ABSTRACT
TBI and PTSD are global issues and are often referred to as signature wounds of the Iraq and Afghanistan wars. Art therapy can provide unique insights into military service members’ injuries and states of mind via externalisation within an art product; however, interpretation of results is complex and subjective. Advance neuroimaging tools such as resting state fMRI can be employed to demonstrate objective measures of brain structure and activity. This case series highlights two distinct patient profiles, suggesting a relationship between resting state connectivity maps and dynamic thalamic connectivity (as well as PCL-C and NSI scores and brain scars) and the corresponding visual elements of masks made during art therapy treatment. Ultimately, this study indicates a need for future research examining potential neurological changes pre- and post-art therapy treatment.
The identification of specific products, scientific instrumentation, or organization is considered an integral part of the scientific endeavor and does not constitute endorsement or implied endorsement on the part of the author, DoD, or any component agency. The views expressed in this study are those of the authors and do not reflect the official policy of the Department of Army/Navy/Air Force, Department of Defense, or U.S. Government.
Introduction
Traumatic brain injury (TBI) is prevalent among US military service members. Between 2000 and 2017, an estimated 370,688 service members (SMs) suffered from TBI, of which mild TBI (mTBI) accounts for 82% of all reported cases (Defense and Veterans Brain Injury Center, Citation2017). While most mTBI symptoms are transient and resolve within three months post-injury (Ruff, Citation2005), an estimated 20% of injured mTBI patients continue to experience chronic impairment (Nathan et al., Citation2015).
Neuroimaging tools such as functional magnetic resonance imaging (fMRI) can provide non-invasive objective information relating to injuries in moderate and severe TBI. However, there are no distinct indicators relating to mTBI, and imaging findings are often inconclusive. Objective, reliable mTBI biomarkers are not currently available, making detection and treatment of mTBI-related symptoms challenging, and significantly increasing the risk of misdiagnosis and/or the overlooking of symptoms. Each brain injury is unique to the precise incident and mechanical forces that caused it, areas of physical damage to the brain, and effects on the patient (Nathan, Bellgowan, et al., Citation2016; Nathan et al., Citation2015). A common saying in TBI clinics is ‘if you’ve met one person with TBI, you have met one person with TBI.’ In other words, no TBIs are the same. With modern medicine’s tendency to utilise diagnostic flow charts and broad population-based clinical practice guidelines to design treatments, individualising care for patients can be challenging.
Nonetheless, there are overlapping symptoms often reported by mTBI patients that pertain to changes in mood, including depression, PTSD, and anxiety (Silver, McAllister, & Yudofsky, Citation2011; Zasler, Katz, & Zafonte, Citation2012), as well as sensory-related changes such as headache and balance (Dolan et al., Citation2012; Zasler et al., Citation2012). These commonalities suggest potential systems or neural networks affected by TBI. One widely studied brain network by fMRI is the task-free default mode network (DMN) (Raichle et al., Citation2001). The DMN consists of a prominent, reproducible pattern of brain connectivity observed during the absence of explicit stimuli, during transitions between task performance (Raichle et al., Citation2001). Aberrant DMN connectivity has been reported in both mTBI and PTSD studies (Bonnelle et al., Citation2011; Nathan et al., Citation2015; Nathan et al., Citation2017; Spielberg, McGlinchey, Milberg, & Salat, Citation2015). Furthermore, some of these connectivity differences are found to correlate with symptoms such as increased fatigue, anxiety, and cognitive impairment (Broyd et al., Citation2009; Whitfield-Gabrieli & Ford, Citation2012).
TBI sustained during deployment is considered a significant predictor of the development of PTSD (Yurgil et al., Citation2014). Clinical symptoms of TBI and PTSD also have significant overlap and include sleep disruption, cognitive impairments (such as decreased memory or concentration), depression, and anxiety, to name a few (Dolan et al., Citation2012). Comorbid TBI and PTSD is a complex condition for which ‘personalized medicine’ methods would be tremendously useful. The National Intrepid Center of Excellence (NICoE), a military treatment centre at the Walter Reed National Military Medical Center (WRNMMC) in Bethesda, Maryland, US, utilises a four-week interdisciplinary programme for active duty SMs diagnosed with TBI and underlying psychological health conditions to include PTSD. A holistic care model is used to individualise diagnosis and treatment for the patient. The centre uses state-of-the-art neuroimaging and behavioural health/rehabilitative medical practices including an array of integrative treatments such as creative arts therapies to include art, music, and dance/movement therapy, which are psychotherapeutic in nature. Other integrative mind–body and wellness techniques, such as yoga, meditation, acupuncture, canine-assisted therapy, therapeutic writing, guided imagery, and biofeedback-assisted relaxation techniques, provide the SMs myriad treatment choices.
Integrative therapies utilised at the NICoE such as art therapy, during which SMs are active engagers rather than passive recipients, elevate the personal nature of treatment and also motivate SMs to be more invested in their care. Art therapy treatment provides an opportunity for an individual’s response or outcome from injury to be assessed using external depiction of internal symbolic and metaphorical content. Recent reports indicate thematic patterns of expression in mask making that may represent common types of injury or responses to trauma in SMs (Walker, Kaimal, Gonzaga, Myers-Coffman, & DeGraba, Citation2017). These studies demonstrate that art therapy, in this case a clinical mask-making directive, provided a platform in which patients were able to express emotions and feelings related to their experiences, often traumatic, and offered visual representations of the self (Walker et al., Citation2017). An analysis of nearly 400 masks found that the art therapy product may serve as a visual representation of the SM’s positive and negative aspects of self in relation to individual personhood, relationships, community, society, and changes over time (Walker et al., Citation2017). Further correlative investigation of the recurring themes in the mask-making products revealed that SMs with higher PTSD scores were more likely to create art therapy products referencing psychological injury and trauma. In contrast, SMs depicting fully integrated images or representing a strong sense of community (via unit insignia and patriotic themes with no fragmentation of visual elements) presented with lower PCL-M scores and PTSD diagnoses (Walker, Jones, & Kaimal, Citation2016).
In addition to using the DMN to study whole brain networks, researchers have sought to identify focal neuroimaging biomarkers sensitive to mTBI. One potential candidate for a brain trauma central biomarker is the thalamus (Nathan, Ollinger, Bonavia, & Riedy, Citation2016; Nathan et al., Citation2012; Sours, George, Zhuo, Roys, & Gullapalli, Citation2015; Tang et al., Citation2011). The thalamus is a focal point at which many brain connections converge. It is critical for processing, integrating, and communicating information across multiple brain regions and multifunctional networks (Kandel, Schwartz, & Jessell, Citation2000). The thalamus is also part of the limbic system (or ‘emotional brain’) and relays sensory and motor signals to the cerebral cortex for further evaluation. LeDoux (Citation1996) describes an alternate pathway, which he coined the ‘low road’ or ‘fast track,’ in which the thalamus feeds sensory information directly to the amygdala in order to ensure a rapid response to perceived survival threats (Carr, Citation2008). In these instances, the thalamus is vulnerable to becoming overwhelmed and can break down. As a result, trauma is often remembered not as a cohesive narration but rather as highly charged physical sensations (van der Kolk, Citation2014). Psychotherapeutic and sensory-based treatments such as art therapy are thought to help integrate and potentially give voice to the trauma experience (Collie, Backos, Malchiodi, & Spiegel, Citation2006; Gantt & Tripp, Citation2016; Lusebrink, Citation2004; Solomon & Siegal, Citation2003; van der Kolk, Citation2014).
In this series, we present a case report of instances where art therapy products created during mask-making and fMRI neuroimaging data represent two relatively distinct patient profiles.
Methods
Ten male SMs with chronic mTBI (time since most significant head injury 7.7 ± 5.8 years) were selected for this case series. The 10 subjects were chosen based on key themes represented in their masks. The first group (mean age 42.6 ± 7 years) depicted overarching themes related to pain and physical or psychological injury (Injured/Traumatic Group). The second group (mean age 38.2 ± 5 years) depicted overarching themes indicating patriotism and community, such as flags and unit insignia (Patriotic Group).
Subjects participated in the NICoE’s four-week interdisciplinary intensive outpatient programme. The patients received an advanced imaging fMRI examination during the second week and engaged in art therapy treatment throughout the four weeks, beginning with a group mask-making session in the first week.
This research was approved by the Institutional Review Board (IRB) of WRNMMC; all participants provided written informed consent.
Mask-making
At the end of the first week of NICoE’s four-week programme, all SMs (maximum six per group) engage in an art therapy mask-making directive. Facilitated by credentialed art therapists, the mask-making project is employed because the process helps patients focus on their own experiences with TBI and PTSD and offers a means to express inner mental states through a safe, externalised representation of the self (Jones, Walker, Masino Drass, & Kaimal, Citation2017; Walker, Citation2017). The SMs are introduced to art therapy as a treatment, and the concept of externalisation via symbolic art-making is discussed. Each SM is given a blank, undecorated papier mâché mask. Paints, clay, markers, and other miscellaneous supplies are set out. The SMs are invited to alter the mask, however, they would like (Jones et al., Citation2017; Walker, Citation2017). The initial session lasts two hours, with more time allotted in ensuing weeks. Some SMs continue to process the content of the masks throughout the four-week programme, and often use the art therapy products as platforms for trauma processing (Jones et al., Citation2017; Walker, Kaimal, Koffman, & Degraba, Citation2016). Art therapists’ observations, along with images of the masks themselves, are uploaded into the military’s electronic health record system – the Armed Forces Health Longitudinal Technology Application (AHLTA) – as part of standard clinical practice. This information on the 10 subjects was pulled retrospectively for and used to inform this case series.
fMRI
Advanced neuroimaging was performed on a 3 T MRI system with a 32-channel phased array head coil. The integrated advanced neuroimaging exam included high-resolution structural imaging along with fMRI, perfusion, diffusion tensor imaging (DTI), and spectroscopy. The task-free resting state functional data used in this study was acquired over a six-minute period at rest in the scanner with eyes closed for consistency, and to reduce potential eye strain and distractions. The fMRI data were intensity normalised, spatially blurred (6 mm FWHM Gaussian Filter), transformed to the MNI152 template and high-pass filtered (0.01 Hz) (Cox, Citation1996). Motion parameters, their first order derivatives, and physiological signals were regressed out. Structural fMRI scans were interpreted by a licensed neuroradiologist using the standardised common data elements for TBI (Duhaime et al., Citation2010). The number of T2 hyperintensities (brain scars) for each individual subject were catalogued as part of the neuroradiologist evaluation of the images (Riedy et al., Citation2016).
Resting state fMRI data
Two major analyses were conducted on the resting state fMRI data:
Default mode network analysis
The resting state fMRI data were decomposed into 25 independent components using probabilistic independent component analysis (Beckmann & Smith, Citation2004; Smith et al., Citation2004). Each component map was subsequently normalised with respect to the standard deviation of the residuals and the component matching the DMN based on the literature was extracted (Beckmann, DeLuca, Devlin, & Smith, Citation2005; Beckmann, Mackay, Filippini, & Smith, Citation2009; Smith et al., Citation2004). Spatial and temporal maps for each subject were obtained using the dual-regression method (Beckmann et al., Citation2009) and the raw single subject correlation maps were converted to z-scores representing the degree to which a specific subject’s resting state data correlate with the default mode component of the group data. Peak connectivity values within key regions of the default mode network were extracted.
Dynamics thalamic connectivity analysis
Time series from seven regions of the left and right thalamus each were extracted using the Oxford Thalamic Connectivity Atlas (Johansen-Berg et al., Citation2005). The principal singular vector of the time series within each region was used to calculate sliding window correlation matrices across thalamic regions (Window length = 100 s, Hamming filter (10%) tapered, time step 1 time point, total of 128 correlation matrices). Each matrix was thresholded (R2 ≥ 0.8, p < 0.001) and each connectivity pattern was assigned a specific symbol (Nathan, Ollinger, et al., Citation2016). Shannon’s Entropy was calculated for the symbol sequences of each thalamus (Nathan, Ollinger, et al., Citation2016).
On the day of their brain scan, all subjects also completed a series of self-reports. In this case series, we analyze and present data from the PTSD Checklist-Civilian Version (PCL-C) and the Neurobehavioral Symptom Inventory (NSI) form. All neuroimaging results and self-report data were compared.
Results
Overall there were marked differences in the fMRI results and the patient self-report exams between the two groups:
Case Series 1 (N = 5) as defined by SMs who represented injured/traumatic themes in mask products demonstrated low thalamic connectivity, low default mode network activity, high PTSD scores (average total score = 54.4), high symptomatology scores on the NSI (average total score = 41.6), and an average of 14 brain scars on the structural MRI scans for the entire group.
Example Patient from Case Series 1 (Injured/Traumatic Group):
Example patient from Case Series 1 is a 39-year-old male active duty SM with 22 years’ time-in-service and six combat deployments. The SM experienced multiple blast injuries from improvised explosive devices (IEDs) along with the loss of life of SMs under his command. He reported no loss of consciousness (LOC) but did experience multiple occurrences of alteration of consciousness (AOC) from these blast events. The SM was referred to the NICoE for history of TBI and possible PTSD (confirmed upon assessment, PCLC total = 77). The SM had experienced significant blast exposure and multiple traumatic losses. The SM’s symptomatology included headaches, sensitivity to light, cognitive difficulties, feelings of helplessness, remorse, hypervigilance, avoidance, and intrusive sensory memories (NSI total = 55). The SM also endorsed substance abuse as an attempt to numb painful experiences and emotions.
The SM was introduced to the mask-making directive in a group art therapy session and continued to work on it throughout his 4-week treatment at the NICoE. The SM’s mask () consisted of an ashen grey and white basecoat with “blood” emanating from the eyes, nose, mouth, and other wound-like gashes around the face. The SM painted the eyes black to indicate death, then altered a glue stick and placed it inside the mouth to represent the Combitube he had used to open his dying comrade’s airway. The SM added “dirt” fingerprints on the nose of the mask to reinforce the symbolism of the attempted mouth-to-mouth resuscitation. The SM explained that he approached the mask-making process intuitively as a response to his traumatic experiences and that it served as a “collage” of all the deaths he had witnessed, which remained frozen in his memory. The SM expressed that the mask enabled him to externalize those images (“get them out of his head”), as well as share his story with others.
Case Series 2 (N = 5) as defined by SMs who represented patriotic themes in mask products demonstrated high thalamic connectivity, high default mode network activity, low PTSD scores (average total score = 40.6), low symptomatology on the NSI (average total score = 28.2), and an average of one brain scars on the structural MRI scans for the entire group.
Example Patient from Case Series 2 (Patriotic Group):
Example patient from Case Series 2 is a 35-year-old male active-duty SM operator with 17 years’ time-in-service. The SM reported a history of multiple TBIs with one significant blast exposure without LOC but brief AOC. The SM’s symptoms included difficulty sleeping, poor memory and concentration, irritability, and headaches (NSI total = 10). The SM did not have a diagnosis of PTSD (PCLC total = 18). His treatment goals included decreased irritability and improved memory/concentration. The SM presented to the group art therapy session with a bright affect and immediately began work on his mask (), carefully depicting an American flag to symbolize his patriotic identity. The SM continued participating in art therapy throughout his treatment at the NICoE and completed a second canvas painting based on the scenic countryside from his childhood. The SM expressed that art therapy had been enjoyable and beneficial for him.
Comparison of fMRI, PCL-C and NSI data group averages
The figures below illustrate the group average differences between the two groups: Group1–Injured/Traumatic themes and Group 2 – Patriotic theme masks. demonstrates the differences in brain default mode network activity between the two groups, with lower DMN activity seen in Group 1. illustrates the differences in thalamic connectivity between the two groups, with lower thalamic connectivity detected in Group 1. summarises the average PCL-C and NSI scores for the two groups, with Group 1 trending towards higher symptomology and PTSD scores.
Figure 3. Resting state default mode network regions and corresponding average z-score connectivity values with 1 standard deviation from the mean. Results from Mann-Whitney U-tests at p < 0.05 denoted by *. (Group 1 = injured/traumatic, Group 2 = patriotic).
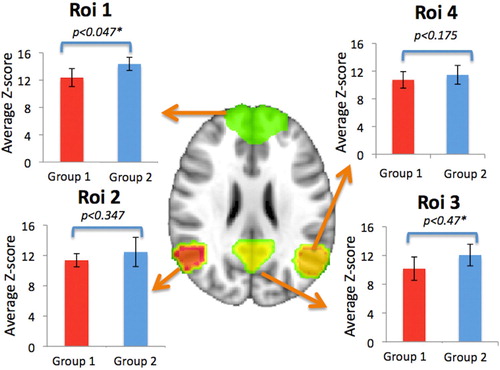
Figure 4. Dynamic connectivity of the left and right thalamus showing average Shannon’s Entropy measures with 1 standard deviation from the mean. Results from Mann-Whitney U-tests at p < 0.05 denoted by *. (Group 1 = injured/traumatic, Group 2 = patriotic).
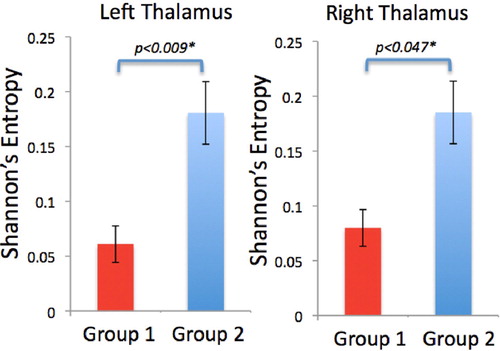
Figure 5. Average Total PCL-C scores and average total NSI scores with 1 standard error from the mean. Group 2 had overall lower total PCL-C and NSI scores. (Group 1 = injured/traumatic, Group 2 = patriotic).
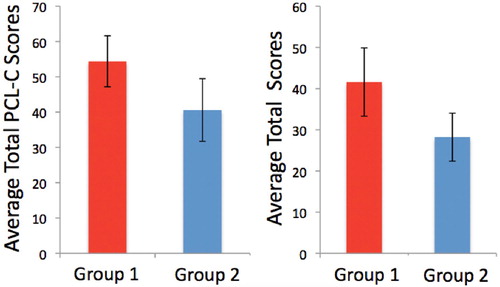
Note: While p-values are included in the below figures, the number of subjects in this case report is too small to draw any concrete conclusions about statistical significance. However, the authors believe the values found at least create an impetus for future research with a larger, statistically sound number of subjects.
Discussion
In this case series, distinctive associations were observed between the military service members’ art therapy products and advanced neuroimaging findings. SMs who expressed patriotic themes in mask products made in art therapy had fMRI results that were closer to non-injured military controls (data not shown) and reported less PTSD and symptomology. Conversely, the group that produced injured or trauma-themed masks demonstrated abnormal fMRI results, more brain scars, and increased PTSD and symptomology. One possible interpretation of this is that the patriotic groups’ physical and psychological injuries were either less severe or already somewhat compensated, suggesting the subjects in the group who expressed injured themes are still working through issues associated with TBI and PTSD. Alternatively, the subjects in the patriotic group could have attained better recovery of some symptoms in contrast to the other group of subjects. We also conjecture that fully integrated depictions of the US flag might represent protective factors for the SMs, including sense of belonging and of higher purpose in providing security to the country.
The two case examples featured in this paper support the possibility that visual elements of art therapy products (and their subjective, patient-reported descriptions and meaning) can be correlated with brain activity seen in fMRI scans. Further dissection of the abnormal fMRI results indicates the injured/traumatic-themed group presented with lower entropy in the thalamic region of the brain. Prior research suggests that trauma interrupts the normal functioning of the thalamus, causing it to shut down or slow due to sensory overload (van der Kolk, Citation2014). In other words, the brain is not able to integrate traumatic experiences, and the danger remains unprocessed and ongoing. Individuals often cope with this sensory overload via dissociation or numbing behaviours. Trauma survivors may also appear rigidly stuck in the past because the thalamus (responsible for sensory integration) and the Dorsolateral Prefrontal Cortex (the ‘timekeeper’) have gone off-line (van der Kolk, Citation2014). An essential part of the healing process is the reintegration of these various neurological systems since ‘consciousness arises from a continuous “dialogue” between the thalamus and the cortex’ (Carr, Citation2008; Llinás & Ribary, Citation2001). Additionally, art therapy is thought to engage the very sensory channels (kinesthetic, tactile, visual, etc.) that are hijacked by the injured brain during a traumatic event (Lusebrink, Citation2004). By promoting thalamic connectivity, art therapy can potentially help re-engage, re-integrate, and regulate consciousness. Creating a mask, in particular, seems to aid in identity formation and self-awareness after experiencing trauma (Walker et al., Citation2017). The art therapy process also allows distance between the person and the event in the form of a tangible record (i.e. the artwork). In the example of the more ‘injured’ patient, the SM indicated he was able to communicate previously unspeakable horrors and integrate the memories into the past.
Art therapy provides outward physical representations of thoughts, emotions, and feelings with unconstrained creative opportunity for self-representation which may provide a surrogate of ‘state of mind’ as captured by task-free resting state fMRI. Resting state fMRI is thought to provide a means to measure one’s ‘state of mind’ when the brain switches states during the absence or presence of stimuli. However, ‘state of mind’ is a complex idea and is determined by many factors such as emotions, feelings, and pathology which are often represented as differences in connectivity patterns in resting state fMRI. In this case series, the injured/traumatic group demonstrated lower DMN connectivity and entropy on resting state fMRI suggesting they could not put their minds at ease during rest. This group also demonstrated higher PTSD scores of which rumination and constant stress is a common symptom. For these patients, art therapy may help signal the shift from the survival brain, which is focused on self-preservation, to the learning brain, which is relaxed and receptive to new information (Ford, Citation2009; Tripp, Citation2016). However, future studies with larger sample sizes will be required to demonstrate correlations of art therapy results and the state of the human brain. Follow-up studies including fMRI pre- and post-treatment are needed to support the idea that engagement in art therapy can help to create healthier brain function and connectivity. Performing brain scans before and after art therapy treatment has the potential to monitor and demonstrate changes in the brain induced by not only mask-making but other directives used within art therapy, as well.
In future, larger-scale studies the authors are also interested to explore whether or not group dynamics or prospective career timeline (i.e. whether they are anticipating continued service or transitioning out of the military) affect service members’ choice of theme depiction. Themes would be monitored for patterns within patient cohorts to determine whether the service members are more comfortable depicting traumatic content if others from their cohort have opted to do so. Conversely, if they choose to avoid traumatic content if no one else from their cohort is openly symbolising such. Initial therapist impression is themes range within group and there are many variable which affect a service members’ choice of theme. Another variable to monitor is the patients’ prospective career timeline within career and whether service members who are about to leave the service feel more comfortable uncovering and processing traumatic content, while those who are planning to return to duty may feel the need to focus on service to their country and depict unified, patriotic themes surrounding the military experience. Of interest is whether any injured service members, according to their PCL-C and NSI scores, depicted integrated patriotic content and if so, what led to an avoidance of traumatic processing to include the variables just mentioned.
A key benefit of art therapy as observed by the authors is that the creative and psychotherapeutic processes provide patients with the opportunity to freely express symptoms and associated trauma, which are not merely physical in nature. The ability to express specific experiences, emotions or memories and the associated granularity/richness of those subjective psychological elements cannot fully be expressed with standard clinical testing. Cognitive and physical tasks involved in art-making can offer assessment opportunities, outcome improvement, and therapeutic, artistic, and verbal processing of the injury experience (David, Citation1999; Walker et al., Citation2017). The ‘open canvas’ concept of art therapy, therefore, offers a more robust and holistic option for describing trauma and disability in a respectful and dignified manner. This small case series illustrates the potential for combining personal, subjective and individualised patient outcomes in art therapy, and objective measures of brain activity and function with advanced fMRI. The integration of art therapy helps to better engage the patient in the treatment process, offers an additional perspective of the patient with complex injuries, and serves as a catalyst for personalised medicine.
Acknowledgements
We would like to thank Arnold Fisher and the Intrepid Fallen Heroes Fund for founding the National Intrepid Center of Excellence. The authors would also like to thank the National Endowment for the Arts for their support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Notes on contributors
Melissa S. Walker is the Healing Arts Program Coordinator and an art therapist at the National Intrepid Center of Excellence, a directorate of the Walter Reed National Military Medical Center, and Lead Art Therapist for Creative Forces: NEA Military Healing Arts Network. Melissa works with active duty service members suffering from traumatic brain injury and psychological health conditions. Dedicated to helping recovering military service members safely express their deep thoughts and emotions in a creative environment, Melissa has helped develop the Healing Arts Program at the National Intrepid Center of Excellence since 2010. There, she and her team engage patients in creative arts therapies, powerful treatments for helping them express their invisible wounds. Masks made by service members as part of the NICoE art therapy program were highlighted in a 2015 edition of the National Geographic magazine, and the program is also highlighted in Melissa's 2016 TED talk. Melissa received her Master's Degree in Art Therapy from New York University.
Adrienne M. Stamper, MA, is a Virginia native and earned her dual-Master's degree in Art Therapy and Counseling from George Washington University. She has clinical experience working with various populations, including inpatient-psychiatric, forensic, children suffering from emotional disorders, pediatric oncology, and our military. Adrienne is a dual American/Irish citizen, and has lived and studied abroad in both Rome and India. In 2016, she officially joined The Creative Forces: NEA Military Healing Arts Network, and treats active-duty service members who have been diagnosed with traumatic brain injury (TBI) and underlying psychological health conditions. She is passionate about healing the wounds of war and is particularly interested in exploring the neuroscience behind art therapy and trauma.
Dr. Dominic E. Nathan earned his Ph.D. in biomedical engineering from Marquette University under the guidance of Drs. Robert W. Prost, Ph.D. and Dean C. Jeutter, Ph.D. His dissertation focused on modeling cognitive processes of upper extremity motor control using artificial neural networks. Dr. Nathan is a contractor at the National Intrepid Center of Excellence, Walter Reed National Military Medical Center serving as a Computer Scientist in the department of Neuroradiology. His research interests span the areas of machine learning and nonlinear dynamics for modeling physiological signals and multi-modal data for traumatic brain injury clinical biomarker development.
Gerard Riedy, MD, PhD, is a board-certified neuroradiologist and PhD biochemist with training from Johns Hopkins and MIT. With $15 million in research grants he has directed the NICOE advanced neuroimaging laboratory since its inception in 2010. This laboratory focuses on the implementation and analysis of advanced neuroimaging techniques for the evaluation of military TBI and PTSD.
Additional information
Funding
References
- Beckmann, C. F., DeLuca, M., Devlin, J. T., & Smith, S. M. (2005). Investigations into resting-state connectivity using independent component analysis. Philosophical Transactions of the Royal Society B: Biological Sciences, 360, 1001–1013. doi: 10.1098/rstb.2005.1634
- Beckmann, C. F., Mackay, C. E., Filippini, N., & Smith, S. M. (2009). Group comparison of resting-state fMRI data using multi-subject ICA and dual regression. Neuroimage, 47(Suppl. 1), S148. doi: 10.1016/S1053-8119(09)71511-3
- Beckmann, C. F., & Smith, S. M. (2004). Probabilistic independent component analysis for functional magnetic resonance imaging. IEEE Transactions on Medical Imaging, 23, 137–152. doi: 10.1109/TMI.2003.822821
- Bonnelle, V., Leech, R., Kinnunen, K. M., Ham, T. E., Beckmann, C. F., De Boissezon, X., … Sharp, D. J. (2011). Default mode network connectivity predicts sustained attention deficits after traumatic brain injury. Journal of Neuroscience, 31(38), 13442–13451. doi: 10.1523/JNEUROSCI.1163-11.2011
- Broyd, S. J., Demanuele, C., Debener, S., Helps, S. K., James, C. J., & Sonuga-Barke, E. J. (2009). Default-mode brain dysfunction in mental disorders: A systematic review. Neuroscience & Biobehavioral Reviews, 33, 279–296. doi: 10.1016/j.neubiorev.2008.09.002
- Carr, R. (2008). Sensory processes and responses. In N. Hass-Cohen, & R. Carr (Eds.), Art therapy and clinical neuroscience. (pp. 2–61). London & Philadelphia: Jessica Kingsley Publishers.
- Collie, K., Backos, A., Malchiodi, C., & Spiegel, D. (2006). Art therapy for combat-related PTSD: Recommendations for research and practice. Art Therapy: Journal of the American Art Therapy Association, 23(4), 157–164. doi: 10.1080/07421656.2006.10129335
- Cox, R. W. (1996). AFNI: Software for analysis and visualization of functional magnetic resonance neuroimages. Computers and Biomedical Research, 29, 162–173. doi: 10.1006/cbmr.1996.0014
- David, I. R. (1999). An exploration of the role of art as therapy in rehabilitation from traumatic brain injury (Doctoral dissertation). The Union Institute: ProQuest Dissertations Publishing. Retrieved from http://search.proquest.com/docview/304569092
- Defense and Veterans Brain Injury Center. (2017). DoD Numbers for Traumatic Brain Injury Worldwide. Retrieved from https://dvbic.dcoe.mil/files/tbi-numbers/worldwide-totals-2000-2017_aug-10-2017_v1.0_2017-09-21.pdf
- Dolan, S., Martindale, S., Robinson, J., Kimbrel, N. A., Meyer, E. C., Kruse, M. I., … Gulliver, S. B. (2012). Neuropsychological sequelae of PTSD and TBI following War deployment among OEF/OIF veterans. Neuropsychology Review, 22(1), 21–34. doi: 10.1007/s11065-012-9190-5
- Duhaime, A. C., Gean, A. D., Haacke, E. M., Hicks, R., Wintermark, M., Mukherjee, P., … Riedy, G. (2010). Common data elements in radiologic imaging of traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 91(11), 1661–1666. doi: 10.1016/j.apmr.2010.07.238
- Ford, J. (2009). Neurobiological and development research: Clinical implications. In C. Courois, & J. Ford (Eds.), Treating complex traumatic stress disorders: An evidence-based guide (pp. 31–33). New York: W. W. Norton.
- Gantt, L., & Tripp, T. (2016). The image comes first: Treating pre-verbal trauma with art therapy. In J. King (Ed.), Art therapy and neuroscience: Theoretical and practical perspectives (p. 93). New York: Routledge.
- Johansen-Berg, H., Behrens, T. E., Sillery, E., Ciccarelli, O., Thompson, A. J., Smith, S. M., & Matthews, P. M. (2005). Functional–anatomical validation and individual variation of diffusion tractography-based segmentation of the human thalamus. Cerebral Cortex, 15(1), 31–39. doi: 10.1093/cercor/bhh105
- Jones, J. P., Walker, M. S., Masino Drass, J., & Kaimal, G. (2017). Art therapy interventions for active duty service members with post-traumatic stress disorder and traumatic brain injury. International Journal of Art Therapy, 23(2), 70–85. doi: 10.1080/17454832.2017.1388263
- Kandel, E. R., Schwartz, J. H., & Jessell, T. M. (2000). Principles of neural science (4th ed.). New York, NY: McGraw-Hill.
- LeDoux, J. E. (1996). The emotional brain: The mysterious underpinnings of emotional life. New York: Simon & Schuster.
- Llinás, R., & Ribary, U. (2001). Consciousness and the brain. The thalamocortical dialogue in health and disease. Annals of the New York Academy of Sciences, 929, 166–175. doi: 10.1111/j.1749-6632.2001.tb05715.x
- Lusebrink, V. J. (2004). Art therapy and the brain: An attempt to understand the underlying processes of art expression in therapy. Art Therapy: Journal of the American Art Therapy Association, 21(3), 125–135. doi: 10.1080/07421656.2004.10129496
- Nathan, D. E., Bellgowan, J. F., French, L. M., Wolf, J. P., Oakes, T., Mielke, J. B., … Riedy, G. (2017). Assessing the impact of post traumatic stress symptoms on resting state function networks in a military chronic mild traumatic brain injury sample. Brain Connectivity, 7(4), 236–249. doi: 10.1089/brain.2016.0433
- Nathan, D. E., Bellgowan, J. F., Oakes, T. R., French, L. M., Nadar, S. R., Sham, E. B., … Riedy, G. (2016). Assessing quantitative changes in intrinsic thalamic networks in blast and nonblast mild traumatic brain injury: Implications for mechanisms of injury. Brain Connectivity, 6(5), 389–402. doi: 10.1089/brain.2015.0403
- Nathan, D. E., Oakes, T. R., Yeh, P. H., French, L. M., Harper, J. F., Liu, W., … Riedy, G. (2015). Exploring variations in functional connectivity of the resting state default mode network in mild traumatic brain injury. Brain Connectivity, 5(2), 102–114. doi: 10.1089/brain.2014.0273
- Nathan, D. E., Ollinger, J., Bonavia, G. H., & Riedy, G. (2016). Exploring the quantification of dynamic functional connectivity within intrinsic thalamic networks of mild traumatic brain injured subjects using entropy. 5th biennial conference on resting state and brain connectivity, Austria.
- Nathan, D. E., Wang, B. Q., Wolfowitz, R. D., Liu, W., Yeh, P. H., Graner, J. L., … Riedy, G. (2012, August). Examining intrinsic thalamic resting state networks using graph theory analysis: Implications for mTBI detection. Engineering in medicine and biology society (EMBC), 2012 annual international conference of the IEEE, (pp. 5445–5448). IEEE.
- Raichle, M. E., MacLeod, A. M., Snyder, A. Z., Powers, W. J., Gusnard, D. A., & Shulman, G. L. (2001). A default mode of brain function. Proceedings of the National Academy of Sciences, 98, 676–682. doi: 10.1073/pnas.98.2.676
- Riedy, G., Senseney, J., Liu, W., Ollinger, J., Sham, E., Krapiva, P., … Oakes, T. R. (2016). Structural MRI radiologic findings in military traumatic brain injury. Radiology, 279(1), 207–215. doi: 10.1148/radiol.2015150438
- Ruff, R. (2005). Two decades of advances in understanding of mild traumatic brain injury. Journal of Head Trauma Rehabilitation, 20, 5–18. doi: 10.1097/00001199-200501000-00003
- Silver, J. M., McAllister, T. W., & Yudofsky, S. C. (2011). Textbook of traumatic brain injury. Arlington, VA: American Psychiatric Pub.
- Smith, S. M., Jenkinson, M., Woolrich, M. W., Beckmann, C. F., Behrens, T. E., Johansen-Berg, H., … Mattews, P. M. (2004). Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage, 23, S208–S219. doi: 10.1016/j.neuroimage.2004.07.051
- Solomon, M., & Siegel, D. (Eds.). (2003). Healing trauma: Attachment, mind, body and brain. New York: W.W. Norton.
- Sours, C., George, E. O., Zhuo, J., Roys, S., & Gullapalli, R. P. (2015). Hyper-connectivity of the thalamus during early stages following mild traumatic brain injury. Brain Imaging and Behavior, 9(3), 550–563. doi: 10.1007/s11682-015-9424-2
- Spielberg, J. M., McGlinchey, R. E., Milberg, W. P., & Salat, D. H. (2015). Brain network disturbance related to posttraumatic stress and traumatic brain injury in veterans. Biological Psychiatry, 78(3), 210–216. doi: 10.1016/j.biopsych.2015.02.013
- Tang, L., Ge, Y., Sodickson, D. K., Miles, L., Zhou, Y., Reaume, J., & Grossman, R. I. (2011). Thalamic resting-state functional networks: Disruption in patients with mild traumatic brain injury. Radiology, 260(3), 831–840. doi: 10.1148/radiol.11110014
- Tripp, T. (2016). A somatically-informed bilateral art therapy protocol for reprocessing trauma. In J. King (Ed.), Art therapy, trauma, and neuroscience: Theoretical and practical perspectives (p. 173). New York: Routledge.
- van der Kolk, B. A. (2014). The body keeps the score: Brain, mind, and body in the healing of trauma. New York: Viking.
- Walker, M. (2017). Art therapy approaches within the national intrepid center of excellence at walter reed national military medical center. In P. Howie (Ed.), Art therapy with military populations: History, innovation, and applications. (pp. 111–123). London: Routledge.
- Walker, M. S., Jones, J. P., & Kaimal, G. (2016, July). Art therapy for active duty military service members with TBI & PTSD. Paper presented at the annual meeting of the American Art therapy association, Baltimore, MD.
- Walker, M. S., Kaimal, G., Gonzaga, A., Myers-Coffman, K., & DeGraba, T. (2017). Active-duty military service members’ visual representations of PTSD and TBI in masks. International Journal of Qualitative Studies on Health and Well-Being 12(1), 1267317. doi: 10.1080/17482631.2016.1267317
- Walker, M. S., Kaimal, G., Koffman, R., & Degraba, T. J. (2016). Art therapy for PTSD and TBI: A senior active duty military service member’s therapeutic journey. The Arts in Psychotherapy, 49, 10–18. doi: 10.1016/j.aip.2016.05.015
- Whitfield-Gabrieli, S., & Ford, J. M. (2012). Default mode network activity and connectivity in psychopathology. Annual Review of Clinical Psychology, 8, 49–76. doi: 10.1146/annurev-clinpsy-032511-143049
- Yurgil, K., Barkauskas, D., Vasterling, J. J., Nivergelt, C., Larsan, G., Schork, N., & Baker, D. G. (2014). Association between traumatic brain injury and risk of posttraumatic stress disorder in active-duty marines. JAMA: The Journal of the American Medical Association, 71(2), 149–157.
- Zasler, N. D., Katz, D. I., & Zafonte, R. D. (Eds.). (2012). Brain injury medicine: Principles and practice. New York, NY: Demos Medical Publishing.


