömqvist B. Posterolateral uninstrumented fusion. Acta Orthop Scand 1993; 64(Suppl 251)97–9
- Strömqvist B, Fritzell P, Hägg O. One-year report from the Swedish National Spine Register. Swedish Society of Spinal Surgeons. Acta Orthop 2005; 76(Suppl 319)1–24
- Sturesson B, Udén A, Vleeming A. A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test. Spine 2000; 25: 364–8
- Summers B N, Eisenstein S M. Donor site pain from the ilium. A complication of lumbar spine fusion. J Bone Joint Surg (Br) 1989; 71B: 677
- Szypryt E P, Twining P, Mulholland R C, Worthington B S. The prevalence of disc degeneration associated with neural arch defects of the lumbar spine assessed by magnetic resonance imaging. Spine 1989; 14: 977–81
- Thomsen K, Christensen F B, Eiskjaer S P, Hansen E S, Fruensgaard S, Bunger C E. 1997 Volvo Award winner in clinical studies. The effect of pedicle screw instrumentation on functional outcome and fusion rates in posterolateral lumbar spinal fusion: a prospective, randomized clinical study. Spine 1997; 22: 2813–22
- Tjörnstrand B, Selvik G, Egund N. Lindstrand A. Roentgenstereophotogrammetry in high tibial osteotomy for gonarthrosis. Arch Orthop Trauma Surg 1981; 99: 73–81
- Vaccaro A R, Anderson D G, Patel T, Fischgrund J, Truumees E, Herkowitz H N, Phillips F, Hilibrand A, Albert T J, Wetzel T, McCulloch JA. Comparison of OP-1 Putty (rhBMP-7) to iliac crest autograft for posterolateral lumbar arthrodesis: a minimum 2-year follow-up pilot study. Spine 2005a; 30: 2709–16
- Vaccaro A R, Patel T, Fischgrund J, Anderson D G, Truumees E, Herkowitz H, Phillips F, Hilibrand A, Albert T J. A 2-year follow-up pilot study evaluating the safety and efficacy of OP-1 Putty (rhBMP-7) as an adjunct to iliac crest autograft in posterolateral lumbar fusions. Eur Spine J 2005b; 14: 623–9
- Vainionpää S, Kilpikari J, Laiho J, Helevirta P, Rokkanen P, Törmälä P. Strength and strength retention in vitro, of absorbable, selfreinforced polyglycolide (PGA) rods for fracture fixation. Biomaterials 1987; 8: 46–8
- Vishteh A G, Crawford N R, Chamberlain R H, Thramann J J, Park S C, Craigo J B, Sonntag V K.H, Dickman C A. Biomechanical comparison of anterior versus posterior lumbar threaded interbody fusion cages. Spine 2005; 30: 302–10
- Walheim G G, Selvik G. Mobility of the pubic symphysis. In vivo measurements with an electro-mechanic method and a roentgen-stereophotogrammetric method. Clin Orthop 1984, 191: 129–35
- Weinhoffer S L, Guyer R D, Herbert M, Griffith S L. Intradiscal pressure measurements above an instrumented fusion. A cadaveric study. Spine 1995; 20: 526–31
- Whitecloud III TS, Davis J M, Olive P M. Operative treatment of the degenerated segment adjacent to a lumbar fusion. Spine 1994; 19: 531–6
- Zdeblick T A. A prospective, randomized study of lumbar fusion. Preliminary results. Spine 1993; 18: 983–91
- Zoega B, Kärrholm J, Lind B. Mobility provocation radiostereometry in anterior cervical spine fusions. Eur Spine J 2003; 12: 631–6
- Öhlén G. Spinal sagittal configuration and mobility. A kyphometer study. 1989, Thesis, Department of Orthopaedic Surgery, Karolinska Institute, Stockholm
- Öhlén G, Spangfort E, Tingvall C. Measurement of spinal sagittal configuration and mobility with Debrunner’s kyphometer. Spine 1989; 14: 580–3