ABSTRACT
Introduction
Atogepant is a selective calcitonin gene-related peptide (CGRP) receptor antagonist that is utilized in adults for the prevention of episodic and chronic migraine. Cumulative findings support the involvement of CGRP in migraine pathophysiology, and atogepant functions by competitively antagonizing CGRP receptors, which results in the inhibition of trigeminovascular nociception. The mechanism of action addresses the cause of migraine pain, providing an effective preventive treatment option.
Areas covered
The key milestones in its development, including preclinical achievements, phase I, II, and III clinical trials, and regulatory approvals are reviewed. Additionally, clinical efficacy, safety profile, and tolerability of atogepant are discussed. The literature review is based on a comprehensive search of English peer-reviewed articles from various electronic databases, including PubMed and ClinicalTrials.gov.
Expert opinion
The development of atogepant represents a significant breakthrough in migraine prevention, particularly due to its improved safety profile that reduces the risk of liver injury, which was a major limitation of first-generation gepants. Drug–drug interaction studies with atogepant highlight the necessity for more inclusive study populations. Given that migraine disproportionately affects females, future clinical development programs should include diverse patient demographics to ensure the findings are generalizable to all individuals suffering from migraine.
1. Introduction
The cumulative evidence following the discovery of calcitonin gene-related peptide (CGRP) resulted in the approval of migraine-specific therapies [Citation1]. CGRP is a 37-amino acid neurotransmitter released from the trigeminovascular system that facilitates nociceptive transmission and neurogenic inflammation [Citation2]. Its release facilitates the creation of hyper-responsive states of trigeminal afferents and second-order neurons in the trigeminal nucleus caudalis [Citation3]. Release of CGRP further contributes to pain sensitization through mast cell degranulation [Citation4]. A pivotal study demonstrated that CGRP is a relevant peptide released during a migraine attack, plus CGRP levels are elevated when pain is present and decrease interictally [Citation5–7]. Infusions of CGRP initiate premonitory symptoms and migraine-type attacks in individuals suffering from migraine and not in healthy volunteers [Citation8,Citation9]. Administration of triptans relieves migraine symptoms and normalizes CGRP levels in the peripheral blood [Citation10,Citation11]. CGRP receptor antagonists, commonly referred to as gepants, represent the latest class of drugs to receive approval for the targeted treatment of migraine. Gepants are competitive antagonists of CGRP receptors, with a consequent reversal of CGRP-mediated nociception. The antagonistic activity inhibits the intracellular increase of cyclic adenosine monophosphate (cAMP), ultimately leading to the inhibition of trigeminovascular nociception.
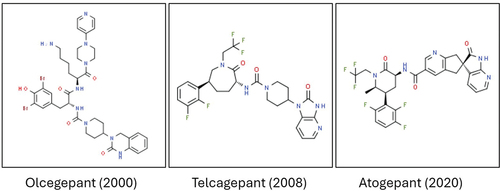
The earliest generation of gepants was introduced nearly two decades ago. Olcegepant was effective in aborting migraine attacks [Citation12], but the clinical development was interrupted due to difficulties in producing an oral formulation. Other gepants like telcagepant, MK-3207 and BI 44,370 TA demonstrated comparable effectiveness but the observed liver abnormalities prompted the discontinuation of clinical development [Citation13,Citation14]. Second-generation gepants that include ubrogepant, atogepant, and rimegepant did not exhibit any significant hepatotoxicity and are currently approved for the treatment of migraine [Citation15,Citation16]. They are available in various oral formulations, including pills and disintegrating tablets. This review centers its attention on atogepant, a potent CGRP receptor antagonist that is approved for migraine prophylaxis in adults with episodic and chronic migraine [Citation17]. Atogepant is chemically distinct from the earliest generation of gepants and was conceived with structural changes that reduce the formation of reactive metabolites. In this article, we provide a thorough review of the discovery strategy and following studies that substantiate the clinical utilization of atogepant.
2. Preclinical development and mechanism of action
Atogepant is a competitive antagonist for the human CGRP receptor. Preclinical activities evaluated the affinity and selectivity of atogepant in human embryonic kidney cells that expressed cloned CGRP receptors [Citation18]. Radioligand binding using [125I] hCGRP and cAMP accumulation assays assessed affinity, functional potency, and selectivity [Citation18]. CGRP receptor-binding affinity of atogepant was high and CGRP-stimulated cAMP responses were potently inhibited [Citation18]. Binding of [125I] hCGRP to cloned human CGRP receptors was inhibited with a Ki (± standard error of the mean) of 0.015 ± 0.002 nM [Citation18]. Atogepant showed a similar affinity for rhesus CGRP receptors (Ki = 0.009 nM) and a weaker affinity for rat (Ki = 0.7 nM) and dog CGRP receptors (Ki = 1.2 nM). In human and rhesus CGRP receptors, CGRP-stimulated cAMP responses were blocked by atogepant with a half-maximal inhibitory concentration (mean ± standard error of the mean) of 0.026 ± 0.005 nM and 0.045 ± 0.005 nM [Citation18]. Atogepant exhibited selectivity and inhibitory activity for CGRP and AMY1 receptors with a lack of noticeable affinities for calcitonin, adrenomedullin, and other neurotransmitter receptor targets [Citation18]. The half-maximal inhibitory concentration or IC50 of atogepant for CGRP and AMY1 receptors is 0.03 nM and 2.40 nM, respectively. Concomitant inhibition of AMY1 and CGRP receptors may provide additional benefits compared to inhibition of CGRP receptor alone. An academic study found that atogepant antagonizes CGRP vasorelaxation in human coronary, meningeal and cerebral arteries [Citation19]. A less potent antagonistic activity was observed in coronary arteries, implying that the prophylactic effects of atogepant may be mediated by preventing the vasodilatory response in cranial arteries [Citation19].
Pharmacodynamic evaluation of atogepant has been reported in a rat nitroglycerin (NTG) model of migraine and a capsaicin-induced dermal vasodilation (CIDV) experiment conducted in primates [Citation18]. In rats, NTG administration sensitizes trigeminal and cortical structures and produces attacks phenotypically similar to spontaneous migraine [Citation20]. The CIDV experiment has been previously used in the development strategy of CGRP therapeutics [Citation21,Citation22]. A dose-dependent reduction of facial allodynia was observed when atogepant (3–30 mg/kg) was administered 1 hour before NTG delivery [Citation18]. In addition, atogepant concentrations in the plasma and inhibition of CIDV were characterized by a predictable exposure/efficacy relationship [Citation18]. Atogepant produced significant CIDV inhibition with concentrations >20 nM not accompanied by an additional decrease in blood flow. In the off-target screen, atogepant at 10 μM was associated with <50% inhibition for more than 100 targets, including numerous transporters, enzymes, and neurotransmitter receptors [Citation18]. In rats, abrupt withdrawal after chronic dosing was characterized by minimal behavioral/physical signs, suggesting that atogepant acts outside of the central nervous system [Citation18]. Recent academic studies described that the analgesic effects of atogepant occur in trigeminal neurons through brief and immediate inhibitions of C-nociceptors and prolonged and delayed inhibitions of Aδ nociceptors, which differs from other preventive treatments of migraine like fremanezumab and onabotulinumtoxin A [Citation23–25]. Possible mechanisms of action of atogepant include inhibition of vasodilation, neurogenic inflammation, and nociceptive transmission induced by CGRP.
3. Pharmacokinetics
Atogepant pharmacokinetics is similar in individuals with migraine and healthy subjects. Following oral administration, effective plasma concentrations are reached within 30 minutes and time to reach peak plasma concentration (Tmax) is approximately 2 hours [Citation26]. The half-life is approximately 10 hours with no evidence of accumulation after repeated daily intake [Citation27]. There is a restricted penetration of the brain, and the apparent volume of distribution is high. Atogepant pharmacokinetics is dose proportional up to 300 mg/day with no relevant food effects [Citation27]. Hepatic metabolism occurs predominantly through oxidation via cytochrome P450 (CYP) 3A4, with the most prevalent circulating components in plasma being the parent compound and a glucuronide metabolite [Citation27]. A minor contribution occurs from CYP2D6 enzymes. Atogepant is a substrate of drug transporters, such as organic anion transporting polypeptide (OATP) and P-glycoprotein. Recommendations for dose adjustments with concomitant use of strong CYP3A4 inhibitors and OATP inhibitors have been provided (). Atogepant is mainly eliminated via feces and only to a lesser extent by the kidneys.
Table 1. Drug–drug interactions and recommendations for dose-adjustment of atogepant.
4. Clinical development
Oral atogepant was tested in two phase III studies conducted in adults with episodic and chronic migraine [Citation28,Citation29]. Earlier, a phase IIb/III dose-finding study was performed in adults with episodic migraine between 2016 and 2018 [Citation30]. The three studies evaluated the effects of atogepant administered every day for 3 months. The mean change from baseline in monthly migraine days (MMDs) was the primary endpoint. Secondary endpoints evaluated days with acute medication use, monthly headache days, average 50% reduction in 3-month MMDs and disability. In the dose/finding study, participants received placebo, atogepant every day (10, 30, or 60 mg) or atogepant twice a day (30 or 60 mg). Daily dosages of atogepant were more effective than placebo for the prevention of episodic migraine. In the ADVANCE study, adults with episodic migraine received placebo or atogepant every day (10, 30, or 60 mg). Daily administrations of atogepant were more effective than placebo for the prevention of migraine. In the PROGRESS study, adults with chronic migraine received placebo, atogepant every day (60 mg) or atogepant twice a day (30 mg). Daily atogepant and atogepant twice a day demonstrated superiority over placebo for the prevention of migraine. Of interest, atogepant improved patient-reported outcomes such as daily functioning and quality of life [Citation31]. A dedicated trial evaluated efficacy, safety, and tolerability of atogepant in adults with episodic migraine that previously tried two to four classes of conventional oral preventive therapies without success [Citation32]. A total of 315 participants received placebo or atogepant every day (60 mg) for 12 weeks. Compared with placebo, atogepant significantly reduced MMDs and days with acute medication use. In adults with episodic migraine, long-term tolerability and safety of atogepant every day (60 mg) were confirmed in a 40-week extension study [Citation33]. A further 52-week safety study reaffirmed the tolerability and safety of atogepant every day (60 mg) [Citation34]. Atogepant demonstrated sustained reductions in activity impairment and improvements in quality of life throughout the study year [Citation35]. Time course efficacy analyses demonstrated a rapid onset of action as early as 1 day and continued improvement over 52 weeks [Citation34,Citation36,Citation37]. The proportion of subjects with a value higher than or equal to 50%, 75%, and 100% reduction in MMDs was 60%, 37%, and 21% during weeks 1–4 and augmented to 84%, 70%, and 48% at the end of the year [Citation34]. An extension study of the PROGRESS trial has been completed in China, but only three subjects were recruited (NCT04829747). The reasons for the recruitment of only three subjects are unknown. More extension studies are currently ongoing (NCT04686136 and NCT05861427). The number of subjects experiencing treatment-emergent adverse events (TEAEs) was comparable across atogepant and placebo groups [Citation28,Citation29]. Common TEAEs related to atogepant were mild to moderate in severities, such as infections of the upper respiratory tract, nausea, constipation, and urinary tract infections [Citation34]. Transient elevations of hepatic enzymes resolved after atogepant discontinuation and no hepatic issues were reported [Citation34].
Atogepant received approval for the prophylaxis of episodic and chronic migraine with or without aura by the US Food and Drug Administration [Citation17]. More recently, atogepant has been approved in Mexico, Argentina, Canada and the European Union and is under review in several other countries. Oral doses of 10, 30, or 60 mg are taken once daily depending on migraine features, cerebrovascular comorbidities, old age and concomitant drugs. In healthy individuals, once-daily and repeated supratherapeutic doses (170 and 300 mg) were tolerated with no meaningful elevations in the plasma of serum alanine aminotransferase and did not affect cardiac repolarization [Citation38,Citation39]. Atogepant was not associated with any relevant pharmacokinetic change in individuals with mild, moderate, or severe hepatic impairment [Citation40]. Atogepant was not associated with any meaningful pharmacokinetic interactions with naproxen or acetaminophen [Citation41], ethinyl estradiol/levonorgestrel [Citation42], esomeprazole [Citation43] and topiramate [Citation44]. Concomitant administrations of multiple doses of itraconazole (a strong CYP3A4 inhibitor) and a single dose of rifampicin (a strong OATP inhibitor) significantly increased the systemic exposure of atogepant [Citation45]. To date, there is no evidence that administration of atogepant with CYP3A4 or OATP inhibitors could potentially relieve migraine without inducing side effects. Systemic exposure decreased when atogepant was co-administered with multiple doses of rifampicin (a strong CYP3A4 inducer) [Citation45]. No meaningful interactions were described when atogepant was co-administered with ubrogepant [Citation46] or sumatriptan [Citation47].
5. Post-launch
The availability of atogepant provides a valid therapy for patients who do not respond to oral conventional preventatives, such as antihypertensives, antiepileptics, and antidepressants. Competitors of atogepant are represented by monoclonal antibodies binding to the CGRP peptide (eptinezumab, fremanezumab, and galcanezumab) or its receptor (erenumab) and a second-generation gepant (rimegepant). The recommended dosage of atogepant is 60 mg daily, while it is advisable to lower the dose to 10 mg daily when CYP3A4 or OATP inhibitors are co-administered. Potent CYP3A4 inhibitors can increase systemic exposure to atogepant, whereas co-administrations with weak or moderate CYP3A4 inhibitors are not anticipated to be meaningful. Dose adjustment is not recommended in individuals with mild to moderate liver impairment, while atogepant should be avoided in cases of severe liver impairment. At the moment, the use of atogepant during lactation or pregnancy is not supported by data. The long half-life of a monoclonal antibody targeting the CGRP pathway may not be ideal in individuals with cardiovascular comorbidities and women who are pregnant or considering pregnancy. Real-world studies evaluating atogepant effects have not been published. A single case of secondary Raynaud´s phenomenon (RP) has been described in the digits after treatment with atogepant [Citation48]. When atogepant was discontinued, no further episodes of RP have been reported. The reporting of alopecia from the FDA Adverse Event Reporting System was low for atogepant [Citation49]. Real-world investigations require specific attention on elderly patients, females in pregnancy or with comorbid cardiovascular diseases. Further studies will evaluate the potential of atogepant for induction of medication overuse headache (MOH) during long-term treatment and the safety of combining atogepant with other CGRP therapeutics.
6. Expert opinion
The progress from the initial generation of gepants to the second and third generations, including atogepant, represents a breakthrough in the field of migraine therapeutics (). The earlier generation faced setbacks, with telcagepant, MK-3207, and BI 44,370 TA that raised alarms due to observed liver abnormalities. The improved safety profile of atogepant marks a positive trajectory in the development of migraine-specific therapies, ensuring patients have access to effective treatments with minimized risks. Drug-induced liver injury has been characterized between telcagepant and second-generation gepants [Citation50,Citation51]. Hepatotoxicity of telcagepant is led by a combined inhibition of electron transport chain and bile acid transporter, while the other gepants including atogepant display only a single mechanism as their biggest potential liability. Nowadays, it is possible to identify liver safety profiles of drugs in vitro and to predict hepatotoxicity in clinical trials [Citation52,Citation53].
Figure 1. Chemical structure of atogepant and previous-generation gepants. The number in brackets indicates the year of the first publication on the relevant gepant. The chemical structures were obtained from ChemSpider.com.
A critical examination of the drug–drug interaction studies conducted with atogepant reveals a gap in aligning study populations with the epidemiology of migraine, which predominantly affects females. Only a single study was exclusively performed in female participants [Citation42]. Two studies predominantly featured female participants [Citation45,Citation46], three included equal proportions of males and females [Citation38,Citation41,Citation43] and four were conducted in a predominantly male population [Citation39,Citation40,Citation44,Citation47]. Concerning the three studies that enrolled a comparable number of men and women, no sex-related differences were assessed. The low number of drug–drug interaction studies evaluating a predominantly female population poses challenges in extrapolating the findings to the broader population of migraine sufferers, particularly considering the known sex differences in migraine prevalence. A more balanced and inclusive approach to study populations, with a greater emphasis on the female demographic, could have provided a more comprehensive understanding of atogepant safety and drug–drug interactions.
In retrospect, the development of atogepant highlights the importance of continuous refinement and adaptation in drug discovery [Citation54,Citation55]. While addressing hepatic concerns marks a significant achievement, there is a need for more representative study populations in drug interaction studies. Moving forward, a concerted effort to ensure inclusivity in future clinical trials, particularly in conditions with known sex disparities like migraine, is necessary. This approach will enhance the generalizability of findings and ensure that treatments, such as atogepant, are tailored to meet the diverse needs of patients affected by migraine. Real-world studies with economical evaluations will clarify the impact of preventive therapy with atogepant on health services.
Article highlights
Atogepant is approved to prevent episodic and chronic migraine in adults.
Atogepant inhibits CGRP and AMY1 receptors primarily outside of the central nervous system.
Clinical success of atogepant overcomes the hepatotoxicity issues of first-generation gepants.
Drug–drug interaction studies with atogepant do not reflect the female predominance of migraine.
Atogepant effects in real-world data are currently missing.
Declaration of interest
C Baraldi has received fees and honoraria from Allergan, AbbVie, Lundbeck, Teva and Eli Lilly and Company. D Beier has participated in clinical trials, has given lectures, and has served on the advisory or speaker boards for Novartis, Eli Lilly, Lundbeck, Pfizer, Allergan/AbbVie and Teva. They have also received travel support from Allergan/AbbVie, Teva, Pfizer and Lundbeck outside the submitted work. P Martelletti is the editor and chief for The Journal of Headache and Pain and SN Comprehensive Clinical Medicine. He is also an EU Expert for the European Medicines Agency. L Pellesi has been employed by Lundbeck in the past 2 years. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Edvinsson L, Haanes KA, Warfvinge K, et al. CGRP as the target of new migraine therapies-successful translation from bench to clinic. Nat Rev Neurol. 2018;14(6):338–350. doi: 10.1038/s41582-018-0003-1
- Labastida-Ramírez A, Caronna E, Gollion C, et al. Mode and site of action of therapies targeting CGRP signaling. J Headache Pain. 2023;24(1):125. doi: 10.1186/s10194-023-01644-8
- Iyengar S, Johnson KW, Ossipov MH, et al. CGRP and the trigeminal system in migraine. Headache. 2019;59(5):659–681. doi: 10.1111/head.13529
- Balcziak LK, Russo AF. Dural immune cells, CGRP, and migraine. Front Neurol. 2022;13:874193. doi: 10.3389/fneur.2022.874193
- Goadsby PJ, Edvinsson L, Ekman R. Release of vasoactive peptides in the extracerebral circulation of humans and the cat during activation of the trigeminovascular system. Ann Neurol. 1988;23(2):193–196. doi: 10.1002/ana.410230214
- Goadsby PJ, Edvinsson L, Ekman R. Vasoactive peptide release in the extracerebral circulation of humans during migraine headache. Ann Neurol. 1990;28(2):183–187. doi: 10.1002/ana.410280213
- Gallai V, Sarchielli P, Floridi A, et al. Vasoactive peptide levels in the plasma of young migraine patients with and without aura assessed both interictally and ictally. Cephalagia. 1995;15(5):384–390. doi: 10.1046/j.1468-29821995.1505384.x
- Lassen L, Haderslev P, Jacobsen V, et al. CGRP may play a causative role in migraine. Cephalalgia. 2002;22(1):54–61. doi: 10.1046/j.1468-2982.2002.00310.x
- Guo S, Vollesen ALH, Olesen J, et al. Premonitory and nonheadache symptoms induced by CGRP and PACAP38 in patients with migraine. Pain. 2016;57(12):2773–2781. doi: 10.1097/j.pain.0000000000000702
- Goadsby PJ, Edvinsson L. The trigeminovascular system and migraine: studies characterizing cerebrovascular and neuropeptide changes seen in humans and cats. Ann Neurol. 1993;33(1):48–56. doi: 10.1002/ana.410330109
- Benemei S, Cortese F, Labastida-Ramírez A, et al. Triptans and CGRP blockade - impact on the cranial vasculature. J Headache Pain. 2017;18(1):103. doi: 10.1186/s10194-017-0811-5
- Olesen J, Diener HC, Husstedt IW, et al. Calcitonin gene-related peptide receptor antagonist BIBN 4096 BS for the acute treatment of migraine. N Engl J Med. 2004;350(11):1104–1110. doi: 10.1056/NEJMoa030505
- Ho TW, Mannix LK, Fan X, et al. Randomized controlled trial of an oral CGRP receptor antagonist, MK-0974, in acute treatment of migraine. Neurology. 2008;70(16):1304–1312. doi: 10.1212/01.WNL.0000286940.29755.61
- Tepper SJ. History and review of anti-calcitonin gene-related peptide (CGRP) therapies: from translational research to treatment. Headache. 2018;58(Supplement 3):238–275. doi: 10.1111/head.13379
- Negro A, Martelletti P. Gepants for the treatment of migraine. Expert Opin Investig Drugs. 2019;28(6):555–567. doi: 10.1080/13543784.2019.1618830
- Deng X, Zhou L, Liang C, et al. Comparison of effectiveness and safety of lasmiditan and CGRP-antagonists for the acute treatment of migraine in adults: systematic review and network meta-analysis of randomised trials. J Headache Pain. 2024;25(1):16. doi: 10.1186/s10194-024-01723-4
- Deeks ED. Atogepant: first approval. Drugs. 2022;82(1):65–70. doi: 10.1007/s40265-021-01644-5
- Moore E, Bell IM, Fraley ME, et al. Pharmacologic characterization of atogepant: a potent and selective calcitonin gene-related peptide receptor antagonist. Cephalalgia. 2024;44(1):3331024231226186. doi: 10.1177/03331024231226186
- Rubio-Beltran E, Chan KY, Danser AJ, et al. Characterisation of the calcitonin gene-related peptide receptor antagonists ubrogepant and atogepant in human isolated coronary, cerebral and middle meningeal arteries. Cephalalgia. 2020;40(4):357–366. doi: 10.1177/0333102419884943
- Sufka KJ, Staszko SM, Johnson AP, et al. Clinically relevant behavioral endpoints in a recurrent nitroglycerin migraine model in rats. J Headache Pain. 2016;17(1):40. doi: 10.1186/s10194-016-0624-y
- Hershey JC, Corcoran HA, Baskin EP, et al. Investigation of the species selectivity of a nonpeptide CGRP receptor antagonist using a novel pharmacodynamic assay. Regul Pept. 2005;127(1–3):71–77. doi: 10.1016/j.regpep.2004.10.010
- der Schueren BJ, de Hoon BJ, Vanmolkot FH, et al. Reproducibility of the capsaicin-induced dermal blood flow response as assessed by laser Doppler perfusion imaging. Br J Clin Pharmacol. 2007;64(5):580–590. doi: 10.1111/j.1365-2125.2007.02939.x
- Melo-Carrillo A, Strassman AM, Schain AJ, et al. Combined onabotulinumtoxinA/atogepant treatment blocks activation/sensitization of high-threshold and wide-dynamic range neurons. Cephalalgia. 2021;41(1):17–32. doi: 10.1177/0333102420970507
- Strassman AM, Melo-Carrillo A, Houle TT. Atogepant - an orally-administered CGRP antagonist - attenuates activation of meningeal nociceptors by CSD. Cephalalgia. 2022;42(9):933–943. doi: 10.1177/03331024221083544
- Melo-Carrillo A, Strassman AM, Broide R, et al. Novel insight into atogepant mechanisms of action in migraine prevention. Brain. 2024 Feb 27;awae062. doi: 10.1093/brain/awae062
- Boinpally R, Shebley M, Trugman JM. Atogepant: mechanism of action, clinical and translational science. Clin Transl Sci. 2024;17(1):e13707. doi: 10.1111/cts.13707
- QULIPTA (atogepant) [package insert]. North Chicago (IL) (USA): AbbVie Inc; 2023 Jun [cited 2024 Apr 11]. Available from: https://www.rxabbvie.com/pdf/QULIPTA_pi.pdf
- Ailani J, Lipton RB, Goadsby PJ, et al. Atogepant for the preventive treatment of migraine. N Engl J Med. 2021;385(8):695–706. doi: 10.1056/NEJMoa2035908
- Pozo-Rosich P, Ailani J, Ashina M, et al. Atogepant for the preventive treatment of chronic migraine (PROGRESS): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2023;402(10404):775–785. doi: 10.1016/S0140-6736(23)01049-8
- Goadsby PJ, Dodick DW, Ailani J, et al. Safety, tolerability, and efficacy of orally administered atogepant for the prevention of episodic migraine in adults: a double-blind, randomised phase 2b/3 trial. Lancet Neurol. 2020;19(9):727–737. doi: 10.1016/S1474-4422(20)30234-9
- Lipton RB, Pozo-Rosich P, Blumenfeld AM, et al. Effect of Atogepant for preventive migraine treatment on patient-reported outcomes in the randomized, double-blind, phase 3 ADVANCE trial. Neurology. 2023;100(8):e764–e777. doi: 10.1212/WNL.0000000000201568
- Tassorelli C, Nagy K, Pozo-Rosich P, et al. Safety and efficacy of atogepant for the preventive treatment of episodic migraine in adults for whom conventional oral preventive treatments have failed (ELEVATE): a randomised, placebo-controlled, phase 3b trial. Lancet Neurol. 2024;23(4):S1474–4422(24)00025–5. doi: 10.1016/S1474-4422(24)00025-5
- Klein BC, Miceli R, Severt L, et al. Safety and tolerability results of atogepant for the preventive treatment of episodic migraine from a 40-week, open-label multicenter extension of the phase 3 ADVANCE trial. Cephalalgia. 2023;43(1):3331024221128250. doi: 10.1177/03331024221128250
- Ashina M, Tepper SJ, Reuter U, et al. Once-daily oral atogepant for the long-term preventive treatment of migraine: findings from a multicenter, randomized, open-label, phase 3 trial. Headache. 2023;63(1):79–88. doi: 10.1111/head.14439
- Lipton RB, Halker Singh RB, Mechtler L, et al. Patient-reported migraine-specific quality of life, activity impairment and headache impact with once-daily atogepant for preventive treatment of migraine in a randomized, 52-week trial. Cephalalgia. 2023;51(8):3331024231190296. doi: 10.1177/03331024231190296
- Schwedt TJ, Lipton RB, Ailani J, et al. Time course of efficacy of atogepant for the preventive treatment of migraine: results from the randomized, double-blind ADVANCE trial. Cephalalgia. 2022;42(1):3–11. doi: 10.1177/03331024211042385
- Lipton RB, Pozo-Rosich P, Blumenfeld AM, et al. Rates of response to atogepant for migraine prophylaxis among adults: a secondary analysis of a randomized clinical trial. JAMA Netw Open. 2022;5(6):e2215499. doi: 10.1001/jamanetworkopen.2022.15499
- Boinpally R, McNamee B, Yao L, et al. A single supratherapeutic dose of atogepant does not affect cardiac repolarization in healthy adults: results from a randomized, single-dose, phase I crossover trial. Clin Pharmacol Drug Dev. 2021;10(9):1099–1107. doi: 10.1002/cpdd.940
- Min KC, Kraft WK, Bondiskey P, et al. Atogepant is not associated with clinically meaningful alanine aminotransferase elevations in healthy adults. Clin Transl Sci. 2021;14(2):599–605. doi: 10.1111/cts.12917
- Boinpally R, Jakate A, Butler M, et al. single-dose pharmacokinetics and safety of atogepant in adults with hepatic impairment: results from an open-label, phase I trial. Clin Pharmacol Drug Dev. 2021;10(7):726–733. doi: 10.1002/cpdd.916
- Boinpally R, Spaventa J, Chen K, et al. Evaluation of the pharmacokinetic interaction and safety of atogepant co-administered with acetaminophen or naproxen in healthy participants: a randomized trial. Clin Drug Investig. 2021;41(6):557–567. doi: 10.1007/s40261-021-01034-5
- Ankrom W, Xu J, Vallee MH, et al. Atogepant has no clinically relevant effects on the pharmacokinetics of an ethinyl estradiol/levonorgestrel oral contraceptive in healthy female participants. J Clin Pharmacol. 2020;60(9):1157–1165. doi: 10.1002/jcph.1610
- Boinpally R, Butler M, Rojo J, et al. Evaluation of the pharmacokinetic interactions and safety of atogepant coadministered with esomeprazole. Pain Manag. 2023;13(6):351–361. doi: 10.2217/pmt-2023-0040
- Boinpally R, McGeeney D, Borbridge L, et al. Pharmacokinetics and safety of coadministered atogepant and topiramate in healthy participants: a phase 1, open-label, drug-drug interaction study. Clin Pharmacol Drug Dev. 2023;12(10):1013–1021. doi: 10.1002/cpdd.1267
- Boinpally R, Chen W, McGeeney D, et al. Effects of CYP3A4 inhibition/induction and OATP inhibition on the pharmacokinetics of atogepant in healthy adults. Pain Manag. 2023;13(8):445–456. doi: 10.2217/pmt-2023-0056
- Blumenfeld AM, Boinpally R, De Abreu Ferreira R, et al. Phase Ib, open-label, fixed-sequence, drug-drug interaction, safety, and tolerability study between atogepant and ubrogepant in participants with a history of migraine. Headache. 2023;63(3):322–332. doi: 10.1111/head.14433
- Boinpally R, Jakate A, Butler M, et al. Atogepant and sumatriptan: no clinically relevant drug-drug interactions in a randomized, open-label, crossover trial. Pain Manag. 2022;12(4):499–508. doi: 10.2217/pmt-2021-0073
- Bedrin K, Ailani J, Dougherty C. Raynaud’s phenomenon associated with calcitonin gene-related peptide receptor antagonists case report. Headache. 2022;62(10):1419–1423. doi: 10.1111/head.14417
- Ruiz M, Cocores A, Tosti A, et al. Alopecia as an emerging adverse event to CGRP monoclonal antibodies: cases series, evaluation of FAERS, and literature review. Cephalalgia. 2023;43(2):3331024221143538. doi: 10.1177/03331024221143538
- Woodhead JL, Siler SQ, Howell BA, et al. Comparing the liver safety profiles of 4 next-generation CGRP receptor antagonists to the hepatotoxic CGRP inhibitor telcagepant using quantitative systems toxicology modeling. Toxicol Sci. 2022;188(1):108–116. doi: 10.1093/toxsci/kfac051
- Yamazaki M, Miyake M, Sato H, et al. Perturbation of bile acid homeostasis is an early pathogenesis event of drug induced liver injury in rats. Toxicol Appl Pharmacol. 2013;268(1):79–89. doi: 10.1016/j.taap.2013.01.018
- Woodhead JL, Pellegrini L, Shoda LKM, et al. Comparison of the hepatotoxic potential of two treatments for autosomal-dominant polycystic kidney disease using quantitative systems toxicology modeling. Pharm Res. 2020;37(2):24. doi: 10.1007/s11095-019-2726-0
- Woodhead JL, Yang K, Oldach D, et al. Analyzing the mechanisms behind macrolide antibiotic-induced liver injury using quantitative systems toxicology modeling. Pharm Res. 2019;36(3):48. doi: 10.1007/s11095-019-2582-y
- Tao X, Yan Z, Meng J, et al. The efficacy and safety of atogepant for the prophylactic treatment of migraine: evidence from randomized controlled trials. J Headache Pain. 2022;23(1):19. doi: 10.1186/s10194-022-01391-2
- Rizzoli P, Marmura MJ, Robblee J, et al. Safety and tolerability of atogepant for the preventive treatment of migraine: a post hoc analysis of pooled data from four clinical trials. J Headache Pain. 2024;25(1):35. doi: 10.1186/s10194-024-01736-z
