ABSTRACT
Purpose
To examine stroke inpatients’ real-life wayfinding behaviour and how the built environment of rehabilitation clinics might influence their behaviour and experiences.
Methods
Stroke inpatients in seven rehabilitation clinics were observed (n = 70), each over the course of 12 consecutive hours. Their paths through the clinic and the locations of encountered wayfinding-related events were mapped on the floor plans and described in the written notes. The observations were supplemented by a survey asking patients about their wayfinding experiences.
Results
For a third of observed patients, at least one wayfinding-related event was observed on the observation day, and 50% of patients reported getting lost in their clinic at least once. Most wayfinding-related events occurred between patient rooms and therapy rooms, and patients frequently relied on backtracking or the help of the staff to find their way. Clinics’ layout organization was found to play a role in the wayfinding behaviour of patients.
Conclusions
Wayfinding is a common challenge that stroke inpatients encounter in rehabilitation clinics. Avoiding multiple decision nodes on the paths between patient rooms and therapy rooms and creating distinct identities for corridor segments in the decision nodes and the areas in front of elevators would likely improve wayfinding performance.
Introduction
Disabilities and impairments following a stroke are unique and complex (Adamson et al., Citation2004). Aside from the common motor disability (Langhorne et al., Citation2009), stroke patients can have additional impairments that influence how they perceive and interact with their environment. Mild cognitive impairment and vascular dementia are two examples (Sun et al., Citation2014). Other impairments can be in the form of decreased vision or eye movement, visual field abnormalities, visual perceptual difficulties (Rowe et al., Citation2009), or sensory deficits (Carey, Matyas & Oke, 1993). Many stroke patients experience visuospatial deficits such as unilateral neglect (lack of awareness on one side of the body) and topographic disorientation (lack of configurational understanding of the surroundings; Robertson & Halligan, Citation1998). As a result, stroke patients typically struggle with spatial awareness and navigation, limiting their ability to find their way (Feigin et al., Citation2017). Around a quarter of stroke survivors maintain navigation impairment 12 months after the acute phase, negatively affecting their quality of life (Hamre et al., Citation2020).
Wayfinding ability is essential for everyday independence and not relying on others for assistance (Van Der Ham et al., Citation2013). Due to the complex spatial configurations of healthcare facilities, wayfinding might be more challenging for patients, who are usually under stress and experiencing various medical symptoms (Baskaya et al., Citation2004). This is especially the case for stroke patients recovering in rehabilitation clinics. Patients need to quickly adapt to new post-stroke impairments and, in some circumstances, to the use of mobility aids (e.g., a wheelchair or a walker) in an unfamiliar setting. Their inpatient stay is usually several weeks long (Nikolaus et al., Citation2006) but could extend to several months. Patients have to attend therapies multiple times per day and have meals in the clinic’s main dining room or a smaller dining room on their ward, with their daily covered distance sometimes exceeding 2 km (Kevdzija & Marquardt, Citation2022). Due to the challenging environment and daily schedule, wayfinding issues are frequent in stroke patients recovering in rehabilitation clinics (Kevdzija & Marquardt, Citation2018).
Clear wayfinding in a rehabilitation clinic is vital for reducing patients’ stress and improving their mobility and overall independence. Patients’ wayfinding issues can also present a burden on staff resources and performance (Peponis, Zimring, & Choi, Citation1990). Patients being late for their appointments due to wayfinding problems can cause delays and disruptions in therapy schedules and staffing (Cooper, Citation2010). Getting lost might also be dangerous, especially for patients with higher levels of physical, cognitive, and visual impairments, who have an increased risk of falls (Rabadi et al., Citation2008). At the same time, stroke patients undergoing recovery in rehabilitation clinics are preparing to return home, and training their wayfinding ability is essential for their everyday life (Delgrange et al., Citation2020). In addition to virtual reality navigation training that is increasingly being used in the treatment of stroke patients (Claessen, van der Ham et al., Citation2016; Kaplan et al., Citation2021; Morganti et al., Citation2019), finding their way independently in the real-life physical environment of rehabilitation clinics could potentially serve as a training ground for preparing patients for their return home. In contrast to virtual environments, which primarily provide visual information and are associated with the absence of locomotion, the approach of requiring patients to go to therapies on their own could provide an opportunity for training navigation that integrates visual and physical information (Claessen, Visser-Meily et al., Citation2016). However, this has not been thoroughly investigated so far.
When looking at the research focusing on wayfinding outside of the healthcare facility context, the influence of spatial configuration and architectural design on navigation ability was recognized already in early studies. Floor plans and environmental cues (e.g., landmarks, signage) overlaid on those floor plans are essential components in the wayfinding process (Baskaya et al., Citation2004). Initial research revealed a link between the main building path network features, such as decision points, distances, direction changes within a floor plan, and navigation difficulty (Best, Citation1970). The subsequent studies suggested that the primary influence on wayfinding performance was the complexity of floor plan configurations (Hillier et al., Citation1984; O’Neill, 1991a; Peponis et al., Citation1990, Haq & Zimring, Citation2003; O’Neill, 1991b). In further research, healthcare buildings were identified as one of the most complex environments for wayfinding, where similarities between corridors might cause confusion and frustration to people attempting to navigate them (Wright et al., Citation1993). They are large and unfamiliar environments in which wayfinding strategies are frequently not included in the architectural planning process, and wayfinding systems are often an afterthought and overlay (Devlin, Citation2014). Furthermore, signage with textual and symbolic wayfinding information might not be universally understood (Iftikhar et al., Citation2021), especially by people with diverse needs and abilities (Morag et al., Citation2016).
According to these findings, it can be hypothesized that the healthcare facilities’ frequently complex spatial configurations may influence stroke patients’ wayfinding performance during an inpatient stay. Still, the aspects of the built environment that contribute to the wayfinding ability of stroke patients are not yet understood. There is a lack of knowledge on how stroke patients find their way during their inpatient stay in rehabilitation clinics and what their real-life wayfinding experiences are. A variety of stroke-related impairments and multiple cognitive functions involved in wayfinding make it a challenging topic to investigate (Asselen et al., Citation2006). Furthermore, the researchers’ limited access to healthcare facilities, differences in the design of each facility and other logistical issues make rigorous research studies and comparisons difficult (Ulrich et al., Citation2008, Kalantari & Snell, Citation2017). These challenges are likely behind the lack of empirical studies investigating the relationship between stroke patient wayfinding and the built environment and why many research studies turned to virtual reality as the tool to investigate wayfinding in healthcare facilities.
This study aims to provide insights into stroke patients’ real-life wayfinding behaviour in rehabilitation clinics, the daily challenges they encounter and how the built environment might affect their wayfinding. These findings are a part of larger research investigating barriers and facilitators that stroke patients experience in the built environment of rehabilitation clinics.
Materials and methods
Patient shadowing, accompanied by a patient survey, was used to investigate stroke inpatients’ wayfinding behaviour and experiences. Shadowing is a method where a researcher closely observes and records the actions and behaviour of a single individual during their everyday activities (McDonald, Citation2005). A single researcher (the author) shadowed ten patients in seven different clinics (n = 70), each for 12 consecutive hours on an ordinary rehabilitation day (from 07:00 h to 19:00 h). Shadowing took place in all spaces accessible to patients except their rooms and therapy rooms. While the observed patient was in therapy, the researcher used this time for breaks or to check the shadowing notes taken so far. The researcher had meals at the same time as the observed patient. Patients’ paths throughout the clinics and the areas where they encountered an event related to wayfinding were recorded and described using paper floor plans and time log sheets. For the purpose of patient shadowing, a wayfinding-related event was defined as “the difficulty with finding the right way, mistaking the corridor or the floor, or asking for directions.” The events when patients were visiting certain scheduled areas (e.g., a particular therapy room) for the first time or only searching for the room number in the right corridor segment were not included as wayfinding-related events in this study. The focus of observations was on wayfinding behaviour in the familiar environment and the influence of the building’s layout. When able (due to post-stroke impairments) and willing to complete it, the observed patients also filled in a survey (n = 60). Patients were asked whether they ever got lost in their clinic and, if answered affirmatively, where this happened. They were also asked if they experienced any barriers in the built environment of the rehabilitation clinic.
Settings
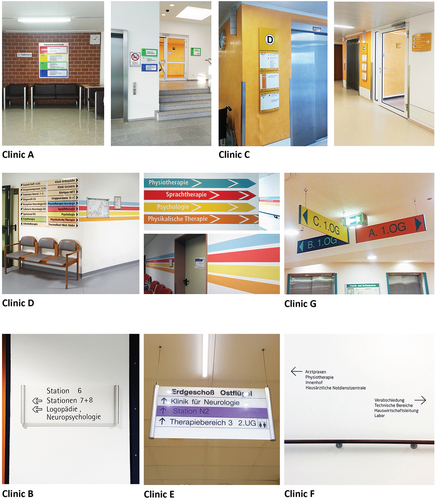
Patient shadowing took place in seven rehabilitation clinics in Germany. The participating clinics had different spatial configurations () and were comparable in size and number of beds. These clinics were dedicated post-acute rehabilitation facilities. Patients were not limited to the environment of their ward; they were expected to independently go to therapy rooms, dining rooms, and other common or diagnostics spaces often placed in different building areas and on various floors.
Table I. Characteristics of the participating clinics
Participants
Seventy stroke patients undergoing recovery as inpatients in rehabilitation clinics participated in the study (). Using the given inclusion and exclusion criteria, the medical staff selected ten participants in each clinic. Inclusion criteria were that: (1) the potential participants were in rehabilitation after a stroke, (2) they were independently mobile in the clinics (with or without the use of mobility aids, such as a wheelchair or a walker), and (3) they gave their written or verbal consent for participating in the study. The study excluded patients suffering from dementia, severe communication and cognitive impairments, severe multi-morbidity (somatic, psychiatric, or psycho/geriatric), significant mobility impairment before the stroke, and orthopaedic, neurological, or other conditions of consequence for the study.
Table II. Patient participants’ characteristics
Procedure
In the first step, the medical staff of the clinic identified possible study participants. A familiar staff member approached the patient and informed them about the research study. Patients were then asked if they wanted to participate. In the case that the patient expressed an interest in participating, they were given a large-print information sheet and a consent form. Once this was done and the patient accepted to participate, the shadowing day was scheduled. Patients were also given a large-print survey on the observation day to complete during the researcher’s stay in their clinic.
Data processing and analysis
The first step in data analysis was to digitalize the shadowing data recorded on the floor plans. In the next step, each patient’s path (from point A to point B) was analysed to determine whether a wayfinding-related event occurred on it, what exactly happened and where, and how the patient found the right way. Furthermore, each path was examined for its characteristics regarding the number of choice nodes (Peponis et al., Citation1990), level changes, and the angle between the possible corridor choices. The open-ended survey responses were translated from the German language and coded using NVivo11 software.
The presented results combine a narrative description of observed patients’ behaviours related to wayfinding (and their survey responses) with reporting the frequency and characteristics of the wayfinding-related events. Each patient was assigned a code name (a letter and a number). The letter relates to the clinic where the patient was observed (A to G), and the number represents patient’s number in the order of observations (1 to 10).
Results
Frequency of wayfinding-related events
On the day of the observation, about a third of patients in each mobility level group experienced a wayfinding-related event (). The occurrence of these events was not specific to a single patient group, they were observed in all groups regardless of patients’ mobility level. One or more wayfinding-related events were observed in 24 out of 70 participating patients (10 female and 14 male). There were 42 occasions when a wayfinding-related event was observed among these 24 patients. Out of those 42 events, 35 happened in corridors of the clinics. The other seven happened when the patient had mistaken a floor when going out of the elevator.
Table III. Number and percentage of wayfinding-related events observed for each mobility level (n = 70)
In their survey responses, 29 patients reported never getting lost in their clinic, 14 got lost once, and 15 got lost more than once. Hence, half of the patients that answered this question reported getting lost in their clinic at least on one occasion. Furthermore, some patients might have been reluctant to report getting lost in the clinic since there was a discrepancy between shadowing data and their survey responses. Six out of 29 patients who reported never getting lost in the clinic encountered at least one wayfinding-related event on the day when they were shadowed.
Locations and overcoming strategies
Wayfinding-related events most commonly happened on the patient’s way to therapy or going back from the therapy area to their room (88,1% of all observed events). Patients relied on backtracking (22 events) and asking for directions (13 events) to find their way in most cases (). The common situations when patients encountered a wayfinding-related event were making a wrong turn in the corridor (18 events) and stopping and looking around (12 events). In one example, the patient had trouble finding his way due to a tall mirror used for treatments that was hung on the wall. The patient started walking towards the mirror before realizing that the corridor had ended and that he was heading in the wrong direction.
Table IV. Characteristics of the observed events of wayfinding-related events (n = 42)
Spatial configurations
The lowest number of wayfinding-related events was observed in clinics B and G (3 and 2 respectively), with patients in clinic E encountering the most wayfinding-related events (11 observed events), followed by clinic A (7 events), clinic F (7 events), clinic C (6 events) and clinic D (6 events). This difference is most likely driven by differences in the spatial configuration complexity of clinics.
Clinics B and G have a central vertical core with wards organized radially around it. Even though the spatial configuration is simple, patients make errors when exiting the elevator since all floors are arranged in the same way. One patient of Clinic B “left the elevator on the wrong level” (B2), and another reported: “I wanted to go back to my room and went to the wrong ward.” A patient of clinic G “confused basement and ground floor” (G4) and another patient from the same clinic “mixed up floors, mixed up wards” (G7).
On the other hand, Clinic E was modified from a tuberculosis sanatorium and had a more complex spatial configuration, with a central intensive station, long patient wards, and a separate building for mobile patients. Therapies are spread throughout the clinic, and several therapy rooms are also placed on the basement level. One patient reports getting lost “[…] on the way to the gym. I then asked the staff. On the way out of the elevator, signage is very confusing” (E9). Another patient also encountered a wayfinding-related event “in the basement when going to the entrance hall” (E7). The third patient reported getting lost in the clinic “only at the beginning, in my first week” (E4).
Clinic A, similarly, has a complex spatial configuration with separate buildings since it was adapted from a different function (centre for brain-injured soldiers after WWII) and has grown over time. These separate buildings are connected on the basement level, which most patients have to use to reach therapies. Patients find this environment challenging for wayfinding, reporting getting lost “in the basement” (A8) and “finding therapy rooms” (A6). Another patient reported getting lost “in the basement, I approached someone and asked for directions” (A1). A third patient reported: “I got lost once in the basement; a physician had helped me to find my destination. I got lost two times on the first floor. A nurse helped me to find the right way” (A9). One patient also offered advice for providing “better wayfinding” in the clinic’s architecture by “adapting to dependent patients and considering their needs” (A4).
Surprisingly, clinic F was also where a high number of wayfinding-related events were observed. This clinic was opened in 2014, and it is the newest of the participating clinics. Patients of Clinic F describe it as challenging for wayfinding, reporting that “it is difficult to find your way, I always have to look left and right” (F2) and that “everything looks the same” (F4). “Corridors are all the same; I often don’t know in which corridor I am. Visitors also get lost. Maybe colour or signs would help.” (F8). Since this clinic has a remarkably compact and symmetric layout with three courtyards, this distinct symmetry might have contributed to challenging wayfinding. Furthermore, the patients often did not notice the minimalistic signage design adopted in this clinic (thin black letters on white walls, ).
Clinic C has an elongated floor plan with connected wards, and all the floors are not the same. As a result, the elevators do not connect all the building parts. Having to take different elevators to reach different building sections on the same level created a wayfinding challenge for patients of this clinic. One patient reports: ’Elevator stopped on the wrong floor. I ended up on the 2nd floor.’ (C4), and another patient got lost in the clinic “mostly when using the elevator” (C1). An additional patient got lost on the way to therapy, which required using a different elevator to the one closest to the patient’s ward (C6).
Even though Clinic D has a simple two-wing floor plan on the upper floors, the basement floor is the location of all therapy rooms, and it is shared with the nearby orthopaedic clinic. Two wayfinding-related events were observed on the upper floors when a patient had mistaken the floor upon exiting the elevator. The rest of the observed cases occurred in the basement. One patient reported getting lost “when changing from one to the other clinic area” (D4), which was on the building’s basement level, and another “in the basement, then someone from the ward came to help” (D3). A third patient from this clinic “walked in the wrong direction, down the corridor, instead of to the nearby elevator” (D5). Another patient shared their general experience with wayfinding in this clinic: “Wayfinding is difficult. Everything seems chaotic to me” (D2).
Visual communication and signage
The participating clinics had different approaches regarding visual communication and signage design. The two main strategies that could be identified () were (1) using colours to guide the patients (assigning each floor a different colour, colour stripes on the walls) and (2) the minimalistic signage design (black letters on white walls/signs). During patient shadowing, it was observed that the minimalistic signs were often not noticed by patients, while the colourful wall-stripe design in clinic D was confusing for patients, who sometimes got lost in this area (4 observed events). One patient in this clinic mentioned “the labelling of the wards in the elevator and labelling of the rooms in the therapy area“ as barriers in the clinic’s built environment (D4). In one of the clinics with a minimalistic signage design (clinic E), a patient also reported signage as a barrier, stating that “the signs are not visible or not there” (E7). One patient in clinic F suggested that the use of colours might be helpful for wayfinding (F8). In contrast to this, clinic E adopted the approach of colour coding for different wards, and patients still found it confusing (E9) and unclear (E2). In clinic A, which has a complex configuration resulting from growth in stages, colour coding of the floors was used as a signage strategy. One patient in this clinic stated that “room numbers are misleading, there is too little signage” (A6). A patient of clinic G reported a similar experience: “Information is too small/not quickly recognisable. Numbering of the rooms is not immediately logical” (G4). Most observed patients did not even look at the signage while travelling through the clinic, as they were already staying there as inpatients for some time, and this was a relatively familiar environment.
Characteristics of patients’ paths
As 42 wayfinding events were observed among the shadowed 70 patients, the characteristics of the paths where these events occurred were explored. An average path where patients encountered wayfinding-related events had four choice nodes (four places where a choice had to be made on which direction to turn). The most common number of possible choices in the node where they encountered wayfinding-related events was two (). There was also one level (floor) change on an average path. When the deviation angle (measured angle between the two possible corridor choices in the choice node) was examined, the corridors were in a straight line (forming a 0° angle) in twenty cases; they formed an angle lower than 90° in three cases and a 90° or larger angle in twelve cases (). These results indicate that the patients had to choose between going left or right or between continuing straight or turning (left or right) in the choice node in most observed cases. In cases when the observed patient had mistaken the floor, the patient would look out and decide that this was the floor where they needed to get out when the elevator door opened (due to someone else calling the elevator on that floor).
Table V. Characteristics of the wayfinding-related events in the corridors (n = 35)
It was also observed that the corridor segments in the decision nodes were often similar in basic dimensions and visual characteristics (e.g., length, width, wall colour). When the wayfinding-related event was observed in each case, this choice node was marked, and the corridor segments that were possible choices were measured for their length and width difference in the floor plan. The average width difference between the possible corridor segment choices was 0.34 m (Mo = 0 m, Md = 0.04 m), and the average length (depth from the observer’s point) difference was 10.04 m (Mo = 2.1 m, Md = 6.01 m). In all cases, the wall colour was the same in each corridor segment from the choice node.
Additional covered distance
When a patient encountered a wayfinding-related event in 27 of 42 recorded cases, they covered a longer distance than necessary to find the right path. This was more frequently the case when the wayfinding-related event occurred in the corridor (compared to the events of exiting the elevator). These events increased the expected distance between patients’ starting point and destination by adding an additional segment where the patient was going in the wrong direction and then backtracking to find the right path. This search for the right path and subsequent backtracking resulted in an average added distance of 44.43 m, ranging from 0.5 to 184.75 m (). This finding implies that patients commonly took a long time to realize they were on the incorrect path and had difficulty retracing their steps following a wrong turn. When patients exited the elevator on the wrong floor, they quickly realized their error and walked an extra 8.76 m on average (ranging from 5.9 m to 13.8 m).
Table VI. Characteristics of wayfinding-related events observed in corridors and between floors (n = 27)
Discussion
This research study investigated the wayfinding behaviour of stroke inpatients in rehabilitation clinics. There were five main findings: (1) wayfinding-related events were frequently observed and reported in stroke patients, regardless of their mobility level, (2) patients most commonly experienced these events on the paths between patient rooms and therapy rooms, (3) patients mainly relied on backtracking or help of the staff to find their way, (4) they had to cover a substantial additional distance as a result, and (5) the complexity of spatial configurations and the similarity of corridor segments likely contributed to challenging wayfinding. Compared to most research investigating wayfinding, where the participants would have to find their way in an unfamiliar environment, this study adopted a different approach. Stroke patients’ behaviour was observed on their typical inpatient day during recovery after some time spent in a rehabilitation clinic (median length of stay was 19.5 days on the observation day). This approach provided real-life insight into the characteristics of wayfinding-related events that patients experience. The results show that stroke patients still experience navigation challenges, even in an environment that is not entirely new to them.
The finding that many stroke patients have difficulties finding their way is in line with research studies using very different methods, such as the self-report survey (Van Der Ham et al., Citation2013), Floor Maze Test (FMT; Hamre et al., Citation2020), wayfinding performance tasks (Asselen et al., Citation2006) or Virtual Tübingen test (Claessen et al., Citation2017). In this study, around a third of participating patients were observed to encounter at least one wayfinding-related event, and half of the participants reported getting lost in their clinic at least once. This finding suggests that a careful design of wayfinding systems (e.g., layout, visual communication) in rehabilitation clinics is important for the stroke patient population. Challenging wayfinding combined with patients’ specific stroke-related impairments such as cognitive impairments (Jokinen et al., Citation2015) and visuospatial neglect (Maxton et al., Citation2013) might make patients dependent on the staff members to bring them from one location to another. This practice was observed in the clinics participating in this study, and it could further contribute to patients’ feeling of loss of control (Bendz, Citation2003) and limit the possibilities for exercising mobility and independence.
Building layout considerations
Many aspects of the built environment of healthcare facilities may influence wayfinding, such as maps, signs, logical clustering of functions, furniture, logical pairing of interior architecture elements, structural elements, architectural features, and other design elements (artwork, furniture, plants, wall colour, display boards and vending machines; Pati et al., Citation2015). Our study observed the influence of the building’s layout (spatial configuration) and corridor’s visual characteristics on patients’ wayfinding performance. Research focusing on wayfinding performance of stroke patient population in relatively familiar inpatient healthcare settings is lacking, but some similarities can be observed with results from other contexts. In patients with dementia, who commonly experience cognitive decline that affects their navigation ability, the layout of the circulation system was identified as the most influential environmental factor impacting wayfinding (Marquardt & Schmieg, Citation2009). In this study, people with dementia were able to find their way easier in the case of a straight circulation system compared to layouts that included numerous shifts in direction. In another study outside of the healthcare context, routes that seemed straighter and closer to the target were preferred by people navigating (Van Tilburg & Igou, Citation2014). In our study, the building’s spatial configuration (e.g., radial, compact), the number of choice nodes on the path (corridor intersections where the patient had to choose a direction) and the angle between the possible choices in the node were identified as some of the main factors influencing the wayfinding performance. This finding shows similarities with the studies focusing on other user groups and indicates that the building’s layout plays a role in stroke patients’ wayfinding.
The lowest amount of wayfinding-related events were observed in clinics with a central vertical core and radially distributed wards (3 or 4 building wings). The radial layout was likely the simplest to navigate due to the reduced number of choice nodes on the paths—the patient only had to choose the correct building wing when exiting the elevator. Similarly, studies in virtual environments suggest that fewer choices at nodes and fewer rather than more routes and corridors may facilitate successful wayfinding (Cubukcu & Nasar, Citation2005; Slone et al., Citation2015). The principle of reducing the number of choice nodes could be used in layout planning for new buildings, especially for connections between patient rooms and therapy areas. Given that patients’ daily lives mainly consist of attending multiple therapies per day, it is not surprising that most wayfinding-related events were observed on the way from the patient’s room to therapies and vice versa. The connections between these two functional units within a rehabilitation clinic should be given special attention since patients must visit therapies multiple times per day. Wayfinding challenges between these two areas are likely to impact patients’ quality of daily life in rehabilitation clinics and the healthcare processes. Here, the number of choice nodes (corridor intersections/choices in navigation) should be reduced to three or fewer.
One of the most challenging aspects of spatial problem-solving is dealing with symmetrical architectural environments (Remolina & Kuipers, Citation2004). In a study by Baskaya et al. (Citation2004), 63.2% of the participants in a symmetrical building felt “completely lost”, in contrast to only 6.5% of those in an asymmetrical setting (p. 851). A similar influence of symmetrical layouts was observed in other contexts (An et al., Citation2019; Hölscher & Dalton, Citation2008). Therefore, wayfinding could be negatively affected by the use of symmetry and the repetition of similar elements (Baskaya et al., Citation2004). This is comparable to the findings of this study, where the corridor segments in the decision nodes (where the wayfinding-related events were observed) were similar in basic dimensions and appearance. Unsymmetric spatial configurations should be explored in rehabilitation clinic design from the standpoint of easier wayfinding, and corridor symmetry in the choice nodes should be avoided by architectural differentiation of the corridor segments. This can be achieved using various orientation cues, such as widening the corridor at a certain point and creating a more open space, creating distinctive environments with the use of windows, plants, art, seating areas, materialization and colour. The hierarchy of corridors and their role in a clinic’s circulation system, analogous to the hierarchy of urban streets in a city, should be considered in the design (Allison, Citation2007).
Furthermore, different building floors should be given different visual identities as well. This study offered some new insights into the multilevel wayfinding behaviour of stroke patients. As most wayfinding research focuses on single floor levels and not level changes (Hölscher et al., Citation2006), this aspect of the built environment is still not explored sufficiently. Still, one of the most common sources of confusion about one’s direction and location in a building is the level changes (Hölscher et al., Citation2013). Wayfinding can be particularly difficult in multistorey buildings because of the way the floors are arranged and since there is no visual reference between the floors (Hölscher et al., Citation2013). Understanding these challenges may help designers make decisions that enable more successful wayfinding (Devlin, Citation2014). For example, each clinic’s floor could be given a specific architectural and visual identity around elevator exits to minimize the wayfinding challenges observed in this study. Various corridor configurations and dimensions, corridor widenings and space openings, different views, or various landmarks could be used to establish these different identities for each floor, visible from the buildings’ vertical circulation (elevators and stairs). This strategy might help patients recognize the floors and make fewer wayfinding mistakes when travelling vertically through the building.
Signage and auditory information considerations
The participating clinics used different signage and colour coding strategies to aid wayfinding, and no auditory information was used. Therefore, the influence of visual and auditory signage could not be assessed in this study. Still, some patients reported the signage to be confusing, unclear, and in the case of minimalistic design—not visible or not at all there. As buildings become larger and more complex, providing adequate wayfinding using only signs and other cues becomes more challenging, particularly if the indicated directions conflict with how people understand and use the space (Dogu & Erkip, Citation2000). The principle of a building’s spatial organization needs to be communicated to the wayfinding users by the structure itself since signage often cannot compensate for architectural failures (Arthur & Passini, Citation1992). Signage, furnishings and lighting could be used as additional supporting components, but they should not be relied on to compensate for inadequate architectural design (Marquardt, Citation2011). Consequently, signs and maps do not fundamentally solve wayfinding problems (Jamshidi & Pati, Citation2021).
It is essential to strategically plan the buildings’ spatial configuration in the early design stages since this can directly affect patients’ wayfinding, independence, and daily lives during rehabilitation. This is not always possible, especially in the case of existing buildings. Here, minor changes in the form of signage and colour coding of the wards/floors could potentially improve the wayfinding performance of patients. In this study, the common strategy of using colourful lines on the wall (or floor) in healthcare facilities was observed to create confusion among study participants. The need to remember the colour of the particular arrow along the route might be a challenge for people with different abilities and impairments (Morag et al., Citation2016). Therefore, signage needs to be simple, readily available, legible, and structured to aid navigation, and pictograms should be considered as many patients might be unable to read (Marquez et al., Citation2017). Creating distinct landmarks may also be particularly important in existing buildings with symmetrical layouts (Baskaya et al., Citation2004). Various technologies could also be considered to guide patients along the way, e.g., auditory signals in elevators already commonly used in healthcare facilities. Dynamic displays could present relevant information along the route and guide the person, using different fonts or language, according to their needs (Hashim et al., Citation2014), or a dynamic system could guide each person with arrows projected on the floor (Morag et al., Citation2016). Mobile wayfinding applications could also be explored for wayfinding purposes, combined with signage and other navigation strategies (Harper et al., Citation2020). All these strategies need further evaluation for their impact on the wayfinding performance of stroke patients who can experience complex impairments limiting their ability to read the signs or understand environmental cues.
Considerations for patients’ diverse abilities
People who have limitations in their health or cognitive abilities are more reliant on their external environment as they cannot always adapt their surroundings to their particular needs (Lawton & Simon, Citation1968). This is why the way the buildings’ layout and signage are designed is of great importance for stroke patients during recovery. At the same time, challenging wayfinding and longer covered distances observed as one of the results in this study might not solely be a negative aspect of the built environment for some patients. Patients in the advanced rehabilitation phases might benefit from a more challenging environment that prepares them for going back home and the built environment barriers they might experience at home or in the community. The patients’ daily paths to and from therapies could be valuable for exercising wayfinding in a more controlled environment. For this reason, patients’ abilities and needs in different recovery stages should be considered in the design and placement of patients in the wards that are differently positioned in the building. Patients in the beginning stages of rehabilitation would benefit from a barrier-free and easy-to-navigate environment that supports their independence, while patients in the later stages could benefit from more complex environments for wayfinding training. The clinic’s spatial configuration and connections between the two main functional areas: patient rooms and therapy rooms, might greatly influence patients’ wayfinding ability. Ideally, the therapy areas should be located on the same level as the wards for patients with severe impairments in the beginning stages of rehabilitation to reduce distances and the number of choice nodes, and allow them to find their way easily and independently.
Strengths and limitations
The main strengths of this study are that: (1) it offered insights into the usual daily wayfinding behaviour of stroke patients in seven large multilevel rehabilitation clinics, (2) focusing on one patient at a time over an extended period (one whole day) provided information on the wayfinding challenges they encounter, as well as how they overcome them, and (3) employing two complementing research methods allowed for the exploration of two different perspectives on the phenomenon studied. This research study also has some limitations that need to be mentioned. Participants’ behaviour might have been altered due to close and extended observation. To minimize the behaviour modifications, patients were only told that their paths were being observed and not that the study focused on their wayfinding behaviour. Furthermore, only one day in the recovery journey of a stroke patient was observed and their navigation ability and needs might change over time. Moreover, excluding patients with dementia, severe communication and cognitive impairments and other specific conditions removed the representation of their wayfinding experiences; their spatial needs also require special attention. An additional limitation is the missing cognitive assessment of the participants, which might have provided helpful information for understanding their wayfinding abilities. It was also not possible to assess the influence of signage on wayfinding performance in this study. Furthermore, none of the participating clinics used audio signals to announce the floors in the elevators, and the influence of such strategies could not be observed. Even with the highlighted limitations, this study offers novel insights into the wayfinding behaviour of stroke patients. Future research could use additional methods such as eye-tracking in virtual reality environments to examine the patients’ wayfinding behaviour in relation to their post-stroke cognitive impairments or in-depth interviews to further explore their wayfinding experiences.
Conclusion
There is still a lack of understanding of how the built environment of rehabilitation clinics might affect the behaviour and activities of stroke patients in rehabilitation clinics. This study suggests that challenging wayfinding is commonly experienced by patients during their inpatient stay and that the building’s layout might play an important role. As the building’s layout organization is frequently chosen in the early design stages, the implications of each layout type need to be considered already at the start of planning. Each building’s layout type likely introduces a set of wayfinding challenges that the planners need to be aware of and apply targeted mitigation strategies. Even minor design interventions implemented during building renovations could improve the ease of wayfinding. Newly built clinics and the existing clinics might benefit from further research on the relationship between the built environment and stroke patient wayfinding. Therefore, when carefully planned, the built environment of rehabilitation clinics could potentially improve stroke patients’ daily experiences of wayfinding during recovery.
Ethics statement
The complete research study entitled “Mobility of stroke patients in neurological rehabilitation clinics” was approved by the Ethical Committee at the Technische Universität Dresden (approval number: EK 452102016).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
Notes on contributors
Maja Kevdzija
Dr.-Ing. Maja Kevdzija, EDAC is an Assistant Professor at the Faculty of Architecture and Planning at TU Wien, Austria in the field of Healthcare Design. She obtained her PhD in 2020 at the Faculty of Architecture at Technische Universität Dresden, Germany. Her research study on mobility-supporting rehabilitation clinics for stroke patients was awarded the Healthcare Environment Award 2020 in the Post-Graduate Student category, the 2021 European Healthcare Design Award in the Design Research category and the 2021 EDRA Certificate of Research Excellence (CORE) with Merit Status. Her research focuses on improving built environments for rehabilitation after a stroke.
References
- Adamson, J., Beswick, A., & Ebrahim, S. (2004). Is stroke the most common cause of disability? Journal of Stroke and Cerebrovascular Diseases, 13(4), 171–12. https://doi.org/10.1016/j.jstrokecerebrovasdis.2004.06.003
- Allison, D. (2007). Hospital as a city: Employing urban design strategies for effective wayfinding. Health Facilities Management, 20(6), 61–65.
- An, D., Ye, J., & Ding, W. (2019). Spatial features and elements affecting indoor wayfinding—a case study in a transit hub. In H. Krömker (Ed.), HCI in Mobility, Transport, and Automotive Systems. HCII 2019. Lecture Notes in Computer Science() (Vol. 11596). Cham: Springer. 357–367 . https://doi.org/10.1007/978-3-030-22666-4_26.
- Arthur, P., & Passini, R. (1992). Wayfinding: People, signs, and architecture. New York: McGraw-Hill.
- Asselen, M., Van Kessels, R. P. C., Kappelle, L. J., Neggers, S. F. W., Frijns, C. J. M., & Postma, A. (2006). Neural correlates of human wayfinding in stroke patients. Brain Research, 1067(1), 229–238. https://doi.org/10.1016/j.brainres.2005.10.048
- Baskaya, A., Wilson, C., & Özcan, Y. Z. (2004). Wayfinding in an unfamiliar environment: different spatial settings of two polyclinics. Environment and Behavior, 36(6), 839–867. https://doi.org/10.1177/0013916504265445
- Bendz, M. (2003). The first year of rehabilitation after a stroke - From two perspectives. Scandinavian Journal of Caring Sciences, 17(3), 215–222. https://doi.org/10.1046/j.1471-6712.2003.00217.x
- Best, G. (1970). Direction Finding in Large Buildings, in D. V. Canter (Ed.), Architectural Psychology - Proceedings of the conference at Dalandhui, RIBA, London, 72–75.
- Claessen, M. H. G., Visser-Meily, J. M. A., De Rooij, N. K., Postma, A., & Van Der Ham, I. J. M. (2016). A direct comparison of real-world and virtual navigation performance in chronic stroke patients. Journal of the International Neuropsychological Society, 22(4), 467–477. https://doi.org/10.1017/S1355617715001228
- Claessen, M. H. G., van der Ham, I. J. M., Jagersma, E., & Visser-Meily, J. M. A. (2016). Navigation strategy training using virtual reality in six chronic stroke patients: A novel and explorative approach to the rehabilitation of navigation impairment. Neuropsychological Rehabilitation, 26(5–6), 822–846. https://doi.org/10.1080/09602011.2015.1045910
- Claessen, M. H. G., Visser-Meily, J. M. A., Meilinger, T., Postma, A., de Rooij, N. K., & van der Ham, I. J. M. (2017). A systematic investigation of navigation impairment in chronic stroke patients: Evidence for three distinct types. Neuropsychologia, 103, 154–161. https://doi.org/10.1016/j.neuropsychologia.2017.07.001
- Cooper, R. (2010). Wayfinding for health care: Best practices for today's facilities. Chicago, IL: AHA Press/Health Forum.
- Cubukcu, E., & Nasar, J. L. (2005). Relation of physical form to spatial knowledge in largescale virtual environments. Environment and Behavior, 37(3), 397–417. https://doi.org/10.1177/0013916504269748
- Delgrange, R., Burkhardt, J. M., & Gyselinck, V. (2020). Difficulties and problem-solving strategies in wayfinding among adults with cognitive disabilities: A look at the bigger picture. Frontiers in Human Neuroscience, 14(February).
- Devlin, A. S. (2014). Wayfinding in healthcare facilities: Contributions from environmental psychology. Behavioral Sciences, 4(4), 423–436. https://doi.org/10.3390/bs4040423
- Dogu, U., & Erkip, F. (2000). Spatial factors affecting wayfinding and orientation: A case study in a shopping mall. Environment and behavior, 32(6), 731–755.
- Feigin, V. L., Norrving, B., & Mensah, G. A. (2017). Global Burden of Stroke. Circulation Research, 120(3), 439–448. https://doi.org/10.1161/CIRCRESAHA.116.308413
- Hamre, C., Fure, B., Helbostad, J. L., Wyller, T. B., Ihle-Hansen, H., Vlachos, G., Ursin, M. H., & Tangen, G. G. (2020). Impairments in spatial navigation during walking in patients 70 years or younger with mild stroke. Topics in Stroke Rehabilitation, 27(8), 601–609. https://doi.org/10.1080/10749357.2020.1755814
- Haq, S., & Zimring, C. (2003). Just down the road a piece: The development of topological knowledge of building layouts. Environment and behavior, 35, 132–160.
- Harper, C., Duke, T., Crosser, A., Avera, A., & Jefferies, S. (2020). Designing hospital wayfinding systems, touchscreen kiosks, environmental cues and mobile apps: An evaluation of a mobile wayfinding application. In Advances in Intelligent Systems and Computing (Vol. 957). Springer International Publishing. 89–96 . https://doi.org/10.1007/978-3-030-20451-8_9
- Hashim, M. J., Alkaabi, M. S., & Bharwani, S. (2014). Interpretation of way-finding healthcare symbols by a multicultural population: Navigation signage design for global health. Applied Ergonomics, 45(3), 503–509. https://doi.org/10.1016/j.apergo.2013.07.002
- Hillier, B., Hanson, J., & Peponis, J. (1984). What do we mean by building function? (pp. 61–72). (J. A. Powell, I. Cooper, S. Lera, Eds.). London: Designing for Building Utilization, Spon.
- Hölscher, C., Meilinger, T., Vrachliotis, G., Brösamle, M., & Knauff, M. (2006). Up the down staircase: Wayfinding strategies in multi-level buildings. Journal of Environmental Psychology, 26(4), 284–299. https://doi.org/10.1016/j.jenvp.2006.09.002
- Hölscher, C., & Dalton, R. C. (2008). Comprehension of layout complexity: Effects of architectural expertise and mode of presentation. In J. S. Gero & A. K. Goel (Eds.), Design Computing and Cognition ‘08. Dordrecht: Springer. 159–178 . https://doi.org/10.1007/978-1-4020-8728-8_9
- Hölscher, C., Büchner, S., & Strube, G. (2013). Multi-floor buildings and human wayfinding cognition. Behavioral and Brain Sciences, 36(5), 551–552. https://doi.org/10.1017/S0140525X1300040X
- Iftikhar, H., Shah, P., & Luximon, Y. (2021). Human wayfinding behaviour and metrics in complex environments: A systematic literature review. Architectural Science Review, 64(5), 452–463. https://doi.org/10.1080/00038628.2020.1777386
- Jamshidi, S., & Pati, D. (2021). A narrative review of theories of wayfinding within the interior environment. HERD, 14(1), 290–303.
- Jokinen, H., Melkas, S., Ylikoski, R., Pohjasvaara, T., Kaste, M., Erkinjuntti, T., & Hietanen, M. (2015). Post-stroke cognitive impairment is common even after successful clinical recovery. European Journal of Neurology, 22(9), 1288–1294. https://doi.org/10.1111/ene.12743
- Kalantari, S., & Snell, R. (2017). Post-occupancy evaluation of a mental healthcare facility based on staff perceptions of design innovations. HERD: Health Environments Research & Design Journal, 10(4), 121–135. https://doi.org/10.1177/1937586716687714
- Kaplan, A. D., Cruit, J., Endsley, M., Beers, S. M., Sawyer, B. D., & Hancock, P. A. (2021). The effects of virtual reality, augmented reality, and mixed reality as training enhancement methods: A meta-analysis. Human Factors, 63(4), 706–726.
- Kevdzija, M., & Marquardt, G. (2018). Physical barriers to mobility of stroke patients in rehabilitation clinics. Breaking Down Barriers, 147–157. https://doi.org/10.1007/978-3-319-75028-6_13
- Kevdzija, M., & Marquardt, G. (2022). Impact of distance on stroke inpatients’ mobility in rehabilitation clinics: A shadowing study. Building Research and Information, 50(1–2), 74–88. https://doi.org/10.1080/09613218.2021.2001302
- Langhorne, P., Coupar, F., & Pollock, A. (2009). Motor recovery after stroke: A systematic review. Lancet neurology, 8(8), 741–754. https://doi.org/10.1016/S1474-4422(09)70150-4
- Lawton, M. P., & Simon, B. (1968). The ecology of social relationships in housing for the elderly. The Gerontologist, 8(2), 108–115. https://doi.org/10.1093/geront/8.2.108
- Marquardt, G., & Schmieg, P. (2009). Dementia-friendly architecture: Environments that facilitate wayfinding in nursing homes. American Journal of Alzheimer’s Disease and Other Dementias, 24(4), 333–340. https://doi.org/10.1177/1533317509334959
- Marquardt, G. (2011). Wayfinding for people with dementia: A review of the role of architectural design. HERD, 4(2), 75–90. https://doi.org/10.1177/193758671100400207
- Maxton, C., Dineen, R. A., Padamsey, R. C., & Munshi, S. K. (2013). Don’t neglect’ neglect’- An update on post stroke neglect. International Journal of Clinical Practice, 67(4), 369–378. https://doi.org/10.1111/ijcp.12058
- McDonald, S. (2005). Studying actions in context: A qualitative shadowing method for organisational research. Qualitative Research, 5(4), 455–473.
- Morag, I., Heylighen, A., & Pintelon, L. (2016). Evaluating the inclusivity of hospital wayfinding systems for people with diverse needs and abilities. Journal of Health Services Research & Policy, 21(4), 243–248. https://doi.org/10.1177/1355819616642257
- Marquez, D. X., Hunter, R. H., Griffith, M. H., Bryant, L. L., Janicek, S. J., & Atherly, A. J. (2017). Older Adult Strategies for Community Wayfinding. Journal of Applied Gerontology, 36(2), 213–233. https://doi.org/10.1177/0733464815581481
- Morganti, F., Sabattini, P., & Casale, R. (2019). Can motor and cognitive rehabilitation work together? The example of spatial disorientation treatment after stroke. In A. A. M. Hassan, M. E. De, & G. Eds (Eds.), New Techno (Vol. 1002, pp. 46–57). Cham: Springer. https://doi.org/10.1007/978-3-030-16785-1
- Nikolaus, G., Zwingmann, C., & Jäckel, W. H. (2006). The system of rehabilitation in Germany. In J. Bengel, W. H. Jäckel, & J. Herdt (Eds.), Research in rehabilitation. Results from a research network in Southwest Germany (pp. 3–19). Stuttgart: Schattauer.
- Pati, D., Harvey, T. E., Willis, D. A., & Pati, S. (2015). Identifying elements of the health care environment that contribute to wayfinding. HERD: Health Environments Research & Design Journal, 8(3), 44–67. https://doi.org/10.1177/1937586714568864
- Peponis, J., Zimring, C., & Choi, Y. K. (1990). Finding the building in wayfinding. Environment and Behavior, 22(5), 555–590. https://doi.org/10.1177/0013916590225001
- Rabadi, M. H., Rabadi, F. M., & Peterson, M. (2008). An analysis of falls occurring in patients with stroke on an acute rehabilitation unit. Rehabilitation Nursing: the Official Journal of the Association of Rehabilitation Nurses, 33(3), 104–109. https://doi.org/10.1002/j.2048-7940.2008.tb00213.x
- Remolina, E., & Kuipers, B. (2004). Towards a general theory of topological maps. Artificial intelligence, 152(1), 47–104. https://doi.org/10.1016/S0004-3702(03)00114-0
- Robertson, I. H., & Halligan, P. W. (1998). Spatial Neglect. A Clinical Handbook for Diagnosis and Treatment. East Sussex, UK: Psychology Press.
- Rowe, F., Brand, D., Jackson, C. A., Price, A., Walker, L., Harrison, S., Eccleston, C., Scott, C., Akerman, N., Dodridge, C., Howard, C., Shipman, T., Sperring, U., Macdiarmid, S., & Freeman, C. (2009). Visual impairment following stroke: Do stroke patients require vision assessment?. Age and ageing, 38(2), 188–193. https://doi.org/10.1093/ageing/afn230
- Slone, E., Burles, F., Robinson, K., Levy, R. M., & Iaria, G. (2015). Floor plan connectivity influences wayfinding performance in virtual environments. Environment and Behavior, 47(9), 1024–1053. https://doi.org/10.1177/0013916514533189
- Sun, J.-H., Tan, L., & Yu, J.-T. (2014). Post-stroke cognitive impairment: epidemiology, mechanisms and management. Annals of Translational Medicine, 2(8), 80. https://doi.org/10.3978/j.issn.2305-5839.2014.08.05
- Ulrich, R. S., Zimring, C., Zhu, X., DuBose, J., Seo, H.-B., Choi, Y.-S., Quan, X., & Joseph, A. (2008). A review of the research literature on evidence-based healthcare design Design Journal. & 1(Part I), 101–165. https://doi.org/10.1177/193758670800100306 Healthcare Leadership White Paper Series #5. HERD: Health Environments Research
- Van Der Ham, I. J. M., Kant, N., Postma, A., & Visser-Meily, J. M. A. (2013). Is navigation ability a problem in mild stroke patients? Insights from self-reported navigation measures. Journal of Rehabilitation Medicine, 45(5), 429–433. https://doi.org/10.2340/16501977-1139
- van Tilburg, W. A. P., & Igou, E. R. (2014). Moving onwards: An action continuation strategy in finding the way. Journal of behavioral decision making, 27(5), 408–418. https://doi.org/10.1002/bdm.1817
- Wright, P., Hull, A. J., & Lickorish, A. (1993). Navigating in A hospital outpatients department – The merits of maps and wall signs. J Archit Plann Res, 10, 76–89.