Abstract
Introduction
Hip dysplasia is characterized by an excessively oblique and shallow acetabulum with insufficient coverage of the femoral head. It is a known cause of pain and the development of early osteoarthritis in young adults. The periacetabular osteotomy is the joint-preserving treatment of choice in young adults with symptomatic hip dysplasia. The surgical aim of this extensive procedure is to reorient the acetabulum to improve coverage and eliminate the pathological hip joint mechanics. Intraoperative assessment of the achieved acetabular reorientation is therefore crucial. The “classic” surgical approaches for the periacetabular osteotomy inflict extensive trauma to the tissues and some involve detachment of muscles. The type of surgical approach may affect the occurrence of complications, duration of surgery, intraoperative blood loss, transfusion requirements, and length of hospital stay. The aims of the PhD thesis were I) to assess the outcome of a new, minimally invasive transsartorial approach for periacetabular osteotomy; II) to compare the minimally invasive approach with the previously used “classic” ilioinguinal approach; and III) to assess the reliability of a novel device for intraoperative assessment of the achieved acetabular reorientation.
Methods
Three studies underly this PhD thesis. In studies I and II, the experience with the minimally invasive and ilioinguinal approaches was retrospectively assessed by database inquiry and evaluation of radiographic material. Data regarding patient demographics, patient history, intraoperative measures and complications was recorded in a validated database. Center-edge and acetabular index angles were measured in preoperative and postoperative pelvic radiographs to assess preoperative dysplasia and the achieved acetabular reorientation. The well-defined study groups consisted of 94 and 263 periacetabular osteotomies in studies I and II, respectively. In study III, intraoperative angle measurements were carried out prospectively in 35 periacetabular osteotomies. The obtained measures (center-edge and acetabular index angles) were compared with those of postoperative pelvic radiographs. Furthermore, a cadaver study was conducted to evaluate intra- and interobserver variability of the device and to assess whether pelvic positioning influenced the variability of measurements. The applied methodology was critically reviewed.
Results
Study I – The minimally invasive approach had the following outcome. The mean duration of surgery was 73 min and the median intraoperative blood loss was 250 ml. Blood transfusion was required following 3% of the procedures. There were no cases of moderate or severe technical and neurovascular complications, and the achieved center-edge and acetabular index angles suggest that optimal reorientation can be achieved. Hip joint survival with total hip arthroplasty as the end point was 98% at 4.3 years.
Study II – When compared with the outcome of the ilioinguinal approach, the procedures performed by using the minimally invasive approach had a statistically significant shorter duration of surgery, less intraoperative blood loss and hemoglobin reduction, and fewer transfusion requirements. The achieved reorientation was comparable between groups. There were no cases of moderate or severe complications in the minimally invasive group and three cases (3%) of arterial thrombosis in the ilioinguinal group. At follow-up 4.9 years after hip joint surgery, survival rates were 97% in the minimally invasive group and 93% in the ilioinguinal group.
Study III – Intraoperatively obtained angle measures differed less than ±5˚ from measurements on postoperative pelvic radiographs, and the intra- and interobserver variability of the device was confined well within ±5˚. Positioning did not influence the variation of angle measurements beyond intraobserver variability of the device.
Interpretation
The new minimally invasive transsartorial approach appears to be a safe technique, allowing optimal acetabular reorientation, and seems to minimize tissue trauma. In addition, short-term hip joint survival rate is encouraging. The outcome compares favorably with that of the ilioinguinal approach, and the results support continued use of the minimally invasive approach for periacetabular osteotomy. Optimal reorientation of the acetabulum is crucial in periacetabular osteotomy. The novel measuring device is a potentially helpful tool for intraoperative assessment of center-edge and acetabular index angels. It is simple to use and facilitates repeated reliable angle measurements during acetabular reorientation, making intraoperative radiographs unnecessary. The new, minimally invasive approach and the novel measuring device represent important surgical advances in contemporary periacetabular osteotomy.
List of papers
The PhD thesis is based on the following papers, referred to in the text by Roman numerals (I–III):
Troelsen A, Elmengaard B, Søballe K.
A new minimally invasive transsartorial approach for periacetabular osteotomy.
J Bone Joint Surg Am 2008; 90: 493-498.
Troelsen A, Elmengaard B, Søballe K.
Comparison of the minimally invasive and the ilioinguinal approaches for periacetabular osteotomy.
Acta Orthop 2008; 79: 777-784.
Troelsen A, Elmengaard B, Rømer L, Søballe K.
Reliable angle assessment during periacetabular osteotomy with a novel device.
Clin Orthop Relat Res 2008; 466: 1169-1176.
Acknowledgements
The studies forming the basis for this PhD thesis were performed during a research fellowship at the Orthopaedic Research Unit, University Hospital of Aarhus, in the period 2006 to 2008. My employment as a research fellow was financed primarily by a grant from the Danish Rheumatism Association and through my clinical employment at the Department of Orthopaedic Surgery, University Hospital of Aarhus. Contributions were also made by the Guildal Foundation and Helga and Peter Kornings Foundation.
I thank my co-authors, supervisors, and colleagues for their contributions. I am especially indebted to Professor Kjeld Søballe, who has given me excellent supervision, great opportunities, the best possible working conditions, and been patient with my impatience. I look forward to our future cooperation. I thank Brian Elmengaard, MD, PhD, for excellent supervision and introducing me to research in Aarhus; Steffen Jacobsen, MD, DMSc, for shared insights on the topic of hip dysplasia and his always honest opinions; Lone Rømer, MD, for important contributions and discussions regarding radiological aspects of hip dysplasia; and Michael Brix, MD, for taking such personal interest in development of my general orthopaedic surgical skills.
I wish to thank those who make “everything possible”: Karen Fousing, Tina Stenumgaard, Jette Kirkegaard, Margit Jensen, and the staff in the archives for always providing fast, careful, and excellent solutions; Søren Johnsen, Alma Pedersen, Anders Riis and Frank Mehnert, for their great contribution to my work with the PAO Database; and Peter Holm-Nielsen for providing access to the cadaver specimen.
Finally, I dedicate this thesis to my wife Signe and our children Clara and Villads. Thank you!
Conflicts of interest
No conflicts of interest declared
Introduction
Hip dysplasia in young adults
Etiology
Hip dysplasia is a congenital or early developmental condition. It exists as an independent condition with primary development of the dysplastic pathomorphology. Dysplastic changes also develop secondary to congenital dislocation of the hip, Legg-Calvé-Perthes disease, or generalized conditions with neuromuscular affection, such as cerebral palsy and Down's syndrome (Citation[1-4]). Hip dysplasia develops due to a mismatch in the normal containment of the femoral head in the acetabulum. This mechanism is influenced by bony malformations, abnormalities in muscular and soft tissue tension across the hip joint, intrauterine mechanical factors, and possibly genetic predisposition (Citation[1],Citation[5-7]).
Pathomorphology
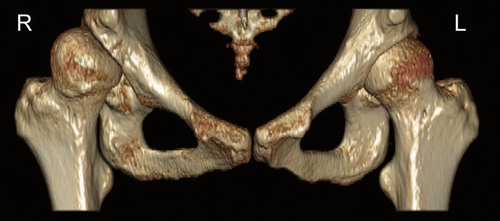
Hip dysplasia is initially diagnosed and assessed on weight-bearing anteroposterior pelvic radiographs (Citation[8]). In cases of borderline dysplasia or for preoperative planning, the dysplastic anatomy is assessed three-dimensionally by CT scanning (Citation[9-11]). In hip dysplasia, acetabular and proximal femoral dysplasia coexists. Acetabular dysplasia is characterized by an excessively oblique and shallow acetabulum with insufficient coverage of the femoral head laterally and anteriorly (). The proximal femoral dysplasia shows varying characteristics depending on the condition. In primary development of hip dysplasia or following successful reduction of congenital hip dislocation, the following characteristics coexist in varying degrees: lateralization and ovoid shaping of the femoral head, increased femoral neck anteversion, and increased neck-shaft angle (Citation[1],Citation[2],Citation[12-14]). Childhood Legg-Calvé-Perthes disease may results in characteristic widening of the femoral head. Development of hip dysplasia under influence of a neuromuscular disorder may result in severe dysplasia with lateral subluxation of the femoral head or dislocation of the hip joint (Citation[1-4]). Sequelae of Legg-Calvé-Perthes disease, persisting hip dislocation, and neuromuscular disorders will not be dealt with in this thesis.
Radiographic indices and diagnosis
Historically, radiographic indices for description of the dysplastic pathomorphology have been developed for conventional anteroposterior pelvic radiographs. In 1939, Wiberg described in his doctoral thesis the center-edge angle, which is still the most commonly used radiographic parameter in clinical and epidemiological studies of hip dysplasia (Citation[15]). The center-edge angle describes the position of the femoral head relative to the acetabulum and is widely accepted for diagnostic purposes (). A clear-cut definition of certain hip dysplasia does not exist, and suggested cut-off values are based on arbitrary grounds with no correlation to the clinical status of patients. However, in the majority of studies a center-edge angle either <20° or <25° is chosen, with the latter definition, or an approximation to it, prevailing in many clinical studies reporting surgical outcome (Citation[16-22]). In daily clinical work and in this thesis, a center-edge angle < 25° defines hip dysplasia. Another widely adopted radiographic angle measure, describing the obliquity of the weight-bearing sclerotic zone of the acetabulum, is the acetabular index of Tönnis (Citation[23]) (). These two parameters are not only used for diagnostic purposes, but are assessed during reorienting joint-preserving surgery in hip dysplasia (periacetabular osteotomy) to ascertain whether the intended reorientation has been achieved (Citation[16],Citation[24-27]). Additionally, the acetabular version should be assessed as part of preoperative planning and during surgery to ascertain appropriate anteversion after acetabular reorientation (). Other radiographic parameters have been described (Citation[8],Citation[23],Citation[28-33]) but seem less widespread, at least for diagnostic and surgical purposes in adult hip dysplasia. Three-dimensional CT scanning allows informative assessment of coverage deficiencies, the acetabular version, femoral neck version, and joint degeneration (Citation[12-14],Citation[34]).
Symptoms and the osteoarthritic pathway
The debut of symptoms seems related to soft tissue overload and/or tearing of the acetabular labrum caused by increased contact pressures and possible “shearing” femoroacetabular impingement (Citation[35-40]). In classic cases, the symptomatic patient is an otherwise healthy 20- to 40-year old female. Prior to debut of symptoms, most patients have an average level of activity. The most frequent complaint is of sharp pain located in the groin. Patients may experience fatigue and limping. Range of motion in the hip is often normal and may show increased internal rotation if femoral neck anteversion is excessive (Citation[41],Citation[42]).
By using the center-edge angle as a diagnostic discriminator (either < 20° or < 25°), the estimated prevalence in Caucasian populations is approximately 3.5%–5.5% (Citation[43-45]). Hip dysplasia is recognized as a risk factor for the development of osteoarthritis; however, few people develop premature symptoms and osteoarthritis as young adults (Citation[45],Citation[46]). Possible mechanisms have been described, but it remains unclear why some people seem predisposed. An epidemiological estimate from the Copenhagen City Heart Study cohort shows that hip dysplasia is approximately equally distributed between genders (Citation[45]). However, approximately 75% to 80% of patients undergoing surgery with hip dysplasia are females (Citation[16],Citation[17],Citation[26],Citation[47],Citation[48]), suggesting that females are at higher risk of soft tissue overload and subsequent development of osteoarthritis. As shown in studies by Wiberg (Citation[15]), Cooperman et al. (Citation[49]), and others (Citation[50],Citation[51]), severe dysplasia will in most cases eventually cause osteoarthritis, whereas moderate and mild dysplasia do not necessarily affect hip joint integrity (Citation[46]). Research in recent years has shed light on possible mechanisms interacting with the dysplastic pathomorphology to initiate the osteoarthritic pathway. Tearing of the acetabular labrum is frequently seen in symptomatic patients, in both the absence and presence of joint degeneration (Citation[36-38],Citation[40]). It can be hypothesized that femoroacetabular impingement results in repeated micro trauma and tearing of the acetabular labrum, thereby exposing the watershed zone of the acetabulum and causing cartilage delamination (Citation[35],Citation[52-56]). The pathomorphology of hip dysplasia causes increased contact pressures in the joint, which will further contribute to joint overload and tearing of the acetabular labrum and adjacent soft tissue (Citation[57-59]). At early stages after debut of pain, conventional radiographic signs of osteoarthritis are normally absent (Citation[40]).
Surgical treatment
Until the early 1980s, several reorienting triple or spherical acetabular osteotomies for treatment of hip dysplasia had been introduced (Citation[23],Citation[60],Citation[61]). None of these techniques gained popularity as the obvious joint preserving treatment in young adults with hip dysplasia. In 1983, a group lead by Professor Reinhold Ganz from Bern, Switzerland, started the development of a new periacetabular osteotomy for the treatment of hip dysplasia (Citation[16]). This technique has become the joint preserving treatment of choice in young adults with symptomatic hip dysplasia (Citation[17],Citation[20],Citation[22],Citation[26],Citation[27],Citation[48],Citation[62-66]). It is often referred to as the “Bernese” or “Ganz” periacetabular osteotomy.
The periacetabular osteotomy
In the periacetabular osteotomy, the acetabulum is reoriented to enhance the coverage of the femoral head, and the aim is to achieve congruity, to stabilize the hip joint, to medialize the hip joint center, and to reduce contact pressures (Citation[16],Citation[62],Citation[67],Citation[68]) (). This will relieve pain, improve function, and is likely to prevent further overload of the labrum, cartilage, and soft tissues, thereby delaying or preventing the development of osteoarthritis (Citation[17],Citation[20],Citation[26],Citation[48],Citation[63],Citation[64]). As outlined by Ganz et al. (Citation[16]), the periacetabular osteotomy has several technical advantages compared with existing techniques: the posterior column remains intact leaving the pelvis stable, allowing partial weight bearing immediately postoperative and minimal internal fixation; extensive three-dimensional mobilization of the acetabular fragment is possible; the blood supply of the acetabulum is unaffected; and the dimensions of the true pelvis are maintained. In general, the periacetabular osteotomy is performed in patients after closure of the triradiate cartilage, but the exact indications for periacetabular osteotomy may differ between institutions. For daily clinical practice, the following indications have been developed: 1) symptomatic acetabular dysplasia defined by persistent pain; 2) a center-edge angle of <25˚; 3) a congruent hip joint; 4) maintained range of motion with hip flexion of >110˚ and; 5) preoperative osteoarthritis corresponding to Tönnis grades 0-1.
Surgical approaches and technique
Since the development of the periacetabular osteotomy, several surgical approaches have been used. Most surgeons prefer the ilioinguinal or modified Smith-Petersen (iliofemoral) approaches (Citation[18],Citation[20],Citation[24],Citation[63],Citation[69]) (). A short description of the surgical techniques is given in Appendix A. These “classic” approaches inflict an extensive trauma to the tissues, and some involve detachment of muscles, such as the rectus femoris and sartorius. The type of surgical approach may affect the occurrence of complications, duration of surgery, intraoperative blood loss, transfusion requirements, the ability to obtain an optimal acetabular reorientation, and the length of hospital stay (Citation[20],Citation[69],Citation[70]). The learning curve associated with the periacetabular osteotomy is well documented, and technical and neurovascular complications have been reported by experienced surgeons (Citation[16],Citation[26],Citation[68-71]).
Acetabular reorientation and assisting tools
Achieving an optimal acetabular reorientation is a cornerstone of the periacetabular osteotomy. Under- or overcorrection of the acetabulum can cause a feeling of instability or impingement, respectively (Citation[27],Citation[71],Citation[72]), and negatively influence the joint preserving goals of the procedure (Citation[20],Citation[64],Citation[65]). The aim of the reorientation is to achieve an acetabular index angle between 0° and 10°, a center-edge angle between 30° and 40°, and appropriate acetabular anteversion.
Suggested methods for the intraoperative assessment of the acetabular reorientation have inherent limitations. Angle measures can be assessed by taking anteroposterior pelvic radiographs during reorientation of the acetabulum. Several radiographs may be necessary, and the surgeon has to wait until the radiographs have been developed and the angles measured. Alternatively, the assessment can be made by eye by using fluoroscopy, but this approach is qualitative, and measuring errors are unknown. Image-guided techniques seemingly facilitate surgery but without improving acetabular correction, and they are relatively expensive (Citation[73-76]).
Outcomes of surgery
Studies reporting the outcome of periacetabular osteotomy often represent heterogenic patient populations in terms of diagnosis, severity of dysplasia, preoperative osteoarthritis, simultaneous surgical procedures, and duration of follow-up (Citation[17-20],Citation[22],Citation[26],Citation[48],Citation[62-65],Citation[77-81]). The modified Smith-Petersen, ilioinguinal, and direct anterior approaches have been used (Citation[17-20],Citation[22],Citation[26],Citation[48],Citation[63-66],Citation[70],Citation[79]).
Parameters such as duration of surgery, intraoperative blood loss, and transfusion requirements reflect the invasive characteristics of the periacetabular osteotomy (). The mean duration of surgeries are reported to be approximately 3 to 4½ hours (Citation[18],Citation[20],Citation[63],Citation[65],Citation[70]) and mean intraoperative blood losses to be approximately 700 to 2300 ml (Citation[18],Citation[20],Citation[26],Citation[62],Citation[63],Citation[65],Citation[80]). One study reports the requirement of a mean of four portions of blood following all procedures (Citation[65]). Length of hospital stay is rarely reported; however, approximately 5 to 10 days of admission seem normal (Citation[18],Citation[63],Citation[80]). Moderate and severe neurovascular complications are most frequently reported to occur at a rate of approximately 0% to 5% (Citation[16-18],Citation[20],Citation[22],Citation[26],Citation[48],Citation[63],Citation[77],Citation[82]). The learning curve related to the occurrence of complications (Citation[16],Citation[26],Citation[68-70]) affects the outcome in some studies. Periacetabular osteotomy can in classical terms, be considered and extensive surgical procedure with a risk of disabling complications.
Table 1. Summary of studies reporting duration of surgery, blood loss, transfusion requirements, or length of hospital stay
In most studies, the aim of the reorientation was achieved with regard to mean postoperative center-edge and acetabular index angles (Citation[17],Citation[48],Citation[62-64],Citation[77],Citation[79]). The short-term hip joint survival rates are in most studies >90%. Few studies report medium and long-term hip joint survival (Citation[62],Citation[64],Citation[65]). Recently, a hip joint survival rate of 60.5% has been reported at a mean follow-up of 20.4 years (Citation[64]). Clinical scores improve following periacetabular osteotomy, and there is evidence that significant improvements last up to 10 years (Citation[65]).
Conservative treatment?
Whereas many patients with asymptomatic mild and moderate hip dysplasia will not develop osteoarthritis at an early age (Citation[46]), it remains unclear whether this is the case in some symptomatic patients with persistent hip pain. This lack of knowledge could potentially lead to the performance of unnecessary surgery in marginal cases. Conservative treatment might then be a treatment option, but the selection criteria are unknown. However, when patients with persistent symptoms are referred, they often suffer moderate or severe pain which affects daily living, and given the ability of the periacetabular osteotomy to relieve pain, improve function, and preserve the joint (Citation[17],Citation[20],Citation[26],Citation[48],Citation[63],Citation[64]), surgery is justified.
Aims of PhD thesis
In the past, periacetabular osteotomy has been associated with extensive surgical approaches with potentially severe complications and the absence of simple, reliable, and validated tools for intraoperative assessment of the acetabular reorientation. This obviously leaves room for advances in the surgical treatment. A safe surgical procedure with achievement of optimal acetabular reorientation is the surgical mainstay of a successful periacetabular osteotomy.
The overall aim of this PhD thesis was to explore and validate intraoperative methods for the periacetabular osteotomy in order to optimize the surgical treatment of hip dysplasia in young adults. The individual studies that make up the PhD thesis had the following aims:
To assess whether a new, minimally invasive transsartorial approach for periacetabular osteotomy is safe, allows optimal acetabular reorientation, and minimizes tissue trauma. The length of hospital stay, duration of surgery, intraoperative blood loss, hemoglobin reduction, transfusion requirements, hip joint survival, complications, and achieved acetabular reorientation were retrospectively assessed in a study group of 94 periacetabular osteotomies by means of a database inquiry (the PAO Database and the Danish Hip Arthroplasty Register) and the evaluation of radiographic material.
To assess whether the new, minimally invasive approach produces an outcome similar to that of the “classic” ilioinguinal approach for the periacetabular osteotomy. The approaches were compared with respect to the outcome parameters of study I to explore whether the results supported continued use of the minimally invasive approach. Data were assessed retrospectively by a database inquiry and evaluation of radiographic material, similar to that in study I, in a study group of 263 periacetabular osteotomies.
To assess the reliability of a simple, novel measuring device for intraoperative assessment of the achieved acetabular reorientation, in terms of center-edge and acetabular index angle measurements. Prospective intraoperative angle measurements and postoperative pelvic radiographs were made in 35 patients to assess the reliability of the measuring device. In addition, a cadaver study was conducted to assess the intra- and interobserver variability of the device and to assess the influence of variations in pelvic positioning on variability of angle assessment.
Methods: Description and critical considerations
Introduction of new techniques
A new minimally invasive approach
To improve outcome associated with the surgical approach, a new, minimally invasive transsartorial approach for the periacetabular osteotomy was developed by the main supervisor, Kjeld Søballe. The surgical aim of this new approach was to minimize tissue trauma and to allow a safe periacetabular osteotomy with optimal reorientation of the acetabulum. This new approach has been used at our institution since April 2003. The ilioinguinal and modified Smith-Petersen approaches were used previously in successive time periods.
The patient is placed on a radiolucent operating room table in the supine position. The placement of the drapes allows for full mobilization of the lower extremity on the operated side. Fluoroscopic evaluation is necessary throughout the operation, and therefore the pelvis is kept in a neutral position in order to avoid excessive tilting or rotation. The fluoroscopy equipment is positioned to facilitate obtaining the anterior-posterior and 60˚ (false profile) views.
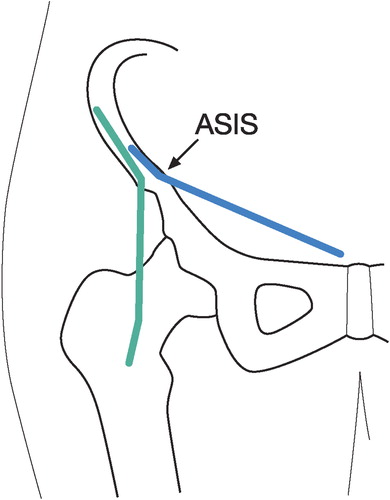
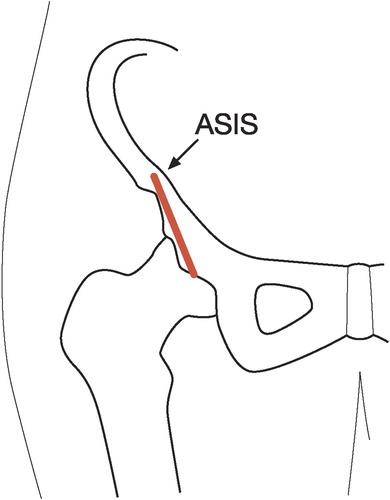
The skin incision begins at the anterior superior iliac spine and continues distally along the sartorius muscle. The length of incision is approximately 7 cm (). The fascia is carefully incised, and the lateral femoral cutaneous nerve isolated and carefully retracted. To facilitate transverse retraction of the soft tissues, a semi flexed position of the hip joint is maintained during performance of the osteotomies. For this purpose a splint is used. A periosteal elevator is placed subperiosteally along the medial aspect of the ilium, starting at the anterior superior iliac spine, and it is advanced until it lies just below the linea terminalis. The inguinal ligament is cut at the attachment to the anterior superior iliac spine, allowing further mobilization of the soft tissues. The periosteal elevator is then pushed medially, splitting the sartorius muscle in the direction of its fibers and the deep fascia of the muscle is cut. The periosteal elevator is then replaced with a blunt retractor positioned along the medial aspect of the ilium to retract the iliopsoas and the medial part of the split sartorius muscles medially (). At this point the osteotomies are performed. The time spend on the approach is approximately 10 minutes. The technique of performing the osteotomies utilizing this approach is described in full length in the appendix to study I.
A novel measuring device for intraoperative angle assessment
To implement a simple and reliable technique for intraoperative assessment of the center-edge and acetabular index angles during acetabular reorientation, the main supervisor developed a measuring device (). The measuring device has been utilized during surgery since September 1999 to facilitate decision making during acetabular reorientation, but was not validated until 2007 (III).
Figure 7. The measuring device is used under fluoroscopy in the anteroposterior plane. It is mounted bilaterally at the anterior-superior iliac spines. The position is secured by inserting small spikes. To secure alignment of the pelvis for angle measurement, a rod connects the spikes. The measuring device is mounted during surgery with the disc for center edge-angle measurement.
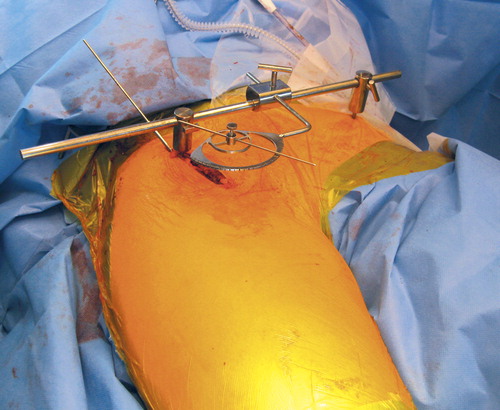
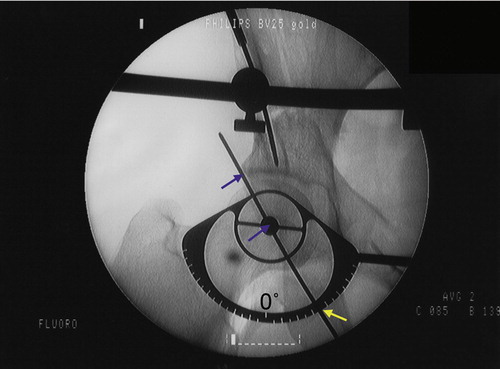
The measuring device is used under fluoroscopy in the anteroposterior plane. It is mounted bilaterally at the anterior-superior iliac spines, and the position is secured by inserting small spikes. To secure alignment of the pelvis for angle measurement, a rod connects the spikes. Adjustable angle measuring discs can be mounted on the alignment rod. Two different angle measuring discs are used: (1) the disc for acetabular index angle measurement is positioned and adjusted until it is placed correctly in relation to the most medial and lateral points of the sclerotic acetabular roof; and (2) the disc for center-edge angle measurement is positioned and adjusted until it is placed correctly in relation to the center of the femoral head and the most lateral point of the sclerotic acetabular roof (). If fine tuning of the reorientation is necessary, the measuring discs are easily adjusted for new assessment of the angle measures. The version of the acetabulum cannot be measured by using the device but is equally important and must be addressed to achieve an appropriate anteversion. This is accomplished by identifying the anterior and posterior acetabular rim. With appropriate anteversion it is observed that 1) the posterior rim is lateral to the anterior rim and the center of the femoral head and 2) the anterior rim is medial to the center of the femoral head (Citation[8],Citation[26],Citation[68],Citation[83]).
Figure 8. The angle measuring disc for measurement of the center-edge angle. It is positioned by recognizing the center of the femoral head and the lateral limit of the sclerotic acetabular roof as landmarks (blue arrows). The 0° mark is labeled. The measured angle in this case is 35° (yellow arrow).
The PAO Database
Description
The database of periacetabular osteotomies, the PAO Database, is assigned to the Danish Hip Arthroplasty Register. All periacetabular osteotomies performed at Aarhus University Hospital between December 1998 and February 2007 are registered in the database. All registered data are collected prospectively in patient journals and are then subsequently entered into the database. A total of 450 periacetabular osteotomies are registered in the database. Of these, 349 procedures were performed by the main supervisor. Baseline characteristics of the PAO database are given in . Data regarding age, gender, weight, diagnosis, hospital length of stay, previous surgery, surgical approach, method of anesthesia, duration of surgery, intraoperative blood loss, intraoperative supplemental surgery, transfusion requirements, and complications can be assessed in the PAO database. The occurrence of moderate and severe neurovascular or technical complications (i.e., an injury to great vessels or nerves, an arterial thrombosis, unintended extension of the osteotomy into the joint or through the posterior column, or deep infection) is available in the database. Minor complications (e.g., lateral femoral cutaneous nerve dysesthesia, delayed union, and heterotopic ossification) are not. The PAO Database and the Danish Hip Arthroplasty Register can be combined to assess whether patients had subsequent total hip arthroplasties. Database inquiry was made in studies I + II.
Table 2. Baseline characteristics of the PAO Database
Validity of database
To assess the validity of the PAO Database as data source for future studies, the contents of the database were compared with the contents of patient files in 122 procedures. All data of being assessed for validity had previously been entered into the PAO Database by another observer. The following parameters were assessed for errors: diagnosis, previous surgery (yes/no), correct labeling of previous surgery, primary surgeon, surgical approach, method of anesthesia, duration of surgery, intraoperative blood loss, intraoperative supplemental surgery (yes/no), correct labeling of intraoperative supplemental surgery, transfusion requirements, occurrence of moderate and severe complications (yes/no), and correct labeling of moderate and severe complications. The proportions of erroneous data in the PAO Database for each parameter are summarized in .
Table 3. Outcome of validity assessment of the PAO Database showing the proportions of erroneous data for each parameter
For most parameters, the proportion of erroneous data is confined within a few percent, making the database a valid data source. Exceptions are the parameters of “diagnosis” and “previous surgery (yes/no),” which show errors in 8.2% and 4.1% of entered data, respectively. In all cases (n = 10) of erroneous diagnosis, it had not been noted that the diagnosis underlying hip dysplasia was congenital dislocation of the hip, and previous surgical attempts had been missed in five cases. These types of error would not have interfered with criteria of in- and exclusion of patients in studies I + II, and based on the otherwise low frequency of erroneously entered data, the PAO Database can be considered a valid data source for the present research purposes. So far, the diagnosis underlying hip dysplasia or previous surgical attempts have not been found to be significant prognostic parameters of hip joint failure following periacetabular osteotomy (Citation[64]). It should however be taken into consideration that particularly patients with previous surgical attempts in childhood in many cases represent cases of severe pathomorphology.
Even though data are collected prospectively and the purpose of the database is to monitor treatment outcome, it does not represent a truly prospective cohort. The main reasons are that data are entered into the database retrospectively and the exact research aims were not stated when data collection was initiated.
Study methods
Study designs
In studies I (case-series) + II (case-control) the outcome of the minimally invasive and ilioinguinal approaches were assessed retrospectively by querying the PAO Database, evaluation of radiographic material, evaluation of hemoglobin values, and querying the Danish Hip Arthroplasty Register. In study I, only the outcome of the minimally invasive approach was assessed, whereas the outcome of the minimally invasive and the ilioinguinal approaches were compared in study II. In study III both a prospective intraoperative investigation (case-series) and a two-observer comparative cadaver study were performed to evaluate the reliability of the novel angle measuring device.
In general the collection of data for a retrospective study is limited by the lack of predefined criteria of how to enter data. Comparing cases is influenced by diversity of data presentation, and data can be missing or incomplete. However, the presence of a tool for monitoring treatment with defined parameters of outcome, such as the PAO Database, may facilitate a more uniform registration of data in patient files. During the conduct of studies I + II the majority of outcome parameters showed a complete dataset. Exceptions were missing radiographic material, missing hemoglobin values, and missing weight data, which were not available in 1% to 5% of periacetabular osteotomies. Data assessed from the radiographic material and blood specimens are not registered in the PAO Database. If all data are prospectively entered directly into the database, the methodology of future studies may be strengthened.
The prospective intraoperative measurements of center-edge and acetabular index angles, carried out in study III, secure a uniform and complete registration of data. Intraoperative measurements of angles performed by a second, blinded observer could have conveyed interesting information on the reliability of the novel measuring device in the intraoperative setting. However, both intra- and inter-observer variability assessment was performed in a subsequent cadaver study, as outlined below.
Criteria of in- and exclusion
In studies I + II, the general inclusion criteria were periacetabular osteotomy performed by the main supervisor. Applied exclusion criteria in both studies were: hips with dysplastic changes secondary to Legg-Calvé-Perthes disease, procedures including supplemental hip surgery, and procedures not performed by using hypotensive epidural anesthesia. In study I, all periacetabular osteotomies were performed by using the minimally invasive approach. In study II, procedures performed by using the modified Smith-Petersen approach were excluded, allowing only a group of cases (minimally invasive approach) and controls (ilioinguinal approach).
Hips with dysplastic changes secondary to Legg-Calvé-Perthes disease represent a pathomorphological and biomechanical condition that is markedly different from hips with primary development of dysplastic changes (Citation[79]). It remains unclear whether the challenges associated with a periacetabular osteotomy in these patients will affect intraoperative outcome parameters and hip joint survival following the procedure. Supplemental hip surgery during a periacetabular osteotomy ranges from simple hardware removal to trochanteric osteotomy. No matter what the extent of the supplemental procedure, it will potentially affect duration of surgery, intraoperative blood loss, hemoglobin reduction, transfusion requirements, and length of hospital stay (Citation[18]). A supplemental trochanteric osteotomy has so far not been shown to have a significant effect on hip joint survival (Citation[64]). Hypotensive epidural anesthesia has shown the potential to lower intraoperative blood loss and transfusion requirements in hip replacement surgery when compared with conventional means of anesthesia (Citation[84],Citation[85]). It is the preferred method of anesthesia at our institution for both hip replacement surgery and periacetabular osteotomies. Given the possible blood sparring effect of hypotensive epidural anesthesia during periacetabular osteotomy compared with conventional means of anesthesia, procedures not performed using this method were excluded.
Following exclusions, the study group in study I consisted of 94 periacetabular osteotomies, and in study II the study groups consisted of 98 (ilioinguinal approach) and 165 (minimally invasive approach) periacetabular osteotomies, respectively. The selected criteria of in- and exclusion of procedures were chosen to secure well-defined, none-biased, and homogeneous study groups. The establishment of such clear criteria is in contrast to the diversity represented by other studies reporting the outcome of periacetabular osteotomy (Citation[18],Citation[20],Citation[26],Citation[65],Citation[70]).
The prospective intraoperative angle measurements in study III were in all 35 cases performed by the main supervisor. Patients with dysplastic changes secondary to Legg-Calvé-Perthes disease were excluded, and none of the patients had trochanteric osteotomies. Measurements were made regardless of anesthetic method. The main concern of this study was to present a group of hip joints which were homogeneous with respect to the preoperative pathomorphology and the anatomy following acetabular reorientation. This was done to secure standardized conditions for reliability testing of the novel angle measuring device.
Overlap of study groups
Study I reports the initial experience with the minimally invasive approach between April 2003 and August 2005, and study II reports the total experience with the ilioinguinal and minimally invasive approaches between December 1998 and February 2007. Similar in- and exclusion criteria were applied in both studies, and of the 165 periacetabular osteotomies performed by using the minimally invasive approach in study II, data from 94 procedures were reported in study I.
The above-mentioned information was clearly stated in study II and should be available for future reviews and meta-analysis exploring outcome of the periacetabular osteotomy. The subsequent report in study II of the same data as in study I is appropriate since the aim of the study had a somewhat different and comparative nature. Furthermore, the length of follow-up differs between studies, conveying additional information regarding hip joint survival.
Baseline characteristics
The baseline characteristics (age, weight, and gender) of periacetabular osteotomies included in study II are shown in . Groups were comparable and only the difference in age of 3.6 years was close to being statistically significant, with those in the minimally invasive group being older. Even though an upper age limit has never existed or been proposed in the literature, a shift towards also operating on older patients with hip dysplasia might explain the tendency towards patients seemingly being older at the time of surgery. When the baseline characteristics in study II are compared with those of the entire database (), the gender distribution is skewed towards a higher proportion of males in the entire database than were included in study II. The majority (73%) of patients in the PAO Database with dysplastic changes secondary to Legg-Calvé-Perthes disease are males. Hips with dysplastic changes secondary to Legg-Calvé-Perthes disease were excluded in the study, which in part explains the higher proportion of females. In study III, the study group consisted of 31 females and 4 males with “classic” dysplastic changes and a median age at surgery of 30 years (range, 14–57 years).
Table 4. Comparison between study groups of baseline characteristics in study II.
In the literature, the mean age at surgery varies from the early 20s to the late 30s, and the proportion of females undergoing surgery is approximately 75% to 80% (Citation[16-20],Citation[22],Citation[26],Citation[48],Citation[62],Citation[63],Citation[66],Citation[70],Citation[77],Citation[79-81]), which in any case makes the baseline characteristics presented above comparable to those in the literature.
Indications for surgery
The stated indications for performing a periacetabular osteotomy in studies I-III were: 1) symptomatic acetabular dysplasia, 2) a center-edge angle of Wiberg < 25˚, 3) a congruent hip joint, 4) maintained range of motion, and 5) no or early signs of osteoarthritis (Tönnis grade 0-1). In addition, though not stated, the triradiate cartilage should be closed to avoid alternations in acetabular growth due to reorientation.
What is symptomatic acetabular dysplasia? There is no clear definition of this based on research in the literature. In daily clinical practice the following is applied: patients should have persistent relevant hip pain for at least 3 to 6 months prior to surgical intervention. A similar approach is described in other studies (Citation[17],Citation[18],Citation[48],Citation[78]). Relevant hip pain is primarily groin pain, and other causes of hip-related pain should be diagnosed and treated before performing a periacetabular osteotomy. This is especially the case in borderline cases of acetabular dysplasia and atypical symptoms or pain patterns. There is no direct evidence that duration of symptoms or the level of pain preoperatively affects the outcome of periacetabular osteotomy, but a low preoperative clinical score, though unadjusted for the degree of preoperative osteoarthritis, has proven to be a significant risk factor for conversion to total hip replacement (Citation[64]).
Is a center-edge angle < 25˚ the right level? The literature is characterized by some diversity with respect to what level of the center-edge angle indicates periacetabular osteotomy. There are studies in support of a 25° cut-off level (Citation[16-18],Citation[77]) and a 20° cut-off level (Citation[78]), whereas other studies are without a clear statement of a cut-off level (Citation[20],Citation[26],Citation[48],Citation[62]). The preoperative upper limit of the center-edge angle is reported to be as high as 34° (Citation[48]), which approximates normal values for the center-edge angle. In a population-based setting, the mean center-edge angle is 35° for both genders, and the lower limit of ± 2 standard deviations corresponds to 20° (Citation[86]). Even though, acetabular dysplasia defined as ≤ 20° was found to be a significant predictor of hip osteoarthritis in a population-based setting (Citation[45]), another case-control study with 10-year follow-up did not show significant differences in the reduction of joint space width or in self-reported hip pain when comparing dysplastic hips to normal hips (Citation[46]). The poor correlation between symptoms and center-edge angle in a population-based setting makes any cut-off value defining clear pathology somewhat arbitrary. However, selecting a cut-off limit of 20° or 25° in symptomatic patients seems appropriate, with some guarantee that symptoms, rim overload, and threatening joint degeneration can be attributed to acetabular dysplasia.
What is a congruent hip joint? Congruency of the hip joint can be defined as a concentric relationship between the circumferential shapes of bearing surfaces on the femoral head and the acetabulum. This is evaluated on a preoperative anteroposterior pelvic radiograph. An anteroposterior radiograph of the pelvis with lower extremities abducted and internally rotated has been suggested by several authors for further assessment of the joint congruency achievable following acetabular reorientation (Citation[16],Citation[18],Citation[26],Citation[63],Citation[78]). The abduction view is no longer recorded at our institution, in part to reduce the exposition to radiation and in part because it did not change the indication for surgery. Good joint congruity has been shown to be associated with better clinical and radiographic outcome following rotational acetabular osteotomy in patients with severe osteoarthritis (Citation[87]). Performing joint preserving surgery in moderate or severe osteoarthritic hip joints is, from our point of view however, not indicated due to the documented association with joint failure (Citation[17],Citation[18],Citation[20],Citation[62],Citation[64],Citation[65],Citation[78]). Also following rotational acetabular osteotomy, aspherical femoral head shape was found to be associated with poor radiological results (Citation[33]). Hip joint congruity was not measured directly, but loss of spherical shape might indicate poor congruity. From a biomechanical point of view, a congruent hip joint would seem to facilitate impingement-free range of motion with an even distribution of load forces, thereby protecting the joint from joint deterioration.
What is meant by maintained range of motion? Few studies mention range of motion in the indications for surgery or report the preoperative range of motion (Citation[18],Citation[22],Citation[63],Citation[65]). Hip flexion >100° or ≥110° have been suggested as discriminators (Citation[22],Citation[63]). In studies I–III, hip flexion >110˚ and internal rotation of >15˚ are used as indications for surgery. Important biomechanical considerations underlie the selection of these somewhat arbitrary cut-off values. Because of the biomechanical changes induced by the acetabular reorientation, hip flexion and internal rotation may be reduced (Citation[65]). Slight reductions in hip flexion and internal rotation are not likely to cause clinical problems if the preoperative values are >110˚ and >15˚, respectively. If below these cut-off values, patients are at risk of impingement at hip flexion and forced external rotation of the lower extremity. However, there is nothing to support these arguments in terms of improved functional outcome or hip joint survival.
Why should patients only have osteoarthritis corresponding to Tönnis grades 0 or 1? Several studies have documented an association between preoperative moderate or severe osteoarthritis (Tönnis grades 2 and 3) and conversion to total hip replacement following periacetabular osteotomy (Citation[17],Citation[18],Citation[20],Citation[62],Citation[64],Citation[65],Citation[78]). An actual risk estimate with joint failure as endpoint has recently been reported, showing a hazard ratio of 3.39 per higher preoperative Tönnis grade (Citation[64]). Thus, according to contemporary indications for periacetabular osteotomy, only hip joints with Tönnis grades 0 or 1 should undergo joint preserving surgery. Further supporting this approach is that the periacetabular osteotomy has proven more cost-effective than total hip replacement in dysplastic hips with osteoarthritis corresponding to Tönnis grade 1. In contrast, total hip replacement is clearly more cost-effective in Tönnis grade 3 hips, and the cost-effectiveness of periacetabular osteotomy in Tönnis grade 2 hips is doubtful (Citation[88]). In the early days of the periacetabular osteotomy its limitations were not yet explored and exact indications for surgery were unknown. Even though the intended indication for surgery included Tönnis grades 0 and 1, some patients may have had higher preoperative grades during the early period of performing the periacetabular osteotomy at our institution.
Validity of clinical outcome parameters
Duration of surgery was measured from the start of the skin incision to the completion of the skin closure. This interval is relevant in terms of expressing the duration of surgical trauma inflicted on the tissues. There was a clear tendency for the number of minutes spent on each operation to be round up or down to match the nearest “5-minute” marker. As there is no protocol for the procedure of rounding values up or down, the “true” duration of surgery is thought to differ between 0 to 5 minutes from the reported value.
Intraoperative blood loss was estimated on the basis of the volume of blood in the suction bottles and swaps in the operating room. Visual estimation of blood loss has in general been shown to be unreliable (Citation[89],Citation[90]). At the low levels of intraoperative blood loss reported in studies I + II, the estimated external blood loss is most likely overestimated (Citation[89],Citation[90]). The reported amount of intraoperative blood loss for each periacetabular osteotomy tends to be round up or down to the nearest “50-ml” marker. This is likely to introduce error to reported values, but, as mentioned earlier, estimating blood loss in the clinical setting has considerable inherent errors. In addition to the recognized intraoperative blood loss, a considerable hidden blood loss has been recognized in other hip-related surgery (Citation[91],Citation[92]). The reduction in hemoglobin was also calculated in studies I + II to shed more light on the magnitude of the total blood loss. Reduction in hemoglobin was calculated from the preoperative value and from the first available value on the first or second postoperative day. The true endpoint when assessing blood loss in otherwise healthy young patients is the need for allogenic blood transfusion. Transfusion requirements were calculated as the total number of intraoperatively and postoperatively administered SAGM units. In general, the indications for blood transfusion follow national guidelines, but given the retrospective design, there was no specific protocol for prescription of transfusions related to the studies. In general, postoperative blood transfusion was prescribed on the basis of clinical symptoms of anemia assessed by the surgeon in attendance.
Length of hospital stay was calculated from the day before surgery to the day of discharge (study I) or from the day of surgery to the day of discharge (study II). This difference is of course unfortunate, but knowing the difference in definitions, comparison is fairly easy. The two definitions are considered to be equally valid since patients were always admitted to the department 1 day before periacetabular osteotomy. In general, the patients were discharged when they were able to walk with crutches (normal walking and stair climbing), ensuring partial weight bearing on the operated side. Again, there was no prospective protocol to secure standardized criteria for patient discharge in studies I + II.
Validity of radiographic evaluation
All patients had preoperative and postoperative supine anteroposterior pelvic radiographs taken routinely. The center-edge angle of Wiberg (Citation[15]) and the acetabular index angle of Tönnis (Citation[23]) were measured for assessment of the preoperative degree of hip dysplasia and the achieved acetabular reorientation (). Excessive pelvic rotation is known to distort values for the center-edge angle beyond inherent measuring errors, and the foramen obturator index of Tönnis was assessed to exclude excessively rotated pelvises, defined by values outside the interval 0.7 to 1.8 (Citation[93]). The same observer made all measurements on both preoperative and postoperative radiographs.
The center-edge and acetabular index angle are commonly used to characterize the anatomy of hip dysplasia (Citation[10-12],Citation[14],Citation[15],Citation[23]). They give a good, well-understood and accepted description of the two-dimensional properties of hip dysplasia. The equally important properties of the acetabular version are not described or quantified in the present radiographic material, but only assessed during surgery by identification of the anterior and posterior acetabular rims securing appropriate anteversion (Citation[8],Citation[26],Citation[68],Citation[83],Citation[94]) ().
Pelvic radiographs in the present material are all recorded with the patient supine. Radiographic parameters of hip dysplasia, such as the center-edge and acetabular index angles, are not affected beyond inherent measuring errors when the patient is repositioned between the supine and weight-bearing positions (Citation[8]). Only pelvic tilt and the appearance of acetabular version changes upon repositioning, and assessing the center edge and acetabular index angles on either supine or weight-bearing radiographs does not therefore introduce risk of misinterpretation (Citation[8],Citation[95]). The protocol for preoperative evaluation has recently been changed and is now made on weight-bearing anteroposterior pelvic radiographs (Citation[8]).
There is an inherent variability of angle measurements on assessment on conventional radiographs. In study III, the magnitude of this variability is assessed for the center-edge and acetabular index angles by performing double measurements on postoperative pelvic radiographs. Standard deviations were ±2.0° and ±1.7° for the center-edge and acetabular index angles, respectively, thereby confining 95% of repeated measurements well within ±5°. These values are confirmed in another report by the same author and are comparable to what is reported in the literature (Citation[8],Citation[93],Citation[96],Citation[97]). By using conventional radiographs for assessment of the center-edge and acetabular index angles, the inherent problems adding to variability are: 1) identification of the center of the femoral head, 2) identification of the medial and lateral limits of the sclerotic acetabular roof, and 3) construction of the line of reference.
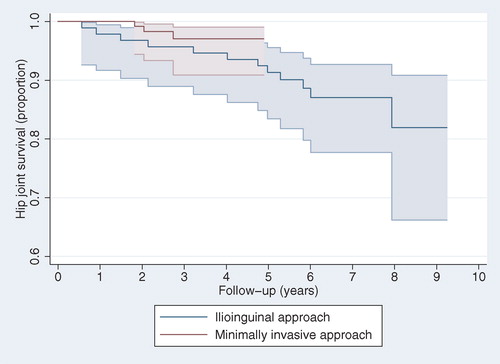
Analysis of hip joint survival
Hip joint survival was analyzed in studies I and II by means of displaying the Kaplan-Meier estimates. For the Kaplan-Meier estimate, the exact follow-up time or time to failure is used to express the cumulative survival probability (Citation[98]). The method is widely applied and accepted for survival analysis, though only used in a few other studies reporting outcome of periacetabular osteotomy (Citation[17],Citation[26],Citation[64]).
By combining data in the PAO Database and the Danish Hip Arthroplasty Register, it is possible to assess whether a periacetabular osteotomy and later a total hip arthroplasty, the endpoint of the hip joint survival analysis, have been carried out in the same patient. The Danish Hip Arthroplasty Register is a validated and reliable tool for this assessment (Citation[99]). Foreign patients who had a periacetabular osteotomy at our institution were excluded from survival analysis, because only patients who have subsequently had total hip arthroplasties in Danish hospitals are available in the Danish Hip Arthroplasty Register.
The cumulative probability of hip joint survival with the use of conversion to total hip arthroplasty as endpoint is only in part descriptive of surgical success. Despite a joint preserving periacetabular osteotomy, some patients will experience development of end-stage osteoarthritis and pain, which eventually leads to conversion to total hip arthroplasty. Therefore clinical scores and detection of progressive osteoarthritis should be mentioned as clinically relevant endpoints.
Interference of learning curve, accumulated surgical experience, and general developments
The periacetabular osteotomies included in study II were performed between December 1998 and February 2007, and the ilioinguinal and minimally invasive approaches were used in sequential time periods. During this period of more than 8 years, the main supervisor accumulated great experience with respect to every aspect of performing the periacetabular osteotomy. It is likely that this accumulation of experience will positively influence the outcomes of the most recently performed procedures. Furthermore, there is a documented learning curve related to performing periacetabular osteotomy (Citation[16],Citation[26],Citation[68-70]), which may negatively influence the outcomes of the first procedures. This may skew the comparison of the approaches, making the outcome of the ilioinguinal approach appear less favorable. Accordingly, interpretations should be and are made with precaution. In study I, the periacetabular osteotomies included were performed between April 2003 and August 2005 using the minimally invasive approach. No particular learning curve for the main supervisor was identified when assessing the relationship between the number of procedures performed and the duration of surgery, thereby implying that a steady state of the learning curve had already been reached.
When data have been collected over a period of more than 8 years and assessment of outcome parameters are made retrospectively, it is likely that general developments of clinical practice in the department will introduce bias to the results. It is difficult to quantify the exact importance of these developments and the bias they introduce. The best example is perhaps the general efforts to fast track the course of hospital stay in hip and knee arthroplasty surgery (Citation[100],Citation[101]). This has especially increased focus on treatment of pain, early mobilization and discharge procedures, with possible impact on patients undergoing periacetabular osteotomy because they are admitted to the same department.
Validity of methods for validation of the novel measuring device
To investigate the reliability of the novel measuring device in study III, a cadaver study was performed in addition to the prospective clinical trial. The aim of the cadaver study was to assess the intra- and interobserver variability of the novel measuring device and to evaluate the effect of pelvic tilt or rotation on measurement of the center-edge and acetabular index angles. Work with and handling of the cadaver specimen was done in conformity with ethical principles of research, and prior to death the individual had given written consent to use of the body for research purposes. The female cadaver specimen was partial and consisted of the pelvis, hips, thighs, and knees with intact skin and soft tissues. Initially, the spikes and the alignment rod of the measuring device were mounted. The position of the pelvis was then adjusted until it was in a neutral position. This was confirmed by achieving a foramen obturator index of 1.0 and a distance between the pubic symphysis and the sacrococcygeal joint of 4 cm on an anteroposterior pelvic radiograph (the tube was oriented perpendicular to the table and the tube to film distance was 110 cm, resulting in a magnification of 15%). This position of the pelvis was easily reproducible, and there was no risk of introducing measuring error in excess of the inherent error of angle assessment (Citation[8],Citation[93],Citation[96],Citation[97]).
The measurements of the center-edge and acetabular index angles using the measuring device were carried out as described previously. Two observers (observer 1, experienced with the device; observer 2, inexperienced with the device) performed the angle measurements on the right hip of the cadaver. The C-arm of the fluoroscope was tilted in 2.5° increments to the left and to the right of the cadaver in an arc totaling 25°. In this way, 11 measurements of both angles were carried out from an angle of 12.5° to the left and to 12.5° to the right of the cadaver. Another 11 measurements of both angles were performed similarly, tilting the C-arm of the fluoroscope in 2.5° increments in the cranial and caudal directions in an arc totaling 25°. For each measurement, the femoral head was focused in the middle of the image. The observers were blinded to each other's measurements and to the actual position of the C-arm. The order of measurements was random with respect to the position of the C-arm. Observer 1 repeated all measurements of both angles.
The setup secured that all measurements by both observers were performed under identical conditions. This gave valid estimates of the intra- and interobserver variability of the measuring device. Additional repeated measurements by observer 2 could have conveyed interesting information on differences in intraobserver variability between the experienced and inexperienced observer.
Radiographic dysplastic parameters, such as the center-edge and acetabular index angles, are in general only affected beyond inherent measuring error if the image is severely distorted (Citation[15],Citation[93],Citation[96],Citation[97]). When utilizing the measuring device, it is important to know whether it adds variability to angle measurements when tilting and rotating the pelvis. This could introduce a potential risk of misinterpreting the achieved angle measures. The applied total arch of 25° for pelvic tilt is approximately twice that of the change in pelvic tilt for females when repositioning (from supine to weight bearing) and approximately 4 times the change in pelvic tilt for males when repositioning (Citation[8]). The evaluation therefore covers any clinically relevant use of the measuring device.
The measuring device was built to mimic construction of the center-edge and acetabular index angles the way they are drawn on anteroposterior pelvic radiographs. The device could therefore not be expected to decrease inherent variability of angle construction. As the inherent measuring error of angle assessment is confined within ±5° (Citation[8],Citation[93],Citation[96],Citation[97]), this was selected as the limit for a satisfactory result in assessment of the variability of the device intraoperatively and for variability assessment in the cadaver study.
The prospective intraoperative measurements were compared with those on the postoperative pelvic radiographs. Double measurements of angles on the postoperative pelvic radiographs acted as a measure of the inherent variability of angle assessment. The measuring device was not compared against any radiographic gold standard. Measurements of the center-edge and acetabular index angles using three-dimensional imaging techniques could be considered a gold standard, although a CT scanning, for example, is unlikely to be conducted postoperatively. It seems meaningful to compare the angle measurements obtained with the device with those on postoperative pelvic radiographs because this is the commonly used imaging technique to evaluate the result of the acetabular reorientation.
Statistical analysis
In studies I + II, normally distributed data were presented as means with 95% confidence intervals and comparisons were made by using a two-sample t-test. Data that were not normally distributed were presented as medians with interquartile range and were compared by using a two-sample Wilcoxon rank-sum (Mann-Whitney) test. For testing of differences in parameters given as proportions, Pearson's chi-squared test was used. Learning curve assessment in study I was made by linear regression analysis. The use of Kaplan-Meier survival analysis is discussed above. The level of significance was set at P < 0.05.
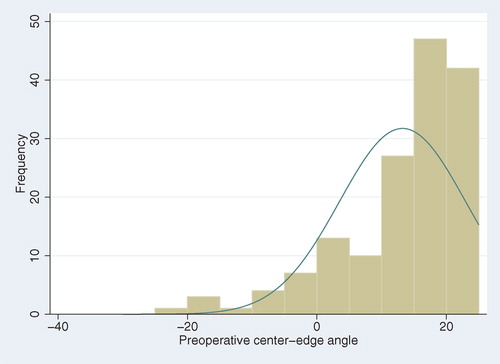
To assess whether data were normally distributed or not, histograms and Q–Q plots were made for all parameters before data analysis. Some parameters, such as the preoperative hemoglobin level, have almost by definition normally distributed data. Other parameters are deprived of their normal distribution because of the impact of surgical indications and surgical aims. An example is the center-edge angle, which in epidemiological studies has been shown to be normally distributed with a mean value of approximately 35° (Citation[86]). However, a periacetabular osteotomy is only indicated in patients with a center-edge angle < 25°, thereby introducing an artificial cut-off in the distribution of preoperative center-edge angles (). Similarly, the distribution of postoperative center-edge angles is influenced by the surgical aim to achieve an angle between 30° and 40°. One would believe that these skewed distributions of the pre- and postoperative center-edge angles would apply in other studies. This would warrant reporting the median value of the pre- and postoperative center-edge angles, but this is rarely done (Citation[63]).
Figure 9. Histogram showing the distribution of preoperative center-edge angles. The cut-off at 25° clearly distorts the normal distribution of data.
In study II, several parameters were compared between the ilioinguinal and the minimally invasive groups. Given the retrospective design, with known sizes of patient groups, a sample size calculation was not warranted. However, the power of the study to detect the actual differences between groups can be calculated. Looking at, for example, the drop in hemoglobin reduction using the known sample sizes, standard deviations and significance level, a study power >0.99 is found.
In study III, the variability between angle measurements obtained intraoperatively and postoperatively was determined, and the data presented as mean of the difference with standard deviation and 95% limits of agreement. This approach for data assessment is described by Bland and Altman and is called the 95% limits of agreement method (Citation[102],Citation[103]). Data were presented in a plot as suggested by the same authors (a Bland-Altman plot) (). The intraobserver variability of angle measurements on postoperative radiographs and intra- and interobserver variability of angle measurements in the cadaver study were assessed and presented in the same way. The intraobserver variability of angle measurements on postoperative radiographs were compared with 1) the variability between angle measurements obtained intraoperatively and on postoperative radiographs, and 2) the intra- and interobserver variability of angle measurements in the cadaver study. These comparisons were done by using Pitman's variance ratio test. Angle measures of the different series in the cadaver study were presented as range, mean, and standard deviation. The variability of these series of measurements was compared with the intraobserver variability of the device by using Pitman's variance ratio test.
Figure 10. Bland-Altman plot of the difference against the average of center-edge angle measurements postoperatively and intraoperatively with the device. The mean of differences (solid line), the standard deviation of differences (dotted lines), and the 95% limits of agreement (dashed lines) are presented.
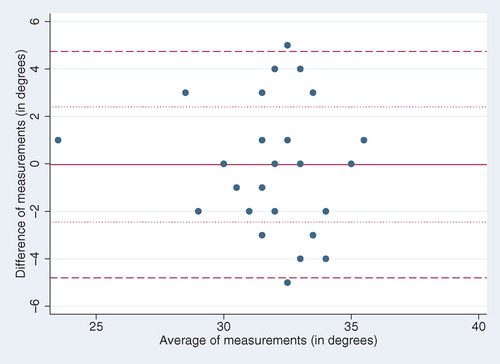
Figure 11. Kaplan-Meier hip joint survivorship curves following periacetabular osteotomy with total hip arthroplasty as endpoint. The colored areas (minimally invasive=red; ilioinguinal=blue) indicate the 95% confidence intervals of the survival rates. The number of hip joints remaining in each group is given for every year of follow-up below the x-axis. Please note that the y-axis does not start at “0”.
Use of the 95% limits of agreement method has been advocated by its inventors, mainly to avoid other potentially misleading approaches, such as regression and correlation, when comparing methods of measurement. Furthermore, the method actually conveys information that is useful clinically. In the case of comparing intraoperatively and postoperatively obtained angle measurements, 95% of the differences between measurements would be expected to lie within the 95% limits of agreement. For the center-edge angle, these limits were -4.8° to +4.7° (), and since these values were confined within ±5°, the variability was considered to be satisfactory. This means that the values can be interpreted in a clinical context and a decision can be made as to whether measurement methods agree sufficiently to warrant application of the novel measuring device.
Summary of results
The overall aim of the studies was to explore and validate intraoperative methods for periacetabular osteotomy with the objective of optimizing the surgical treatment of hip dysplasia. The studies were performed by means of database inquiry, evaluation of radiographic and serologic material (I + II), a prospective clinical trial, and a cadaver study (III).
Study I
Key research questions: Is a new, minimally invasive approach for the periacetabular osteotomy safe, can optimal acetabular reorientation be achieved, and does the new approach minimize tissue trauma?
Results: In 94 periacetabular osteotomies, there were no cases of moderate or severe technical and neurovascular complications, and the achieved median center-edge angle of 34˚ and acetabular index angle of 3˚ suggests that optimal reorientation can be achieved. The length of hospital stay, duration of surgery, intraoperative blood loss, hemoglobin reduction, and transfusion requirements were at relatively low levels. Hip joint survival with total hip arthroplasty as the end point was 98% at 4.3 years ().
Table 5. Clinical and radiographic measures associated with the minimally invasive approach in study I
Conclusion: The results suggest that the minimally invasive approach is safe, minimizes tissue trauma, and allows optimal acetabular reorientation.
Study II
Key research question: Does the minimally invasive approach produce an outcome similar to that of the “classic” ilioinguinal approach for the periacetabular osteotomy?
Results: When compared with the outcome of the ilioinguinal approach (n = 98 procedures), the procedures performed using the minimally invasive approach (n = 165 procedures) had statistically significant shorter duration of surgery, less intraoperative blood loss and hemoglobin reduction, and fewer transfusion requirements. The achieved reorientation was comparable between groups. There were no cases of moderate or severe complications in the minimally invasive group and three cases (3%) of arterial thrombosis in the ilioinguinal group (). At a follow-up of 4.9 years, the hip joint survival rates were 97% in the minimally invasive group and 93% in the ilioinguinal group ().
Table 6. Clinical and radiographic measures of the minimally invasive and ilioinguinal approaches
Conclusion: The outcome of the minimally invasive approach compares favorably with that of the ilioinguinal approach. Continued use of the minimally invasive approach is supported by the findings.
Study III
Key research question: Can reliable intraoperative assessment of center-edge and acetabular index angles be made during acetabular reorientation by using a simple, novel measuring device? To be reliable the variability of angle measures should not exceed that of inherent variability when assessing angles on radiographs (± 5˚).
Results: The inherent variability of angle assessment on radiographs was confirmed to be confined within ± 5˚. In the prospective clinical part of the study, it was found that intraoperatively obtained angle measures differed less than ± 5˚ from measurements on postoperative pelvic radiographs. The level of this variability did not exceed that of the inherent variability of angle assessment (). In the cadaver part of the study, it was found that intra- and interobserver variability of the device was confined to well within ± 5˚ and that the two values did not differ from each other or from the inherent variability of angle assessment (). Finally, pelvic positioning did not influence the variation of angle measurements beyond the inherent intraobserver variability of the device within the arcs (± 12.5˚) of tilt and rotation applied in this study.
Table 7. Summary of measurements in the clinical and cadaver studies
Conclusion: The simple, novel measuring device is a reliable tool for repeated intraoperative angle assessment during acetabular reorientation of the periacetabular osteotomy.
Discussion
Periacetabular osteotomy – what advances are needed?
Since the development of the periacetabular osteotomy in the early 1980s, its use has spread worldwide. It is now the joint preserving treatment of choice in young adults with symptomatic hip dysplasia. The procedure has the potential to relieve pain, improve functions of daily living, and to preserve hip joints by delaying or even preventing development of early osteoarthritis (Citation[17-20],Citation[22],Citation[26],Citation[48],Citation[62-65],Citation[77-81]).
From a critical point of view, more reports on the medium and long-term results after periacetabular osteotomy are needed to fully document its advantages and justify its wide application. In two of three studies reporting the results of medium and long-term follow-up, the patients are those initially operated on by the inventors from Bern (Citation[62],Citation[64],Citation[65]). The question is then, can the periacetabular osteotomy be applied in other centers with an equally successful result? Another critical argument is that no randomized controlled trials have been performed to document the effect of periacetabular osteotomy versus conservative treatment or total hip arthroplasty. However, one should remember that the periacetabular osteotomy is performed only (or should only be performed) in symptomatic patients with very little or no degenerative signs who suffer persistent pain and loss of daily function. They have a need for treatment after unsuccessful conservative treatment, but are not yet candidates for total joint replacement. Future research should aim at clarifying what predicts good and bad outcomes of periacetabular osteotomy.
Going through the literature in search of intraoperative measures of periacetabular osteotomy, such as duration of surgery, intraoperative blood loss, transfusion requirements, and complications (Citation[16-18],Citation[20],Citation[22],Citation[26],Citation[48],Citation[62],Citation[63],Citation[65],Citation[70],Citation[77],Citation[80],Citation[82]), it becomes evident that advances are needed. The main requirement for periacetabular osteotomy, performed in otherwise healthy young adults, is a safe surgical procedure with optimal acetabular reorientation and preferably with minimum values for duration of surgery, intraoperative blood loss, transfusion requirements, and complications. Until recently such procedure had not been described (study I).
What advances does the new approach offer and is it truly minimally invasive?
The minimally invasive characteristics of the new transsartorial approach are defined not only by the 7 centimeter skin incision. They are evident at all stages of surgery. No muscles are detached and only the sartorius muscle is split in the direction of the fibers. The tissue trauma is further minimized by the relatively brief duration of surgery. This is in part due to the limited time spent on the approach and closure. There were no moderate and severe complications. When a transsartorial approach is used, the sartorius and iliopsoas muscles protect the femoral vessels and nerve against direct and indirect damage. The abductor muscles are spared, and the acetabular blood supply is therefore left intact. The relatively small intraoperative blood loss and transfusion requirements also suggest minimal soft tissue trauma. The duration of surgery, intraoperative blood loss, transfusion requirements, and absence of moderate and severe complications with the new approach compare favorably with those associated with other techniques reported in the literature (Citation[16-18],Citation[20],Citation[22],Citation[26],Citation[48],Citation[62],Citation[63],Citation[65],Citation[70],Citation[77],Citation[80],Citation[82]). The achieved measures of the postoperative center-edge and acetabular index angles suggest that good acetabular reorientation is not compromised with the new, minimally invasive transsartorial approach. Finally, short-term hip joint survival has shown encouraging results.
The results of the new, minimally invasive approach presented in studies I + II suggest that this new approach offers the needed advances in periacetabular osteotomy, with respect to intraoperative measures. Given the accumulated experience of the surgeon, the outcome compares favorably with that of the “classic” ilioinguinal approach. But is it truly minimally invasive? From a critical point of view, the outcome parameters used may be regarded as only substitute measures implying that little tissue trauma is inflicted. However, the chosen outcome parameters are highly clinically relevant and can be directly interpreted. In total hip arthroplasty, C-reactive protein has been shown to increase as part of the inflammatory response to surgical trauma (Citation[104],Citation[105]), but no significant differences were detected when comparing a mini-incision with a standard incision group (Citation[106]). Also the increase in mid-thigh circumference did not differ between groups (Citation[106]). To fully assess the extent of surgical trauma, a postoperative MR scanning would allow some quantification of the invasiveness into soft tissues. Even this technique is not directly interpretable in terms of knowing what outcome to expect or in the setting of informing patients on intraoperative outcome. The aim of future studies should be to investigate whether the results of the minimally invasive approach, presented in studies I + II, can be achieved by other experienced surgeons in similar surgical settings.
A controversy in contemporary periacetabular osteotomy is whether arthrotomy and labral intervention should be performed or not. A few reports claim that labral lesions are associated with a poor prognosis after periacetabular osteotomy (Citation[64],Citation[65]), but there are no results of sufficient methodological value to support either approach. In the periacetabular osteotomies presented in studies I + II, arthrotomy and labral intervention were not performed, and primary intra-articular assessment was not considered necessary. The minimally invasive approach does not permit intra-articular surgical intervention. The approach can, however, be extended to make this possible, although thereby losing its minimally invasive characteristics.
Achieving surgical aims with the novel measuring device – what advances are offered?
Existing techniques for intraoperative assessment of center-edge and acetabular index angles have inherent limitations. Intraoperative angel assessment using pelvic radiographs is time-consuming, and several radiographs may be needed before the intended reorientation has been achieved; assessment by eye using fluoroscopy is potentially unreliable, even for someone very experienced; and computer-assisted and image-guided techniques are expensive without improving the achieved acetabular reorientation (Citation[73-76]). Using the novel measuring device, one can obtain reliable measures of the center-edge and acetabular index angles with variability well within that of angle measurements on conventional radiographs. Compared with existing techniques for intraoperative center-edge and acetabular index angle assessment, the novel measuring device has the advantages of 1) being simple to use, 2) being relatively inexpensive, 3) making conventional intraoperative radiographs unnecessary, 4) facilitating fast repeated angle measurements during fine-tuning of correction, and 5) being equally reliable in the hands of inexperienced and experienced users.
Achieving an optimal reorientation is a cornerstone of the successful periacetabular osteotomy. The optimal technique for this purpose remains unknown, but the novel measuring device represents an advance. It is a reliable and fully validated tool for intraoperative assessment of the center-edge and acetabular index angles. Assessment of the acetabular version is equally important and must also be done during acetabular reorientation. The aim of future studies should be to incorporate all properties of three-dimensional acetabular reorientation in a validated, reliable, simple, and inexpensive technique.
Future application
Development of the minimally invasive transsartorial approach and the novel measuring device represent marked surgical advances in contemporary periacetabular osteotomy. The results support the continued use of both techniques. In general, periacetabular osteotomy is considered to be technically demanding. Using the minimally invasive approach requires a good understanding of how osteotomies are performed and the acetabulum reoriented. It is therefore recommended that only surgeons with previous experience with the performance of periacetabular osteotomy consider using the minimally invasive approach. The measuring device is equally reliable in the hands of inexperienced and experienced users, making wide application of this technique a straightforward matter.
Appendix
Appendix A
Short outline of the surgical techniques for the modified Smith-Petersen and ilioinguinal approaches, as they were performed at our institution
Specific modifications of the Smith-Petersen approach have been reported (Citation[69]). The skin incision was made along the anterior third of the iliac crest to the anterior superior iliac spine and then curved distally and continued vertically along the tensor fasciae latae for approximately 10 cm. The internervous planes between the tensor fasciae latae and sartorius, and between the gluteus medius and rectus femoris were developed. In contrast to the previously described modification of the Smith-Petersen approach, the rectus femoris was not detached. In some of the first cases, the origin of the sartorius muscle was detached by means of an osteotomy.
The ilioinguinal approach was performed as previously described (Citation[107]), but without lateral extension along the iliac crest. The skin incision extended from the anterior superior iliac spine, along the inguinal ligament, and terminated at the level of the pubic symphysis near the midline. The inguinal ligament was incised, leaving the origins of the abdominal musculature and fascia attached to the proximal part of the split ligament. Further access was created by incising the iliopectineal fascia that separates the lacuna musculorum and lacuna vasorum. This allowed mobilization of the iliopsoas muscle, which, combined with medial retraction of the external iliac vessels, created access to performance of the osteotomies through two windows: one medial and one lateral to the iliopsoas muscle.
Theses from the Orthopaedic Research Group
PhD and Doctoral Theses from the Orthopaedic Research Group, www.orthoresearch.dk, University Hospital of Aarhus, Denmark
PhD Theses
The influence of local bisphosphonate treatment on implant fixation
Thomas Vestergaard Jakobsen, December 2008
Adjuvant therapies of bone graft around non-cemented experimental orthopaedic implants. Stereological methods and experiments in dogs
Jørgen Baas, July 2008
Acta Orthopaedica (Suppl 330) 2008;79
CoCrMo alloy, in vitro and in vivo studies
Stig Storgaard Jakobsen, June 2008
Rehabilitation outcome after total hip replacement; prospective randomized studies evaluating two different postoperative regimes and two different types of implants
Mette Krintel Petersen, June 2008
Efficacy, effectiveness, and efficiency of accelerated perioperative care and rehabilitation intervention after hip and knee arthroplasty
Kristian Larsen, May 2008
Rehabilitation of patients aged over 65 years after total hip replacement - based on patients' health status
Britta Hørdam, February 2008
Evaluation of Bernese periacetabular osteotomy; prospective studies examining projected load-bearing area, bone density, cartilage thickness and migration
Inger Mechlenburg, August 2007
Acta Orthopaedica (Suppl 329) 2008;79
Combination of TGF-β1 and IGF-1 in a biodegradable coating. The effect on implant fixation and osseointegration and designing a new in vivo model for testing the osteogenic effect of micro-structures in vivo
Anders Lamberg, June 2007
On the longevity of cemented hip prosthesis and the influence on implant design
Mette ørskov Sjøland, April 2007
Reaming procedure and migration of the uncemented acetabular component in total hip replacement
Thomas Baad-Hansen, February 2007
Studies based on the Danish Hip Arthroplasty Registry
Alma B. Pedersen, 2006
DEXA-scanning in description of bone remodeling and osteolysis around cementless acetabular cups
Mogens Berg Laursen, November 2005
Biological response to wear debris after total hip arthroplasty using different bearing materials
Marianne Nygaard, June 2005
The influence of RGD peptide surface modification on the fixation of orthopaedic implants
Brian Elmengaard, December 2004
Stimulation and substitution of bone allograft around non-cemented implants
Thomas Bo Jensen, October 2003
Surgical technique's influence on femoral fracture risk and implant fixation. Compaction versus conventional bone removing techniques
Søren Kold, January 2003
The influence of hydroxyapatite coating on the peri-implant migration of polyethylene particles
Ole Rahbek, October 2002
Gene delivery to articular cartilage
Michael Ulrich-Vinther, September 2002
In vivo and vitro stimulation of bone formation with local growth factors
Martin Lind, January 1996
Doctoral Theses
Gene therapy methods in bone and joint disorders. Evaluation of the adeno-associated virus vector in experimental models of articular cartilage disorders, periprosthetic osteolysis and bone healing
Michael Ulrich-Vinther, March 2007
Acta Orthopaedica (Suppl 325) 2007;78
Adult hip dysplasia and osteoarthritis. Studies in radiology and clinical epidemiology
Steffen Jacobsen, December 2006
Acta Orthopaedica (Suppl 324) 2006;77
Calcium phosphate coatings for fixation of bone implants. Evaluated mechanically and histologically by stereological methods
Søren Overgaard, 2000
Acta Orthop Scand (Suppl 297) 2000;71
Growth factor stimulation of bone healing. Effects on osteoblasts, osteomies, and implants fixation
Martin Lind, October 1998
Acta Orthop Scand (Suppl 283) 1998;69
Hydroxyapatite ceramic coating for bone implant fixation. Mechanical and histological studies in dogs
Kjeld Søballe, 1993
Acta Orthop Scand (Suppl 255) 1993;54
References
- Lee MC, Eberson CP. Growth and development of the child's hip. Orthop Clin N Am. 2006; 37: 119–132
- Weinstein SL. Natural history and treatment outcomes of childhood hip disorders. Clin Orthop Relat Res. 1997; 344: 227–242
- Chung CY, Park MS, Choi IH, Cho TJ, Yoo WJ, Lee KM. Morphometric analysis of acetabular dysplasia in cerebral palsy. J Bone Joint Surg Br. 2006; 88: 243–247
- Shaw ED, Beals RK. The hip joint in Down's syndrome. A study of its structure and associated disease. Clin Orthop Relat Res. 1992; 278: 101–107
- Harrison TJ. The influence of the femoral head on pelvic growth and acetabular form in the rat. J Anat. 1961; 95: 12–24
- Ponseti IV. Growth and development of the acetabulum in the normal child. Anatomical, histological, and roentgenographic studies. J Bone Joint Surg Am. 1978; 60: 575–585
- Wynne-Davies R. A family study of neonatal and late-diagnosis congenital dislocation of the hip. J Med Genet. 1970; 7: 315–333
- Troelsen A, Jacobsen S, Rømer L, Søballe K. Weightbearing anteroposterior pelvic radiographs are recommended in DDH assessment. Clin Orthop Relat Res. 2008; 466: 813–819
- Anda S, Terjesen T, Kvistad KA. Computed tomography measurements of the acetabulum in adult dysplastic hips: which level is appropriate?. Skeletal Radiol. 1991; 20: 267–271
- Nakamura S, Yorikawa J, Otsuka K, Takeshita K, Harasawa A, Matsushita T. Evaluation of acetabular dysplasia using a top view of the hip on three-dimensional CT. J Orthop Sci. 2000; 5: 533–539
- Tallroth K, Lepistö J. Computed tomography measurement of acetabular dimensions: normal values for correction of dysplasia. Acta Orthop. 2006; 77: 598–602
- Anda S, Terjesen T, Kvistad KA, Svenningsen S. Acetabular angles and femoral anteversion in dysplastic hips in adults: CT investigation. J Comput Assist Tomogr. 1991; 15: 115–120
- Noble P, Kamaric E, Sugano N, Matsubara M, Harada Y, Ohzono K, Paravic V. Three-dimensional shape of the dysplastic femur: Implications for THR. Clin Orthop Relat Res. 2003; 417: 27–40
- Jacobsen S, Rømer L, Søballe K. The other hip in unilateral hip dysplasia. Clin Orthop Relat Res. 2006; 446: 239–246
- Wiberg G. Studies on dysplastic acetabula and congenital subluxation of the hip. With special reference to the complication of osteoarthritis. Acta Chir Scand. 1939; 83((suppl 58))5–135
- Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988; 232: 26–36
- Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995; 77: 73–85
- Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999; 363: 21–32
- Crockarell J, Jr, Trousdale RT, Cabanela ME, Berry DJ. Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin Orthop Relat Res. 1999; 363: 45–53
- Trumble SJ, Mayo KA, Mast JW. The periacetabular osteotomy. Minimum 2 year followup in more than 100 hips. Clin Orthop Relat Res. 1999; 363: 54–63
- Pogliacomi F, Stark A, Vaienti E, Wallensten R. Periacetabular osteotomy of the hip: the ilioinguinal approach. Acta Bio Medica. 2003; 74: 38–46
- Clohisy J, Barrett S, Gordon J, Delgado E, Schoenecker P. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005; 87: 254–259
- Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. Springer, Berlin, Heidelberg, New York 1987
- Clohisy J, Barrett S, Gordon J, Delgado E, Schoenecker P. Periacetabular osteotomy in the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2006; 88((suppl 1))65–83
- Mechlenburg I, Nyengaard J, Rømer L, Søballe K. Changes in load-bearing area after Ganz periacetabular osteotomy evaluated by multislice CT scanning and stereology. Acta Orthop Scand. 2004; 75: 147–153
- Peters CL, Erickson JA, Hines JL. Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am. 2006; 88: 1920–1926
- Søballe K. Pelvic osteotomy for acetabular dysplasia. Acta Orthop Scand. 2003; 74: 117–118
- Sharp I. Acetabular dysplasia. J Bone Joint Surg Br. 1961; 43: 268–272
- Heyman CH, Herndon CH. Legg-Perthes Disease. A method for the measurement of the roentgenographic result. J Bone Joint Surg Am. 1950; 32: 767–778
- Goodman SB. Comparison of radiographic parameters for analysis of normal and dysplastic hips in the adult. Contemp Orthop 1990; 20: 505–511
- Murray RO. The aetiology of primary osteoarthritis of the hip. Brit J Radiol. 1965; 38: 810–824
- Nötzli HP, Müller SM, Ganz R. The relationship between fovea capitis femoris and weight bearing area in the normal and dysplastic hip in adults: a radiologic study. Z Orthop. 2001; 139: 502–506, (In German)
- Okano K, Enomoto H, Osaki M, Shindo H. Outcome of rotational acetabular osteotomy for early hip osteoarthritis secondary to dysplasia related to femoral head shape. 49 hips followed for 10-17 years. Acta Orthopaedica. 2008; 79: 12–17
- Jacobsen S, Rømer L, Søballe K. Degeneration in dysplastic hips. A computer tomography study. Skeletal Radiol. 2005; 7: 1–7
- Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991; 73: 423–429
- Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy 2003; 19: 1055–60
- Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res 2004; 426: 145–50
- Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, Clohisy JC. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006; 88: 1448–57
- Jacobsen S. Adult hip dysplasia and osteoarthritis. Studies in radiology and clinical epidemiology. Acta Orthop. 2006; 77((Suppl 324))1–37
- Troelsen A., Jacobsen S, Bolvig L, Gelineck J, Rømer L, Søballe K. Ultrasound versus magnetic resonance arthrography in acetabular labral tear diagnostics: a prospective comparison in 20 dysplastic hips. Acta Radiologica 2007; 48: 1004–10
- Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. Instr Course Lect. 2001; 50: 229–38
- Garbuz DS, Masri BA, Haddad F, Duncan CP. Clinical and radiographic assessment of the young adult with symptomatic hip dysplasia. Clin Orthop Relat Res. 2004; 418: 18–22
- Croft P, Cooper C, Wickham C, Coggon D. Osteoarthritis of the hip and acetabular dysplasia. Ann Rheum Dis. 1991; 50: 308–310
- Smith RW, Egger P, Coggon D, Cawley MI, Cooper C. Osteoarthritis of the hip joint and acetabular dysplasia in women. Ann Rheum Dis. 1995; 54: 179–181
- Jacobsen S, Sonne-Holm S. Hip dysplasia: a significant risk factor for the development of hip osteoarthritis. A cross-sectional survey. Rheumatology (Oxford). 2005; 44: 211–218
- Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B. Joint space width in dysplasia of the hip: a case-control study of 81 adults followed for ten years. J Bone Joint Surg Br. 2005; 87: 471–477
- Murphy SB, Millis MB, Hall JE. Surgical correction of acetabular dysplasia in the adult. Clin Orthop Relat Res. 1999; 363: 38–44
- Garras DN, Crowder TT, Olson SA. Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg Br. 2007; 89: 721–724
- Cooperman DR, Wallensten R, Stulberg SD. Acetabular dysplasia in the adult. Clin Orthop Relat Res. 1983; 175: 79–85
- Hasegawa Y, Iwata H, Mizuno M, Genda E, Sato S, Miura T. The natural course of osteoarthritis of the hip due to subluxation or acetabular dysplasia. Arch Orthop Trauma Surg. 1992; 111: 187–191
- Murphy SB, Ganz R, Müller ME. The prognosis in untreated dysplasia of the hip. A study of radiographic factors that predict the outcome. J Bone Joint Surg Am. 1995; 77: 985–989
- Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech 2000; 33: 953–60
- Ferguson SJ, Bryant JT, Ganz R, Ito K. An in vitro investigation of acetabular labral seal in hip joint mechanics. J Biomech 2003; 36: 171–8
- McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res 2001; 393: 25–37
- McCarthy JC, Noble PC, Schuck MR, Wright J, Lee J. The watershed labral lesion: its relationship to early arthritis of the hip. J Arthroplasty 2001; 16(Suppl.1)81–7
- Crawford MJ, Dy CJ, Alexander JW, Thompson M, Schroder SJ, Vega CE, et al. The 2007 Frank Stinchfield Award. The biomechanics of the hip labrum and the stability of the hip. Clin Orthop Relat Res. 2007; 465: 16–22
- Mavcic B, Pompe B, Antolic V, Daniel M, Iglic A, Kralj-Iglic V. Mathematical estimation of stress distribution in normal and dysplastic human hips. J Orthop Res. 2002; 20: 1025–30
- Russell ME, Shivanna KH, Grosland NM, Pedersen DR. Cartilage contact pressure elevations in dysplastic hips: a chronic overload model. J Orthop Surg. 2006; 1: 6
- Mavcic B, Iglic A, Kralj-Iglic V, Brand RA, Vengust R. Cumulative hip contact stress predicts osteoarthritis in DDH. Clin Orthop Relat Res. 2008; 466: 884–91
- Steel HH. Triple osteotomy of the innominate bone. J Bone Joint Surg Am. 1973; 55: 343–50
- Schramm M, Hohmann D, Radespiel-Troger M, Pitto RP. Treatment of the dysplastic acetabulum with Wagner spherical osteotomy. A study of patients followed for a minimum of twenty years. J Bone Joint Surg Am. 2003; 85: 808–14
- Kralj M, Mavcic B, Antolic V, Iglic A, Kralj-Iglic V. The bernese periacetabular osteotomy: clinical, radiographic and mechanical 7-15-year follow-up of 26 hips. Acta Orthop. 2005; 76: 833–40
- Pogliacomi F, Stark A, Wallensten R. Periacetabular osteotomy. Good pain relief in symptomatic hip dysplasia, 32 patients followed for 4 years. Acta Orthop Scand. 2005; 76: 67–74
- Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year follow-up of bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008; 466: 1633–1644
- Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999; 363: 9–20
- Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999; 364: 92–98
- Hipp JA, Sugano N, Millis NB, Murphy SB. Planning acetabular redirection osteotomies based on joint contact pressures. Clin Orthop Relat Res. 1999; 364: 134–143
- Trousdale RT, Cabanela ME. Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop Scand. 2003; 74: 119–126
- Hussell JG, Mast JW, Mayo KA, Howie DW, Ganz R. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res. 1999; 363: 64–72
- Davey JP, Santore RF. Complications of periacetabular osteotomy. Clin Orthop Relat Res. 1999; 363: 21–32
- Hussell JG, Rodriguez JA, Ganz R. Technical complications of the Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999; 363: 81–92
- Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999; 363: 93–99
- Hsieh PH, Chang YH, Shih CH. Image-guided periacetabular osteotomy: computer-assisted navigation compared with the conventional technique: a randomized study of 36 patients followed for 2 years. Acta Orthop. 2006; 77: 591–597
- Langlotz F, Bächler R, Berlemann U, Nolte LP, Ganz R. Computer assistance for pelvic osteotomies. Clin Orthop Relat Res. 1998; 354: 92–102
- Langlotz F, Stucki M, Bächler R, Scheer C, Ganz R, Berlemann U, Nolte LP. The first twelve cases of computer assisted periacetabular osteotomy. Comput aided surg. 1997; 2: 317–326
- Armiger RS, Armand M, Lepisto J, Minhas D, Tallroth K, Mears SC, et al. Evaluation of a computerized measurement technique for joint alignment before and during periacetabular osteotomy. Comput Aided Surg. 2007; 12: 215–24
- Murphy S, Deshmukh R. Periacetabular osteotomy: preoperative radiographic predictors of outcome. Clin Orthop Relat Res. 2002; 405: 168–74
- Cunningham T, Jessel R, Zurakowski D, Millis MB, Kim YJ. Delayed gadolinium-enhanced magnetic resonance imaging of cartilage to predict early failure of Bernese periacetabular osteotomy for hip dysplasia. J Bone Joint Surg Am. 2006; 88: 1540–8
- Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007; 89: 1417–23
- Atwal NS, Bedi G, Lankester BJ, Campbell D, Gargan MF. Management of blood loss in periacetabular osteotomy. Hip Int. 2008; 18: 95–100
- van Bergayk AB, Garbuz DS. Quality of life and sports-specific outcomes after Bernese periacetabular osteotomy. J Bone Joint Surg Br. 2002; 84: 339–43
- Valenzuela RG, Cabanela ME, Trousdale RT. Sexual activity, pregnancy, and childbirth after periacetabular osteotomy. Clin Orthop Relat Res. 2004; 418: 146–52
- Mast JW, Brunner RL, Zebrack J. Recognizing acetabular version in the radiographic presentation of hip dysplasia. Clin Orthop Relat Res. 2004; 418: 48–53
- Sharrock NE, Salvati EA. Hypotensive epidural anesthesia for total hip arthroplasty: a review. Acta Orthop Scand. 1996; 67: 91–107
- Niemi TT, Pitkänen M, Syrjälä M, Rosenberg PH. Comparison of hypotensive epidural anaesthesia and spinal anaesthesia on blood loss and coagulation during and after total hip arthroplasty. Acta Anaesthesiol Scand. 2000; 44: 457–64
- Jacobsen S, Sonne-Holm S, Søballe K, Gebuhr P, Lund B. Hip dysplasia and osteoarthritis. A survey of 4.151 subjects from the osteoarthrosis substudy of the Copenhagen city heart study. Acta Orthop. 2005; 76: 149–58
- Okano K, Enomoto H, Osaki M, Shindo H. Joint congruency as an indication for rotational acetabular osteotomy. Clin Orthop Relat Res. Sep 3, 2008, [Epub ahead of print]
- Sharifi E, Sharifi H, Morshed S, Bozic K, Diab M. Cost-effectiveness analysis of periacetabular osteotomy. J Bone Joint Surg Am. 2008; 90: 1447–1456
- Larsson C, Saltvedt S, Wiklund I, Pahlen S, Andolf E. Estimation of blood loss after cesarean section and vaginal delivery has low validity with a tendency to exaggeration. Acta Obstet Gynecol Scand. 2006; 85: 1448–52
- Dildy GA, 3rd, Paine AR, George NC, Velasco C. Estimating blood loss: can teaching significantly improve visual estimation?. Obstet Gynecol. 2004; 104: 601–6
- Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004; 86: 561–5
- Foss NB, Kehlet H. Hidden blood loss after surgery for hip fracture. J Bone Joint Surg Br. 2006; 88: 1053–9
- Jacobsen S, Sonne-Holm S, Lund B, et al. Pelvic orientation and assessment of hip dysplasia in adults. Acta Orthop Scand. 2004; 75: 721–9
- Jamali AA, Mladenov K, Meyer DC, Martinez A, Beck M, Ganz R, Leunig M. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the ”cross-over-sign”. J Orthop Res. 2007; 25: 758–65
- Konishi N, Mieno T. Determination of acetabular coverage of the femoral head with use of a single anteroposterior radiograph. A new computerized technique. J Bone Joint Surg Am. 1993; 75: 1318–33
- Ball F, Kommenda K. Sources of error in the roentgen evaluation of the hip in infancy. Ann Radiol (Paris). 1968; 11: 298–303
- Portinaro NM, Murray DW, Bhullar TP, Benson MK. Errors in measurement of acetabular index. J Pediatr Orthop. 1995; 15: 780–4
- Kirkwood B, Sterne J. Essential medical statistics. 26: Survival analysis: displaying and comparing survival patterns. Blackwell, USA, UK, Australia 2003; 272–286
- Pedersen A, Johnsen S, Overgaard S, Søballe K, Sørensen HT, Lucht U. Registration in the danish hip arthroplasty registry: completeness of total hip arthroplasties and positive predictive value of registered diagnosis and postoperative complications. Acta Orthop Scand. 2004; 75: 434–41
- Larsen K, Sørensen OG, Hansen TB, Thomsen PB, Søballe K. Accelerated perioperative care and rehabilitation intervention for hip and knee replacement is effective: a randomized clinical trial involving 87 patients with 3 months of follow-up. Acta Orthop. 2008; 79: 149–59
- Husted H, Holm G, Jacobsen S. Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: fast-track experience in 712 patients. Acta Orthop. 2008; 79: 168–73
- Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986; 1: 307–310
- Bland JM, Altman DG. Applying the right statistics: analyses of measurement studies. Ultrasound Obstet Gynecol. 2003; 22: 85–93
- White J, Kelly M, Dunsmuir R. C-reactive protein level after total hip and total knee replacement. J Bone Joint Surg Br. 1998; 80: 909–11
- Larsson S, Thelander U, Friberg S. C-reactive protein (CRP) levels after elective orthopedic surgery. Clin Orthop Relat Res. 1992; 275: 237–42
- Ogonda L, Wilson R, Archbold P, Lawlor M, Humphreys P, O'Brien S, Beverland D. A minimal-incision technique in total hip arthroplasty does not improve early postoperative outcomes. A prospective, randomized, controlled trial. J Bone Joint Surg Am. 2005; 87: 701–10
- Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993; 292: 62–76