1. Introduction
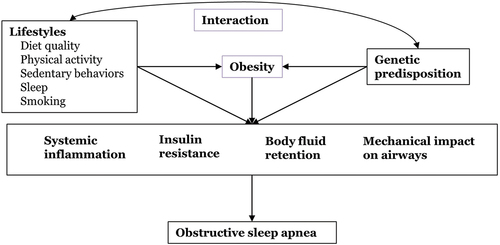
Obstructive sleep apnea (OSA) is a highly prevalent chronic sleep disorder in the adult population characterized by recurrent collapses of upper airway, intermittent hypoxia and frequent arousals during sleep, leading to impaired daytime function and increased risk of cardiovascular disease and mortality. In addition to age and sex, obesity is the strongest risk factor for OSA identified in epidemiologic studies. Obesity increases OSA risk not only through the mechanical impact on airway patency and lung function (e.g. narrowed airways due to excess pharyngeal adipose tissues and reduced lung volumes due to increased abdominal pressure from visceral fat), but also through obesity-induced downstream biochemical alterations (e.g. inflammation and insulin resistance; ). Mounting evidence suggests that OSA is manifested as a metabolic disorder, with intricate relationships with metabolic alterations such as diabetes, dyslipidemia, systemic inflammation and leptin resistance [Citation1–3]. Recent studies support a bidirectional association between OSA and diabetes independent of obesity. Chronic inflammation, a hallmark of obesity and diabetes, is associated with increased incidence of OSA after accounting for obesity and diabetes status. Insulin resistance and leptin insensitivity, which are two common pathophysiological features in individuals with metabolic syndrome, have been shown to impair neuromechanical control of upper airway muscles and may predispose individuals to the development of OSA. Taken together, these studies suggest that interventions targeting obesity and metabolic pathways are beneficial for the prevention and treatment of OSA.
Promoting healthy lifestyles (e.g. diet, exercise, sleep) has proved to be an effective strategy to combat obesity, alleviate metabolic dysregulation and improve pulmonary functions (e.g. the OSA-COPD overlap syndrome) in numerous studies. Compelling evidence reveals strong favorable effects of a healthful dietary pattern and an active lifestyle on weight change and profiles of inflammatory and metabolic biomarkers [Citation4,Citation5] (). Further, physical inactivity and sedentary behavior could cause lower-extremity edema and induce body fluid shift toward the neck during sleep, narrowing the upper airway and increasing its collapsibility [Citation6]. Although these are plausible and important pathways through which healthy lifestyles may protect against OSA, there have been limited studies on the role of heathy lifestyles in OSA.
2. Randomized controlled trials
A randomized controlled trial (RCT) of 81 patients with mild OSA found that a low-calorie diet with supervised lifestyle modification resulted in marked reduction in weight and AHI and moderately improved OSA symptoms and quality of life over 1-year follow-up, compared with routine dietary and exercise counseling [Citation7]. Continued monitoring of this RCT at the 2-year and 4-year post-intervention follow-up observed sustained favorable effects on body weight, AHI and OSA symptoms, as well as lower incidence of progression from mild to moderate OSA in the lifestyle intervention group compared with the control group. Another RCT of 34 patients with co-morbid coronary artery disease evaluated the effect of a 4-week aerobic exercise training program and reported significant decrease in AHI (particularly AHI during NREM sleep) in the exercise intervention group compared with the control group [Citation8]. The beneficial effects of exercise training on AHI were suggested to be driven by reduced nocturnal rostral fluid shift and enlarged upper airway cross-sectional area [Citation8], lowering airway collapsibility during sleep [Citation6]. Other RCTs of exercise training in OSA patients in general reported similar findings, although the magnitude of AHI decreases varied across studies ranging from a reduction of 18.2 events/hour to a reduction of 3.7 events/hour. A recent meta-analysis of 6 RCTs including 196 OSA patients provides the most updated summary of evidence that exercise intervention leads to a significant AHI decrease of 8.9 events/hour (95%: −13.4, −4.3) with moderate heterogeneity across studies (I2 = 68.6%) [Citation9]. Interestingly, multiple studies noted that these improvements were not entirely due to concurrent weight change and could be achieved without significant changes in body weight. This suggests the independent benefits of physical activity on OSA-related outcomes beyond its impact on weight loss, such as lowering inflammation, improving metabolic functions and mitigating body fluid retention. Of these 6 RCTs, four studies evaluated excessive daytime sleepiness using the Epworth Sleepiness Scale (ESS) and reported concurrent improvement in sleepiness (change in ESS: −3.1; 95% CI: −5.6, −0.6) [Citation9]. Despite consistent findings, prior studies are in general small in sample size (e.g. N < 50) with short follow-up. Future studies in larger, more diverse populations are warranted to address these limitations and investigate whether lifestyle modifications are associated with improved long-term health outcomes among patients with OSA.
3. Physical activity and sedentary behavior
Evidence, particular evidence from prospective studies, is also limited for the role of physical activity in OSA prevention. Only a few population-based studies have examined the association between physical activity and OSA. For example, in a subset of the Multi-Ethnic Study of Atherosclerosis (MESA) with objective measures of sleep-disordered breathing and physical activity, greater actigraphy-measured activity levels, as well as better neighborhood walking environment, were cross-sectionally associated with lower severity of OSA [Citation10]. Other cross-sectional studies based on self-reported physical activity reported largely consistent findings, with lower prevalence and severity of OSA observed for individuals with higher physical activity levels. Some of these cross-sectional studies are large in sample size, including one study involving over 14,000 US Hispanics/Latinos from the Hispanic Community Health Study/Study of Latinos [Citation11] and another study involving 155,448 residents of Canada [Citation12]. However, due to the cross-sectional study design, we cannot determine whether the observed associations are attributed to the compromised ability to participate in exercise as a consequence of certain hallmark OSA symptoms (e.g. sleepiness, fatigue, daytime dysfunction). Of note, two prospective studies provide further insights into the role of physical activity in OSA development [Citation13,Citation14]. In a large study of more than 137,000 men and women from three US cohorts, compared with those who participated in activities <6 metabolic equivalent task (MET)-hours/week (equivalent to two hours of walking per week at an average pace), participants whose activity levels were ≥36.0 MET-hours/week (equivalent to three hours of running per week) had a 54% lower incidence of developing clinically diagnosed OSA [Citation13]. This inverse association remains robust after accounting for BMI, waist circumference and other lifestyle factors. This study also shows that both moderate and vigorous physical activity are strongly associated with lower incidence of OSA, suggesting that maintaining an active lifestyle even by increasing daily walking could potentially prevent the development of OSA.
Sedentary behavior is another highly prevalent modern lifestyle that promotes obesity, inflammation and metabolic disorders. Prior studies have shown adverse associations of sedentary behavior with health outcomes independent of physical activity such as hypertension, diabetes and cardiovascular disease. Two cross-sectional studies and one prospective study have shown consistent positive associations between sedentary hours and OSA even after adjusting for levels of physical activity [Citation13,Citation15,Citation16]. However, all these studies are based on self-reported sedentary behavior, and future studies using objective assessment are needed to characterize patterns of sedentary behavior (e.g. sedentary time without interruption versus sedentary time with frequent breaks) and OSA risk.
4. Diet
Despite a crucial role of diet in modulating inflammation and metabolic functions, evidence on diet and OSA is scarce and limited to cross-sectional studies. In MESA, higher overall diet quality measured the Alternative Healthy Eating Index (AHEI-2010) was associated with lower OSA prevalence. When examining individual dietary components included in AHEI-2010, the results were particularly robust for the associations with intakes of whole grains and red/processed meat [Citation17]; higher intakes of whole grains (contributing to higher diet quality) were associated with lower OSA prevalence, whereas higher intakes of red/processed meat (contributing to lower diet quality) were associated with higher prevalence. Positive associations of AHI with intakes of red/unprocessed meat and refined cereal grains were reported in another small Greek cohort of OSA patients [Citation18,Citation19]. Three other cross-sectional studies reported higher OSA prevalence or severity associated with unhealthy dietary patterns such as the Western dietary pattern or the inflammatory dietary pattern [Citation20–22]. Another pilot study involving eight OSA patients assigned two weeks of personalized, combined pharmacological and behavioral therapy (including a hypocaloric diet) according to their OSA endotypes and reported significant reductions in AHI, oxygen desaturation index and ESS [Citation23]. There is currently a lack of prospective studies to elucidate the potential cyclical relationship between diet and OSA. Also, few prospective studies have examined specific dietary factors, such as alcohol drinking and coffee consumption, in relation to OSA risk. Given the direct influence of alcohol and caffeine on sleep, considering both amount and timing of consumption is required to fully understand the role of these dietary factors in OSA.
5. Sleep
Sleep is essential for regulation of metabolic homeostasis, energy balance and global rejuvenation of the immune systems. Suboptimal sleep quantity and quality have been shown to contribute to increased risk of obesity and cardiometabolic disease. However, sleep disturbances, such as poor sleep quality and short sleep duration, are generally considered as consequences of OSA that leads to arousals and sleep fragmentation. As a result, few studies have evaluated whether sleep hygiene interventions have the potential to lower the incidence and progression of OSA. Emerging evidence supports that other dimensions of sleep health that are less likely to be directly influenced by OSA, such as sleep regularity, are strongly associated with metabolic, inflammatory and cardiovascular profiles [Citation24]. This opens up a possible new research avenue for assessing the impact of behavioral sleep interventions on OSA.
6. Future directions
A number of studies have shed light on gene–lifestyle interactions that healthy lifestyles may counteract the genetic susceptibility to obesity, diabetes and cardiovascular disease, which help identify potential susceptible populations who may benefit most from lifestyle modifications. Although there is a strong genetic basis for the pathogenesis of OSA, no studies to my knowledge have examined whether adopting a healthy lifestyle could attenuate the genetic risk for OSA (). In addition to lifestyle interventions, recent investigations also start to assess whether pharmacologic interventions to improve metabolic functions have favorable associations with OSA-related outcomes. For example, intensified antidiabetic treatment to improve glycemic control among patients with diabetes and OSA over a 4-month period was shown to reduce AHI and sleep time with oxygen saturation below 90% that were not entirely due to weight loss [Citation25]. Another RCT reported that diabetes treatment using empagliflozin reduced not only adverse cardiovascular and renal outcomes but risk of new-onset OSA [Citation26]. Little is known regarding the potential interactions of these pharmacologic interventions with non-pharmacologic interventions in OSA. Future research is needed to explore whether lifestyle modifications, which have minimal side effects, could amplify these positive pharmacologic effects on OSA. Finally, there are other important lifestyle factors that are not covered in this article. For example, while smoking is linked with a wide variety of adverse health outcomes, the role of smoking in OSA remains equivocal with conflicting results from prior studies and requires more sophisticated investigations.
In summary, while additional research is needed, growing studies add to the evidence on the importance of healthy lifestyles (particularly more physical activity, less sedentary time and higher diet quality) in the prevention and treatment of OSA and comorbid conditions. Clinicians should be aware of these links and make appropriate recommendations, such as healthy eating and regular exercise, to their patients. To provide more personalized strategies in the era of precision medicine, the associations of various healthy lifestyles with OSA outcomes need to be characterized in further details, such as dose-response relationships and interactions with genetic predisposition.
Declaration of interests
The author has no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Aurora RN, Punjabi NM. Obstructive sleep apnoea and type 2 diabetes mellitus: a bidirectional association. Lancet Respir Med. 2013;1(4):329–338.
- Huang T, Lin BM, Stampfer MJ, et al. A population-based study of the bidirectional association between obstructive sleep Apnea and Type 2 diabetes in three prospective U.S. cohorts. Diabetes Care. 2018;41(10):2111–2119.
- Huang T, Goodman M, Li X, et al. C-reactive protein and risk of OSA in four US cohorts. Chest. 2021;159(6):2439–2448.
- Lee IM, Djoussé L, Sesso HD, et al. Physical activity and weight gain prevention. Jama. 2010;303(12):1173–1179.
- Huang T, Tobias DK, Hruby A, et al. An increase in dietary quality is associated with favorable plasma biomarkers of the brain-adipose axis in apparently healthy US women. J Nutr. 2016;146(5):1101–1108.
- Redolfi S, Bettinzoli M, Venturoli N, et al., Attenuation of obstructive sleep apnea and overnight rostral fluid shift by physical activity. Am J Respir Crit Care Med. 2015;191(7):856–858.
- Tuomilehto HP, Seppä JM, Partinen MM, et al., Lifestyle intervention with weight reduction: first-line treatment in mild obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179(4):320–327.
- Mendelson M, Lyons OD, Yadollahi A, et al. Effects of exercise training on sleep apnoea in patients with coronary artery disease: a randomised trial. Eur Respir J. 2016;48(1):142–150.
- Mendelson M, Bailly S, Marillier M, et al. Obstructive sleep apnea syndrome, objectively measured physical activity and exercise training interventions: a systematic review and meta-analysis. Front Neurol. 2018;9:73.
- Billings ME, Johnson DA, Simonelli G, et al. Neighborhood walking environment and activity level are associated with OSA: The Multi-Ethnic Study of Atherosclerosis. Chest. 2016;150(5):1042–1049.
- Murillo R, Reid KJ, Arredondo EM, et al. Association of self-reported physical activity with obstructive sleep apnea: results from the Hispanic Community Health Study/Study of Latinos (HCHS/SOL). Prev Med. 2016;93:183–188.
- Hall KA, Singh M, Mukherjee S, et al. Physical activity is associated with reduced prevalence of self-reported obstructive sleep apnea in a large, general population cohort study. J Clin Sleep Med. 2020;16(7):1179–1187.
- Liu Y, Yang L, Stampfer MJ, et al. Physical activity, sedentary behavior, and incidence of obstructive sleep apnea in three prospective US cohorts. Eur Respir J. 2021;59(2):2100606.
- Awad KM, Malhotra A, Barnet JH, et al. Exercise is associated with a reduced incidence of sleep-disordered breathing. Am J Med. 2012;125(5):485–490.
- Buman MP, Kline CE, Youngstedt SD, et al. Sitting and television viewing: novel risk factors for sleep disturbance and apnea risk? Results from the 2013 National Sleep Foundation Sleep in America Poll. Chest. 2015;147(3):728–734.
- Kline CE, Krafty RT, Mulukutla S, et al. Associations of sedentary time and moderate-vigorous physical activity with sleep-disordered breathing and polysomnographic sleep in community-dwelling adults. Sleep Breath. 2017;21(2):427–434.
- Reid M, Maras JE, Shea S, et al. Association between diet quality and sleep apnea in the Multi-ethnic Study of Atherosclerosis. Sleep. 2019; 42(1). DOI: https://doi.org/10.1093/sleep/zsy194.
- Kechribari I, Kontogianni MD, Georgoulis M, et al. Higher refined cereal grain intake is positively associated with apnoea-hypopnoea index in patients with obstructive sleep apnoea. J Hum Nutr Diet. 2021. DOI:https://doi.org/10.1111/jhn.12933
- Kechribari I, Kontogianni MD, Georgoulis M, et al. Associations between red meat intake and sleep parameters in patients with obstructive sleep Apnea. J Acad Nutr Diet. 2020;120(6):1042–1053.
- Gaona-Pineda EB, Martinez-Tapia B, Rodríguez-Ramírez S, et al. Dietary patterns and sleep disorders in Mexican adults from a national health and nutrition survey. J Nutr Sci. 2021;10:e34.
- Lopes TVC, Borba MES, Lopes RVC, et al. Association between inflammatory potential of the diet and sleep parameters in sleep apnea patients. Nutrition. 2019;66:5–10.
- Du Y, Duan X, Zheng M, et al. Association between eating habits and risk of obstructive sleep apnea: a Population-Based Study. Nat Sci Sleep. 2021;13:1783–1795.
- Messineo L, Magri R, Corda L, et al. Phenotyping-based treatment improves obstructive sleep apnea symptoms and severity: a pilot study. Sleep Breath. 2017;21(4):861–868.
- Huang T, Mariani S, Redline S. Sleep irregularity and risk of cardiovascular events: The Multi-Ethnic Study of Atherosclerosis. J Am Coll Cardiol. 2020;75(9):991–999.
- Gutiérrez-Carrasquilla L, López-Cano C, Sánchez E, et al. Effect of glucose improvement on nocturnal sleep breathing parameters in patients with Type 2 diabetes: The Candy Dreams Study. J Clin Med. 2020;9(4):1022.
- Neeland IJ, Eliasson B, Kasai T, et al. The impact of empagliflozin on obstructive sleep Apnea and cardiovascular and renal outcomes: an exploratory analysis of the EMPA-REG OUTCOME Trial. Diabetes Care. 2020;43(12):3007–3015.