KEYWORDS:
1. Introduction
The outbreak of the coronavirus disease 2019 (COVID‐19) has posed an unprecedented challenge to the health care communities across the globe [Citation1]. As of June 17th, 2020, a total of 8,339,829 confirmed COVID-19 cases with 448,420 deaths have been reported [Citation2]. Different parts of the world are seeing different levels of COVID-19 activity with regards to the infection rate, susceptible population, and mortality rate. The COVID-19 pandemic is a rapidly evolving emergency and is a subject of regular debate and advanced research [Citation3,Citation4]. Patients with hematological disorders and solid malignancies have special needs and oncologists are facing a compound challenge [Citation5–Citation7].
2. Learning from previous outbreaks
COVID-19 pandemic is the 3rd outbreak of the 21st century [Citation8]. Every major outbreak is different and has unique challenges. To ensure the preparedness to manage cancer patients in COVID-19 times, lessons should be learned from the previous similar viral outbreaks of Severe Acute Respiratory Syndrome (SARS) and the Middle East respiratory syndrome (MERS) as all the three viruses belong to the same genus of ‘Beta coronaviruses’. Also, all three coronavirus outbreaks share similar symptoms of cough, fever, and shortness of breath, and can lead to pneumonia, acute respiratory distress syndrome (ARDS), and multiorgan failure [Citation9,Citation10].
Amongst all the three viral infections, SARS-CoV-2 is most infectious, and hence COVID-19 related morbidity has outnumbered the SARS and MERS combined disease burden by huge margins. In general, COVID-19 associated mortality (ranging from 1.38% to 3.4% in most studies) has been noted to be lower when compared to SARS (~10%) and MERS and SARS due to the larger (34–40%). Despite a lower-case fatality rate, the total number of deaths due to COVID-19 has outweighed that due to MERS and SARS due to the greater number of cases. Referring to oncology, cancer patients had a dismal outcome during the previous viral outbreaks [Citation11–Citation13]. As a group, cancer patients are vulnerable and have compromised overall health, and on anticancer drugs that also suppress the immune system. For instance, Alaskar et al reported a 100% mortality upon acquiring MERS in their case series of nine patients with cancer [Citation11].
Mortality Similarly, reports of cancer patients with COVID-19 have shown to be at a higher risk of becoming critically ill when compared to the general population [Citation14]. For instance, Wu et noted a case fatality rate of 5.6% in cancer patients with COVID-19 which was twice (2.3%) that of the overall case-fatality rate with COVID-19. Recent Nationwide data analysis by Liang et al on COVID-19 cases from 575 hospitals in China showed a higher cancer incidence in 1590 patients (1% vs 0.29%) than in the general Chinese population [Citation10]. Cancer patients had a higher risk of severe events (39% vs 8%; p = 0.0003) than non-cancer patients. Also, they found cancer patients with recent chemotherapy or surgery to have higher severe events than those without cancer treatment [Citation15].
3. Impact of Hematological malignancies on COVID-19 case rate, disease severity, and mortality rate
As the COVID-19 pandemic is evolving, our knowledge of the COVID-19 disease process is steadily increasing. So far, data on patients with cancer is limited, and with no definitive answers, cancer specialists are facing a huge clinical challenge and burden in their clinical practice. Hematological malignancies differ from solid malignancies in their prevalence, cancer biology, treatment response, and prognosis.
Multiple myeloma, leukemia, and lymphoma are preliminary bone marrow cancers. Similarly, Myelofibrosis, myelodysplastic syndrome, and aplastic anemia are the other hematological conditions defined by a variable amount of fibrosis, dysplasia, or hypo proliferation. Bone marrow failure, infiltration by leukemia cells, or suppression due to chemotherapy in turn leads to pancytopenia and/or febrile neutropenia.
So far, none of the studies have shown that patients with hematological malignancies are at increased risk to acquire the SARS-CoV-2 viral infection. However, there is ample evidence that confirms that once acquired, patients with malignancies tend to dismal outcome [Citation16–Citation18]. Hong et al from China reported a rapid transmission of COVID-19 disease in their hematology ward [Citation17]. They noted extremely high mortality (>50%) for inpatients of hematologic malignancies with COVID-19 Citation12.
A recent retrospective analysis of 128 hospitalized patients with hematological cancers in Wuhan, China was done, out of which 13 had COVID-19 [Citation19,Citation20]. The study compared hematological cancer patients who developed COVID-19 with (A) hematological cancer patients without COVID-19 and (B) health care providers with COVID-19. The important findings observed were no significant differences in baseline covariates were noted between patients with hematological cancers developing or not developing COVID-19 [Citation16]. Secondly, the case rate to develop COVID-19 was similar between hospitalized persons with hematological cancers (13 out of 128, 10%) compared with normal health care providers (16 out of 226, 7%). But, the severity of the COVID-19 disease and the associated case fatality rate was higher in the former group than the later (62% vs 0%, P = 0.002). This study suggests that there are no known factors that can preemptively indicate which hematological cancer patients have more chances to develop COVID-19. Also, a similar case rate suggests that the risk to acquire SARS-CoV-2 in an individual does not increase due to hematological cancer per se but once acquired, the severity and mortality are significantly higher than normal individuals Citation31.
A similar finding was noted by another study from Spain conducted by Martín-Moro et al [Citation20]. They noted that patients with concurrent hematological cancers and COVID-19 (13 cases) had a more severity and higher mortality (8 deaths out of 13 cases) when compared to 11 hospitalized health care providers with COVID-19 (0 deaths out of 11) Citation30.
4. Approach to patients with acute leukemias
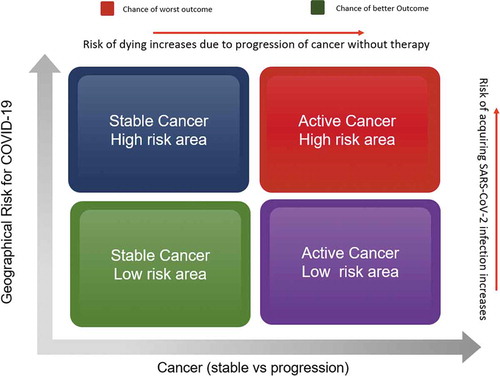
Based on the clinical experience from the retrospective studies on hematological malignancies with COVID-19, various hematology societies; The American Society of Hematology (ASH), The European Society for Medical Oncology (ESMO) and other experts have laid down interim recommendations [Citation17,Citation21,Citation22]. Although the current situation is liquid and subject to change, the COVID-19 pandemic is likely to stay with us for a considerable time in the future. This means that hematologists and transplant specialists across the globe need to work collaboratively to assist and learn from each other’s experiences ().
Figure 1. Hypothesis of the patient prognosis based on cancer stability and geographical risk of acquiring SARS-CoV-2 infection.
4.1. Acute lymphoblastic leukemia
Every attempt should be made to treat patients with a newly diagnosed with Acute lymphoblastic leukemia (ALL) with curative intent even during the COVID-19 pandemic. A nasopharyngeal swab for COVID screening along with a baseline Chest CT before induction as well as consolidation therapy is recommended even if there are no symptoms.
Factors that needs consideration while choosing the treatment protocol are (A) age of the patient (B) Status of Ph chromosome (C) COVID-19 status of the patient. The best treatment protocol should have minimal myelosuppression and risk to acquire COVID-19 without compromising the disease outcomes. Regimens like HCVAD (hyper fractionated cyclophosphamide, vincristine, doxorubicin, methotrexate, cytarabine, dexamethasone, and intrathecal chemotherapy) are usually well-tolerated by individuals (Ph-Negative ALL) younger than 60 years. For individuals, more than 60 years, other less intense options but with similar outcomes could be mini-HCVD + Inotuzumab (a monoclonal antibody against CD22). As steroids form an integral part of ALL treatment, experts suggest continuing to use steroids in patients with ALL unlike in general population where it is recommended to avoid steroids for the risk of acquiring SARS-CoV-2 secondary to steroid-induced immunosuppression. Patients with Ph-Positive ALL, tyrosine kinase inhibitors (TKIs) are the preferred agent of choice. Treatment with either ponatinib alone, ponatinib plus blinatumomab or low dose inotuzumab has been recommended. After the induction phase is over, every attempt should be made to give consolidation and maintenance therapies to ensure a better outcome.
4.2. Acute myeloid leukemia
Barring few adjustments, the overall management of newly diagnosed Acute myeloid leukemia (AML) should aim for curative intent and should not change during the COVID-19 pandemic (like treatment approach to ALL). Standard induction protocol should follow for younger individuals with age lesser than 60 years and if possible, should be treated as an inpatient to minimize the risk of exposure to SARS-CoV-2. In resource constraint settings, where hospitalization is not feasible due to high COVID-19 related disease load, or in individuals more than 60 years, the low-intensity protocol is preferred; Venetolax plus hypomethylating agents (HMA) or low-dose cytarabine (LDAC) + Venetolax or cladribine + LDAC ± Venetolax. Similar to ALL, patients with AML should also receive consolidation therapy and maintenance phase during COVID-19 pandemic (as an outpatient) to ensure disease remains in remission. For patients whose allogeneic HSCT is delayed due to the COVID-19 pandemic should be kept on the maintenance phase as a bridging therapy [Citation16].
5. Approach to patients with chronic leukemias
5.1. Chronic myeloid leukemia
Patients with chronic myeloid leukemia (CML) are not at a higher risk of acquiring SARS-CoV-2 infection than the general population. Also, the standard of care treatment with tyrosine kinase inhibitors (TKI) therapy does not cause immunosuppression and hence there is no rationale to delay or hold TKI therapy in patients with chronic-phase CML. The major concern that should be kept in mind is the toxicity profile of TKIs which often involves the cardiopulmonary system and might be confusing to COVID-19 pneumonia. For instance, amongst TKIs, dasatinib most commonly causes pleural effusion [Citation23]. Therefore, any patient with CML on TKIs if shows COVID-19 like symptoms should be tested with a nasopharyngeal swab for RTPCR along with (COVID-19-neutralizing IgG. If the patient found to be COVID-19 positive, TKIs should be temporarily held until recovery. In the case of COVID-19 negative result or if the IgG serology is positive, TKIs should be continued.
5.2. Chronic lymphocytic leukemia
Certain specific characteristics are specified in the case of Chronic lymphocytic leukemia (CLL). First, it is usually a disease of old individuals with a median age at diagnosis ranging from 65–70 years [Citation24]. Secondly, it is a B cell disorder and the associated hypogammaglobulinemia predisposes for increased risk of recurrent infections. CLL is the most common form of leukemia in the western world, and with the old age and other associated comorbidities, this population is likely to perform worse, however, this needs confirmation. Based on the International Workshop on Chronic Lymphocytic Leukemia (iwCLL), for those CLL patients in whom treatment is indicated, it is advisable to avoid intense regimens like fludarabine, cyclophosphamide, and rituximab (FCR) due to risk of severe myelosuppression [Citation25]. Similarly, the monoclonal antibodies, such as rituximab and obinutuzumab, may lead to B-cell depletion, reduce the humoral immunity further, and hence are recommended to avoid. Several oral target agents are now available, such as ibrutinib (BTK inhibitor), acalabrutinib (a second-generation BTK inhibitor), and venetoclax for use in CLL which can be used either alone or in combination depending upon various patient or disease-related risk factors.
6. Approach to Hematopoietic stem cell transplantation (HSCT) during the COVID-19 pandemic
Hematopoietic stem cell transplantation (HSCT) is one of the important treatment modalities for many hematologic malignancies. Unfortunately, there could be many immediate and long-term complexities of HSCT that include but not limited to graft-versus-host disease (GVHD), donor rejection, conditioning-related toxicity, relapse of primary cancer, and infections. Hence, during COVID-19 pandemic, the decision to proceed with HSCT in a case of hematological malignancy weighs on multiple factors; (A) disease status of patient, (B) performance status, (C) local case burden of COVID-19, (D) availability of alternative bridging therapy, (E) transplant center experience, (F) local guidelines and regulations. For instance, HSCT in a case of relapse refractory lymphoma might be an urgent indication while a case of multiple myeloma can be potentially postponed.
Thanks to the newer molecules and targeted therapies, many newer and less intense chemotherapy regimens have been found effective and can be used as a bridging therapy to keep the disease under control or in remission till the COVID-19 crisis is contained. An example of such bridging therapy could be the use of hypomethylating agents in acute myeloid leukemia and other hematological malignancies [Citation26]. In any scenario, hematologists and transplant specialists should discuss the benefits and harms of doing HSCT with the recipients before making a final decision. The shared decision making should be based on local guidelines and recommendations by various cancer societies and oncology experts.
Ensuring the wellbeing of the donor in case of unrelated HSCT is also prudent for the timely harvesting and availability of cells for transfusion. Alternative measures like cryopreserving donor’s stem cells have been recommended before initiating the conditioning regimen [Citation27,Citation28]. Hamadani et al recently used the Center for International Blood and Marrow Transplant Research (CIBMTR) database and compared the outcomes of HSCT using cryopreserved versus fresh grafts [Citation27]. They found that graft cryopreservation did not have any significant impact on bone marrow recovery, no increased risk of acute GVHD, and no decreased overall survival after allogeneic-HSCT. European society of blood and bone marrow transplantation (EBMT) and the World Marrow Donor Association (WMDA) has recently proposed guidelines for selecting and evaluating the donors and recipients based on their COVID-19 status, close contact with a confirmed COVID-19 case, recent travel, and severity of underlying cancer [Citation29–Citation32].
7. Risk of acquiring COVID-19 in a post-HSCT setting
During the post-HSCT period, the immune system is under the process of immunomodulation with gradual reconstitution of a donor-derived immune system. During this phase however, there is an increased risk to acquire opportunistic infections [Citation33,Citation34]. Similarly, transplant recipients are also at risk of acquiring SARS-CoV-2 infection owing to severe and prolonged marrow suppression and delayed immune recovery [Citation35]. In addition, differentiating COVID-19 related symptoms from other close mimickers is crucial due to difference in the management strategies. Recently, Dr. Per Ljungman from EBMT conducted a webinar on COVID-19 disease in post HSCT settings [Citation36]. As per the report, till 20 March 2020, Europe has already witnessed 15 cases of COVID-19 cases in post-HSCT setting (15 allogenic and 3 autologous). Out of these, one patient has succumbed to COVID-19 illness. Most cases were reported from Spain (5 patients) followed by Italy (3 patients). The median age of the patients was 59 years, 10 patients presented with upper respiratory symptoms, and remaining with lower respiratory tract systems. Based on this result, they recommended holding HSCT unless it is urgent.
8. Impact on cancer patients of reallocating resources toward COVID-19 care
Working in a resource constraint setting is one of the scenarios, which oncologists and hematologists from developed countries rarely experience. Heath care infrastructure of most of the developed countries like the US and Europe are overwhelmed while catering to patients with COVID-19. We believe this is the right time for oncologists to face the reality of rationalizing their limited resources toward patients who have the best chance to survive. Zhou et al recently reported that only one patient survived out of 32 COVID-19 patients who were mechanically ventilated in their study population [Citation37]. Based on this study plus our previous oncology experience, we know that cancer patients are usually poor performers owing to their compromised heart-lung functions and poor ECOG status. Hence, we strongly recommend that it is not too late to hold a preemptive end-of-life and palliative care discussion with cancer patients who might not benefit from aggressive measures in case they acquire SARS-CoV-2 infection. To cope up with the saturating health care infrastructure; for instance, higher demands for regular and ICU beds, personnel, blood products, etc. during the expected COVID surge, transplant centers have been postponing HSCTs whenever clinically possible [Citation38,Citation39].
9. Recognizing the scarcity of blood products
Blood Banks play a pivotal role in the orchestra of team managing sick and complex cases of cancer and HSCT. It has been observed worldwide that the COVID-19 pandemic has crumpled the supply chain of blood donation and refill of the blood stores leading to an unprecedented shortage of blood components. Pagano et al found that rechecking the blood request indications, ordering one unit at a time, and canceling elective surgeries were effective measures in replenishing the blood component stores in their facility [Citation40]. Such measures should be pro-actively implemented in all hospitals and medical centers so that a constant reserve pool of blood and other components are available to the needy 24 × 7. Similarly, there is an additional burden on the transfusion medicine team who also own the additional responsibility of arranging apheresis for procuring convalescent plasma therapy for critically ill patients with COVID-19 [Citation41].
10. Preventing burnout and providing supportive care
It is particularly important to ensure that health care providers and the supporting staff stay healthy, mentally as well as physically and motivated during COVID-19 crisis. Creating a multilayered approach with a strong back-up labor pool is recommended to ensure coverage is always available in case of urgent call out of a staff member due to COVID-19. At the same time, it is very important to ensure the emotional and physical well-being as provider burnout is expected during the care of COVID-19 patients [Citation42,Citation43]. Providing adequate PPEs, reallocating clinical duties of vulnerable staff like diabetics and pregnant women and regular psychological and mental evaluation are few of the many measures toward ensuring a healthy environment for the frontline staff. National Comprehensive Cancer Network (NCCN) has also reemphasized the importance of employee and leadership well-being to assure a safe work environment while providing comprehensive cancer care [Citation42,Citation43].
Similarly, we should also recognize the extreme stress and anxiety which many patients might be going through during COVID-19. One of the common concerns of cancer patients is whether having cancer makes them more prone to acquire SARS-CoV-2 infection [Citation8]. Other challenges like groceries, maintaining a healthy diet, planning travel are amongst the innumerable daily challenges faced by cancer patients. Most of the cancer centers are advocating for the avoidance of unnecessary office visits, postponing chemotherapy cycles or elective surgeries to a later date if the disease is stable, providing home visits with necessary labs and follow-ups, and utilizing telemedicine services to provide virtual consultations if required{Citation}. At the same time, patients are advised to avoid public transportation for travel, to cancel leisure trips, ensure adequate refills for drug prescriptions, and having an UpToDate vaccine status. These challenges are multifactorial and developing and developed countries have their unique hurdles to overcome [Citation6,Citation44].
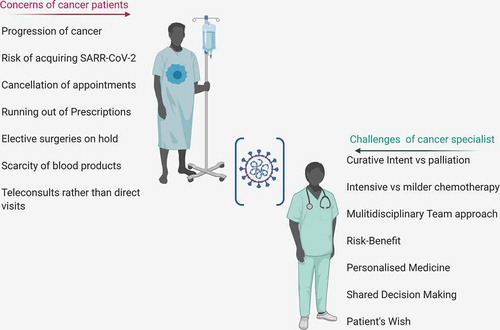
Other major concerns from the patient’s perspective could be the impact of missing scheduled chemotherapy cycles and fear of cancer recurrence. Few of the other practical hurdles which cancer patients are likely experiencing during current times are – inaccessibility to transport due to city lockdown, interruption in the anti-cancer drug supply, cancellation of appointments and elective surgeries, delay in chemotherapy cycles, halt of enrollment into clinical trials and so on () [Citation45]. A recent survey by Waterhouse et al on the challenges of conducting clinical trials during the COVID-19 pandemic discussed many difficulties currently being faced by researchers and investigators. Patients’ enrollment, protocol adherence, patient office visits, and scarce supporting staff and ancillary services, etc. are a few of the major setbacks to effectively conduct clinical trials during COVID-19 times [Citation46,Citation47].
Figure 2. A descriptive image outlining the challenges being faced by cancer patients and the specialist during COVID-19 pandemic.
It is difficult to quantify the damage which the cancer care discipline is suffering during the current COVID-19 pandemic. We recommend that conducting a transparent dialogue with the patients, explaining the scarcity of supplies, and offering them treatment with the best available evidence and resources is the most practical way to approach currently. There is also a concern that cancer patients might not respond appropriately to the vaccines for SARS-CoV-2, that means, the scientific societies must look for alternative effective prophylactic regimens and treatments against COVID-19 other than vaccines.
11. Conclusion
During the current COVID-19 crisis, the management of patients with hematological cancers and other solid malignancies continues to be challenging [Citation48]. Whenever possible, hematologists and cancer specialists should focus on collaborative effort and use similar guidelines consistently for patient care, so that some worthwhile data could be generated to practice evidence-based medicine. Also, a more dedicated data collection, and transparency in the patient reporting the need of the hour. The European Society for Medical Oncology (ESMO) has launched an international collaborative project, called the ESMO-CoCARE Registry which aims toward a timely and efficient data gathering on the current treatment approaches of cancer patients with COVID 19 [Citation49].
12. Expert Opinion
The current pandemic has evolved over the last few months. Our understanding of the disease and its pathogenesis is improving with each passing day. Patients with immunocompromised states need special attention and care during the COVID-19 pandemic. Current literature regarding the management of the patients of hematological malignancies with COVID-19 is sparse and various hematological societies have given interim recommendations to help the practicing hematologists and oncologists.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Sahu KK, Kumar R. Current perspective on pandemic of COVID-19 in the United States. J Fam Med Prim Care. 2020Apr 1;9(4):1784.
- Coronavirus Update (Live): 8,228,019 cases and 444,442 deaths from COVID-19 virus pandemic - worldometer [Internet]. [ cited 2020 Jun 17]. Available from: https://www.worldometers.info/coronavirus/#countries
- Sahu KK, Mishra AK, Lal A. Trajectory of the COVID-19 pandemic: chasing a moving target. Ann Transl Med. 2020 May 30;8(11):694.
- Cascella M, Rajnik M, Cuomo A, et al. Features, evaluation and treatment coronavirus (COVID-19). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 cited 2020 Jun 16. Available from: http://www.ncbi.nlm.nih.gov/books/NBK554776/
- Cruz MC, Flores JAS, Paule JR, et al. Adapting to the contemporary normal in cancer management and workflow during COVID-19 situation in the Philippines: multi-cancer center collaborative approach. Radiother Oncol J Eur Soc Ther Radiol Oncol. 2020 Jun 13;150:70–72.
- Trehan A, Jain R, Bansal D. Oncology care in a lower middle-income country during the COVID-19 pandemic. Pediatr Blood Cancer. 2020 Jun 15:e28438.
- Sahu KK, Siddiqui AD, Cerny J. Managing sickle cell patients with COVID-19 infection: the need to pool our collective experience. Br J Haematol. 2020 May 23. DOI:10.1111/bjh.16880.
- Sahu KK, Mishra AK, Lal A. Coronavirus disease-2019: an update on third coronavirus outbreak of 21st century. QJM Mon J Assoc Physicians. 2020 01;113(5):384–386.
- Lal A, Mishra AK, Sahu KK. CT chest findings in coronavirus disease-19 (COVID-19). J Formos Med Assoc. 2020;119(5):1000–1001.
- Mishra AK, Sahu KK, Lal A, et al. Patterns of heart injury in COVID - 19 and relation to outcome. J Med Virol. 2020 Apr 8. DOI:10.1002/jmv.25847.
- Alaskar A, Bosaeed M, Rehan H, et al. Middle East Respiratory Syndrome (MERS) infection in hematological and oncological patients: a case series from a tertiary care center in Saudi Arabia. Blood. 2019 Nov 13;134(Supplement_1):5871.
- Ángeles-Sistac D, Martin-Onraet A, Cornejo-Juárez P, et al. Influenza in patients with cancer after 2009 pandemic AH1N1: an 8-year follow-up study in Mexico. Influenza Other Respir Viruses. 2020;14(2):196–203.
- Chen Y-M, Perng R-P, Chu H, et al. Impact of severe acute respiratory syndrome on the status of lung cancer chemotherapy patients and a correlation of the signs and symptoms. Lung Cancer Amst Neth. 2004 Jul;45(1):39–43.
- Wu J, Liu J, Zhao X, et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu province: a multicenter descriptive study. Clin Infect Dis Off Publ Infect Dis Soc Am. 2020 Feb 29:ciaa199.
- Liang W, Guan W, Chen R, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–337.
- Gavillet M, Carr Klappert J, Spertini O, et al. Acute leukemia in the time of COVID-19. Leuk Res. 2020 Mar 26;92:106353.
- COVID-19 Lessons from Wuhan. Hematology.org [Internet]. [ cited 2020 Jun 16]. Available from: https://www.hematology.org/covid-19/covid-19-lessons-from-wuhan
- Paul S, Rausch CR, Jain N, et al. Treating leukemia in the time of COVID-19. Acta Haematol. 2020 May 11:1–13. DOI:10.1159/000508199.
- He W, Chen L, Chen L, et al. COVID-19 in persons with haematological cancers. Leukemia. 2020;34(6):1637–1645.
- Martín-Moro F, Marquet J, Piris M, et al. Survival study of hospitalised patients with concurrent COVID-19 and haematological malignancies. Br J Haematol. 2020 May 7. DOI:10.1111/bjh.16801.
- ESMO. Cancer patient management during the COVID-19 Pandemic [Internet]. [ cited 2020 Jun 16]. Available from: https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic
- Sahu KK, Siddiqui AD. From hematologist’s desk: the effect of COVID-19 on the blood system [published online ahead of print, 2020 May 1]. Am J Hematol. 2020. DOI:10.1002/ajh.25849
- Mishra AK, Sahu KK, Kaul S, et al. Dasatinib induced pleuro-pericardial effusion. Acta Bio-Medica Atenei Parm. 2020 19;91(1):142–143.
- Parikh SA, Rabe KG, Kay NE, et al. Chronic lymphocytic leukemia in young (≤ 55 years) patients: a comprehensive analysis of prognostic factors and outcomes. Haematologica. 2014 Jan;99(1):140–147.
- Treon SP, Castillo JJ, Skarbnik AP, et al. The BTK inhibitor ibrutinib may protect against pulmonary injury in COVID-19–infected patients. Blood. 2020 May 21;135(21):1912–1915.
- Pollyea DA, Amaya M, Strati P, et al. Venetoclax for AML: changing the treatment paradigm. Blood Adv. 2019 23;3(24):4326–4335.
- Hamadani M, Zhang M-J, Tang X-Y, et al. Graft cryopreservation does not impact overall survival after allogeneic hematopoietic cell transplantation using post-transplantation cyclophosphamide for graft-versus-host disease prophylaxis. Biol Blood Marrow Transplant J Am Soc Blood Marrow Transplant. 2020 Apr 10;26:1312–1317.
- Managing donor collections during the COVID-19 pandemic [Internet]. Be The Match BioTherapies; 2020 cited 2020 Jun 16. Available from: https://bethematchbiotherapies.com/cell-lines-blog/donor-collections-covid-19/
- Sahu KK, Jindal V, Siddiqui AD, et al. Facing COVID-19 in the hematopoietic cell transplant setting: a new challenge for transplantation physicians. Blood Cells Mol Dis. 2020 Jul 83;83:102439.
- Sahu KK, Siddiqui AD, Cerny J. COVID-19 pandemic and impact on hematopoietic stem cell transplantation. Bone Marrow Transplant. 2020 May 4. DOI:10.1038/s41409-020-0913-6.
- II P. COVID-19 and EBMT recommendations for patients with hematological malignancies [Internet]. [ cited 2020 Jun 16]. Available from: https://gvhdhub.com/medical-information/covid-19-and-ebmt-recommendations-for-patients-with-hematological-malignancies
- Coronavirus - SARS-CoV-2 & COVID-19 - WMDA donor medical suitability recommendations - share [Internet]. [ cited 2020 Jun 16]. Available from: https://share.wmda.info/pages/viewpage.action?pageId=344866320#/
- Ogonek J, Kralj Juric M, Ghimire S, et al. Immune reconstitution after allogeneic hematopoietic stem cell transplantation. Front Immunol. 2016;7:507.
- Sahu KK, Mahagaokar K, Patel B, et al. Strongyloides stercoralis hyperinfection syndrome in mantle cell lymphoma in post-transplant setting. Ann Hematol. 2020 May 6. DOI:10.1007/s00277-020-04049-8.
- Sahu KK, Mishra AK, Martin K, et al. COVID-19 and clinical mimics. Correct diagnosis is the key to appropriate therapy. Monaldi Arch Chest Dis Arch Monaldi Mal Torace. 2020 May 6;90(2).
- Ljungman P, Mikulska M, de la Camara R, et al. The challenge of COVID-19 and hematopoietic cell transplantation; EBMT recommendations for management of hematopoietic cell transplant recipients, their donors, and patients undergoing CAR T-cell therapy. Bone Marrow Transplant. 2020 May 13:1–6. Ahead of print.
- Szer J, Weisdorf D, Querol S, et al. The impact of COVID-19 on the provision of donor hematopoietic stem cell products worldwide: collateral damage. Bone Marrow Transplant. 2020 Mar 23. DOI:10.1038/s41409-020-0873-x.
- Zhou F, Yu T, Du R, et al. Clinical course, and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054–1062.
- Sahu KK, Kumar R. Preventive and treatment strategies of COVID-19: from community to clinical trials. J Fam Med Prim Care. 2020 May 1;9(5):2149.
- Pagano MB, Hess JR, Tsang HC, et al. Prepare to adapt blood supply and transfusion support during the first 2 weeks of the 2019 novel coronavirus (COVID-19) pandemic affecting Washington State. Transfusion (Paris). 2020;60(5):908–911.
- Sahu KK, Jindal V, Siddiqui AD, et al. Convalescent plasma therapy: a passive therapy for an aggressive COVID-19. J Med Virol. 2020 May 21. DOI:10.1002/jmv.26047.
- Dickerson D. Seven tips to manage your mental health and well-being during the COVID-19 outbreak [published online ahead of print, 2020 Mar 26]. Nature. 2020. DOI:10.1038/d41586-020-00933-5
- Ueda M, Martins R, Hendrie PC, et al. Managing cancer care during the COVID-19 pandemic: agility and collaboration toward a common goal. J Natl Compr Cancer Netw JNCCN. 2020 Mar:1–4.
- Sahu KK, Mishra AK, Lal A, et al. India fights back: COVID-19 pandemic. Heart Lung J Crit Care. 2020 Apr 23. DOI:10.1016/j.hrtlng.2020.04.014.
- Jindal V, Sahu KK, Gaikazian S, et al. Cancer treatment during COVID-19 pandemic. Med Oncol Northwood Lond Engl. 2020 May 29;37(7):58.
- Waterhouse DM, Harvey RD, Hurley P, et al. Early impact of COVID-19 on the conduct of oncology clinical trials and long-term opportunities for transformation: findings from an American Society of clinical oncology survey. JCO Oncol Pract. 2020 May 12:OP2000275. DOI:10.1200/OP.20.00275.
- He Y, Lin Z, Tang D, et al. Strategic plan for management of COVID-19 in paediatric haematology and oncology departments. Lancet Haematol. 2020 May;7(5):e359–62.
- ESMO-CoCARE Registry | ESMO [Internet]. [ cited 2020 Jun 17]. Available from: https://www.esmo.org/covid-19-and-cancer/collaborating-on-registries-studies-and-surveys/esmo-cocare-registry
- Sahu KK, Jindal V, Siddiqui AD. Managing COVID-19 in patients with cancer: a double blow for oncologists. JCO Oncol Pract. 2020;16(5):223–225.
