ABSTRACT
Introduction
Although very uncommon, severe injury and death can occur during scuba diving. One of the main causes of scuba diving fatalities is pulmonary barotrauma due to significant changes in ambient pressure. Pathology of the lung parenchyma, such as cystic lesions, might increase the risk of pulmonary barotrauma.
Areas covered
Birt–Hogg–Dubé syndrome (BHD), caused by pathogenic variants in the FLCN gene, is characterized by skin fibrofolliculomas, an increased risk of renal cell carcinoma, multiple lung cysts and spontaneous pneumothorax. Given the pulmonary involvement, in some countries patients with BHD are generally recommended to avoid scuba diving, although evidence-based guidelines are lacking. We aim to provide recommendations on scuba diving for patients with BHD, based on a survey of literature on pulmonary cysts and pulmonary barotrauma in scuba diving.
Expert opinion
In our opinion, although the absolute risks are likely to be low, caution is warranted. Given the relative paucity of literature and the potential fatal outcome, patients with BHD with a strong desire for scuba diving should be informed of the potential risks in a personal assessment. If available a diving physician should be consulted, and a low radiation dose chest computed tomography (CT)-scan to assess pulmonary lesions could be considered.
1. Introduction
Over the past decades, there has been a steady and rapid growth in the number of people participating in recreational scuba diving. The number of certifications issued by Professional Association of Diving Instructors (PADI) is currently reported to be around one million annually. Although fortunately uncommon, severe injury and death can occur during scuba diving. The Divers Alert Network reports about two fatalities per 100,000 dives [Citation1]. Fatal injuries during scuba diving can be related to pulmonary barotrauma due to significant changes in ambient pressure, which can manifest in pneumomediastinum, pneumothorax, and arterial gas embolism [Citation2–5]. In a study of fatal diving accidents, arterial gas embolism was the second most common cause of death, following drowning [Citation2]. Arterial gas embolism as a manifestation of pulmonary barotrauma was reported to cause 13–24% of cases of scuba diving related deaths [Citation6]. Day-to-day changes in atmospheric pressures are usually very small. In contrast, during scuba diving significant changes in pressure occur [Citation7]. Exposure to elevated ambient pressures (hyperbaric conditions) results in changes both in gas volume (Boyle’s law) and partial pressure of the gas (Dalton’s law), which can potentially cause major problems. In recreational scuba diving, typically divers are allowed to descend to depths of 18 meters, whereas more experienced divers are permitted to maximal depths of 30–40 meters sea water (msw). For every 10 meter descent under water, the ambient pressure increases by 1 atmosphere (1 ATA = 100 kPa = 10msw). At a depth of 10 msw, the pressure has doubled while the volume of gas has halved compared to surface level. A diver using scuba apparatus will breathe normal tidal volumes at a higher gas density. When ascending to the surface from a depth of 10 msw the gas volume in the lungs will increase by 100%. It is crucial that the excess volume can be freely exhaled during ascent. To accomplish this goal, proper functioning of the lungs is essential [Citation7]. Pathology of the lung parenchym, such as cystic lesions, increases the risk of airtrapping and might therefore increase the risk of pulmonary barotrauma [Citation1,Citation3,Citation8].
Birt–Hogg–Dubé syndrome (BHD) is an autosomal dominant disorder caused by pathogenic germline variants in the FLCN gene. BHD is characterized by benign skin lesions (fibrofolliculomas) and an increased risk of renal cell carcinoma, pulmonary cystic lesions, and pneumothorax. In 87% of patients with BHD pulmonary involvement consisting of lung cysts and/or pneumothorax is reported [Citation9]. Of note, recurrent pneumothorax has also been reported in patients with BHD in the absence of detectable lung cysts [Citation9,Citation10]. We reported the outcomes of extensive clinical and genetic evaluation in two disorders partially overlapping with BHD, familial multiple discoid fibromas and familial lipomatosis associated with PRDM10 [Citation11–13]. In these families, so far, there was no clear evidence for an increased pneumothorax risk. In a recent publication, however, minimal pulmonary involvement in an additional family carrying a PRDM10 variant was observed [Citation14].
Currently, guidelines on BHD and scuba diving are lacking. No fatalities among patients with BHD during diving have been mentioned in a previous evaluation in our Dutch cohort and, to the best of our knowledge, have not been reported in literature [Citation15]. Studies in larger patient cohorts have not been performed. Despite the lack of evidence-based guidelines, scuba diving by patients with lung cysts is discouraged in the available (limited) literature, and caution in patients with BHD has therefore been recommended in the Netherlands [Citation8,Citation16–18]. The aim of this article is to provide further recommendations for patients with BHD on scuba diving based on expert opinion and a survey of literature on cysts and diving related pulmonary barotrauma.
2. Overview of literature
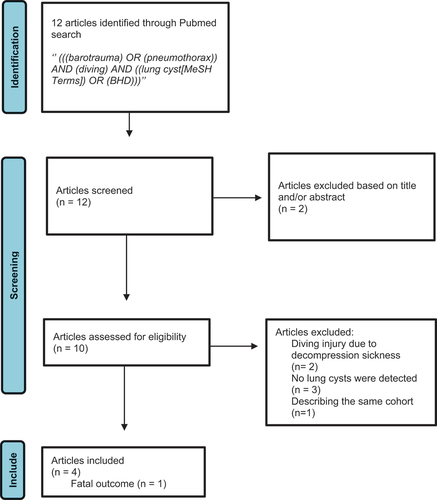
The strategy was aimed at including case reports and series about diving related barotrauma among patients with lung cysts or patients with BHD. A PubMed search with the terms (((barotrauma) OR (pneumothorax)) AND (diving) AND ((lung cyst[MeSH Terms]) OR (BHD))) was carried out on 31 May 2023, see .
Articles were included when they fulfilled the following inclusion criteria 1) articles describing pulmonary barotrauma related to scuba diving and 2) presence of lung cysts on imaging in retrospect or up to one year before the accident, or 3) patients with BHD and none of the following exclusion criteria a) articles in which pulmonary barotrauma occurred during other water sport activities, including breath-hold-diving or diving with uncontrolled ascent b) diving accidents due to decompression sickness.
3. Results
Our search resulted in a total of 12 articles; five of these articles met the above mentioned inclusion criteria. As two articles described the same cohort, one of them was excluded [Citation19,Citation20]. Three of these articles describe cases of diving-related pulmonary barotrauma, which in retrospect showed one or more pulmonary cystic lesions, and one article on diving-related pulmonary barotrauma in patients known to have BHD, see [Citation15,Citation16,Citation19–21].
Table 1. Publications included in our overview.
One of the cases on pulmonary barotrauma in the presence of pulmonary cysts, by Lippmann et al, resulted in a fatal outcome [Citation21]. This concerns a 14 years old boy without remarkable medical history where a medical assessment was performed prior to the dive. During traumacare, chest radiography revealed one lung cyst of 3 cm which may have contributed to the pulmonary barotrauma identified as cause of death. In the article by Toklu et al. three cases of pulmonary barotrauma in professional divers are described in which pulmonary lesions were detected with chest CT in retrospect [Citation16]. One of them showed an accessory azygos lobe and multiple cysts bilaterally. In the other two cases, a large bulla and small bleb were detected, respectively. Tetzlaff et al. reported 15 cases of pulmonary barotrauma in divers [Citation20]. Chest CT revealed lung cysts in 5 of the 15 cases. In two of these five patients, a follow-up chest CT showed that the lung cysts were unchanged after 6 and 15 months. Of note, 10 of these 15 cases occured during regular scuba diving with controlled ascent.
In the article by Johannesma et al., a previous evaluation of our cohort of patients with BHD, two patients (3.7%) developed a spontaneous pneumothorax within 48 hours after diving, both diving at a depth of less than 10 meters. Although these patients did not undergo lung imaging prior to the dive, it is a reasonable assumption that both pneumothoraces were related to the dive as the patients did not have sypmtoms of pneumothorax prior to the dive. For one patient this was the first pneumothorax, wheras the other patient had a history of previous pneumothorax. Around 30% of patients with BHD in this study stated that they had ever dived in the past, of whom 14.8% had dived to a depth >10 meters, all for recreational purposes [Citation15]. Two articles found through the PubMed search, where chest CT after the dive revealed a lung cyst, were excluded due to the fact that they were clearly at risk for decompression sickness with a dive profile that exceeded no-decompression dive limits [Citation22,Citation23].
4. Discussion
Literature regarding the risk of diving-related pulmonary barotrauma in patients with lung cysts is scarce, possibly due to the fact that postmortem analysis in diving fatalities is limited and challenging [Citation24]. To the best of our knowledge, no prospective studies on the predictive value of the presence of lung cysts to determine diving-associated barotrauma risks have been performed. Thus, recommendations are based on observational studies which might explain why this topic remains controversial even among experts in the field. A study including a large cohort of 2633 asymptomatic individuals aged 34–92 years, found a prevalence of lung cysts in 7.6% of participants, of whom 11.5% had multiple cysts (0.9% of all participants) [Citation25]. As no cysts were observed in individuals younger than 40 years, this study indicates that age plays an important role in the chance of having and developing lung cysts. In line with these observations, in a recent study, chest CT scans were performed in 76 young (median age 25 years) military diving candidates with no known lung pathology. An isolated pulmonary cyst was identified in one individual, and that person was subsequently deemed unfit to dive [Citation17]. Nonetheless, the high frequency of pulmonary cysts in the general population combined with the large number of scuba divers and the limited number of fatal accidents indicates that the absolute risk of fatality due to lung cysts is likely to be low. However, since pulmonary lesions have been associated with an increased risk of pulmonary barotrauma, one of the major causes of scuba diving-related fatalities, caution is in our opinion still warranted in patients with BHD until larger cohort studies are available. Based on the risks associated with lung lesions during scuba diving, it has been previously discussed to perform a chest CT as part of the medical certification of divers [Citation17], because lung cysts are usually asymptomatic and will not be detected during routine medical diving screening. However, screening of all divers by chest CT was considered to be impractical and not cost-effective and therefore suggested as an option for professional divers [Citation16,Citation17]. The British Thoracic Society (BTS)-guideline states that lung bullae or cysts increase the risk of barotrauma and are considered contraindications to diving [Citation8]. However, these guidelines were established in 2003 and have not been updated following publications on the frequency of pulmonary cysts in the general population.
Routine chest CT scans are generally not performed in patients with BHD [Citation26]. Therefore, the age of development of pulmonary cysts in BHD is not well established. However, there have been reports of pulmonary cysts and/or pneumothorax in patients with BHD before the age of 18 years, suggesting that the cysts may develop early in life, at least in a subset of patients with BHD [Citation27,Citation28]. The presence of lung cysts might increase the risk of pneumothorax. The cumulative risk of pneumothorax in patients with BHD is estimated at 25–35% [Citation29–31]. In a previous evaluation of our BHD cohort, we estimated a pneumothorax risk of 0.33% per diving episode. Of note, this number was derived from a relatively small cohort of patients with the majority of dives being <10 meters in depth.
The BTS-guidelines state that a history of primary spontaneous pneumothorax (PSP) is a contraindication for diving, unless treated with bilateral pleurectomy and normal chest CT and lung function [Citation8]. The Dutch society of pulmonologists (NVALT) published a position paper also stating that a history of PSP is a contraindication for diving [Citation32]. Currently, there is no international consensus on this point, probably due to pleural adhesions after pleurectomy, which are associated with a higher risk for pulmonary barotrauma [Citation33]. Prior surgical treatment for pneumothorax may not be sufficient for the decision regarding fitness to dive. Even though it will reduce the risk of a recurrent pneumothorax, it may not protect against the risk for diving-related pulmonary barotrauma, including arterial air embolism [Citation34]. Their advice is to avoid diving with a history of PSP, even after pleurectomy or pleurodesis, until more is known about the effect of hyperbaric conditions and the risks of recurrence of pneumothorax under these conditions
In our opinion, according to the BST and NVALT guidelines, scuba diving should be discouraged, even after pleurectomy or pleurodesis, for patients with BHD with a history of pneumothorax. As long as there is no international consensus on this point, we advise patients with BHD to check the current advices in their own country. In addition, this may also be relevant in obtaining a diving insurance, which can also differ per country. In our opinion, also in patients with BHD without a prior history of pneumothorax caution is warranted. If a strong desire for scuba diving persists, patients should be informed about the risks, which should be addressed during genetic counseling. We suggest individualized assessment of risk following consultation with a pulmonologist, specialized in scuba diving if available. A low dose radiation chest CT may be considered to evaluate the presence of lung cysts in order to aid the individualized risk assessment [Citation35]. If lung cysts are detected we would advise against scuba diving until further data is available. Although the absolute risk is likely to be very small, given the number of people diving and the presence of lung cysts in asymptomatic individuals, the risk of pulmonary barotrauma is likely to be increased in the presence of cysts and may result in a potential fatal outcome. In addition, it is very well possible that the presence of lung cysts in fatal diving accidents is underestimated due to the small number of autopsies performed. Given the known occurrence of radiologically inapparent microscopic cysts in patients with BHD and the possibility of cysts developing over time, even patients without identifiable lung cysts or a history of pneumothorax should be warned about the potential higher risk of pulmonary complications compared with the general population [Citation10,Citation36–39]. However, even in the presence of cysts individual risk is likely to be influenced by individual and external factors making individual risk prediction challenging. Additionally, the implications for obtaining insurance may vary from country to country and are likely to influence recommendations. Recommendations on BHD and scuba diving may remain different between countries until guidelines have been established.
Recommendations regarding diving might also be relevant for family members of patients with BHD. For instance, it is generally suggested that genetic testing for children of patients with BHD is deferred until adulthood (around age 20), to allow the children to make individual decisions and start renal surveillance at that age if the familial variant in FLCN is detected. However, children of a patient with BHD could consider earlier testing in case they have a strong desire for scuba diving during adolescence.
It is very likely that BHD, with a previously estimated prevalence of around 1:200.000 is currently underdiagnosed [Citation40]. In the Netherlands over 450 patients have been diagnosed in a population of 17,5 million, which underlines underdiagnosis [Citation41]. A recent population-based study reported a prevalence of pathogenic FLCN variants in 1:3234 unrelated individuals, of whom 68.6% had a BHD-related phenotype [Citation42]. An apparent PSP can be the first manifestation of BHD [Citation43]. In the Netherlands, a chest CT is not performed as part of standard care in patients with a PSP [Citation44]. Thus, BHD may not be recognized and the presence of lung cysts will not be detected during regular medical diving screening. Therefore, it is very important that features that could indicate BHD (including the skin lesions, pneumothorax and/or renal cell carcinoma) are recognized, especially in patients with a desire for scuba diving [Citation43,Citation45].
5. Conclusions
The presence of pulmonary cysts might increase the risk of pulmonary barotrauma. Pulmonary cysts are present in the majority (>80%) of patients with BHD and predispose these patients to the risk of recurrent pneumothoraces. Current guidelines consider the presence of pulmonary cysts or prior history of pneumothorax as contraindications for scuba diving [Citation8]. Although the overall risk associated with scuba diving is likely to be low, the relative paucity of literature and the potential for serious outcomes, including fatality, warrants caution. Therefore, we suggest that all patients with BHD should be educated about the potential risks associated with scuba diving. Those with a strong desire for scuba diving without a history of pneumothorax or known presence of pulmonary cysts should be referred to a pulmonologist for a personal risk assessment, preferably including low dose chest CT to evaluate the presence and quantification of pulmonary cysts.
6. Expert opinion
Given the pulmonary involvement, BHD patients might be at increased risk of pulmonary barotrauma. However, currently, guidelines on BHD and scuba diving are lacking. Advice regarding scuba diving is regularly requested by BHD patients in our center of expertise in the Netherlands, and might be relevant to many individuals and physicians.
Literature regarding the risk of diving-related pulmonary barotrauma in patients with lung cysts is scarce, possibly due to the fact that postmortem analysis in diving fatalities is limited and challenging. Thus, recommendations are based on observational studies which might explain why this topic remains controversial even among experts in the field.
This review provides an overview of the limited literature on this topic, including advice regarding scuba diving for patients with BHD. In our opinion, although the absolute risks are likely to be low, caution is warranted. Hopefully, this overview will facilitate establishment of future evidence based guidelines for patients with BHD with a desire for scuba diving.
Based on recent indications that BHD is likely to have a much higher prevalence than estimated to date, we expect that knowledge of and awareness for BHD will rapidly increase in the years to come. Considering the fact that the number of scuba divers is still rapidly increasing as well, we expect this topic to become more and more relevant.
Article highlights
BHD is characterized by skin fibrofolliculomas, an increased risk of renal cell carcinoma, multiple lung cysts and spontaneous pneumothorax.
Pre-existing pathology of the lung parenchyma, such as cystic lesions, might increase the risk of pulmonary barotrauma.
Currently evidence based guidelines on BHD and scuba diving are lacking, however given the pulmonary involvement, in some countries patients with BHD are generally recommended to avoid scuba diving,
In our opinion, although the absolute risks are likely to be low, caution is warranted if BHD patients have a desire to go scuba diving.
Patients with BHD should be informed about the potential (fatal) risks and associated insurance consequences which may vary between countries.
Declaration of interest
The authors have no relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript. This includes employment, consultancies, honoraria, stock ownership or options, expert testimony, grants or patents received or pending, or royalties.
Reviewer disclosures
Peer reviewers on this manuscript have no relevant financial or other relationships to disclose.
Additional information
Funding
References
- Penrice D, Cooper JS. Diving Casualties. In: StatPearls. Treasure Island (FL): StatPearls; 2022 Nov 28.
- Casadesus JM, Aguirre F, Carrera A, et al. Diving-related fatalities: multidisciplinary, experience-based investigation. Forensic Sci Med Pathol. 2019;15(2):224–232. doi: 10.1007/s12024-019-00109-2
- Ioannidis G, Lazaridis G, Baka S, et al. Barotrauma and pneumothorax. J Thorac Dis. 2015;7(Suppl 1):S38–43. doi: 10.3978/j.issn.2072-1439.2015.01.31
- Vann RD, Butler FK, Mitchell SJ, et al. Decompression illness. Lancet. 2011;377(9760):153–164. doi: 10.1016/S0140-6736(10)61085-9
- Mitchell SJ, Bennett MH, Moon RE, et al. Decompression sickness and arterial gas embolism. N Engl J Med. 2022;386(13):1254–1264. doi: 10.1056/NEJMra2116554
- Casadesus JM, Nieto-Moragas J, Serrando MT, et al. Pulmonary barotrauma in SCUBA diving-related fatalities: a histological and histomorphometric analysis. Forensic Sci Med Pathol. 2023. doi:10.1007/s12024-022-00567-1.
- Tetzlaff K, Thorsen E. Breathing at depth: physiologic and clinical aspects of diving while breathing compressed gas. Clin Chest Med. 2005;26(3):355–380. doi: 10.1016/j.ccm.2005.05.001v
- British Thoracic Society Fitness to Dive Group SotBTSSoCC. British Thoracic Society guidelines on respiratory aspects of fitness for diving. Thorax. 2003;58(1):3–13. doi: 10.1136/thorax.58.1.3
- Bruinsma FJ, Dowty JG, Win AK, et al. Update of penetrance estimates in Birt-Hogg-Dubé syndrome. J Med Genet. 2023;60(4):317–326. doi: 10.1136/jmg-2022-109104
- Onuki T, Goto Y, Kuramochi M, et al. Radiologically indeterminate pulmonary cysts in Birt-Hogg-dube syndrome. Ann Thorac Surg. 2014;97(2):682–685. doi: 10.1016/j.athoracsur.2013.05.120
- van de Beek I, Glykofridis IE, Oosterwijk JC, et al. PRDM10 directs FLCN expression in a novel disorder overlapping with Birt–Hogg–Dubé syndrome and familial lipomatosis. Hum Mol Genet. 2022;32(7):1223–1235. doi: 10.1093/hmg/ddac288
- van de Beek I, Glykofridis IE, Tanck MWT, et al. Familial multiple discoid fibromas is linked to a locus on chromosome 5 including the FNIP1 gene. J Hum Genet. 2023;68(4):273–279. doi: 10.1038/s10038-022-01113-1
- Starink TM, Houweling AC, van Doorn MB, et al. Familial multiple discoid fibromas: a look-alike of Birt-Hogg-dube syndrome not linked to the FLCN locus. J Am Acad Dermatol. 2012;66(2):259 e1–9. doi: 10.1016/j.jaad.2010.11.039
- Schmidt LS, Vocke CD, Ricketts CJ, et al. PRDM10 RCC: a Birt-Hogg-Dubé-like syndrome associated with lipoma and highly penetrant, aggressive renal tumors morphologically resembling type 2 papillary renal cell carcinoma. Urology. 2023;179:58–70. doi: 10.1016/j.urology.2023.04.035
- Johannesma PC, van de Beek I, van der Wel JW, et al. Risk of spontaneous pneumothorax due to air travel and diving in patients with Birt-Hogg-dube syndrome. Springerplus. 2016;5(1):1506. doi: 10.1186/s40064-016-3009-4
- Toklu AS, Kiyan E, Aktas S, et al. Should computed chest tomography be recommended in the medical certification of professional divers? A report of three cases with pulmonary air cysts. Occup Environ Med. 2003;60(8):606–608. doi: 10.1136/oem.60.8.606
- Bonnemaison B, Castagna O, de Maistre S, et al. Chest CT scan for the screening of air anomalies at risk of pulmonary barotrauma for the initial medical assessment of fitness to dive in a military population. Front Physiol. 2022;13:1005698. doi: 10.3389/fphys.2022.1005698
- Gupta N, Sunwoo BY, Kotloff RM. Birt-Hogg-dube syndrome. Clin Chest Med. 2016;37(3):475–486. doi: 10.1016/j.ccm.2016.04.010
- Reuter M, Tetzlaff K, Warninghoff V, et al. Computed tomography of the chest in diving-related pulmonary barotrauma. Br J Radiol. 1997;70(833):440–445. doi: 10.1259/bjr.70.833.9227223
- Tetzlaff K, Reuter M, Leplow B, et al. Risk factors for pulmonary barotrauma in divers. Chest. 1997;112(3):654–659. doi: 10.1378/chest.112.3.654
- Lippmann J, Fock A, Arulanandam S. Cerebral arterial gas embolism with delayed treatment and a fatal outcome in a 14-year-old diver. Diving Hyperb Med. 2011;41(1):31–34.
- Norton MN, Weaver LK. Decompression sickness with incidental pulmonary cyst. Undersea Hyperb Med. 2022;49(3):289–293. doi: 10.22462/05.06.2022.2
- Padilla W, Newton HB, Barbosa S. Weber’s syndrome and sixth nerve palsy secondary to decompression illness: a case report. Undersea Hyperb Med. 2005;32(2):95–101.
- Edmonds C, Caruso J. Recent modifications to the investigation of diving related deaths. Forensic Sci Med Pathol. 2014;10(1):83–90. doi: 10.1007/s12024-013-9491-x
- Araki T, Nishino M, Gao W, et al. Pulmonary cysts identified on chest CT: are they part of aging change or of clinical significance? Thorax. 2015;70(12):1156–1162. doi: 10.1136/thoraxjnl-2015-207653
- Menko FH, van Steensel MA, Giraud S, et al. Birt-Hogg-Dube syndrome: diagnosis and management. Lancet Oncol. 2009;10(12):1199–1206. doi: 10.1016/S1470-2045(09)70188-3
- Geilswijk M, Bendstrup E, Madsen MG, et al. Childhood pneumothorax in Birt-Hogg-dube syndrome: a cohort study and review of the literature. Mol Genet Genomic Med. 2018;6(3):332–338. doi: 10.1002/mgg3.373
- Ardolino L, Silverstone E, Varjavandi V, et al. Birt-Hogg-dube syndrome presenting with macroscopic pulmonary cyst formation in a 15-year-old. Respirol Case Rep. 2020;8(6):e00610. doi: 10.1002/rcr2.610
- Houweling AC, Gijezen LM, Jonker MA, et al. Renal cancer and pneumothorax risk in Birt-Hogg-dube syndrome; an analysis of 115 FLCN mutation carriers from 35 BHD families. Br J Cancer. 2011;105(12):1912–1919. doi: 10.1038/bjc.2011.463
- Toro JR, Pautler SE, Stewart L, et al. Lung cysts, spontaneous pneumothorax, and genetic associations in 89 families with Birt-Hogg-dube syndrome. Am J Respir Crit Care Med. 2007;175(10):1044–1053. doi: 10.1164/rccm.200610-1483OC
- Gupta N, Seyama K, McCormack FX. Pulmonary manifestations of Birt-Hogg-dube syndrome. Fam Cancer. 2013;12(3):387–396. doi: 10.1007/s10689-013-9660-9
- (NVALT) NVvAvLeT. Position paper: Ademhaling onder bijzondere omstandigheden – duiken, vliegen en hoogte. 2021.
- Calder IM. Autopsy and experimental observations on factors leading to barotrauma in man. Undersea Biomed Res. 1985;12(2):165–182.
- Villela MA, Dunworth S, Harlan NP, et al. Can my patient dive after a first episode of primary spontaneous pneumothorax? A systematic review of the literature. Undersea Hyperb Med. 2018;45(2):199–208. doi: 10.22462/03.04.2018.7
- Johannesma PC, van den Borne BE, Gille JJ, et al. Spontaneous pneumothorax as indicator for Birt-Hogg-Dubé syndrome in paediatric patients. BMC Pediatr. 2014;14(1):171. doi: 10.1186/1471-2431-14-171
- Tobino K, Gunji Y, Kurihara M, et al. Characteristics of pulmonary cysts in Birt-Hogg-dube syndrome: thin-section CT findings of the chest in 12 patients. Eur J Radiol. 2011;77(3):403–409. doi: 10.1016/j.ejrad.2009.09.004
- Johannesma PC, Houweling AC, van Waesberghe JH, et al. The pathogenesis of pneumothorax in Birt-Hogg-dube syndrome: a hypothesis. Respirology. 2014;19(8):1248–1250. doi: 10.1111/resp.12405
- Ayo DS, Aughenbaugh GL, Yi ES, et al. Cystic lung disease in Birt-Hogg-dube syndrome. Chest. 2007;132(2):679–684. doi: 10.1378/chest.07-0042
- Cho SM, Chae EJ, Choe J, et al. Progression of pulmonary cysts in Birt-Hogg-dube syndrome: longitudinal thoracic computed tomography study with quantitative assessment. BMC Pulm Med. 2023;23(1):181. doi: 10.1186/s12890-023-02483-8
- Lertsburapa T, Yang X, eds. Orphanet. Syndroom van Birt-Hogg-Dubé; 2008 [cited 2023 Jan 6].Available from: https://www.orpha.net/consor/cgi-bin/OC_Exp.php?Expert=122&lng=NL
- van Riel L, Jansen PR, Boerrigter BG, et al.Correspondence on “frequency of truncating FLCN variants and Birt-Hogg-dube-associated phenotypes in a health care system population” by Savatt. Genet Med. 2023;25(1):158–160. doi: 10.1016/j.gim.2022.08.033
- Savatt JM, Shimelis H, Moreno-De-Luca A, et al. Frequency of truncating FLCN variants and Birt-Hogg-dube-associated phenotypes in a health care system population. Genet Med. 2022;24(9):1857–1866. doi: 10.1016/j.gim.2022.05.006
- Sriram JD, van de Beek I, Johannesma PC, et al. Birt-Hogg-dube syndrome in apparent primary spontaneous pneumothorax patients; results and recommendations for clinical practice. BMC Pulm Med. 2022;22(1): doi: 10.1186/s12890-022-02107-7
- Primaire spontane pneumothorax [Internet]. Federatie Medisch Specialisten. 2022. Available from: https://richtlijnendatabase.nl/richtlijn/primaire_spontane_pneumothorax/startpagina_-_primaire_spontane_pneumothorax.html.
- Johannesma PC, Houweling AC, Menko FH, et al. Are lung cysts in renal cell cancer (RCC) patients an indication for FLCN mutation analysis? Fam Cancer. 2016;15(2):297–300. doi: 10.1007/s10689-015-9853-5