ABSTRACT
Background
Long-COVID diagnosis is prominent, and our attention must support those experiencing debilitating and long-standing symptoms. To establish patient pathways, we must consider the societal and economic impacts of sustained COVID-19. Accordingly, we sought to determine the pertinent areas impacting quality of life (QoL) following a COVID-19 infection.
Research methods
Three hundred and eighty-one participants completed a web-based survey (83% female, 17% male) consisting of 70 questions across 7 sections (demographics, COVID-19 symptoms; QoL; sleep quality; breathlessness; physical activity and mental health). Mean age, height, body mass and body mass index (BMI) were 42 ± 12 years, 167.6 ± 10.4 cm, 81.2 ± 22.2 kg, and 29.1 ± 8.4 kg.m2, respectively.
Results
Participant health was reduced because of COVID-19 symptoms (‘Good health’ to ‘Poor health’ [P < 0.001]). Survey respondents who work reported ongoing issues with performing moderate (83%) and vigorous (79%) work-related activities.
Conclusions
COVID-19 patients report reduced capacity to participate in activities associated with daily life, including employment activities. Bespoke COVID-19 support pathways must consider multi-disciplinary approaches that address the holistic needs of patients to restore pre-pandemic quality of life and address experienced health and wellbeing challenges.
Plain Language Summary: The long-term impact of long-COVID has a dramatic impact upon daily activities and lifestyle. The development of bespoke support pathways to support patients must address the physical and psychological considerations to adequately restore pre-COVID quality of life and address broader societal and economic implications, especially for those that are of working age.
1. Introduction
The introduction of widespread and efficacious vaccination programmes globally has played an integral part in reducing transmission [Citation1], admission to intensive care units [Citation2] and mortality [Citation3] associated with Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2). Effective treatment and management strategies have been implemented to manage clinical presentations [Citation4] however, attention must be directed to increasing the understanding and support for the millions of people globally experiencing severe and debilitating symptom profiles associated with post-coronavirus disease 2019 (COVID-19) syndrome or long-COVID. Affecting 1 in 10 patients [Citation5], long-COVID is clinically defined as a complex symptom profile that develops during or after a COVID-19 infection, continues for >3 months and is not explained by an alternative diagnosis [Citation6]. With reports of sustained symptoms and morbidity in the months and now, years following acute infection, there is a growing demand on health care systems globally to support and rehabilitate patients. And reestablish pre-COVID health status and quality of life (QoL) [Citation7]. Whilst there is currently no established trajectory toward recovery, long-COVID is likely to pose long-term challenges to health and wellbeing, and broad societal and economic impacts [Citation8].
Whilst cases of long-COVID rise exponentially, the extent of symptom prevalence and severity is broad; at this point, there is limited knowledge of risk factors and attributable mechanisms for long-COVID [Citation9]. Whilst global efforts to increase the understanding of long-COVID gains momentum, information relating to the symptom prevalence, severity and impact upon the individuals are greatly needed to inform the development of COVID-19 specific support pathways and rehabilitation services. To be truly effective, the patient support pathways will undoubtedly be as complex as the symptomology, creating a unique challenge for clinical and non-clinical entities to work collaboratively in the interest of achieving improved patient outcomes. Therefore, engaging multi-disciplinary stakeholder groups to support healthcare leaders in a systems approach will be imperative to developing bespoke COVID-19 approaches and achieving widespread patient benefit [Citation10]. To be successful, there is a need to characterize symptom profile and the impacts upon QoL, activities of daily life and importantly, the lived experience [Citation11].
To date, an abundance of cohort studies from acute and clinical settings demonstrate a broad symptom profile and prevalence as synthesized by Hayes et al [Citation12], whereby, it is acknowledged that long-COVID symptoms and severity are disparate from acute COVID-19 and unrelated to acute infection, respectively [Citation13]. Therefore, those recuperating in community settings that did not require clinical intervention (e.g. those with mild symptoms or that were asymptomatic) and have subsequently reported long-COVID, requires further investigation. Accordingly, the current study aimed to characterize and quantify the symptom profile of long-COVID patients living in community settings and outline the impact upon QoL and activities of daily life.
2. Methods
Following institutional ethics approval (ETH2021-1452) from the Human Sciences Research Ethics Committee, an online web-based survey was developed in conjunction with patient and public representatives and hosted using an online survey platform (Qualtrics, Provo, Utah, USA). The survey was available for completion between September 2020 and May 2021 and was distributed via social media (with targeted audiences in public and private COVID-19 groups/pages). In-line with ethics standards, all participants were required to provide informed consent before completing the survey and all responses were anonymized by generating a unique participant ID.
The survey consisted of 70 questions, across 7 sections using validated measures to explore the impact of long-COVID on participant health and wellbeing. The survey included separate sections on; 1) participant characteristics (18 questions: age, body mass index [BMI], sex, comorbidities, and lifestyle factors [smoking status and weekly alcohol consumption], demographics [country of residence and ethnicity], and socioeconomic status [employment status and role, number of household occupants and situation, and approximate income]); 2) COVID-19 symptoms (10 questions), 3) QoL (Short-Form 36 [SF-36] and health-related QoL [HRQoL]) (8 questions); 4) sleep quality (8 questions, Pittsburgh Sleep Quality Index); 5) breathlessness (4 questions: Shortness-of-breath questionnaire); 6) physical activity ([PA]14 questions: SF-36); and 7) mental health (6 questions: HRQoL and SF-36). All questions were scored on Likert or frequency scales. The resulting data was reported in accordance with established and published guidelines specific for e-surveys [Citation14].
2.1. Statistical analysis
Normal distribution was assessed through a visual inspection of the frequency histograms and a Shapiro–Wilk test with all parametric assumptions satisfied. Likert scores were treated as interval data for analysis and reported as arbitrary units (AU). All survey responses were analyzed using frequency counts, Wilcoxon signed-rank tests (within groups), or Mann-Whitney U test (between groups). Data are presented as mean ± standard deviation (SD), median (with interquartile range [IQR]) and/or frequency (n/%), with statistical significance set to P < 0.05. All data were analyzed using IBM SPSS Statistics (v24, NY, USA).
3. Results
3.1. Demographics
Three hundred and eighty-one participants completed the full survey (83% female, n = 316), of which, mean age and BMI were 42 ± 12 years, and 29.1 ± 8.4 kg.m2, respectively. Eighty-one percent (n = 319) of respondents were from the UK, with a further 7% (n = 28) from Europe and 6% from the USA. The majority of respondents were employed full-time (53%, n = 198), part-time (21%, n = 80) or self-employed (10%, n = 39), with the remainder unemployed, students or retired. Those in employment were frontline workers (26%; n = 83), keyworkers (29%; n = 93), working from home (26%, n = 83), office workers (9%, n = 30) or, in high contact roles such as retail (8%, n = 25).
3.2. Healthcare utilization
Of all participants, 79.5% (n = 303) contacted their general practitioner specifically about their COVID-19, 41% (n = 155) contacted a dedicated COVID-19 telephone service (e.g. National Health Service Direct), 5% (n = 19) were referred for specialist treatment, 5% (n = 17) attended an emergency department, and 2% (n = 8) were admitted to hospital for treatment.
3.3. COVID-19 symptoms
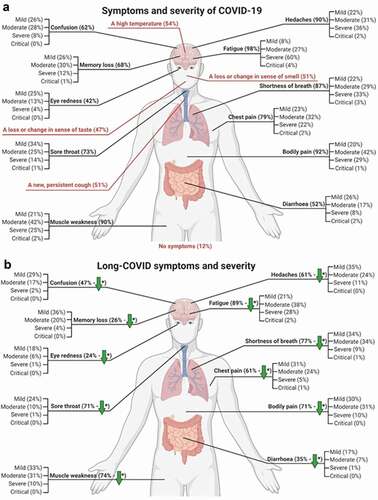
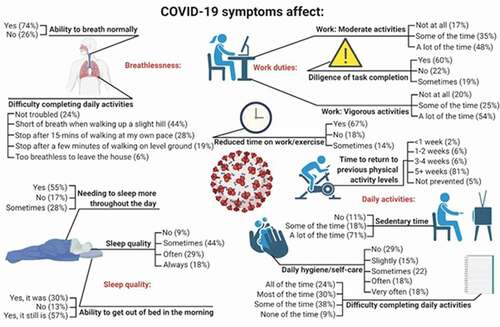
The range and frequency of COVID-19 symptoms are highlighted in their entirety in , with symptom severity reducing from the onset of symptoms to the time this survey was completed for; shortness of breath, bodily pain, muscle weakness, headaches, sore throat, diarrhea, memory loss, confusion and eye redness (P < 0.001; ). Sustained COVID-19 symptoms also affected; fatigue, breathlessness, completion of daily activities, sleep quality and moderate-to-vigorous work activities, with reported severity highlighted in . This was similar across working classifications, including frontline workers (both 91%), keyworkers (both 82%), those working from home (83% and 78%), office workers (72% and 69%), and those working in high-contact roles (82% and 68%). There was no difference in the effect of COVID-19 symptoms on moderate and vigorous activities between those individuals denoting a previous history of a long-term health condition (moderate: U = −1.7, P = 0.094, and vigorous: U = −1.8, P = 0.075).
3.4. Quality of life
As shown in , participant health was universally reduced due to COVID-19 symptoms (from 2 [Citation1,Citation2] ‘Good health’ to 4 [Citation3,Citation4] ‘Poor health’ [Z = −16.1, P < 0.001]). Medium, positive correlations were found between the number of initial symptoms and post COVID-19 general health (r = 0.56, n = 358, p < 0.001). As a result of COVID-19 infection, 27% (n = 104) of participants reported they were unable to live alone without the assistance of another person at the time of completion, 24% (n = 90) reported difficulty in completing daily activities ‘all of the time’, 31% (n = 115) reported difficulty ‘most of the time’, 39% (n = 143) reported difficulty ‘some of the time’, and 5% (n = 33) reported that their COVID-19 symptoms did not affect their ability to complete daily tasks.
Table 1. Frequency and change in symptom profile reported by patients from the onset and during recovery from a COVID-19 infection
3.5. Sleep quality
An increase in daytime sleeping was reported by eighty-three percent (n = 318) of participants as a result of COVID-19 symptoms. There was a reduction in sleep quality found in those with increased daytime sleeping (H(2) = 16.3, p < 0.001), and an increase in sleep duration after experiencing symptoms of COVID-19 (H(4) = 2.416, p < 0.001). Eighty-one percent (n = 348) of participants reported a change in sleep quality and fifty-seven percent (n = 216) reported COVID-19 related symptoms were impacting their ability to get out of bed in the morning. Lower sleep quality was positively associated with reports of poor physical health (r = 0.42, n = 358, p < 0.001) and the number of initial symptoms (r = 0.35, n = 358, p < 0.001). Forty-nine percent (n = 188) of participants also reported taking longer to fall asleep since experiencing symptoms of COVID-19, with 51% (n = 193) sleeping ‘a little less’ or ‘a lot less’ compared with pre-COVID levels.
3.6. Breathlessness
Fifty-eight percent (n = 221) of participants reported symptoms of breathlessness had made them unable to complete their typical activities of daily living compared with pre-COVID-19. Five percent (n = 19) of participants reported they were unable to leave the house due to COVID-19 related breathlessness. Thirty-two percent (n = 122) and twenty-six percent (n = 100) reported being short of breath whilst hurrying or having to stop after short periods of activity, respectively.
3.7. Physical activity
Reportedly, the time taken for participants to return to their pre-COVID PA levels ranged from: >5 weeks (81%, n = 290), 3–4 weeks (6%, n = 21), 1–2 weeks (6%, n = 22), or <1 week (2%, n = 8). However, 64% (n = 244) indicated they had still not been able to return at the time of completing the survey, whilst 5% (n = 18) were unaffected.
3.8. Mental health
Due to COVID-19 symptoms, participants felt depressed, anxious, or worried either; ‘all of the time’ (9%, n = 33), ‘most of the time’ (27%, n = 102), or ‘some of the time’ (57%, n = 216), yet 8% (n = 30) were reportedly unaffected.
4. Discussion
The current study aimed to characterize and quantify the symptom profile of long-COVID patients living in community settings, with a particular focus on characterizing the impact upon QoL and activities of daily life. A broad and debilitating symptom profile was observed, which is reflective of prolonged morbidity being reported in the months following a COVID-19 infection, and resultantly has far-reaching health, wellbeing, economical and societal impacts. Our data support existing work in this area, highlighting a range of symptoms and varying prevalence/severity [Citation7,Citation9,Citation12]. We also observed prolonged periods of morbidity and reduced engagement with daily activities, that result in increased sedentary behaviors (as a consequence of symptoms and reduced sleep quality), consequently impairing quality of life.
For those in employment (n = 328), ongoing issues were observed when performing moderate (83%) and vigorous (79%) work- (e.g. manual handling and shift work) and daily life activities (e.g. structured exercise, walking and socializing with friends and family). Moreover, the impact of COVID-19 symptomology and severity on returning to moderate-to-vigorous work activities did not disproportionally affect those with a long-term health condition(s), suggesting the negative effect of long-COVID may influence work performance/physical activities regardless of baseline health status, a finding supported by other work in this area [Citation13].
Longitudinal investigations that profile changes in symptomology and develop our understanding of the trajectories toward recovery are needed and must outline the extent to which the chronic effects of long-COVID impact population health, wellbeing and QoL. The growing burden of recovery highlights a clear need to develop efficacious interventions and multi-disciplinary support pathways [Citation15] to support COVID-19 patients living in community settings with prolonged symptom profiles and morbidity. Current estimates indicate 1 in 10 people with COVID-19 will go on to experience long-COVID symptoms [Citation9], highlighting a clear need to understand the determinants of recovery, and to inform the development of bespoke COVID-19 intervention approaches. Conservative estimates highlight ~15 million cases worldwide (as of December 2021), including a substantial number of healthcare workers [Citation16], which will continue to increase due to sustained global transmission [Citation17]. What is clear from the data here and elsewhere [Citation18,Citation19], is that the impacts which extend beyond the health and wellbeing of patients and transcend into societal and economical areas will continue for some time [Citation20] and should undoubtedly be considered an international research priority.
Whilst research into the mechanisms and recovery from COVID-19 and especially, long-COVID is ongoing, the current findings highlight an urgent need for COVID-19 specific rehabilitative strategies [Citation21] and patient support pathways to enable a return to pre-COVID QoL. Data here support previous work that has grouped symptoms to include: cardiovascular, pulmonary and respiratory symptoms, pain, fatigue, general infection symptoms, mental wellbeing, cognitive impairment, sensory impairment, and functional impairment [Citation12]. The increased understanding relating to the interaction between different symptoms (e.g. reduced functional status, physical capacity and fatigue) must be addressed with approaches that are cognizant of COVID-19ʹs underlying and not yet fully understood complexity [Citation22]. Attempts to support long-COVID patients and address the aforementioned challenges to population health will require complex design approaches to address broad patients’ needs in the context of COVID-19 and future health pandemics.
Intervention approaches to restore and promote healthy living factors, which are important in chronic illness and healthy living domains [Citation19], are historically constrained by a lack of suitability, scalability and sustainability, due in part to nominal attempts to address complex interactions and encourage cross-disciplinary collaboration [Citation23]. The legacy impacts of COVID-19 and arguably more importantly long-COVID will remain a priority for years to come, but the development of resulting approaches must address the complex and multifactorial issues reported by patients to thwart increasing pressure on local, national, and international health agencies. To be effective, resulting support pathways will undoubtedly be as complex as the symptomology, creating a novel challenge for clinical and non-clinical partners to collaborate effectively in the interest of improved patient outcomes. Adopting an intricate design approach that incorporates all key stakeholders in a whole system approach is imperative to achieve broad widespread patient and population outcomes.
5. Conclusion
The longitudinal impact to which long-COVID affects health and wellbeing is yet to be understood in its entirety, but data here highlights a broad and complex symptom profile that persists in the post-COVID period and reduces QoL. Further work to profile the intricacies of recovery is needed but long-standing morbidity should be addressed with novel COVID-19 specific rehabilitation approaches that are derived from multi-disciplinary collaborations between clinical and non-clinical organizations to restore QoL and achieve widespread population improvements in patient outcomes.
Article highlights
The longitudinal impact to which long-COVID affects health and wellbeing is yet to be understood in its entirety.
Our data highlights a broad and complex symptom profile that persists in the post-COVID period and reduces quality of life.
COVID-19 specific and multi-disciplinary rehabilitation approaches are needed to pre-COVID-19 restore pre-COVID-19 patient status.
Author contributions statement
All authors have made a significant contribution to the work reported in this manuscript. M Faghy, T. Maden-Wilkinson and A. Willmott conceived the study idea and M Faghy, T. Maden-Wilkinson, R. Arena, R. Copeland and A. Willmott developed the study design and method. R. Owen and H. Hodgkins were responsible for the acquisition of data and the resulting data analysis with the support of M. Faghy and A. Willmott.
All listed authors have contributed to the writing, revising, and reviewing the article prior to submission and agreed on all versions prior to submission and following revisions. All authors approved submission to Expert Review of Respiratory Medicine.
All authors agree to take responsibility and be accountable for the contents of the article and to share responsibility to resolve any questions raised about the accuracy or integrity of the published work.
Declaration of Interests
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Hall VJ, Foulkes S, Saei A, et al. Effectiveness of BNT162b2 mRNA vaccine against infection and COVID-19. In: Vaccine coverage in healthcare workers in England, multicentre prospective cohort study (the SIREN Study) 397(10286). SSRN Prepr; 2021;1725–1735.
- Cook TRJ, Roberts JV. Impact of vaccination by priority group on UK deaths, hospital admissions and intensive care admissions from COVID‐19. Anaesthesia. 2021;76:608–616.
- Roghani A. The influence of Covid-19 vaccine on daily cases, hospitalization, and death rate in Tennessee: a case study in the United States [Internet]. Health Policy; 2021 cited 2021 Nov 29]. Available from 2021 Nov 29: http://medrxiv.org/lookup/doi/10.1101/2021.03.16.21253767.
- Lovato A, Rossettini G, de Filippis C. Sore throat in COVID‐19: comment on “clinical characteristics of hospitalized patients with SARS‐CoV‐2 infection: a single arm meta‐analysis. J Med Virol 2021;92(7):714–715.
- Sivan M, Taylor S. NICE guideline on long covid. BMJ. 2020;4938. DOI:https://doi.org/10.1136/bmj.m4938
- NICE. COVID-19 rapid guideline: managing the long-term effects of COVID-19. 2020.
- Demeco A, Marotta N, Barletta M, et al. Rehabilitation of patients post-COVID-19 infection: a literature review. J Int Med Res. 2020;48:0300060520948382.
- O’Sullivan O. Long-term sequelae following previous coronavirus epidemics. Clin Med. 2021;21:e68–70.
- Sudre CH, Murray B, Varsavsky T, et al. Attributes and predictors of long COVID. Nat Med. 2021;27:626–631.
- Rossettini G, Conti C, Suardelli M, et al. COVID-19 and health care leaders: how could emotional intelligence be a helpful resource during a pandemic? Phys Ther. Internet]. 2021 cited 2021 Nov 29;101. Available from: https://doi.org/10.1093/ptj/pzab143
- Gorna R, MacDermott N, Rayner C, et al. Long COVID guidelines need to reflect lived experience. Lancet. 2021;397:455–457.
- Hayes LD, Ingram J, Sculthorpe NF. More than 100 persistent symptoms of SARS-CoV-2 (Long COVID): a scoping review. Front Med. 2021;8:2028.
- Tenforde MW, Kim SS, Lindsell CJ, et al. Symptom duration and risk factors for delayed return to usual health among outpatients with covid-19 in a multistate health care systems network — United States, March–June 2020. Morb Mortal Wkly Rep. 2020;69:993–998.
- Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet E-Surveys (CHERRIES). J Med Internet Res. 2004;6:e132.
- Faghy MA, Ashton RE, Maden-Wilkinson TM, et al. Integrated sports, and respiratory medicine in the aftermath of COVID-19. Lancet Respir Med. 2020;8(9):852.
- NHS sickness absence during the covid-19 pandemic | the BMJ [Internet]. cited 2021 May 13]. Available from 2021 May 13: https://www.bmj.com/content/372/bmj.n471.
- Crook H, Raza S, Nowell J, et al. Long covid—mechanisms, risk factors, and management. BMJ. 2021;374(1648). DOI:https://doi.org/10.1136/bmj.n1648.
- McKibbin W, Fernando R. The economic impact of COVID-19. Econ Time COVID-19. 2020: 45
- Arena R, Myers J, Kaminsky LA, et al. Current activities centered on healthy living and recommendations for the future: a position statement from the HL-PIVOT network. Curr Probl Cardiol. 2021;46(6):100823.
- Maani N, Abdalla SM, Galea S. Avoiding a legacy of unequal non-communicable disease burden after the COVID-19 pandemic. Lancet Diabetes Endocrinol. 2021;9:133–135.
- Faghy MA, Arena R, Stoner L, et al. The need for exercise sciences and an integrated response to COVID-19: a position statement from the international HL-PIVOT network. Prog Cardiovasc Dis. 2021;67:2–10.
- Lemhöfer C, Gutenbrunner C, Schiller J, et al. Assessment of rehabilitation needs in patients after COVID-19: development of the COVID-19-rehabilitation needs survey. J Rehabil Med. 2021;53:jrm00183.
- Reis RS, Salvo D, Ogilvie D, et al. Scaling up physical activity interventions worldwide: stepping up to larger and smarter approaches to get people moving. Lancet. 2016;388:1337–1348.