Supervisors
Kjeld Søballe, Professor, MD, DMSc
Department of Orthopaedics
Aarhus University Hospital, Denmark
Jens Randel Nyengaard, Associate Professor, MD, DMSc
Stereology and EM Laboratory
Aarhus University, Denmark
Søren Kold, MD, PhD
Department of Orthopaedics
Aarhus University Hospital, Denmark
Evaluation committee
Bjarne Møller-Madsen, MD, DMSc
Sector for Children's Orthopaedics
Aarhus University Hospital, Denmark
Svein Anda, Adjunct Professor in Radiology, MD, DMSc
Institute of image diagnostics
NTNU, Trondheim, Norway
Jyri Lepistö, Assistant Chief Orthopaedic Surgeon, MD, PhD
COXA Hospital for Joint Replacement
Tampere, Finland
List of papers
This thesis is based on the following four papers, which will be referred to in the text by their Roman numerals (I–IV).
Mechlenburg I, Nyengaard JR, Romer L, Soballe K. Changes in load-bearing area after Ganz periacetabular osteotomy evaluated by multislice CT scanning and stereology. Acta Orthop Scand 2004 Apr; 75(2): 147-53.
Mechlenburg I, Nyengaard JR, Romer L, Soballe K. Prospective bone density changes after periacetabular osteotomy: a methodological study. Int Orthop 2005 Oct; 29(5): 281-6.
Mechlenburg I, Nyengaard JR, Gelineck J, Soballe K. Cartilage thickness in the hip joint measured by MRI and stereology – a methodological study. Osteoarthritis Cartilage 2007 Apr; 15(4): 366-71.
Mechlenburg I, Kold S, Romer L, Soballe K. Safe fixation with two acetabular screws after Ganz periacetabular osteotomy. Acta Orthop 2007 Jun; 78(3): 344-9.
Preface
This PhD thesis is based on studies carried out during my employment as Research Assistant at the Department of Orthopaedics, Aarhus University Hospital in the period 2004–2007.
I am deeply indebted to a number of persons who have made this work possible. First of all, I have been privileged to have the direction and guidance of three excellent mentors Professor Kjeld Søballe, Associate Professor Jens Randel Nyengaard and MD, PhD Søren Kold. From the inception of this project Kjeld Søballe has provided eminently helpful advice on everything from the design of the studies to the writing process. I am grateful for his faith in my abilities to carry out research and for giving me excellent working conditions in terms of extensive freedom, much responsibility and guidance whenever needed. Jens Randel Nyengaard has likewise made invaluable contributions to the development of ideas, methods and statistical analysis. He has provided excellent scientific advice and critique and encouragement throughout the project. Also, Søren Kold has contributed with insightful and critical comments as well as key suggestions to the design and undertaking of one of the studies.
My great appreciation goes out to all the patients who generously volunteered to participate in my studies. I am also very appreciative to Consultant Radiologist Lone Rømer and Consultant Radiologist John Gelineck for their thorough and comprehensive work and help with interpretation of radiographs, CT and MR images. I have deeply benefited from Secretary Karen Fousing's fantastic organising talent in regard to booking and coordinating the various examinations. Secretaries Lone Glargaard og Tina Stenumgaard are thanked for their always ready help with various subjects and for answering my inquiries so promptly.
I also wish to thank my fellow PhD students and the Bioanalysists in the research group for fruitful discussions at research meetings and journal clubs. I have sincerely enjoyed working with MD, PhD student Maiken Stilling and I wish to thank her for her always ready help and friendship.
Finally, I owe much to my family for always supporting me and encouraging me to achieve my goals. Birgitte Refslund, my close friend, has often put me up for the night when I have stayed over in Aarhus. But most of all, my deepest gratitude goes to my husband André Friis Møller and our children, Sophus, Benedicte and Elisabeth for always supporting me in this research project and helping out so I periodically could work long hours.
For financially support I would like to thank:
Gigtforeningen, Aase og Ejnar Danielsens Fond, Marie & M.B. Richters Fond, Direktør Kurt Bønnelycke og hustru fru Grethe Bønnelyckes Fond, Læge Søren Segel og Johanne Wiibroe Segels Forskningsfond, Købmand Sven Hansen og hustru Ina Hansens Fond, Konsul Johannes Fogh-Nielsens og Fru Ella Fogh-Nielsens Legat, Århus Universitetshospitals Forskningsinitiativ, Danske Fysioterapeuters Jubilæumslegat og Studielegat, Overlæge Poul M. Christiansens & hustrus fond, Augustinus Fonden and Helga og Peter Kornings Fond.
Abstract
The typical dysplastic hip joint is characterised by maldirection of the acetabulum and femoral neck, insufficient coverage of the femoral head focally and globally and erosions of the limbus acetabuli (Citation1). An unknown number of persons with hip dysplasia will suffer from pain in hip or groin, decreased hip function and development of osteoarthritis at a young age. The Bernese periacetabular osteotomy is performed to prevent osteoarthritis in patients with hip dysplasia and has been carried out at Aarhus University Hospital, Denmark since 1996 with more than 500 osteotomies performed. Throughout the years, research and quality improvement of the treatment has taken place and this PhD thesis is part of that process.
The aims of this PhD thesis were to evaluate outcome aspects after periacetabular osteotomy in terms of I) estimating the projected loadbearing surface before and after periacetabular osteotomy, II) estimating bone density changes in the acetabulum after periacetabular osteotomy, III) developing a technique to precisely and efficiently estimate the thickness of the articular cartilage in the hip joint and IV) examining the stability of the re-orientated acetabulum after periacetabular osteotomy.
In study I, we applied a stereologic method based on 3D computed tomography (CT) to estimate the projected loadbearing surface in six normal hip joints and in six dysplastic hips. The dysplastic hips were CT scanned before and after periacetabular osteotomy. We found that the average area of the projected loadbearing surface of the femoral head preoperatively was 7.4 (range 6.5–8.4) cm2 and postoperatively 11 (9.8–14.3) cm2. The area of the projected loadbearing surface was increased significantly with a mean of 49% (34–70%) postoperatively and thus comparable with the load-bearing surface in the normal control group. Double measurements were performed and the error variance of the mean was estimated to be 1.6%. The effect of overprojection, on the projected loadbearing surface was minimal. Consequently, the stereo-logic method proved to be precise and unbiased. The study indicates that this method is applicable in monitoring the loadbearing area in the hip joint of patients undergoing periacetabular osteotomy.
In study II, a method based on CT and 3D design-based sampling principles was used to estimate bone density in different regions of the acetabulum. Baseline density was measured within the first seven days following periacetabular osteotomy and compared with density two years postoperatively. Double measurements were performed on three patients, and the error variance was estimated to be 0.05. Six patients with hip dysplasia scheduled for periacetabular osteotomy were consecutively included in the study. Bone density increased significantly in the anteromedial quadrant of the acetabulum as well as in the posteromedial quadrant between the two time-points. In the anterolateral quadrant bone density was unchanged following surgery, and the same was true for the posterolateral quadrant. We suggest that the observed increase in bone density medially represents a remodelling response to an altered load distribution after periacetabular osteotomy. The described method is a precise tool to estimate bone density changes in the acetabulum.
Study III. As periacetabular osteotomy is performed on dysplastic hips to prevent osteoarthritic progression, changes in the thickness of the articular cartilage is a central variable to follow over time. 26 dysplastic hips on 22 females and 4 males were magnetic resonance imaged (MRI) preoperatively. The first 13 patients were examined twice, with complete repositioning of the patient and set-up in order to obtain an estimate of the precision of the method used. To show the acetabular and femoral cartilages separately, an ankle traction device was used during MRI. This device pulled the leg distally with a load of 10 kg. The mean thickness of the acetabular cartilage was 1.26 mm, SD 0.04 mm. The mean thickness of the femoral cartilage was 1.18 mm, SD 0.06. The precision calculated as the error variance was estimated for the thickness of the acetabular cartilage to 0.01 and femoral cartilage 0.02. We suggest that the method can be advantageous for assessing the progression of osteoarthritis in dysplastic hips after periacetabular osteotomy.
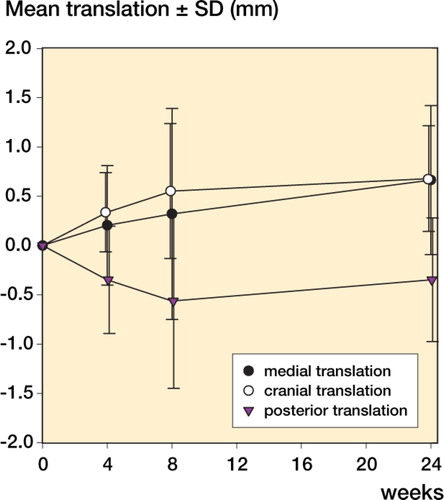
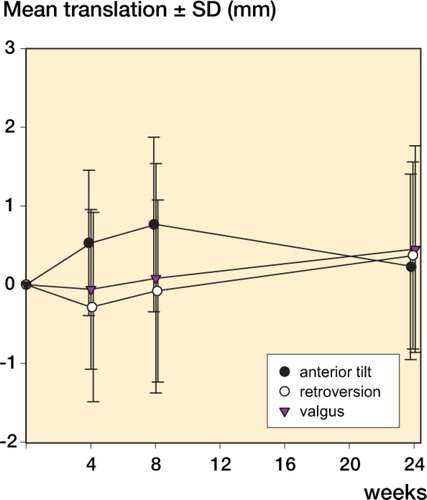
In study IV, 32 dysplastic hips, 27 females and 5 males were included in the study. Radiostereometric examinations (RSA) were done at one week, four weeks, eight weeks and six months. Data are presented as mean + SD. Six months postoperatively, the acetabular fragment had migrated 0.7 mm + 0.8 medially, and 0.7 mm + 0.5 proximally. Mean rotation in adduction was 0.5° + 1.3. In other directions, mean migration was below 0.5 mm/°. There was no statistical difference between migration 8 weeks and 24 weeks postoperatively in translation or rotation. Due to the limited migration, we find our postoperative partial weight-bearing regime safe.
In conclusion, the studies in the present PhD thesis indicate that the projected loadbearing area of the hip joint increases considerable in patients undergoing periacetabular osteotomy and a method to estimate this area was described. Bone density increases in the medial quadrants two years postoperative and a method is developed to precisely estimate bone density on CT images. Also a method to precisely estimate cartilage thickness was presented and we suggest that the method can be advantageous for assessing the progression of osteoarthritis in dysplastic hips after periacetabular osteotomy. Due to the very limited migration of the acetabular fragment fixated with two screws, we find our fixation sufficient and the postoperative partial weight-bearing regimen safe.
1. Introduction
A growing interest in hip dysplasia and periacetabular osteotomies to restore sound biomechanics of the hip joint is emerging (Citation2-6).
Dys is Greek for abnormal and plassein is the Greek term for “to create” or “to form” and morphological changes in the anatomy of the hip joint are exactly what hip dysplasia is. The changes can be more or less distinct and different imaging modalities are used to diagnose and evaluate the severity of hip dysplasia; primarily x-ray recording, but to some degree also computerised tomography (CT), magnetic resonance imaging (MRI), ultrasound (UL) and arthroscopy are used.
Untreated hip dysplasia can result in a degenerative process in the joint and eventually secondary osteoarthritis in an early age (Citation7). Total hip arthroplasty is not an optimal treatment of these patients because younger patients have high frequencies of aseptic loosening of the hip replacement implant and thus need for revision surgery (Citation8;Citation9).
The Bernese periacetabular osteotomy was introduced by the Swiss surgeon, Reinhold Ganz and he published the first results in 1988 after treatment of seventy five hips (Citation10). The Bernese osteotomy is a joint preserving surgical treatment of hip dysplasia that aims to normalise the hip joint anatomy. The Bernese periacetabular osteotomy has been performed at the Orthopaedic Department at Aarhus University Hospital since 1996. As it is a fairly new treatment, various aspects of the outcome have not yet been investigated. Aspects that already have been examined are: postoperative clinical outcome in terms of pain reduction (Citation11;Citation12), functional postoperative outcome (Citation12-14), quality of life (Citation12), ability to deliver vaginally (Citation15), radiological outcome measures in relation to progression of osteoarthritis (Citation16) and assessment of radiologically measured angles (Citation11;Citation17-21). Also different methods have been developed to estimate the contact pressure in the dysplastic hip joint (Citation20;Citation22;Citation23), and evaluation of walking pattern before and after surgery (Citation24;Citation25).
The background for this thesis was the wish to evaluate outcome aspects related to acetabular- coverage, bone density and migration. Furthermore, we set out to develop a technique to estimate the thickness of the articular cartilage in the hip joint.
2. Hip dysplasia
2.1 Pathogenesis of hip dysplasia
Normally, at birth the femoral head sits deep in the acetabulum held by surface tension of the synovial liquid. The growth and the hemispherical morphology of acetabulum are dependent on the presence of a normally growing and correctly placed spherical femoral head that works as a convex matrice. If for some reason the normal development is disturbed pre-or postnatally, pathologic relations may develop between the femoral head and the acetabulum (Citation26), leading to dislocation, subluxation and hip dysplasia. Only hip dysplasia is dealt with in this thesis.
Hip dysplasia is multifactorial in origin influenced by genetic and intrauterine factors, such as mechanical (rump presentation and oligohydramnios) and hormonal factors (Citation27). To ease the passage through the birth canal, the hip joint is quite mobile perinatally. Postnatally, the laxity of the ligaments will subside and the femoral head will normally position itself deeply in the acetabulum (Citation1). The theory is that if the femoral head does not migrate sufficiently into the acetabulum, dysplasia may develop because the matrice to stimulate acetabular growth is not correctly positioned.
Hip dysplasia is more common in females than in males (Citation28). This implies that the factors influencing the development of the disease affect girls more than boys. A possible mechanical factor may be that twice as many girls than boys are born in rump presentation (Citation1). Rump presentation results in hyperflexion and adduction in the hip joint which may stretch the joint capsula.
Another mechanical argument is used in relation to children from African countries where mothers carry their babies on the back. In this position, the child's hip joint is flexed and abducted pushing the femoral head deep into the acetabular cavity, and the assumption is that this cultural practise might partly explain the low prevalence of hip dysplasia in Africa compared to North America, Europe and Japan. In cultures in which where swaddling (hip adducted and extended) is practised, the prevalence of hip dysplasia is also high (Citation29).
The precise prevalence of hip dysplasia in adults is unknown but estimated to be 3.4 % in Denmark (Citation30), but not all these persons will experience clinical symptoms: pain and decreased function. In most instances, hip dysplasia is not diagnosed until adulthood due to no or few clinical symptoms in adolescence or due to limited knowledge about the disease among general practioners. The prevalence of hip dysplasia varies throughout the literature, depending on the cut-off values applied when measuring the CE-angle. Some researchers define a hip dysplastic as a CE-angle < 25° (Citation31-33) whereas others use CE-angle < 20° (Citation30;Citation34). Furthermore, ethnic differences in prevalence exist, such as high prevalence in Japan (Citation35;Citation36) and low prevalence in Africa (Citation37). Hip dysplasia is bilateral in 30–40% of the cases (Citation30).
2.2. Morphological changes
The dysplastic hip joint has a complex morphology characterised by a wide shallow acetabular cavity with an excessively oblique articulating roof. The acetabular cover of the femoral head is globally deficient (Citation38;Citation39) and the acetabular rim is hypertrophied possibly due to excessive pull from the often hypertrophic labrum. Anteversion is normal (Citation39-41), but occasionally the acetabulum is retroverted (Citation42;Citation43).
The femoral head is usually perfectly rounded; the joint as such is congruent, but the weight-bearing area between the acetabular roof and head is reduced. The articular cartilage is significantly thicker than normal (Citation44). Hip dysplasia is often associated with increased anteversion of the femoral neck (Citation39;Citation45) and with valgus neck-shaft angle that results in a reduced abductor lever arm (Citation46). However the deformities vary from individual to individual and retroversion of the femoral neck has also been reported in hip dysplasia (Citation46).
It seems that the articular cartilage and the fibrocartilaginous labrum adapt to the biomechanical demands they are exposed to in the dysplastic hip. Increased load is countered by thicker cartilage, and high strain on the labrum is opposed by hypertrophied rim and labrum.
2.3. Osteoarthritis as a result of hip dysplasia
Patients with hip dysplasia are prone to developing osteoarthritis of the hip at a young age (Citation7;Citation35). The reasons for this are not fully understood, but an explanation could be that the reduced contact area between acetabulum and the femoral head as well as a reduced abductor lever arm increase the load per contact-area in the hip joint (Citation38). The increased load is a strain on the articular cartilage and believed to result in degeneration of cartilage and eventually osteoarthritis (Citation7;Citation28;Citation47;Citation48).
A complementary theory suggests that a degenerated or damaged labrum initiates cartilage degeneration in dysplastic hips (Citation2;Citation49;Citation50). Labral lesions and acetabular rim fractures are results of the overload of the acetabular rim (Citation49), and arthroscopic studies show that the labrum often is affected in dysplastic hips (Citation2;Citation51), supposedly because of the high strain placed on it due to reduced bony support. Also, cartilage degeneration and subchondral cysts generally arise in the anterolateral part of the acetabulum (Citation52;Citation53). This theory is plausible and also offers a likely explanation why only some patients with hip dysplasia develop osteoarthritis.
In the hip joint biomechanical factors seem to be important in development of osteoarthritis, such as; joint incongruence due to developmental or congenital malformations (Citation54), excessive high loads (Citation55-57) and subluxation. Subluxation of the hip joint or untreated severe dysplasia will invariably lead to osteoarthritis (Citation58), but the rate and the extent of secondary osteoarthritis development in mild to moderate hip dysplasia is unknown (Citation50). Aronson (Citation59) argued that up to 50% of the patients with hip dysplasia would suffer from osteoarthritis by the end of the fifth decade.
The initial clinical symptoms of osteoarthritis are often vague, but usually present is noncharacteristic pain in the groin radiating to the anterior femur and the knee when loading the joint – especially at the end of range positions. The walking distance is reduced and some experience locking, snapping, weakness or instability of the hip joint (Citation60). When osteoarthritis progresses most patients develop a loading triad: pain when a movement is initiated, followed by temporary alleviation, succeeded by worsening. The pain is often localized in the groin with pain radiating down the femur and the greater trochanter and possibly down to the knee. The overall hip function of the patients operated on at our institution is measured with the Harris Hip Score (Citation61).
The radiological symptoms of osteoarthritis are narrowing of the joint space, increased sclerosis of the head and acetabulum, cysts in the head or acetabulum, osteophytes and later loss of sphericity of the femoral head. In these studies Tönnis' classification (Citation62) is used to determine the grade of osteoarthritis. A more quantitative method to estimate osteoarthritis is measuring the minimal joint space width (Citation63).
3. Periacetabular osteotomy
3.1. Advantages of Bernese periacetabular osteotomy
The purpose of periacetabular osteotomy is to increase acetabular cover of the femoral head and thereby distribute pressures better over the available cartilage surface. After age 14–15 years, when the triradiate cartilage is closed, the Bernese periacetabular osteotomy provides effective correction of residual dysplasia, and the surgical intervention can alter the natural history of hip dysplasia and improve hip-joint longevity (Citation64). The joint preserving procedure offers good pain relief in symptomatic hip dysplasia (Citation11;Citation12;Citation65), complete or partial healing of cysts (Citation66), and is not associated with higher mortality than total hip arthroplasty. Nor is periacetabular osteotomy an impediment for an eventual later total hip arthroplasty (Citation60;Citation67).
The advantages of the Bernese osteotomy compared to other pelvic osteotomies are several. The posterior column remains intact, conserving the stability of the pelvic ring. Hence the patients are allowed partial weight bearing on the second postoperative day. The osteotomised fragment is fixated sufficiently with only two screws (study IV). The shape of the pelvis is minimally changed (Citation68) and the majority of patients will be able to deliver a child vaginally (Citation15;Citation60). Because the sacropelvic ligaments are not attached to the acetabular fragment, the reorientation potential is large in three dimensions (Citation69;Citation70) and there is little doubt that Bernese osteotomy can achieve more correction than other techniques used in adult dysplastic patients such as triple innominate.
The triple innominate osteotomy of Steel (Citation71) is performed by transecting the ischial tuberosity in addition to performing osteotomies of the pubic ramus and the ileum. Disruption of the posterior column leads to fragment instability, requiring no weight bearing postoperatively (Citation60). Furthermore, the triple osteotomy has been found to narrow the inlet and outlet of the pelvis (Citation3).
3.2. Indications for surgery
Despite complex and individual morphological changes, diagnosing hip dysplasia is essentially done on an anteroposterior (AP) pelvic radiograph. On the basis of a standard supine AP pelvic radiograph, the radiologist measures the centre edge angle of Wiberg (Citation58) and the acetabular index angle of Tönnis (Citation62) (). In addition, joint space width is measured and degenerative changes such as cysts, osteophytes, sclerosis and fragmentation of the anterolateral acetabular edge are described (Citation45;Citation49). If the CE-angle is < 25°, another anteroposterior radiograph is recorded, this time with the hip joints in 25° abduction. This enables the radiologist to evaluate the congruency of the hip joint.
Figure 1. CT image of left dysplastic hip joint with global insufficient coverage of the femoral head and increased anteversion of the femoral neck.

Figure 2. Radiograph of osteoarthritis in right hip joint with moderate loss of sphericity of the head and severe narrowing of the joint space. The left hip is normal.

Figure 3. The CE angle and Tönnis' angle are measured on an AP radiograph in order to diagnose hip dysplasia. Joint space width is measured and degenerative changes described.
Earlier, the patients also had CT imaging preoperatively to obtain a three-dimensional evaluation of the individual morphological features to aid in surgical planning. With the extensive experience of the surgeon, this is no longer necessary, but the participants in studies I and II were operated on when preoperative CT scanning was standard procedure. Currently, approximately 15% of the patients have preoperative CT scan if there is uncertainty about the degree of osteoarthritis anteriorly or posteriorly in the joint.
If hip dysplasia is radiologically verified, the patient must fulfil the following criteria to be a candidate for Bernese periacetabular osteotomy:
Radiologically diagnosed dysplasia (i.e. CE-angle < 25°).
Osteoarthritis degree ≤ 2 according to the criteria of Tönnis ().
Pain from the hip.
Minimum 110° flexion in the hip and good rotation.
Closed growth zones in the pelvis.
Table 1. Progressive degenerative changes in the hip joint (Citation62)
3.3. Surgical technique
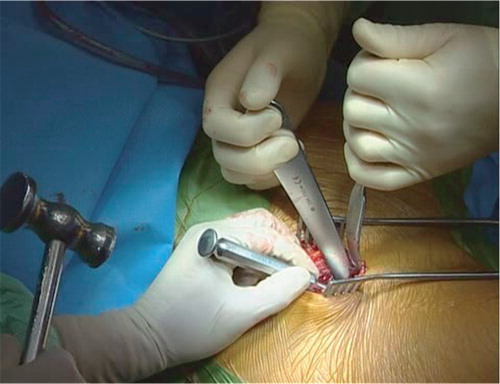
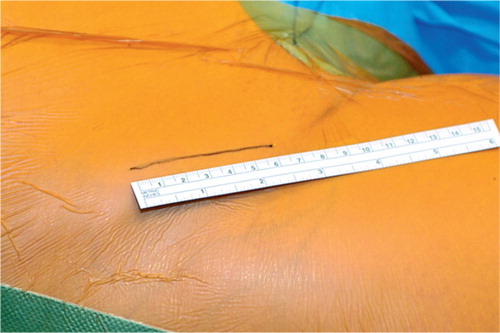
All periacetabular osteotomies in the patients included in this thesis were performed by the same surgeon with a minimally invasive surgical approach called the trans-sartorial approach. Hypotensive epidural anaesthesia was used because it reduces the loss of blood and results in a better view in the operation field. The incision was made from the anterior superior iliac spine descending 6 cm distally ().
Figure 4. Minimally invasive trans-sartorial approach with only a 6 cm incision starting from the anterior superior iliac spine.
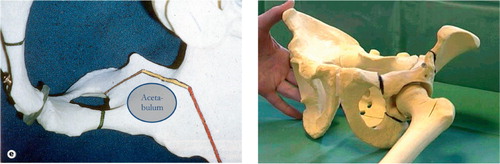
The fascia over the sartorius muscle was incised and the lateral femoral cutaneous nerve was exposed and was noticeable in the operation field throughout surgery. With this approach the tensor faciae latae muscle and the abductor muscles are kept intact and the sartorius muscle is split in fibre direction. The pubic bone was osteotomised and under fluoroscopic control the ischial osteotomies and the posterior iliac osteotomy were performed ( and ).
Figure 6. The pubic, ichial and iliac osteotomy viewed from the inside of the pelvis and seen from the outside. Note that the posterior column remains intact.
For the latter, an oblique view was used to ensure that the cut was extra-articular and to avoid penetration of the posterior column of the acetabulum (Citation72). After the iliac bone was osteotomised, the acetabular fragment was repositioned to optimise coverage of the femoral head. This positioning is very challenging and clearly the most demanding aspect of the procedure (Citation73). The correction was performed by measuring the centre-edge angle and Tönnis' angle with a specially made measuring device peroperative, using the fluoroscope. The aim is a Tönnis' angle between 0–10° and a centre-edge angle of 35° if possible. Intraoperative fluoroscopy assisted in evaluating the acetabular coverage and fixation of the two cortical screws inserted in the iliac crest. Before closing the operation field, local anaesthesia was infiltrated in the affected muscles and a catheter was placed in the wound to allow injection of local anaesthesia directly into the wound during the first twelve hours postoperatively. Based on data from the first 120 patients operated with the minimal invasive trans-sartorial approach, the mean duration of the operation is an hour and 10 minutes, average blood loss is 200 (150–350) ml, and the percentage receiving blood transfusions is 3.4% (Citation74).
An additional intertrochanteric osteotomy to improve joint congruency is occasionally necessary but such patients were not included in this project.
In spite of suspicion of labral tear, the capsule is not opened for inspection. The rationale is that periacetabular osteotomy normalises the distribution of force in the joint and relieves the strain on the rim and the labrum and hence alleviates the symptoms. Furthermore, attempts at resuturing the labrum may be unsuccessful. If a patient complains of pain postoperatively, MRI with contrast is performed to enable visualisation of the labrum and if a labral tear is found, the patient is offered an arthroscopy of the hip.
While in hospital (4–5 days) the patients are seen daily by a physiotherapist for active hip range of motion exercises. The patients are mobilised 6 hours postoperatively, and on the first day patients are allowed 30 kg of weight bearing and given instructions in maintaining the weight-bearing limit with the use of crutches. From the eighth postoperative week, the patients are allowed to full weight bearing.
After discharge from hospital, the patients are seen for control by the physiotherapist and by the surgeon. Control x-ray examinations are performed after 8 weeks, 3, 6 and 10 years ().
3.4. Potential complications
Periacetabular osteotomy is a technically demanding procedure, and the complication rate is initially high (Citation10;Citation69;Citation75) but drops markedly with experience (Citation76). With a steep learning curve, it is clear that the potential complications are numerous. The complications are not equally severe, and divided into major and moderate they are the following:
Major: Intraarticular osteotomy, major nerve injury, deep vein thrombosis, arterial thrombosis, infection in joint, major haemorrhage, reflex sympathetic dystrophy (Citation76).
Moderate: loss of fixation, pubic or iliac nonunion, excessive lateral or anterior correction leading to impingement, heterotopic ossification, haematoma, lateral femoral cutaneous nerve dysaesthesias (Citation38;Citation73;Citation76;Citation77).
Dysaesthesias of the lateral femoral cutaneous nerve happen fairly frequently at our institution, and they are hardly considered a complication but rather an expected event after the operation because the nerve is stretched during surgery. The patients are informed preoperatively about the nerve numbness on the lateral thigh, and that the dysaesthesia diminishes in size or disappears with time (Citation76).
Unfavourable outcome is associated with higher age of the patient, moderate to severe osteoarthritis at surgery, a labral lesion, less anterior coverage correction, overcorrection and a suboptimal angle of Tönnis (Citation69).
4. Aims of studies
The aims of this thesis were:
Study I: Estimate the area of the projected load-bearing surface of the femoral head pre- and postoperative by computed tomography and stereology.
Study II: Describe a method to estimate bone density in different regions of the acetabulum based on computed tomography and 3D design-based sampling techniques.
Study III: Develop a precise method for estimating the thickness of the articular cartilage in the hip joint based on magnetic resonance imaging and stereology.
Study IV: Assess the stability of the reoriented acetabular fragment postoperative by radiostereometric analysis. And examine the correlation between the amount of re-orientation measured by change in radiographic angles and the migration of the acetabular fragment.
5. Methodological considerations
5.1. Material
The overall purpose was to evaluate periacetabular osteotomy performed in patients with hip dysplasia and therefore, it was essential to include a homogeneously sample of patients not confounded by competing diseases or syndromes. For that reason, the patients in the four studies were included after fairly strict inclusion and exclusion criteria to ensure that the sample of patients only had hip dysplasia. The patients were scheduled for Bernese periacetabular osteotomy at Aarhus University Hospital, and they were included consecutively according to the inclusion criteria described earlier (p.10).
Exclusion criteria were:
Diseases that predispose to hip dysplasia (e.g. Down's syndrome, Charcot-Marie-Tooth disease, Ehlers-Danlos' syndrome, cerebral paresis, meningomyelocele).
Legg-Calvé-Perthes disease.
Need for a femoral intertrochanteric osteotomy.
Previous surgery of the hip.
Non-spherical femoral head.
Subluxated femoral head (interrupted Shenton's line > 5 mm).
Pregnancy or potential pregnancy.
Metal implants such as pacemaker (study III).
Age > 20 years (studies I and II).
Nearly all patients receiving the written patient information agreed to participate in the studies. Patients with hip dysplasia have often experienced years of contact to doctors and numerous radiographs without the correct diagnosis being made. As a result, they are grateful for getting a diagnose and an explanation of their hip pain when they are referred to the Orthopaedic Departments. Also, some of them have children experiencing similar hip symptoms and all things considered, they are enthusiastic about entering research projects about hip dysplasia. Inclusion of patients is thus not difficult; however, the researchers have to have an awareness of not exploiting patients' eagerness to participate in research. We had ethical considerations related to asking the patients to participate in the CT studies (I and II) that involved two extra pelvic CT scans. On that account they received an extra radiation dose of 8.4 mSv. The patients in studies III and IV apart from the RSA and MRI examinations, also accepted DEXA scans, MRI with contrast and ultrasound of the hip. From a research point of view, such a battery of examinations on the same patient population is exceptional, but for the patients it is time consuming and associated with extra radiation. Naturally, we had permission from the local ethic committee, and we discussed the ethical implications and ended up deciding that the results of the studies and the potential improvements of the surgery justified asking the patients to participate.
5.2. Design of studies
All four studies were prospective clinical studies designed as a paired design, which means that a variable in a group of patients is compared before and after an intervention. Study III so far consists of preoperative data only, but it is designed with future follow-up examinations. A paired design is a strong statistical design because comparing within the same group of patients lowers the biological variation of the data. Subsequently, fewer patients need to be included in the study to reach sufficient statistical power.
5.3. Sample size
Size of sample in studies I and II was not based on a power calculation. In study I, we expected a major increase in projected load-bearing surface and assumed that we needed only a few patients to show this increase and test our method. In study II, we did not estimate sample size because the purpose of the study was to develop a method.
MRI study (III): This study eventually will consist of two studies: a methodological study (the one included in this thesis) and a clinical study with the purpose of examining changes in the thickness of the articular cartilage over time. We expected the stereological method to be very precise, and we assumed there would not be much biological variation in the data. We expected only minor changes in the cartilage thickness over time. Estimation of sample size was made, our assumptions being: alpha = 0.05 (two-sided), power = 0.80, minimally relevant difference = 0.05 mm and SD = 0.08 mm. Estimated required sample size was: n = 21 patients. We included 26 patients.
RSA study (IV): We expected only minor migration of the acetabular fragment, but the degree of and the direction of migration was difficult to predict, and no similar studies of pelvic osteotomies were found in the literature. A conservative estimate of sample size was made using the following assumptions: alpha = 0.05 (two-sided) and power of the study = 0.80, minimally relevant difference = 0.5 mm and SD = 1 mm. The estimated required sample size was n = 32 patients. We aimed to include 35 patients but ended up with 32.
5.4. Statistics
Statistical analyses were performed with SPSS 11.0 (Inc. Headquarters, 233 S. Walker Drive Chicago, Illinois 60606 USA) software package. In relation to the statistics used, the variables measured in these studies were continuous and measured on an interval scale. Normality was assumed after testing data for normal distribution. Hence parametric statistical tests were used. The level of significance was chosen to be 0.05.
CT study (I): The area of the projected loadbearing surface of the patients pre- and postoperatively were compared by paired t-test. The area of the projected loadbearing surface of the patients postoperatively and the control persons were compared by an unpaired t-test. The correlation between the centre-edge angle and the area of the projected loadbearing surface was analysed with Pearson's correlation coefficient. After double measurements the coefficient of error of the mean (CE) was estimated for the total area of the projected load-bearing surface (Citation78;Citation79).
CT study (II): The 1 week postoperative measurements were compared with the 2 years postoperative measurements using a paired t-test. After double measurements, the coefficient of error of the mean (CE) was estimated for bone density in the three zones of the acetabulum.
MRI study (III): The mean thickness and standard deviation (SD) for the acetabular and femoral cartilage estimated with the three described methods were presented. The coefficient of variation (CV) and the coefficient of error of the mean (CE) were presented for all three methods.
RSA study (IV): The difference between migration at 8 weeks and 24 weeks postoperatively was tested by a paired t-test. The correlation between the amount of re-orientation measured by change in radiographic angles and the migration in all directions of the acetabular fragment was tested by Pearson's coefficient of correlation. The precision was estimated from double examinations on seven patients and expressed as the standard deviation and 95% CI for SD in translations and in rotation.
5.5. Stereologic methods
Stereologic methods are used to obtain quantitative information about three dimensional structures based on observations from section planes or projections (Citation78). The methods are practical tools based on sound mathematical and statistical principles. A major advantage of stereology is that it can be used to minimise the workload using sampling and still provide reliable quantitative information about the whole structure of interest. Systematic uniformly random sampling in studies II and III ensured that the structures of interest were sampled with the same probability.
The design of studies I, II and partly III was based on measurements done on sagittal CT and MR images, and therefore the images were not sampled at random. The assumptions when using the stereologic principles in studies I, II and III were either to use isotropic images or to deal with a spherical structure. Based on radiographs of all included patients, we assumed that the femoral heads were spherical.
5.6. Computed tomography (CT)
CT enables three-dimensional visualisation of the complex morphological changes in the dysplastic hip joint and is often used as a supplement to x-ray recording. Other advantages with CT are good tissue differentiation and no geometric distortion meaning that the form and geometric dimensions of structures in a CT image remain unchanged (no tissue deformation). The disadvantage of CT is the relatively high radiation dose. CT imaging is associated with a negative biological effect and it is estimated that fifty Danes each year will die of radiation-induced cancer that can be traced back to an earlier CT scan. In Denmark, radiologic procedures are assumed to induce 125 incidences of deadly cancer a year (Citation80).
In CT imaging, the x-ray tube and detector rows rotate around the patient. The x-ray tube transmits radiation through the patient and the attenuation of the radiation is registered by rows of detectors. By comparing the attenuation in the tissue columns within a section, the absorption in each voxel is estimated. The CT value is defined as the absorption in specific tissues in relation to water x 1000, and the value is stated in Hounsfield-units (HU). Every voxel in a CT section is given a CT value that numerically corresponds to the absorption that has occurred, and this value is directly readable on the screen by a mouse-click on the desired pixel.
In studies I and II, a multislice CT scanner (Mar-coni Mx8000) was used. Spiral multislice 4 x 2.5 mm CT sections, increment 1.6 mm were performed with a pitch of 0.875 (120 kV, 150 mAs, imaging matrix was 512 x 512, field of view 400 x 400 mm, standard algorithm). Scan data were transferred to a Marconi Mx View workstation and reconstructed. The patients were positioned supine on the scanning table with a 4 cm pillow between the knees and both legs in neutral rotation.
As with other imaging modalities, CT images are subject to various artefacts. An artefact is any structure or CT value that cannot directly be traced back to the scanned object. Metal artefacts typically show up as black or white streaks on the images. The cortical screws fixating the acetabular fragment did result in artefacts but not to a serious extent probably because they were made of titanium (). Motion artefacts too, posed no problem possibly because scanning time was only approximately two minutes.
Figure 8. Sagittal CT image of hip joint after Bernese periacetabular osteotomy. The cortical screws fixating the acetabular fragment only resulted in minor artefacts probably because they were made of titanium which is known to cause few metallic artefacts.
Partial volume effects – over- or underprojection – arises when tissues of different origins enter the same voxel. The absorption value associated with a voxel and later with a pixel is a mean value for the entire voxel. The bigger the voxel, the greater is the risk of obtaining unfortunate mixtures of tissues and subsequent risk of getting false CT values in the reconstructed CT image (Citation80). The problem cannot be avoided altogether, but be minimised by the use of thinner sections and we chose to scan with thin sections and thereby reduce the potential problem of false CT values in study II.
To investigate whether the estimation of the load-bearing surface in study I was affected by overprojection, an object of measurable dimensions was scanned with scan parameters identical to those applied to the patients. We found an overestimation of approximately 3.8% on the projected load-bearing surface due to the overprojection when the estimation was based on 2.5 mm CT images. However, we considered this error due to overprojection too small to be clinically relevant.
5.6.1. Measuring projected load-bearing surface
In study I, the pelvis of the patients was CT scanned before and one week after periacetabular osteotomy in order to compare the load-bearing surface pre- and postoperatively.
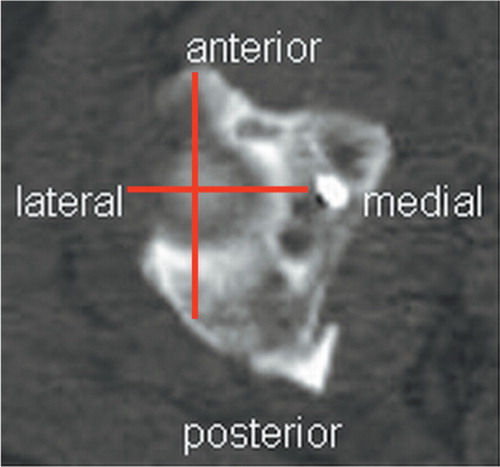
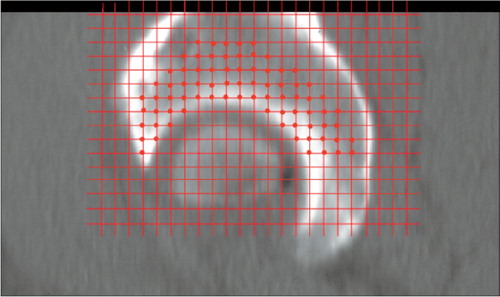
The CT images of the hip joint were reformatted in order to view them as sagittal images through the joint. A system of co-ordinates with an x-axis and a y-axis provided exact information on the position of the cursor on the reformatted CT images. The images were viewed and it was noted on which image the femoral head came into view and on which image the femoral head disappeared. Thereafter the number of images displaying the femoral head was determined and the central image could be identified ().
Figure 9. a) The x-value (in the system of co-ordinates) for the anterior edge and the posterior edge of the femoral head on the central slice was noted after which the diameter and the central point of the femoral head could be determined. b and c) The central point of the femoral head is defined at the position presented in Figure 9a with an exact x-value on all images. On the following sagittal images, the x-value for the projected acetabular margin on the femoral head anteriorly and posteriorly was noted, and the horizontal distance to these two points was measured. This patient has large cysts in the acetabulum and one in the femoral head and has osteoarthritis degree 2.
The measured distances were added, half the maximum diameter of the femoral head subtracted and multiplied by the section thickness. In this way, the distances contributed to the load-bearing area could be divided into four quadrants ().
Figure 10. For the purposes of the study, the acetabulum was divided into four quadrants based on the central point of the femoral head illustrated by an axial CT image of the top of the femoral head. The spot that lights up to the right is an artefact caused by an inserted screw.
The area of a quadrant (am) was estimated by this equation:
A(am) = (∑ Δ(am) − ½ D)t
A = area, Δ = |x(anterior) – x(central point)|, D = maximum diameter and t = section thickness.
The area of the projected load-bearing surface was divided into four quadrants to obtain detailed information on acetabular coverage of the femoral head.
Normal values for the projected load-bearing surface were obtained from 6 control persons, 4 females and 2 males without hip dysplasia. The mean age of the control group was 52 (27–77) years. The persons with normal hip joints were older than the patients with hip dysplasia. The mean radius of the femoral head was 2.2 cm for both groups. The control persons had an acetabular or pelvic fracture requiring CT scanning. The acquired CT data from the normal hip joints were used in this study to compare the load-bearing surface of the patients and the control persons.
5.6.2. Estimation of bone density on CT
An early sign of osteoarthritis secondary to hip dysplasia is a laterally triangular sclerosis in the acetabular roof (Citation81). The sclerosis represents new bone apposition in response to increased pressure to the lateral acetabular rim. Some researchers have found decreased subchondral sclerosis in the periarticular bone after periacetabular osteotomy (Citation38), and for this reason bone density in the acetabulum was investigated immediate after and compared with bone density 2 years after periacetabular osteotomy (study II).
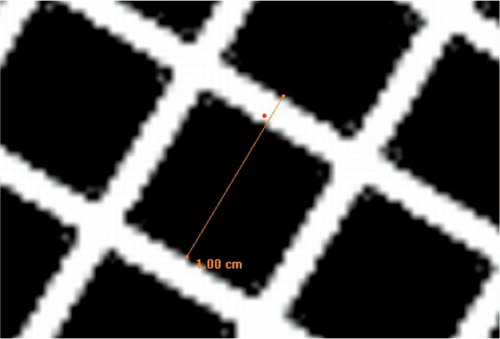
The CT images of the hip joint were reformatted in order to view them as sagittal sections through the joint and the acetabulum was divided into four quadrants exactly as in study I. The objective of dividing the acetabulum into four quadrants was to obtain detailed information on bone density in different regions of the acetabulum using systematic uniformly random sampling. Sections medial to those in which the femoral head was visible were not used for measuring because those sections include the acetabular fossa where an adaptive response in acetabular bone density would not appear. Also, it was a way of defining the medial limit of the acetabulum ().
Figure 11. At first, the acetabulum was divided into three zones: The most joint-close 4 mm was defined as zone 1, the next 4 mm (above 4 to 8 mm) was defined as zone 2 and the next 12 mm (above 8 to 20 mm) was defined as zone 3. Secondly, a point counting grid with squares of 4 x 4 mm was placed on each CT image. Thirdly, where a point in the counting grid hit one of the zones in acetabulum, CT values were registered (red points). Points in cysts, osteophytes and screw were excluded.
In this way, CT values of the three zones of the acetabulum on all sagittal images were collected and a mean CT value for three zones in four quadrants was estimated postoperatively and 2 years after surgery. A data set of about 500 measurements for each acetabulum was collected at each time interval.
The CT scanner was calibrated against air on a weekly basis and against water four times a year. Every 6 months, a reference phantom was used to calibrate the CT number linearity in order to compensate for any potential drift in CT numbers with time. Based on this procedure, we are quite confident that the longitudinal stability of the CT values from this scanner are acceptable over the period of the study.
A place for improvement in this study would be to decide on a consistent method of determining the joint boundary, for instance 1 mm above the boundary on the images. The rapid change in CT value across a boundary from cartilage to subchondral cortical bone will influence the measured bone density in zone 1 due to partial volume averaging. Sometimes the appearance of the boundary was blurred, making it difficult to determine whether a point in the counting grid was in or out.
5.7. Magnetic resonance imaging (MRI)
In study III the patients were MR scanned preoperatively and also 1 and 2½ years postoperative. The examinations were performed on a 1.5 tesla MRI scanner (Siemens, Erlangen, Germany) using a body array surface coil. MRI coils act as transmitter coils of the radiofrequency field and/or receiver coils. The radiofrequency pulse excites the protons and the surface coil receives the resultant signal. The body array surface coil is a receiver coil. It is only used to receive the signal coming from the tissue nearby (Citation82). This makes it possible to achieve the optimum balance between the largest possible field of view and the highest possible spatial resolution. A fat-suppressed three-dimensional fast low angle shot (FLASH) sequence was obtained. FLASH is a T1 weighted gradient echo sequence. This sequence allows thin slices and a 3-D data set. This visualizes the articular cartilage with a high signal and high contrast. The imaging matrix was 256 × 256, field of view 220 × 220 mm with a section thickness of 1.5 mm. The time between two pulse sequences (TR) and the time between the radio frequency pulse and the echo (TE) determine how the resulting image is weighted, as T1-weighted or T2weighted. In study III the TR/TE was 60.0/11.0 ms. The flip-angle was 50° and the time of acquisition was 9.38 min. Articular cartilage has high signal intensity (white) in this sequence.
To show the acetabular and femoral cartilages separately, an ankle traction device was used during MRI. This device pulled the leg distally with a load of 10 kg. Applying 10 kg of traction will separate the femoral and acetabular cartilage sufficiently in a person with little muscle tissue around the hip, whereas the same load has a smaller separating effect on a heavier person with well-developed muscles. Had we applied heavier traction in some of the patients, it would have facilitated separating the surfaces in all patients. Obviously, applying 10 kg of traction on all patients was planned as a standardisation of the examination procedure, but had we graduated the load of the traction, it would not have given rise to any bias because the purpose of the traction was merely to facilitate measuring femoral and acetabular cartilage separately. Another consideration is that the traction must not be too heavy because 10 minutes of application is uncomfortable for the patients. Otherwise, they may not come back for the follow-up MRI. Optimally, we should have started out with a pilot study graduating the load of traction on persons of various body shapes to test how much load is required to separate the femoral and acetabular cartilage in dissimilarly built persons.
Another factor limiting the effect of the traction is that we used an ankle traction device that when applied will separate not only the hip joint but also the knee joint. It is reasonably to expect that the effect of traction would have improved by using a traction device applied proximal to the knee joint. However, such a device is difficult to construct in a way that avoids the device sliding of the knee joint when the load is applied, hence we ended up using traction applied to the ankle ().
Error due to human judgement and limited contrast in the images is almost always a factor in morphological studies (Citation83). We made the decision not to adjust the contrast of the MR images because this may change the appearance (and possibly size) of the cartilage affecting the validity of the measurements. If adjusting the contrast would help visualize the cartilage, we would have to make sure to make similar adjustments from one image to another, and this is quite difficult.
Occasionally, it was difficult to identify the interface between femoral and acetabular cartilage, although traction was used during MRI to separate the acetabular and femoral cartilages (). To account for this the observer practised the three different methods before performing the actual and recorded measures in order to become experienced in making similar judgements in all images. Naturally, this will be harder to deal with if the methods were to be used clinically with more than one person measuring the cartilage thickness.
Figure 13. Sagittal MR image. In this patient it was difficult to separate the acetabular and femoral cartilage even though traction was applied.

MR images are subject to artefacts resulting from acquisition or data handling problems or from processes within the patient. Artefacts related to the patient include motion artefacts, chemical shift artefacts and magnetic material effects.
Motion results in blurring of image details. The blurring associated with motion is generally slight and occurs in the direction of the motion (Citation84). We did not experience real problems with motion artefacts in study III although it is not easy to lie still for nearly 10 minutes, but the traction device might have helped in maintaining the lower extremity in the same position during imaging.
The term “chemical shift” is used to describe the variation in resonant (Larmor) frequency that results from differences in molecular environments. The relative shift in resonant frequency is caused by slight non-uniformity in the local magnetic field. This phenomenon becomes a factor when imaging at fat-water interfaces. These two substances have different resonant frequencies, and when an image is reconstructed, water and fat are displaced about 5 pixels width (Citation84). This is avoided by using fat suppression which eliminates this phenomenon.
MR images are extremely sensitive to distortions in magnetic field homogeneity. The magnetic field can be locally distorted by implants, such as hip prostheses and surgical wires. The effect is a geometric distortion of the image that is often larger than the size of the object causing the distortion (Citation84). We investigated whether metallic artefacts from the screws inserted in the pelvis at periacetabular osteotomy posed a potential problem for the methods used. There were only minor artefacts from the titanium screws, and these were in the iliac bone and did not interfere with the measurements of cartilage thickness.
MR images can be seriously distorted by field inhomogeneity. We MR imaged a phantom with the same scan protocol as used for the patients. The images of the phantom were measured to assess whether the measured distances agreed with the geometric dimensions of the phantom (). We found that the measured distances on the MR images were nearly 6% longer than the actual distances on the phantom. This was a very disturb-ing result, because it meant that our measurements of cartilage could be up to 6% overestimated compared to the actual thickness of cartilage. Then we consulted a MR physicist for advice, and he did a thorough test with a MRI phantom to verify the spatial resolution and the geometry and found that it was perfect. After having confirmed the validity of the measurements of cartilage thickness on our MR images, we called in the same group of patients for MR imaging 1 and 2½ years after surgery to investigate whether the cartilage thickness changes after Bernese osteotomy. We do not have the results of this study yet.
Figure 14. Linear measurement on MR image of MRI phantom performed to verify the geometry on objects on MR images.
5.7.1. Estimating cartilage thickness
Three different stereologic methods to measure the thickness of cartilage were tested and evaluated for precision and efficiency (). We opened the MR images and measured the cartilage thickness in software (Grain 32, Dimac and KT Algorithms) designed for stereological purposes. The measurements were performed manually by one person without knowledge of clinical data or results of other examinations. The interface between femoral and acetabular cartilage was identified as a result of the traction device used during MRI. The interface between cartilage and bone was easy to discriminate in most images.
Figure 15. Method 1: On the sagittal images of the hip joint, every third image per series was sampled which added up to four to five images. In the software, a user-specified grid of approximately 15 vertical test lines was selected and superimposed on the images, and where the test lines intercepted the cartilage, the orthogonal distance through the cartilage was manually measured. The approximately 60–80 measured distances were summed, and the mean thickness of the acetabular and femoral cartilage was calculated (Citation85).
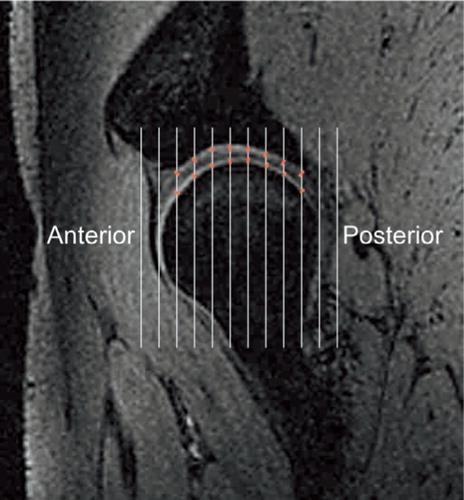
Figure 16. Method 2: On the sagittal images of the hip joint, every third image per series was sampled which added up to four to five images. A grid of approximately 15 vertical test lines was selected and superimposed on the images, and where the test lines intercepted the cartilage, the distance following the direction of the test line through the cartilage was manually measured. The approximately 6080 measured distances were summed (Citation86), and the mean thickness of the acetabular and femoral cartilage was calculated.
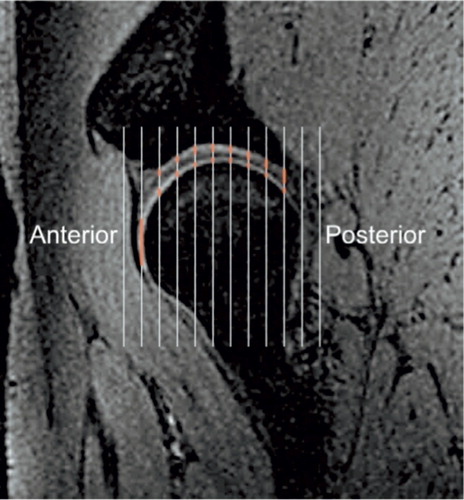
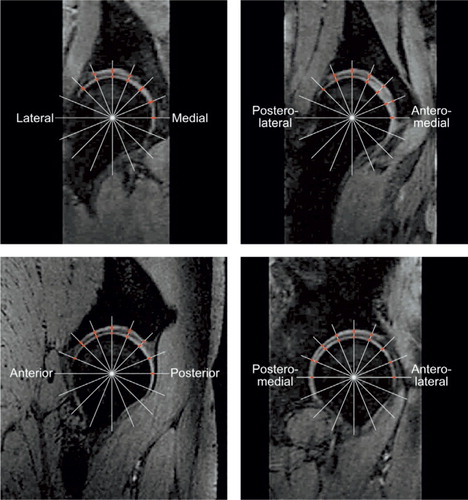
Figures 17. Method 3: Four reconstructed images through the centre of the femoral head were used. This consisted of a sagittal, a coronal and two images placed 45° between coronal and sagittal. On each of the four images, a grid of 15–20 radial test lines was selected and superimposed on the images, and where the test lines intercepted the cartilage, the orthogonal distance through the cartilage was manually measured. The approximately 60-80 measured distances were summed, and the mean thickness of the acetabular and femoral cartilage was calculated.
5.8. Radiostereometric analysis (RSA)
In study IV the patients were examined by RSA. The use of radiographs to evaluate whether a bony fragment or prosthesis migrates from its initial position underestimates the migration, and there fore RSA should be used for this purpose (Citation87). RSA is a very precise and reproducible method investigation (Citation88-92) used to describe movement between two sets of rigid bodies, defined with the help of x-ray-opaque tantalum markers, one set of markers constituting a fixed point (Citation93;Citation94).
During surgery, tantalum markers were inserted into the acetabular fragment (five 1 mm markers were spread well apart) and five markers (0.8 mm) were inserted into the illiac bone above the fragment. At the beginning of the study, the markers in the iliac bone were inserted fairly close to each other. But later we realized that this was not optimal, and the markers were inserted further apart. When the markers are positioned too close to each other, the estimation of especially rotation is less reliable ().
Figure 18. Radiograph with bone markers. The position of the markers affect the estimation of migration. The markers should not be positioned closely.

The analysis of migration was done by stereo radiographs taken with the use of two fixed x-ray tubes with a 40 degree angle between them positioned above the patient's hip. The patient was positioned supine on the examining table, and a calibration box (Carbon Box Aarhus, MEDIS, Netherlands) placed underneath created a 3D coordinate system of the tantalum markers. The calibration box consists of two defined sets of tantalum markers – fiducials and controls and before examination, two x-ray films are placed under the calibration box. In this set-up, the patient's hip was exposed to the two simultaneously firing x-ray tubes (150 microSv, 96 kV and 13 mAs) ().
Figure 19. The RSA set-up with the patient positioned supine on the examining table and a calibration box underneath creating a 3D coordinate system of tantalum markers.

At Aarhus University Hospital, the stereo-x-ray system is digitalized, which means that the digitalized radiographs can be used directly in the analysis program. In this way, the lessening of quality that results when radiographs are printed in hard copy and then digitalized by inscanning is avoided. The digital radiographs (Fuji FCR AC – 3CS/ID) were obtained and the DICOM files were evaluated by RSA-CMS (MEDIS, Leiden, the Netherlands). With this software package, the changes in the position of the acetabular markers in relation to the iliac markers are calculated. At least three acetabular and three iliac markers are necessary to obtain a rigid body of the acetabular fragment and the iliac bone between which the migration is calculated. Because we inserted five markers in the acetabular fragment and five markers in the iliac bone, we did not encounter problems with detecting sufficient markers to calculate the migration of the acetabular fragment ().
Figure 20. The markers in the illiac bone and the markers in the acetabular fragment are detected and connected on the two radiographs in the RSA-CMS software package. The RSA image consists of two image halves on which the same object can be seen but at different angles.
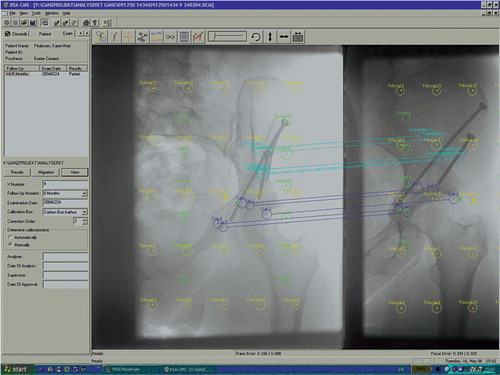
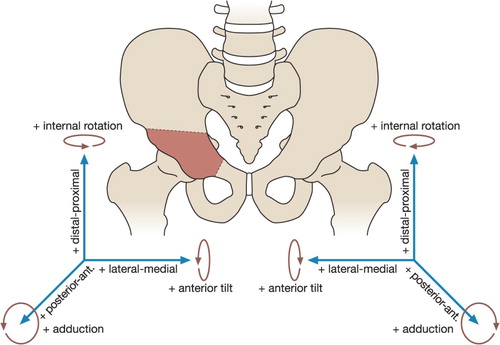
One week after surgery, the first stereo radiograph was taken, and the initial position of the acetabular fragment was determined in relation to fixed points in the iliac bone. Follow-up radio stereometric examinations were done at 4 weeks, 8 weeks and 6 months. Based on the follow-up examinations, the software allows a precise calculation of the translatoric and rotatoric migration of the acetabular fragment in the x-, y-, and z-axes. Migration of the acetabular fragment is expressed as translation and rotation of the centre of gravity of the markers inserted into the acetabular fragment. represents the pelvis and the position of the coordinate system and the direction of positive translations and rotations.
To calculate the precision of the RSA method, double examinations of the first seven patients were performed within a time interval of 10-15 minutes at the 6 month follow up. The patients were asked to step down from the examination table, and x-ray tubes, calibration box and table were repositioned. In this short time interval, no movement of the acetabular fragment should occur with respect to the iliac bone.
One limitation of this study is that the patients were mobilized the second day after surgery, and theoretically the acetabular fragment could have migrated from the position achieved at surgery before the first stereo radiograph was taken. Therefore the total migration of the acetabular fragment may be underestimated in this study.
Another limitation is that on some of the radiographs, some markers were barely visible, hidden behind one or two screws. In those instances, the markers had to be detected manually. This could take quite some time but more critical was that the detection of the correct centre of the markers was encumbered with greater uncertainty and thus could affect the estimation of migration. However, the software enables manual control of marker detection and connection-lines, and consequently incorrect positioning of a marker should be discovered and corrected.
5.9. Measuring angles on radiographs
X-ray recording is the primary imaging modalities used to diagnose hip dysplasia by measuring the centre-edge angle, the anterior centre-edge angle and Tönnis' angle. Initially, at our institution an anteroposterior pelvic radiograph is taken with the patient supine on the examining table and the lower extremities fixed in internal rotation with the use of a wedge-shaped pillow. Internal rotation compensates for the anteversion of the femoral neck, and if the patient externally rotated during recording, the measurement of the neck-shaft angle would result in an increased angle.
In study IV, we hypothesised that the acetabuli that underwent the highest amount of re-orientation evaluated by centre-edge angle of Wiberg (Citation58) and the acetabular index of Tönnis (Citation62) measured pre- and postoperatively also were the acetabuli that migrated most postoperatively. The centre-edge angle assesses the superior coverage of the acetabulum (Citation58), and Tönnis' angle evaluates the orientation of the acetabular roof (Citation62) ().
The centre-edge angle is obtained by drawing a vertical line through the femoral head perpendicular to the horizontal line extending through the centre of both femoral heads. A line is then drawn from the centre of the femoral head to the most superolateral point of the acetabulum (Citation95). A centre-edge angle of less than 20° is clearly dysplastic, and a centre-edge angle above 25° is normal (Citation58). Some researchers define center-edge angles between 20–25° borderline dysplastic (Citation50). This is a delicate issue because the centre-edge angle is used as a measure for deciding whether to offer the patient a periacetabular osteotomy, and not infrequently the centre-edge angle is exactly between 20–25°. At our institution centre-edge angles below 25° are defined as dysplastic. Measured on CT images, normal value for the centre-edge angle is 41° (SD 7°) giving a normal range (± 2SD) of 27–55° (Citation96).
Tönnis' angle is formed by a line parallel to the inter-teardropline and a line from the lateral point to the medial point of the weight-bearing portion of the acetabulum. We chose, however, to replace the inter-teardropline with an inter-ischial tuberosity line because the position of the teardrop changes after Bernese periacetabular osteotomy. According to Tönnis, normal values for Tönnis angle are below 10° (Citation62), but other report normal values of 10±2° (Citation28). Tallroth et al. also found the upper normal value to be 12° measured on CT images (Citation96). As hip dysplasia is often bilateral, the angles should be measures for both hip joints on the radiograph.
When the patient is positioned on the examining table, it is important to avoid rotations and inclination or reclination of the pelvis because this affects the measurement of the centre-edge angle and Tönnis' angle (Citation97). Jacobsen et al. (Citation97) observed a significant effect of varying rotation and incination/reclination on the centre-edge angle in a radiographic cadaver pelvis study. Tönnis reported that when the pelvis is rotated, the Tönnis' angle on the side to which the pelvis it is turned decreases, whereas the angle on the opposite side increases. If the pelvis is brought into increased inclination, the Tönnis' angle decreases and on reclination, increases (Citation98).
According to Anda (Citation99) pelvic inclination in standing and supine pelvic radiographs varies only insignificantly. Also measurements of joint space width of the hip on standing and supine radiographs are concordant (Citation100). But at present, standing radiographs are regarded as superior in assessing hip dysplasia and osteoarthritis because they give the most accurate representation of the femoral head and joint space width in the weight-bearing position (Citation95). Had we been aware of that when we designed the studies, we would have used standing radiographs instead of supine.
A limitation of the measurements in study IV was that double measurements were not made, and thus we do not know whether the measurements were reliable. Other researchers have evaluated the reliability of the centre-edge angle and Tönnis' angle measured on AP radiographs and found the centre-edge angle to be reliable in the intraobserver comparisons but not in interobserver comparisons. Tönnis' angle was reliable according to both intra- and interobserver analysies (Citation101).
However, Troelsen et al. made double measurements on AP radiographs of the centre-edge angle and Tönnis'angle in 20 dysplastic patients (40 hips) to investigate the intraobserver variation. Double measurement of the centre-edge angle showed that given the first measurement, we can expect with 95% confidence that the difference to the second measurement will be between -4.3° and 3.5°. The similar 95% limits of agreement for Tönnis' angle are -2.2° and 4.2° (Citation102).
The difference in the values recorded when measuring angles probably occurs because of difficulty in defining the landmarks used in making these measurements. The lateral margin of the acetabulum in the dysplastic hip is often rounded rather than coming to a sharply well-defined point. The centre of the femoral head should not be difficult to define in a spherical head; however, our experience is that different observers define it slightly differently.
5.10. Precision
In research with measurements of a quantity the question arises: Will the observer obtain the same value at a second measurement under identical conditions? The analysis of this can be performed in different ways, and the result is called repeatability, reproducibility, intra-observer variation or precision, the latter term is used in this thesis. Precision is defined as the closeness of agreement between repeated independent test results obtained under stipulated conditions (Citation103). To estimate the precision of the applied methods, double measurements were performed on the same CT images in studies I and II. In studies III double MRI examinations with complete repositioning of the patient and set-up were done. After measuring twice, the coefficient of variation (CV) and the coefficient of error of the mean (CE) were estimated. First, the variance was calculated as the sum of differences between first and second measurement, divided by number of measurements:
VAR = ∑d2 / number of measurements
Then the coefficient of error of the mean was calculated as:
CV = SD/mean
And the coefficient of error of the mean was calculated as:
CE = SEM/mean
Stereology and CT in study I. To calculate the precision of the method used to estimate the projected load-bearing surface, the same person performed double measurements on the same CT images from two patients. CV was 0.09. CE was 0.02.
Stereology and CT in study II. The precision of the method to quantify bone density of the acetabulum was estimated by performing double measurements of the same scan data by the same operator on three patients. The CV ranged between 0.11–0.19. The CE was 0.05.
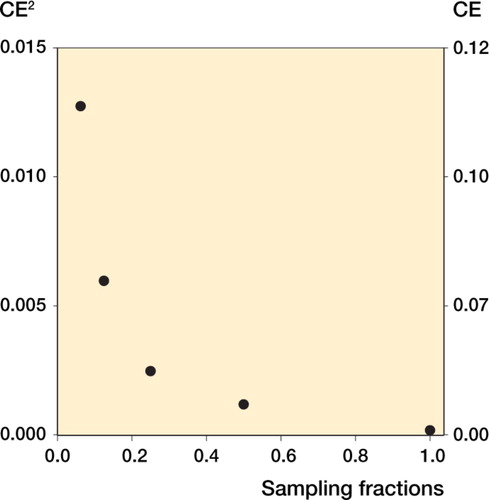
Stereology and MRI. The precision of the three methods quantifying the thickness of the acetabular and femoral cartilage was estimated by performing double measurements on images of 13 patients in whom the MRI procedure had been repeated within a few minutes after complete repositioning of the patient and set-up. The double measurements showed that the CV ranged between 0.05–0.11 and the CE ranged between 0.01–0.03.
RSA. The first seven patients were examined twice, (before and after complete repositioning of the patient and set-up) in order to obtain an estimate of precision of the method used. When the radio-stereometric method is used, it gives no meaning to calculate the CV and CE because the data for translation and rotation are negative as well as positive, and this results in a mean that potentially is zero. Instead the measurement precision is expressed as the standard deviation and 95% CI for SD in translations and in rotation (see ).
Table 2. The precision estimated from seven double RSA examinations (n = 7)
Angles measured on radiographs. These evidently should have been double-measured in study IV in which angles were measured to investigate whether the measurements were precise.
5.10.1. The relation between CV and CE
The precision of an estimate depends on the methods used and the objects investigated (Citation78). If the biological variance of a variable is great, the CV (SD/mean) is affected and thus high. CV includes the biological variation, CV(bio), and error variance of the method (CE). The following relation exists: CV2 = CV2 (bio) + CE2. Ideally, a study is designed such that CE2/CV2∼0.2–0.5, because the CE will then only have a limited influence on the total variation (CV) (Citation78). Hence, in addition to calculating the observed total variation of a variable, it should also be determined if the variation stems primarily from the method (e.g. a stereologic procedure) or from the biological variation of the measured variable.
This can be done by calculating the coefficient of error of the mean (CE = SEM/mean), which is an estimate of the variation of the method. Knowing the CE, one can also identify the influence of the method on the total variation. This is relevant information because it indicates whether the precision of a certain method will gain considerably by measuring more, i.e. collecting more data, or whether this is a waste of time because the majority of the observed variation is due to biological variation. In that case the method will not be much more precise despite the use of much more time. Conversely, the CE of a method can tell whether measuring fewer points can reduce the time needed to use the method.
6. Results
To clearly address the aims of the four studies, the findings of the studies are presented separately.
6.1. Area of the projected load-bearing surface of the femoral head pre- and postoperative
After periacetabular osteotomy, the area was increased by a mean of 49% (35–70%), p < 0.001. The average area of the projected loadbearing surface of the femoral head preoperatively (7.4 cm2) was significantly smaller than the same area postoperatively (11 cm2) and significantly smaller than the average of the normal hip joints (11.8 cm2) ().
Figure 22. Each patient is represented with a dot postoperatively and each control person with a square. The group mean of the area of the quadrants is shown by a bar.
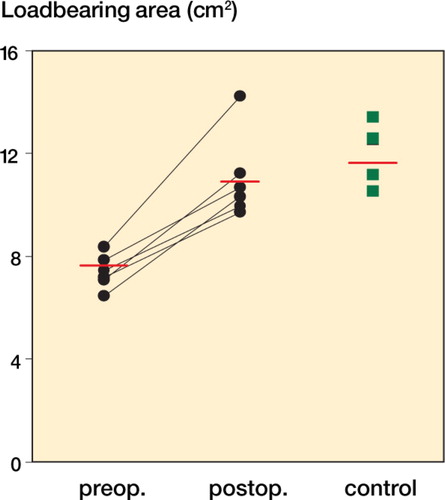
The average area of the projected load-bearing surface of dysplastic hip joints postoperatively was comparable with the load-bearing surface area in the normal control group. The same was true for the quadrants, apart from the area of the posterolateral quadrant, which was smaller (p = 0.001) than the same area in the control group ().
Figure 23. Each patient is indicated by a dot postoperatively and each control persons by a square. The group mean of the area of the quadrants is shown by a bar.
This method to estimate the projected load-bearing surface took approximately 45 minutes to carry out per hip.
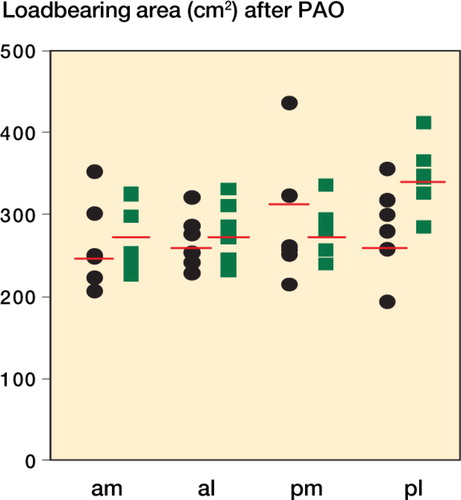
6.2. Bone density in different regions of the acetabulum
Two years after periacetabular osteotomy, bone density in zone 1 in the anteromedial quadrants was increased from a mean CT value of 673 [0.14] (506–764) mean [CV] (min–max) to a mean of 716 [0.11] (577–792), p = 0.025 and density in the posteromedial quadrants increased from a mean CT value of 643 [0.18] (476–784) to a mean of 709 [0.19] (526–896), p = 0.006.
In zone 1, bone density in the anterolateral quadrants was unchanged with a mean CT value of 748 [0.10] (649–854) following the operation and a mean of 718 [0.16] (565–894), p = 0.394 two years later. The same was true for the posterolateral quadrants, in which bone density had an initial CT value of 812 [0.12] (683–975), and two years later it was 789 [0.14] (687–957), p = 0.472 ().
Figure 24. Bone density in zone 1 of the medial and lateral quadrants of the acetabulum just after periacetabular osteotomy and 2 years postoperative. Three patients had a preoperative degree 2 osteoarthritis, and they are marked with a black dot. The other three patients had a preoperative degree 0 osteoarthritis and are represented with a white dot.
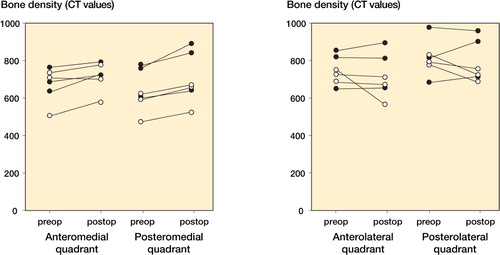
None of the changes in bone density in zones 2 and 3, two years after periacetabular osteotomy, were statistically significant.
This method to estimate bone density took approximately 5 hours to carry out per hip. After double measurements of bone density were performed, the coefficient of error of the mean was estimated to 0.05. The coefficient of error of the mean was 0.06 and 0.07 on the basis of registering the CT value at every second or third cross in the grid.
6.3. Thickness of the articular cartilage in the hip joint
The mean thickness of the acetabular and femoral cartilage estimated with the three described methods is shown in . The observed total variation was highest for method 2, making it the least precise method of the three. Methods 1 and 3 do equally well in relation to total variation and error variance. The two methods are quite similar, but the estimates in method 1 are based on sagittal images, whereas the measurements in method 3 are performed on centre images. All three methods took 15–20 minutes per hip to carry out.
Table 3. Thickness of acetabular and femoral cartilage, standard deviation (SD), coefficient of variation (CV) and coeffient of error of the mean (CE)
The effect on error variance of method 3 if fewer measurements are sampled is shown in .
6.4. Stability of the reoriented acetabular fragment
After radiostereometric examinations were initiated, no included patients were excluded from the study, but one patient did not attend the final examination.
In and the translation and the rotation over time are shown. Tested by paired t-test, there was no statistically significant difference between migration 8 weeks and 24 weeks postoperatively in translation or rotation (p-values ranging between 0.08 and 0.44). Our measurement precision expressed as the maximum standard deviation in translations was 0.58 mm and 0.56° in rotation.
6.5. Change in radiographic angles
A radiographic evaluation undertaken on preoperative and postoperative radiographs of the 32 hips is given in . Tested by Pearson's coefficient of correlation, there is no correlation between the amount of re-orientation measured by change in radiographic angles and the migration in all directions of the acetabular fragment (p = 0.16 to 0.85).
Table 4. Radiographic evaluation on preoperative and postoperative radiographs in 32 hips
7. Discussion
The aim of this Ph.D. thesis was to evaluate outcome aspects after Bernese periacetabular osteotomy, and the methods used and results of the four papers will be discussed in relation to relevant literature.
7.1. Area of the projected load-bearing surface of the femoral head pre- and postoperative
For the patients included in this study, the projected loadbearing surface was increased by an average of 49% postoperatively. The correlation between the centre-edge angle postoperatively and the increase of the projected load-bearing area was not significant, possibly because of the small number of patients included in the present study. Larger studies must clarify whether a correlation between the two exists.
The effect of periacetabular osteotomy on the loadbearing surface can be evaluated by the described method, which is simple to learn and easy to perform. The method is unbiased and based on double measurements, the precision is high. Furthermore, if the estimated projected loadbearing surface is based on every second instead of every sagittal reformatted CT image, the time consumed by the method can be reduced to approximately 25 minutes per hip without loss of high precision.
The group of patients and the group of control persons differed with regard to age and gender. However, the mean radius of the femoral head was 2.2 cm for both groups which justifies comparing the area of the projected load-bearing surface for the normal hip joints with the dysplastic hip joints postoperatively.
Hip dysplasia implies an oblique acetabular roof that covers the femoral head insufficiently. This results in a smaller articulating surface between the femoral head and the acetabulum and causes increased contact pressures. Pressure can be thought of as the stress generated over a surface by a distributed force (Citation104). In order to minimize contact pressures, the distributed forces must be reduced or the part of the articular surface transferring the forces must be increased. The area of the projected load-bearing surface is directly related to the level of contact pressure, and consequently contact pressures for the six patients included in this study was reduced after periacetabular osteotomy.
Studies have shown that contact pressures in dysplastic hip joints are higher than in normal hips (Citation22;Citation105). The present study shows that the average area of the projected load-bearing surface postoperatively (11 cm2) was close to the average area of the projected load-bearing surface for the normal hips (11.8 cm2). Theoretically, this means that contact pressures in dysplastic hip joints postoperatively are at a level comparable to contact pressures for the normal hip joints. However, it is an unproven hypothesis that reducing contact pressure on cartilage will slow or prevent additional joint degeneration. Furthermore, irreparable damage to the cartilage may have happened at the time periacetabular osteotomy was performed in these patients. Therefore it can-not be concluded that the degenerative changes in the hip joint have stopped or decreased after periacetabular osteotomy.
The area of the posterolateral quadrant in the group of dysplastic hip joints was smaller than the same area in the group of normal hips. This finding supports the findings of Haddad et al. (Citation106) who reported that during periacetabular osteotomy, the posterior cover is less well addressed. But what is the clinical importance of this is? The contact stress in the human hip is not uniform, and it changes with different body positions. The changing location of the peak contact stress during gait may indicate predilection sites for further development of osteoarthritis in the hip joint. On the basis of laboratory measurements and by using mathematical models of forces and stresses in the human hip, Mavcic et al. (Citation56) determined the points of the peak contact stress in successive phases of gait. They found that the peak contact stress is mostly located in the posteromedial quadrant of the of the loadbearing area. Furthermore, they found that in dysplastic hips the peak contact stress is located more laterally and anteriorly. However, the location of peak contact stress was only investigated during gait, whereas during rising from chairs, stair climbing and other daily activities the peak contact stress could be located differently.
Owing to the strict inclusion criteria for participating in this study, the data for the six patients are cleared of hip dysplasia conditioned by other illnesses. Consequently, the data material is optimal in terms of examining the effect of periacetabular osteotomy on the projected load-bearing surface on dysplastic hip joints.
7.2. Bone density in different regions of the acetabulum
Our study showed that bone density in zone 1 increased significantly in the medial quadrants. If the six patients were to be analysed in two subgroups (with or without preoperative osteoarthritis), it would appear that bone density in both the lateral quadrants decreased for three patients. However, these changes were not statistically significant. Yet, an increase in density medially and decrease laterally is consistent with how load is distributed after periacetabular osteotomy, and the (non-significant) decrease in the lateral quadrants substantiate the assertion that subchondral sclerosis can be reversed.
For two patients, bone density decreased in three quadrants, and for one patient, bone density increased in all four quadrants, which suggests that subchondral sclerosis was increased and osteoarthritis had progressed 2 years after surgery. Common for these three patients were that they all had grade 2 osteoarthritis preoperatively, whereas the other three patients had no osteoarthritis preoperatively. Bone density in zones 2 and 3 increased for all quadrants except one; however, none of the changes were statistically significant. The results for zones 2 and 3 indicate that bone density in the acetabulum 8 – 20 mm proximal to the joint is unchanged 2 years after periacetabular osteotomy.
When periacetabular osteotomy is performed, the hip joint is corrected and preserved. By collecting prospective bone-remodelling data, we wanted to study how this affected bone density. Schmidt et al. (Citation107) studied bone remodelling 1 year after total hip arthroplasty based on CT. At the acetabular level, one axial scan was performed and bone density immediately proximal to the press-fit acetabular component was decreased, but cortical bone density was increased. This suggests an altered stress pattern within the pelvis resulting from implantation of the cup. These findings are in accord with those of Wright et al. (Citation108) who found that bone-mineral density in the acetabulum decreased significantly 1.3 years after total hip arthroplasty for the treatment of advanced osteoarthritis. The decreased bone density found in these studies is probably the effect of stress shielding. This phenomenon is not likely after periacetabular osteotomy because no implantation has taken place. Trumble et al. (Citation38) reviewed the results of 123 periacetabular osteotomies at an average follow-up of 4.3 years. Based on evaluation of anteroposterior (AP) radiographs of the pelvis, they found increased subchondral sclerosis present in 99 hips preoperatively and in only 15 hips at the latest follow-up.
The CT values for zones 2 and 3 show that bone density gradually increase the more joint-close the CT value was collected, most likely because bone is exposed to a higher load close to the joint. The results for all three zones also showed that the observed total variance (coefficient of variation, CV) on bone density in the acetabulum is within relatively small limits. CV includes the biological variation, CV(bio), and variation due to the applied method (coefficient of error of the mean, CE). In this study, CE2/CV2 = 0.13 when all test points were used, CE2/CV2 = 0.19 when every second test point was used, and CE2/CV2 = 0.25 when every third test point was used. Changes in bone density in the acetabulum can be estimated by the described method, which is unbiased and precise. If bone density is estimated by registering CT values on every second or third cross in the grid, time can be reduced to about 2 or 3 hours per hip, respectively. Based on the above-mentioned considerations, we suggest using only every third test point.
The hypothesis is that because the dysplastic oblique acetabular roof incompletely covers the femoral head, weight-bearing forces are concentrated over a smaller than normal area where the femoral head contacts the acetabulum (Citation28). This mechanical situation equates to an increase in the force per unit area and results in abnormally high levels of stress and strain. The present study demonstrates that when the force per unit area is changed permanently, subchondral bone (zone 1) is remodelled to adapt to these changes by increasing bone density medially to withstand the higher load postoperatively and may show (for three patients) that bone density laterally is decreased as a result of load taken off the lateral part of the acetabulum postoperatively. Wolff's law has been the basis for adaptive bone remodelling theories (Citation109). These theories assume a relation between a local mechanical stimulus and the bone-remodelling rate.
For the past two decades, research into the aetiology of osteoarthritis has mainly concentrated on the destruction of articular cartilage where damage is clearly visible. The pathological changes occur in all elements of the joint, and those in the subchondral trabecular bone may play a primary role in the pathogenesis of osteoarthritis (Citation110). Recent investigations have proved that subchondral bone may be involved and play a significant role in the cartilage degeneration of osteoarthritis. Subchondral bone sclerosis may not be required for initiation of cartilage fibrillation but may be necessary for progression of osteoarthritis (Citation111).
There has been a considerable amount of work undertaken in this study to estimate bone density, and it is not realistic to spend that amount of time in a clinical setting to evaluate acetabular bone density after periacetabular osteotomy. However, the clinical relevance of the study is that subchondral bone density increases medially after periacetabular osteotomy as an adaptive response to changed load distribution.
Owing to the strict inclusion criteria for participating in this study, the findings for the six patients are not due to hip dysplasia caused by other illnesses. Consequently, the data material is optimal for assessing the effect of periacetabular osteotomy on bone density in the acetabulum. Still, more patients have to be followed over a longer period of time to asses the clinical implications of these findings because the group of six patients is too small and heterogeneous to reveal clear evidence of prospective changes in bone density. It is difficult to obtain permission from the ethics committee to CT scan patients several times for research purposes only, and we did not wish to include patients younger than 20 years of age.
7.3. Thickness of the articular cartilage in the hip joint
The three methods (1, 2 and 3) tested in this study were all swift and reproducible, but produced different mean cartilage thickness estimates. The stereologic sampling procedure deployed in method 2 yielded a CV2 twice as high as methods 1 and 3 in the same patients. Precision was equally good in methods 1 and 3; but we favour the former because it deploys images obtained through the centre of the femoral head, allowing perpendicular cartilage surface intersection. We thereby avoid the potential bias (partial volume effect) that may otherwise arise from oblique intersection of the cartilage of the femoral head because of its spherical form and the parallel nature of the imaging planes. Partial volume effect can be present as over- and under-projection and both phenomena are very difficult to control and correct for why the best solution is to use thin sections and thus diminish the problem.
The results for all three methods showed that the observed total variance (coefficient of variation, CV) on cartilage thickness is small. In this study, CE2/CV2 = 0.08 for method 1, CE2/CV2 = 0.06 for method 2 and CE2/CV2 = 0.08 for method 3. This means that the methodological error variance has basically no influence on CV. We also studied the effect on CE at a lower number of measurements to test the effect of reducing the overall time consumed by these methods.
Using one half of the measurements for cartilage thickness estimation produced a CE of 0.03. With 1/4 of the measurements, the CE was 0.05, with 1/8 0.08 and with 1/16 0.11.
Based on CE, sampling of 1/8 of the measurements (no. approx. 10) will produce an acceptable error variance of the method and time consumption will drop to about 5 minutes per hip. However, given the heterogeneity of cartilage loss in osteoarthritis caused by hip dysplasia, it is likely that the dependency of measurement precision on sampling increases with the severity of disease. It is also possible that the relative performance of the three methods varies with the severity, heterogeneity and distribution of cartilage loss. As a first step, we have tested these methods for precision. The next move is to refine method 3 in order to make it possible to measure cartilage thickness in four quadrants. This will enable us to identify the distribution of cartilage loss.
Joint space narrowing in the weight-bearing area is a well-known radiological finding in hip osteoarthritis indicative of articular cartilage wear in the weight-bearing area (Citation52). However, the threshold of clinical relevance of such narrowing (Citation63) is difficult to establish because it is often classified qualitatively (Citation112). Measurements of joint space narrowing provides only an indirect measurement of cartilage integrity (Citation113), and a subjective qualitative assessment of joint space narrowing is not sufficient for drawing conclusions about cartilage thickness because joint space narrowing does not appear before osteoarthritis has progressed as shown by Nishii et al. (Citation114) who detected a high prevalence of cartilage abnormalities in 70 dysplastic hips without joint space narrowing. For that reason estimating the cartilage thickness by the presented stereologic methods based on MRI may be used as a means of early diagnosis of osteoarthritis before the radiographic change is evident. MRI and traction can be applied to patients with hip dysplasia to evaluate cartilage thickness before deciding to perform a periacetabular osteotomy. If the articular cartilage is shown to be obviously thin and irregular on MRI, periacetabular osteotomy can be avoided (Citation115).
In addition, MR imaging and traction can evaluate cartilage abnormalities of the acetabulum and femoral head separately. Nishii et al. (Citation116) conducted MRI evaluations in patients with hip dysplasia and found that abnormalities of the acetabular cartilage seemed to occur earlier than those of the femoral cartilage in general. Hasegawa et al. (Citation112) reported on the basis of MRI that acetabular sclerosis preceded femoral head sclerosis in dysplastic hips, and another study disclosed a significant tendency for more frequent occurrences of cysts in the acetabulum than in the femoral head (Citation53). This might be due to the limited area in which the main load transfer occurs in the acetabular cartilage as compared with the femoral cartilage during gait and climbing of stairs in the patient with hip dysplasia (Citation116). Biomechanical analysis of the dysplastic hip joint has shown that the compressive stress is extremely high at the anterosuperior portion of the weight-bearing area (Citation117;Citation117). Several clinical studies on dysplastic hips support these results by showing that articular cartilage degeneration appears mainly in the anterosuperior part of the weight-bearing area of the femoral head and acetabulum (Citation52;Citation114;Citation118;Citation119).
Nakanishi et al. measured cartilage thickness of the femoral head with MRI and traction in 10 normal volunteers (Citation120). They found the cartilage to be thickest in the central portion around the ligamentum teres (mean 2.8 mm). The medial and the lateral portions were almost the same thickness (medial 1.3 mm, lateral 1.1 mm). Nishii et al. (Citation44) made computational analysis of MR imaging and found average cartilage thickness to be significantly greater in dysplastic hips than in normal hips (1.77 mm vs 1.34 mm). In another study the cartilage thickness of the femoral head in six cadavers was measured using different MRI pulse sequences, and in that study the measured mean thickness of the cartilage ranged between 1.36–1.70 mm (Citation121). These measurements of cartilage thickness are not directly comparable with our results, but they seem to be somehow greater than what we found in this study. The cause of this discrepancy is not based on chemical-shift because we used fat-suppression which eliminates this phenomenon.
Also, we have investigated whether metallic artefacts from the screws inserted in the pelvis at periacetabular osteotomy pose a potential problem for these methods. There are only minor artefacts from the titanium screws, and these do not interfere with the measurements of cartilage thickness.
Methods 1 and 3 were as precise but we favour method 3 which involves sampling four reconstructed images through the centre of the femoral head and using radial test lines, because using this method we avoid partial volume effect.
7.4. Stability of the reoriented acetabular fragment
To our knowledge, this is the first paper dealing with RSA in Bernese periacetabular osteotomy. We consider RSA to be an objective measure of osteotomy migration and find this important to evaluate because of concern about loss of correction and failure of fixation with performing periacetabular osteotomies (Citation69). Our data show that 24 weeks postoperatively, the mean translation of the acetabular fragment is less than 0.7 mm and the mean rotation less than 0.5° in our patient sample. Because there was no statistical difference between migration 8 weeks and 24 weeks postoperatively, we conclude the osteotomies were stable eight weeks after surgery.
In a biomechanical study by Babis et al. (Citation122), periacetabular osteotomies were done on six pelves from cadavers and fixed randomly with three screws from the iliac crest or with two screws supplemented by a transverse screw to the ilium. The pelves were loaded with up to 130 kg in a simulated push-off phase of the gait cycle. Displacement of the pubic osteotomy by mean 12.8 mm and 12.5 mm were measured, and the authors concluded that neither type of fixation provided enough stability to allow immediate weight-bearing after periacetabular osteotomy. However, at our institution patients are only allowed to bear a weight of 30 kg until 8 weeks after surgery and our clinical study clearly demonstrates that acetabular migration is very limited, although the osteotomies in our study was fixated with only two screws.
Yassir et al. (Citation123) tested the stability of Bernese periacetabular osteotomy on eight cadaver hips under simulated weight-bearing conditions using three-dimensional analysis of fragment displacement and angular rotation. The mechanical loading approximated partial weight-bearing in an adult. The acetabular fragment fixated with two screws from the iliac wing, as in our study, was displaced less than 1.5 mm and rotated less than 2.5°. The displacement and angulation found in this biomechanical study is higher also than what we found. According to our data, acetabular migration postoperative does not constitute a clinical problem in terms of loss of correction or failure of fixation, and consequently we find our postoperative partial weight-bearing regime safe.
Radiostereometric measurements of one pelvic osteotomy were performed as early as 1978 (Citation124) with the purpose of obtaining information about the position of the acetabulum pre- and postoperatively, but this study did not evaluate acetabular migration in the time period after surgery. RSA studies estimating migration after fractures have found slightly higher (Citation125;Citation126) or much higher (Citation127;Citation128) migration compared to the amount of migration we found.
The precision of RSA in our study calculated from double examinations was not as high as that reported by Vrooman et al. (Citation88), who in a RSA study of knee prostheses found the maximum standard deviation in translations to be 0.11 mm and 0.24° in rotation. Madanat et al. (Citation103) estimated precision of RSA in a fracture model of the distal radius. They reported that under optimal laboratory conditions, translations of 200 µm can be measured with a precision of 2–6 µm and rotations of 0.5° can be measured with a precision of 0.025–0.096°. The precision for this method applied on patients will be lower than under laboratory conditions because it is impossible to position the patient and the x-ray tubes in exactly the same way under consecutive radiostereometric examinations. Furthermore the optimal distribution of markers is more difficult to obtain in a patient during surgery than in a phantom, and in the patient the markers may be loose or hidden behind a screw, reducing the number of markers used to estimate migration.
The pre- and postoperatively measured angles in our study correspond well with what other groups have found (Citation11;Citation15;Citation28;Citation69). Our hypothesis about a possible correlation between the amount of re-orientation and the degree of migration of the acetabular fragment failed to be true. In another study, we have tested whether a correlation existed between the amount of migration and bone density in the acetabulum (Mechlenburg 2007 submitted data). This was not the case and probably, a range of factors affect migration of the acetabular fragment after surgery.
7.4. A critical view of performing Bernese periacetabular osteotomy
Although the Bernese periacetabular osteotomy provides effective correction of hip dysplasia, it is problematic that we do not know whether some patients would have been better off had the operation not been done.
Hip dysplasia is a significant risk factor for the development of osteoarthritis (Citation129), but not everyone with radiologically verified hip dysplasia develops osteoarthritis. Given that patients with hip dysplasia and hip pain are preferably operated on before osteoarthritis progresses, we will never know whether these patients would have developed osteoarthritis. In a longitudinal study comparing 136 controls with 81 persons with mild or moderate hip dysplasia followed for a decade, Jacobsen et al. did not document a tendency for radiological degeneration (Citation130).
From a scientific point of view, a randomised study should be done to investigate whether patients with mild or moderate dysplasia are better off not being operated on. Severely dysplastic patients should not be included because studies have shown that those patients inevitably will develop osteoarthritis (Citation7;Citation32). But the problems with a randomised study are numerous. It could be considered unethical to include patients in a lengthy study when we have a treatment that evidently reduces the pain (Citation11;Citation12;Citation65) and possibly increases the longevity of the patient's own hip. To what treatment should the patients then be randomised? – Pain-relieving drugs and physiotherapy are not sufficient when patients have pain corresponding to a mean VAS score of 6.7 and moreover have trouble sleeping at night or going to work. It is unlikely that a prospective randomised study of the natural history of untreated hip dysplasia will ever be conducted, because symptomatic patients are treated with an osteotomy before the onset of osteoarthritis, and the natural history is altered by treatment (Citation47).
In line with the principles laid down in Health Care Technology Assessment, the effect of new technologies should be assessed before implementing the technology. Yet, neither total hip arthroplasty nor total knee arthroplasty has been through randomised controlled trials before being implementing in the health services, and no one doubts that they are effective treatments. Therefore, from the clinician's point of view, it would be wrong not to offer Bernese osteotomy to patients with symptomatic hip dysplasia.
8. Conclusion
The potential problems associated with total arthroplasty in young adults have underscored the importance of preserving rather than replacing the hip. Because the patient's own hip is a living tissue with self-maintenance capabilities, the potential of improving the results after Bernese periacetabular osteotomy have not yet been fully exploited. In the coming years, a considerably amount of research ought to be invested in the continued evaluation of treatment strategies to ensure development and quality of these.
In conclusion, the studies in the present PhD thesis indicate that the projected loadbearing area of the hip joint increases considerably in patients undergoing periacetabular osteotomy and a method to estimate this area is described. Bone density is increased in the medial quadrants 2 years after surgery and a method is developed to precisely estimate bone density on CT images. Also a method to precisely estimate cartilage thickness is presented, and we suggest that the method can be advantageous for assessing the progression of osteoarthritis in dysplastic hips after periacetabular osteotomy. Because the very limited migration of the acetabular fragment after fixation with two screws, we find our fixation sufficient and the postoperative partial weight-bearing regimen safe.
A promising perspective with the methods presented in the present studies, especially in study III, is that these methods can be used clinically. The method to estimate cartilage thickness is precise, easy to perform and takes only 15–20 minutes per hip (can be reduced to 5 minutes per hip). A technician can do the measurements and evaluate the progression of osteoarthritis in selected patients.
9. Future research
Currently, we are conducting a study (with more patients than in study II) to examine bone density changes in the acetabulum with DEXA after surgery, and also looking into whether there is an association between bone density and migration. Also, follow-up examinations of study III is ongoing to investigate possible changes in the cartilage thickness over time. A Positron Emission Tomography study is taking place to evaluate acetabular perfusion before and after Bernese periacetabular osteotomy. Finally, a study is underway to examine the association between a damaged labrum and the development/progression of osteoarthritis after the surgical intervention.
10. References
- Jacobsen S, Sonne-Holm S. Ugeskr Laeger Jan 13, 2003; 165(3)210–4, [The dysplastic hip I. Etiology, epidemiology and diagnosis]
- McCarthy J C, Noble P C, Schuck M R, Wright J, Lee J. The Otto E. Aufranc Award: The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res Dec, 2001, 393: 25–37
- Loder R T, Karol L A, Johnson S. Influence of pelvic osteotomy on birth canal size. Arch Orthop Trauma Surg 1993; 112(5)210–4
- Ninomiya S, Nakamura T, Kamogawa M. Nippon Seikeigeka Gakkai Zasshi Aug, 1984; 58(8)779–92, [Natural courses of coxarthrosis and indication of rotational acetabular osteotomy]
- Soballe K. Ugeskr Laeger mar 19, 2001; 163(12)1703, [Hip dysplasia. Treatment with osteotomy by means of Ganz. The Danish Orthopedic Society]
- Millis M B, Murphy S B, Poss R. Osteotomies about the hip for the prevention and treatment of osteoarthrosis. Instr Course Lect 1996; 45: 209–26
- Cooperman D R, Wallensten R, Stulberg S D. Acetabular dysplasia in the adult. Clin Orthop may, 1983, 175: 79–85
- Berry D J, Harmsen W S, Cabanela M E, Morrey B F. Twenty-five-year survivorship of two thousand consecutive primary Charnley total hip replacements: factors affecting survivorship of acetabular and femoral components. J Bone Joint Surg Am Feb, 2002; 84A(2)171–7
- Malchau H, Herberts P, Ahnfelt L. Prognosis of total hip replacement in Sweden. Follow-up of 92,675 operations performed 1978-1990. Acta Orthop Scand Oct, 1993; 64(5)497–506
- Ganz R, Klaue K, Vinh T S, Mast J W. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Jul, 1988, 232: 26–36
- Pogliacomi F, Stark A, Wallensten R. Periacetabular osteotomy. Good pain relief in symptomatic hip dysplasia, 32 patients followed for 4 years. Acta Orthop Feb, 2005; 76(1)67–74
- van Bergayk A B, Garbuz D S. Quality of life and sports-specific outcomes after Bernese periacetabular osteotomy. J Bone Joint Surg Br Apr, 2002; 84(3)339–43
- Ko J Y, Wang C J, Lin C F, Shih C H. Periacetabular osteotomy through a modified ollier transtrochanteric approach for treatment of painful dysplastic hips. J Bone Joint Surg Am Sep, 2002; 84-A(9)1594–604
- Yasunaga Y, Ochi M, Terayama H, Tanaka R, Yamasaki T, Ishii Y. Rotational acetabular osteotomy for advanced osteoarthritis secondary to dysplasia of the hip. J Bone Joint Surg Am Sep, 2006; 88(9)1915–9
- Valenzuela R G, Cabanela M E, Trousdale R T. Sexual activity, pregnancy, and childbirth after periacetabular osteotomy. Clin Orthop Relat Res Jan, 2004, 418: 146–52
- Murphy S, Deshmukh R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin Orthop Dec, 2002, 405: 168–74
- Hisatome T, Yasunaga Y, Tanaka R, Yamasaki T, Ishida O, Ochi M. Natural course of the minimally symptomatic nonoperated hip in patients with bilateral hip dysplasia treated with contralateral rotational acetabular osteotomy. J Orthop Sci Nov, 2005; 10(6)574–80
- Hsieh P H, Shih C H, Lee P C, Yang W E, Lee Z L. A modified periacetabular osteotomy with use of the transtrochanteric exposure. J Bone Joint Surg Am Feb, 2003; 85-A(2)244–50
- Siebenrock K A, Schoeniger R, Ganz R. Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am Feb, 2003; 85-A(2)278–86
- Armand M, Lepisto J, Tallroth K, Elias J, Chao E. Outcome of periacetabular osteotomy: joint contact pressure calculation using standing AP radiographs, 12 patients followed for average 2 years. Acta Orthop Jun, 2005; 76(3)303–13
- Crockarell J, Jr., Trousdale R T, Cabanela M E, Berry D J. Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin Orthop Jun, 1999, 363: 45–53
- Hipp J A, Sugano N, Millis M B, Murphy S B. Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res Jul, 1999, 364: 134–43
- Michaeli D A, Murphy S B, Hipp J A. Comparison of predicted and measured contact pressures in normal and dysplastic hips. Med Eng Phys mar, 1997; 19(2)180–6
- Pedersen E N, Simonsen E B, Alkjaer T, Soballe K. Walking pattern in adults with congenital hip dysplasia: 14 women examined by inverse dynamics. Acta Orthop Scand Feb, 2004; 75(1)2–9
- Pedersen E N, Alkjaer T, Soballe K, Simonsen E B. Walking pattern in 9 women with hip dysplasia 18 months after periacetabular osteotomy. Acta Orthop Apr, 2006; 77(2)203–8
- Anda S. Evaluation of the Hip Joint by Computed Tomography and Ultrasonography. University of Trondheim, Faculty of Medicine, Trondheim 1991
- Pirpiris M, Payman K R, Otsuka N Y. The assessment of acetabular index: is there still a place for plain radiography?. J Pediatr Orthop may, 2006; 26(3)310–5
- Matta J M, Stover M D, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Jun, 1999, 363: 21–32
- Sneppen O, Bünger C, Hvid I. Ortopædisk kirurgi5. FADL, Copenhagen 2002
- Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. Hip dysplasia and osteoarthrosis: a survey of 4151 subjects from the Osteoarthrosis Substudy of the Copenhagen City Heart Study. Acta Orthop Apr, 2005; 76(2)149–58
- Smith R W, Egger P, Coggon D, Cawley M I, Cooper C. Osteoarthritis of the hip joint and acetabular dysplasia in women. Ann Rheum Dis mar, 1995; 54(3)179–81
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip joint. Acta Orthop Scand Suppl 1939; 58: 1–132
- Fredensborg N. The CE angle of normal hips. Acta Orthop Scand Aug, 1976; 47(4)403–5
- Croft P, Cooper C, Wickham C, Coggon D. Osteoarthritis of the hip and acetabular dysplasia. Ann Rheum Dis may, 1991; 50(5)308–10
- Yanagimoto S, Hotta H, Izumida R, Sakamaki T. Long-term results of Chiari pelvic osteotomy in patients with developmental dysplasia of the hip: indications for Chiari pelvic osteotomy according to disease stage and femoral head shape. J Orthop Sci Nov, 2005; 10(6)557–63
- Inoue K, Wicart P, Kawasaki T, Huang J, Ushiyama T, Hukuda S, et al. Prevalence of hip osteoarthritis and acetabular dysplasia in french and japanese adults. Rheumatology (Oxford) Jul, 2000; 39(7)745–8
- Lavy C B, Msamati B C, Igbigbi P S. Racial and gender variations in adult hip morphology. Int Orthop 2003; 27(6)331–3
- Trumble S J, Mayo K A, Mast J W. The periacetabular osteotomy. Minimum 2 year followup in more than 100 hips. Clin Orthop Jun, 1999, 363: 54–63
- Anda S, Terjesen T, Kvistad K A, Svenningsen S. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr Jan, 1991; 15(1)115–20
- Murphy S B, Kijewski P K, Millis M B, Harless A. Acetabular dysplasia in the adolescent and young adult. Clin Orthop Dec, 1990, 261: 214–23
- Kim S S, Frick S L, Wenger D R. Anteversion of the acetabulum in developmental dysplasia of the hip: analysis with computed tomography. J Pediatr Orthop Jul, 1999; 19(4)438–42
- Li P L, Ganz R. Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res Nov, 2003, 416: 245–53
- Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br mar, 1999; 81(2)281–8
- Nishii T, Sugano N, Sato Y, Tanaka H, Miki H, Yoshikawa H. Three-dimensional distribution of acetabular cartilage thickness in patients with hip dysplasia: a fully automated computational analysis of MR imaging. Osteoarthritis Cartilage Aug, 2004; 12(8)650–7
- Jacobsen S, Romer L, Soballe K. Degeneration in dysplastic hips. A computer tomography study. Skeletal Radiol Dec, 2005; 34(12)778–84
- Buly R L, Pellicci P M, Ghelman B. Bilateral femoral retroversion associated with acetabular dysplasia. Clin Orthop Relat Res Jan, 1991, 262: 192–7, A case report
- Murphy S B, Ganz R, Muller M E. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am Jul, 1995; 77(7)985–9
- Trousdale R T, Ekkernkamp A, Ganz R, Wallrichs S L. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am Jan, 1995; 77(1)73–85
- Klaue K, Durnin C W, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br May, 1991; 73(3)423–9
- Jacobsen S. Adult hip dysplasia and osteoarthritis. Studies in radiology and clinical epidemiology. Acta Orthop Suppl Dec, 2006; 77(324)1–37
- McCarthy J C, Noble P C, Schuck M R, Wright J, Lee J. The watershed labral lesion: its relationship to early arthritis of the hip. J Arthroplasty Dec, 2001; 16(8 Suppl 1)81–7
- Noguchi Y, Miura H, Takasugi S, Iwamoto Y. Cartilage and labrum degeneration in the dysplastic hip generally originates in the anterosuperior weight-bearing area: an arthroscopic observation. Arthroscopy Jul, 1999; 15(5)496–506
- Yoshida M, Konishi N. Subchondral cysts arise in the anterior acetabulum in dysplastic osteoarthritic hips. Clin Orthop Relat Res Nov, 2002, 404: 291–301
- Lanyon P, Muir K, Doherty S, Doherty M. Assessment of a genetic contribution to osteoarthritis of the hip: sibling study. BMJ Nov 11, 2000; 321(7270)1179–83
- Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V. The Bernese periacetabular osteotomy: clinical, radiographic and mechanical 7-15-year follow-up of 26 hips. Acta Orthop Dec, 2005; 76(6)833–40
- Mavcic B, Antolic V, Brand R, Iglic A, Kralj-Iglic V, Pedersen D R. Peak contact stress in human hip during gait. Pflugers Arch 2000; 440(5 Suppl)R177–R178
- Mavcic B, Antolic V, Brand R, Iglic A, Ipavec M, Kralj-Iglic V, et al. Weight bearing area during gait in normal and dysplastic hips. Pflugers Arch 2000; 439(3 Suppl)R213–R214
- Wiberg G. A measuring method for distinguishing between a normal and a maldeveloped acetabulum. Acta Chir Scand 1939; 83(suppl 1)28–38
- Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect 1986; 35: 119–28
- Turgeon T R, Phillips W, Kantor S R, Santore R F. The role of acetabular and femoral osteotomies in reconstructive surgery of the hip: 2005 and beyond. Clin Orthop Relat Res Dec, 2005; 441: 188–99
- Harris W H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am Jun, 1969; 51(4)737–55
- Tönnis D. Congenital dysplasia and dislocation of the hip in children and adults. Springer, Berlin Heidelberg New york 1987
- Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. The relationship of hip joint space to self reported hip pain. A survey of 4.151 subjects of the Copenhagen City Heart Study: the Osteoarthritis Sub-study. Osteoarthritis Cartilage Sep, 2004; 12(9)692–7
- Wenger D R, Bomar J D. Human hip dysplasia: evolution of current treatment concepts. J Orthop Sci 2003; 8(2)264–71
- MacDonald S J, Hersche O, Ganz R. Periacetabular osteotomy in the treatment of neurogenic acetabular dysplasia. J Bone Joint Surg Br Nov, 1999; 81(6)975–8
- Nakamura Y, Naito M, Akiyoshi Y, Shitama T. Acetabular cysts heal after successful periacetabular osteotomy. Clin Orthop Relat Res Jan, 2007; 454: 120–6
- Parvizi J, Burmeister H, Ganz R. Previous Bernese periacetabular osteotomy does not compromise the results of total hip arthroplasty. Clin Orthop Relat Res Jun, 2004, 423: 118–22
- Trousdale R T, Cabanela M E, Berry D J, Wenger D E. Magnetic resonance imaging pelvimetry before and after a periacetabular osteotomy. J Bone Joint Surg Am Apr, 2002; 84-A(4)552–6
- Siebenrock K A, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res Jun, 1999, 363: 9–20
- Aminian A, Mahar A, Yassir W, Newton P, Wenger D. Freedom of acetabular fragment rotation following three surgical techniques for correction of congenital deformities of the hip. J Pediatr Orthop Jan, 2005; 25(1)10–3
- Steel H H. Triple osteotomy of the innominate bone. J Bone Joint Surg Am mar, 1973; 55(2)343–50
- Soballe K. Pelvic osteotomy for acetabular dysplasia. Acta Orthop Scand Apr, 2003; 74(2)117–8
- Clohisy J C, Barrett S E, Gordon J E, Delgado E D, Schoenecker P L. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. Surgical technique. J Bone Joint Surg Am mar, 2006; 88(Suppl 1 Pt 1)65–83
- Troelsen A. Minimally Invasive Trans-sartorial Approach. American Academy of Orthopaedic Surgeons 2007 Annual Meeting, San Diego, Ca, 2007
- Trousdale R T, Cabanela M E. Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop Scand Apr, 2003; 74(2)119–26
- Davey J P, Santore R F. Complications of periacetabular osteotomy. Clin Orthop Jun, 1999, 363: 33–7
- Myers S R, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res Jun, 1999, 363: 93–9
- Nyengaard J R. Stereologic methods and their application in kidney research. J Am Soc Nephrol may, 1999; 10(5)1100–23
- Gundersen H J, Jensen E B, Kieu K, Nielsen J. The efficiency of systematic sampling in stereology–reconsidered. J Microsc mar, 1999; 193(Pt 3)199–211
- Joergensen B H. CT-Teknik. Indføring i CT-teknikkens grundprincipper7. Utopia, Ballerup 2004
- Pauwels F. Anat Anz 1976; 139(3)213–20, [Developmental effects of the functional adaptation of bone]
- Schild H H. MRI made easy. Schering AG, Berlin 1990
- Wulfsohn D, Nyengaard J R, Tang Y. Postnatal growth of cardiomyocytes in the left ventricle of the rat. Anat Rec A Discov Mol Cell Evol Biol mar, 2004; 277(1)236–47
- Basic Principles of MR Imaging. Phillips Medical systems. 2005
- Jensen E B, Gundersen H J, Osterby R. Determination of membrane thickness distribution from orthogonal intercepts. J Microsc Jan, 1979; 115(1)19–33
- Gundersen H J, Jensen T B, Osterby R. Distribution of membrane thickness determined by lineal analysis. J Microsc may, 1978; 113(1)27–43
- Nagels J, Valstar E R, Stokdijk M, Rozing P M. Patterns of loosening of the glenoid component. J Bone Joint Surg Br Jan, 2002; 84(1)83–7
- Vrooman H A, Valstar E R, Brand G J, Admiraal D R, Rozing P M, Reiber J H. Fast and accurate automated measurements in digitized stereophotogrammetric radiographs. J Biomech may, 1998; 31(5)491–8
- Valstar E R, Vrooman H A, Toksvig-Larsen S, Ryd L, Nelissen R G. Digital automated RSA compared to manually operated RSA. J Biomech Dec, 2000; 33(12)1593–9
- Valstar E R. Digital Roentgen Stereophotogrammetry: Development, Validation, and Clinical Application. Leiden University. 2001
- Kaptein B L, Valstar E R, Stoel B C, Rozing P M, Reiber J H. A new model-based RSA method validated using CAD models and models from reversed engineering. J Biomech Jun, 2003; 36(6)873–82
- Kiss J, Murray D W, Turner-Smith A R, Bulstrode C J. Roentgen stereophotogrammetric analysis for assesing migration of total hip replacement femoral components. Proc Inst Mech Eng [H] 1995; 66(5)169–75
- Valstar E R, Gill R, Ryd L, Flivik G, Borlin N, Karrholm J. Guidelines for standardization of radiostereometry (RSA) of implants. Acta Orthop Aug, 2005; 76(4)563–72
- Karrholm J. Roentgen stereophotogrammetry. Review of orthopedic applications. Acta Orthop Scand Aug, 1989; 60(4)491–503
- Delaunay S, Dussault R G, Kaplan P A, Alford B A. Radiographic measurements of dysplastic adult hips. Skeletal Radiol Feb, 1997; 26(2)75–81
- Tallroth K, Lepisto J. Computed tomography measurement of acetabular dimensions: normal values for correction of dysplasia. Acta Orthop Aug, 2006; 77(4)598–602
- Jacobsen S, Sonne-Holm S, Lund B, Soballe K, Kiaer T, Rovsing H, et al. Pelvic orientation and assessment of hip dysplasia in adults. Acta Orthop Scand Dec, 2004; 75(6)721–9
- Tonnis D. Normal values of the hip joint for the evaluation of X-rays in children and adults. Clin Orthop Relat Res Sep, 1976, 119: 39–47
- Anda S, Svenningsen S, Grontvedt T, Benum P. Pelvic inclination and spatial orientation of the acetabulum. A radiographic, computed tomographic and clinical investigation. Acta Radiol Jul, 1990; 31(4)389–94
- Auleley G R, Rousselin B, Ayral X, Edouard-Noel R, Dougados M, Ravaud P. Osteoarthritis of the hip: agreement between joint space width measurements on standing and supine conventional radiographs. Ann Rheum Dis Sep, 1998; 57(9)519–23
- Tan L, Aktas S, Copuroglu C, Ozcan M, Ture M. Reliability of radiological parameters measured on anteroposterior pelvis radiographs of patients with developmental dysplasia of the hip. Acta Orthop Belg Oct, 2001; 67(4)374–9
- Troelsen A, Jacobsen S, Romer L, Soballe K. Weight-bearing Anteroposterior Pelvic Radiographs are Recommended in DDH Assessment. Clin Orthop Relat Res Apr, 2008; 466(4)813–9
- Madanat R, Makinen T J, Moritz N, Mattila K T, Aro H T. Accuracy and precision of radiostereometric analysis in the measurement of three-dimensional micromotion in a fracture model of the distal radius. J Orthop Res mar, 2005; 23(2)481–8
- Lucas J, Cooke F W, Friis E A. A Primer of Biomechanics. Springer-Verlag, New York 1999
- Pompe B, Antolic V, Iglic A, Kralj-Iglic V, Mavcic B, Smrke D. Evaluation of biomechanical status of dysplastic human hips. Pflugers Arch 2000; 440(5 Suppl)R202-R203
- Haddad F S, Garbuz D S, Duncan C P, Janzen D L, Munk P L. CT evaluation of periacetabular osteotomies. J Bone Joint Surg Br may, 2000; 82(4)526–31
- Schmidt R, Muller L, Kress A, Hirschfelder H, Aplas A, Pitto R P. A computed tomography assessment of femoral and acetabular bone changes after total hip arthroplasty. Int Orthop 2002; 26(5)299–302
- Wright J M, Pellicci P M, Salvati E A, Ghelman B, Roberts M M, Koh J L. Bone density adjacent to press-fit acetabular components. A prospective analysis with quantitative computed tomography. J Bone Joint Surg Am Apr, 2001; 83-A(4)529–36
- Lengsfeld M, Gunther D, Pressel T, Leppek R, Schmitt J, Griss P. Validation data for periprosthetic bone remodelling theories. J Biomech Dec, 2002; 35(12)1553–64
- Ding M. Age variations in the properties of human tibial trabecular bone and cartilage. Acta Orthop Scand Suppl Jun, 2000; 292: 1–45
- Burr D B, Turner C H, Naick P, Forwood M R, Ambrosius W, Hasan M S, et al. Does microdamage accumulation affect the mechanical properties of bone?. J Biomech Apr, 1998; 31(4)337–45
- Hasegawa Y, Fukatsu H, Matsuda T, Iwase T, Iwata H. Magnetic resonance imaging in osteoarthrosis of the dysplastic hip. Arch Orthop Trauma Surg 1996; 115(5)243–8
- Kim Y J, Jaramillo D, Millis M B, Gray M L, Burstein D. Assessment of early osteoarthritis in hip dysplasia with delayed gadolinium-enhanced magnetic resonance imaging of cartilage. J Bone Joint Surg Am Oct, 2003; 85-A(10)1987–92
- Nishii T, Sugano N, Tanaka H, Nakanishi K, Ohzono K, Yoshikawa H. Articular cartilage abnormalities in dysplastic hips without joint space narrowing. Clin Orthop Relat Res Feb, 2001, 383: 183–90
- Nakanishi K, Tanaka H, Nishii T, Masuhara K, Narumi Y, Nakamura H. MR evaluation of the articular cartilage of the femoral head during traction. Correlation with resected femoral head. Acta Radiol Jan, 1999; 40(1)60–3
- Nishii T, Nakanishi K, Sugano N, Masuhara K, Ohzono K, Ochi T. Articular cartilage evaluation in osteoarthritis of the hip with MR imaging under continuous leg traction. Magn Reson Imaging Oct, 1998; 16(8)871–5
- Mavcic B, Pompe B, Antolic V, Daniel M, Iglic A, Kralj-Iglic V. Mathematical estimation of stress distribution in normal and dysplastic human hips. J Orthop Res Sep, 2002; 20(5)1025–30
- Horii M, Kubo T, Hirasawa Y. Radial MRI of the hip with moderate osteoarthritis. J Bone Joint Surg Br Apr, 2000; 82(3)364–8
- Kawabe K, Konishi N. Three-dimensional modeling of cartilage thickness in hip dysplasia. Clin Orthop Relat Res Apr, 1993, 289: 180–5
- Nakanishi K, Tanaka H, Sugano N, Sato Y, Ueguchi T, Kubota T, et al. MR-based three-dimensional presentation of cartilage thickness in the femoral head. Eur Radiol 2001; 11(11)2178–83
- McGibbon C A, Bencardino J, Palmer W E. Subchondral bone and cartilage thickness from MRI: effects of chemical-shift artifact. MAGMA Feb, 2003; 16(1)1–9
- Babis G C, Trousdale R T, Jenkyn T R, Kaufman K. Comparison of two methods of screw fixation in periacetabular osteotomy. Clin Orthop Relat Res Oct, 2002, 403: 221–7
- Yassir W, Mahar A, Aminian A, Newton P, Wenger D. A comparison of the fixation stability of multiple screw constructs for two types of pelvic osteotomies. J Pediatr Orthop Jan, 2005; 25(1)14–7
- Hansson L I, Olsson T H, Selvik G, Sundén G. A Roentgen Stereophotogrammetric Investigation of Innominate Osteotomy (Salter). Acta Orthop Scand 1978; 49: 68–72
- Ragnarsson J I, Eliasson P, Karrholm J, Lundstrom B. The accuracy of measurements of femoral neck fractures. Conventional radiography versus roentgen stereophotogrammetric analysis. Acta Orthop Scand Apr, 1992; 63(2)152–6
- Ahl T, Dalen N, Lundberg A, Wykman A. Biodegradable fixation of ankle fractures. A roentgen stereophotogrammetric study of 32 cases. Acta Orthop Scand Apr, 1994; 65(2)166–70
- Mattsson P, Larsson S. Stability of internally fixed femoral neck fractures augmented with resorbable cement. A prospective randomized study using radio-stereometry. Scand J Surg 2003; 92(3)215–9
- Mattsson P, Larsson S. Unstable trochanteric fractures augmented with calcium phosphate cement. A prospective randomized study using radiostereometry to measure fracture stability. Scand J Surg 2004; 93(3)223–8
- Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology (Oxford) Feb, 2005; 44(2)211–8
- Jacobsen S, Sonne-Holm S, Soballe K, Gebuhr P, Lund B. Joint space width in dysplasia of the hip: a case-control study of 81 adults followed for ten years. J Bone Joint Surg Br Apr, 2005; 87(4)471–7