Abstract
Purpose: The importance of assistive technology (AT) as a pillar of universal health coverage was recognized at the 71st World Health Assembly (WHA) through the passing of Resolution 71.8 on improving access to AT (May 2018). A systematic analysis was conducted on the responses made to the Resolution by Member States and non-state actors, in order to provide a snapshot of global intent.
Methods: Qualitative content analysis was conducted on over 40 written “Statements” made by Member States and non-state actors in response to Resolution 71.8.
Results: The Resolution provides tangible guidance to the World Health Organisation (WHO) and its member states in order for them to meet commitments within the Convention on the Rights of Persons with Disabilities (CRPD). Statements made in response to the Resolution offer a unique plethora of multi-stakeholder views from differing global perspectives. Analysis identified a range of themes within two overarching themes: intersection of health, human rights and sustainable development; and international collaboration and support within an international agenda framework.
Conclusion: The content analysis synthesises complex global data and identifies directions to positively influence national and regional AT policy and delivery. The complexity of factors demonstrates the importance of an AT systems-thinking approach; that is, the development and application of organised knowledge, skills, procedures and policies related to assistive products. AT systems thinking will be essential for AT to be effectively deployed as a pillar of universal health coverage.
Assistive technology is a key facilitator of health and well-being, playing a critical role in global efforts to improve population health outcomes and strengthening health systems
Access to assistive technology is a public health priority and is an essential health product to be covered under Universal Health Coverage
Effective action on access to assistive technology must encompass the reality of diverse contexts yet common purposes expressed by global actors
This analysis demonstrates the intersection of the health, human rights and sustainable development agendas, and the importance of international collaboration and support in achieving effective access
IMPLICATIONS FOR REHABILITATION
Introduction
In May 2018, the 71st World Health Assembly (WHA) adopted Resolution 71.8 on improving access to assistive technology (AT) [Citation1]. It provides tangible guidance to the World Health Organisation (WHO) and its member states in order for them to meet commitments within the Convention on the Rights of Persons with Disabilities (CRPD) [Citation2]. In response to the Resolution, Member States and non-state actors made more than 40 official “Statements.” These Statements offer a unique plethora of multi-stakeholder views from differing global perspectives. By analysing these Statements, this article seeks to identify major common themes that may inform thinking around AT systems-thinking; which is the development and application of organised knowledge, skills, procedures and policies related to assistive products [Citation3]. Such thinking has the potential to, in turn, influence national and regional AT policy and delivery.
Assistive technology as a universal health issue
AT is the umbrella term for assistive products and related systems and services to maintain and improve function and well-being [Citation4]. AT can improve population health outcomes by improving an individual’s quality of life and empowering productive participation in labour markets and civic life. AT not only improves a person’s functional ability, but also enhances potential life opportunities, such as access to quality education and meaningful employment. AT can further improve health outcomes by managing and preventing secondary conditions resulting from impairments [Citation5]. Access to affordable, quality AT fosters inclusive societies enabling people to live dignified, independent, and healthy lives. As assistive products are essential tools to rationalise health and welfare costs, enabling people in need to remain healthy, independent and productive, AT can also be seen to strengthen health systems, serving to reduce demands on health and social support services, such as long-term care and caregivers [Citation6]; and AT improves service delivery and reduces strain on the health workforce. AT may also contribute substantively to the equitable achievement of the Sustainable Development Goals (SDG’s) and is vital for advancing population health outcomes, both as a mediator and as a moderator of such outcomes [Citation7].
Assistive products are as essential for achieving the goal of Universal Health Coverage (UHC) as are medicines and vaccines. To be provided universally they must be supplied at a cost that is affordable. One way of conceptualising progress towards UHC, as shown in , is along three dimensions: the range of services that are needed, the number and variety of people who need them, and the costs to users or third-party funders [Citation8]. With increasing funds, the needs of non-covered populations may be covered, non-covered services may be provided, and direct costs may be reduced. As a component of UHC, access to AT can be operationalised and measured in the above three dimensions related to the coverage of people; assistive products and services; and financing and payments. Additional funds can be targeted to include people or assistive products that were not covered previously, or to reduce the direct payments needed to acquire, use, maintain or repair assistive products.
Figure 1. Three dimensions to consider when moving towards universal coverage [Citation8].
![Figure 1. Three dimensions to consider when moving towards universal coverage [Citation8].](/cms/asset/3d112f3f-2e19-4c5e-907c-f4356c538065/iidt_a_1774929_f0001_c.jpg)
The provision of assistive products is both an end and a means of UHC: an end as it is a service to be covered by UHC, and a means as it can be used to access (or provide) other health services covered by UHC. For example, a wheelchair, a pressure cushion and continence products are not only life-saving for a child with spina bifida, but also enables school attendance, participation in family life, and access to health services. For an older person with diabetes, protective footwear could prevent an amputation; while low vision aids enable them to continue to live at home. At the same time, low vision aids enable access to health information and communication with health professionals, and protective footwear allows for walking to the health centre. These examples illustrate the virtuous circles that can be stimulated through well-functioning AT systems.
Assistive technology as a public health priority
An estimated one billion people (one in seven) need one or more assistive products in order to live healthy and productive lives. However, access to AT can vary greatly between and within countries; with only one in ten people having access to the necessary assistive products and services they need (1). Barriers to access are many, from lack of awareness, availability of appropriate products and services, and prohibitive costs. Those requiring assistive products and services are 50% more likely to suffer from catastrophic health expenditures when accessing them [Citation9]. Those who need AT are more likely to be trapped in a poverty cycle where disability fuels social exclusion and poverty, which in turn exacerbates risk for disability and ill health [Citation10–12]. Insufficient market competition, and additional tariffs imposed on international trade that deter affordable supply of AT, further perpetuates this cycle of poverty, Additionally, the risk of incurring catastrophic health expenditures (threatening a household’s financial ability to address subsistence needs) remains high, if a country attempts to include AT in UHC.
With ageing populations and non-communicable diseases on the rise, it is estimated that by 2050 more than two billion people (one in four) will require assistive products [Citation4]. Addressing the gap in access and preventing it from widening further by ensuring affordable access to AT, is therefore a key and urgent public health priority. This has led to recognition that access to AT should be developed as a key part of the systems-strengthening approach to population health, and of the implementation of the CRPD and the actions to achieve the Sustainable Development Goals (SDGs)Footnote1.
Assistive technology as a health policy imperative
The goal of the World Health Organisation’s (WHO) 13th General Programme of Work (GPW13) released in May 2018 is to improve the lives of three billion people. This places significant emphasis on improving health and reducing inequities among vulnerable populations which include women, children, older people, people with disabilities, and people who are poor. WHO has been leading global efforts to improve access to AT. In 2014, WHO established the Global Cooperation on Assistive Technology (GATE) initiativeFootnote2 to realise the obligations of the CRPD [Citation2] towards increasing access to AT (article 32 in particular). With these mandates, WHO is focussing its efforts on supporting member states to include AT within UHC. Learning from the development of the WHO model list of essential medicinesFootnote3, GATE published the first WHO model list of Priority Assistive Products List [Citation13] in 2016 which aims to increase the affordability, quality and accessibility of assistive products. In collaboration with key stakeholders, WHO has contributed to shaping the agenda of a AT global partnership – ATscaleFootnote4 – which will align and consolidate international efforts to improve access to AT, with specific focus on market shaping to drive affordability [Citation14].
The work of WHO and its Member States is now further propelled by WHA Resolution 71.8, highlights of which are given in .
Table 1. Key Components of the WHA resolution on improving access to assistive technology.
Purpose
In response to WHA Resolution 71.8, many delegations verbally presented written statements. The objective of this study was to analyse these responses to the Resolution in order to identify and categorise common themes and priorities. Such an analysis has the potential to better understand how global actors can contribute to strengthening a systems-thinking discourse in the field of AT, and to point to a better defined list of strategic actions requested by Member States.
Method
The sample
The sample comprises all 41 written Statements made during the 71st WHA in response to Resolution 71.8: Improving access to assistive technology. The sample includes Statements from 36 Member States from all six WHO regions, 4 Non-State actors (organisations representing civil society) and the WHO secretariat. Ghana, Qatar and Bhutan made regional statements on behalf of the African, Eastern Mediterranean and South-East Asian Regions (representing 79 Member States); in all, the views of 112 of the 194 Member States were heard through the Official Statements, representing and giving voice to a significant range of global perspectives.
Procedure
A systematic approach to qualitative thematic analysis was used to analyse the data, identify and develop themes emanating from the Statements [Citation15]. First, the entire set of Statements was read to gain an overview of the breadth of their content. Notes were made to detail points of interest in the data, as well as potential codes and themes. The next phase of the analysis involved the production of preliminary codes (basic units of analysis) from the data. Two of the authors (author 1 and author 4) independently coded a sample of 10 Statements (8 from member states and 2 from non-state actors). Individual codes were generated, compared and discussed. This inductive process led to the identification of additional codes and separation of broader themes (units of meaning) for further analysis. Finally, the 2nd author in consultation with the 1st author compared statements across WHO region and summarised issues raised.
The 4th author then worked systematically through the entire set of statements, generating codes for all of the data. On completion of this process, a total of 57 codes had been created. Codes were then examined in relation to each other and sorted into preliminary themes. The themes were then reviewed by three authors to determine whether data extracts for each code coherently represented the theme and to ensure that themes were distinct from each other. During this process there was considerable reworking of the codes and themes. A narrative was written for each theme, summarising the central points and verifying that the refined themes were a true reflection of the statements. The final results of the thematic analysis and the code book were reviewed by four of the authors, with consensus being reached through discussion, where needed.
Results
Two overarching themes were identified, namely the intersection of the health, human rights and sustainable development agendas and the importance of international collaboration and support; as well as four subsidiary themes. The results are presented by first describing the challenges faced, then the anticipated outcomes and potential strategies, and thereafter presenting the two overarching themes.
Sub-theme 1: challenges raised by member states
Many of the Statements commenced by summarising the problems or issues facing Member States. This theme is centred on disparities, diversity and changing needs both globally and locally. The increasing need for health and rehabilitation services, including AT, was attributed to ageing populations and the rising prevalence of non-communicable diseases; as well as disability arising from violence or conflict, road traffic accidents and natural disasters. The current and anticipated unmet need for health and rehabilitation services was attributed to issues with the quality and safety of assistive products and related services, as well as environmental barriers to inclusion. A lack of awareness of the scope and the potential of AT, and a lack of affordability of assistive products, were cited as important issues. Several Statements acknowledged disparities at the global level, as well as within countries, due to differing access to resources and geographical challenges of servicing rural and remote communities. Extract from Statements, exemplifying these themes, are produced in .
Table 2. Key statements related to challenges.
Sub-theme 2: desired outcomes and goals
Where the Statements described challenges for necessitating improved access to AT, they also stated outcomes anticipated from addressing these issues. Member states described a range of goals including enhanced inclusion and quality of life, economic participation and productivity, and achievement of UHC. While the emphasis differed between member states, this theme emerged from a convergence around the concepts of health, human rights, and sustainable development (see ).
Table 3. Key statements related to desired outcomes and goals.
Sub-theme 3: strategies
The theme of Strategies reflects the variety of actions and stakeholders required to improve access to AT. These included product-related actions such as promoting innovation and technology transfer and improving manufacturing, procurement, funding and supply chain arrangements. Other strategies focussed on service provision and personnel, such as providing training and strengthening local capacity to provide health and social services and rehabilitation. Inter-sectoral collaboration was recommended, as well as AT user involvement and peer support in the design and delivery of policies and services. Many Statements highlighted the need for national and/or local policies and systems to coordinate discrete actions and ensure that they are based on an assessment of needs and regulated by standards or guidelines that are informed by research and development (see ).
Table 4. Key Statements related to recommended strategies.
Sub-theme 4: connection to other international agendas
In addition to describing how improving access to AT would contribute to goals of health, human rights and sustainable development, many of the Statements referred to formal international agendas and agreements. These include the United Nations Convention on the Rights of Persons with Disabilities (CRPD), Sustainable Development Goals (SDGs), other WHO strategies (e.g., Global Cooperation on Assistive Technology, Rehabilitation 2030, Global Disability Action Plan, EM/RC63/R.3 Improving access to AT, WHO GPW 13, Islamabad declaration on improving access to AT, the Global Strategy and Action Plan on Ageing and Health), the International Labour Organisation’s (ILO) Decent Work Agenda, the Global Disability Summit 2018, and the Ottawa Anti-Personnel Mine Ban Convention. These statements, as illustrated in , highlights the synergies between AT and the formal international health, human rights, and sustainable development agendas, underscoring the point that investing in improving access to AT does not require trade-offs with competing priorities.
Table 5. Key Statements revealing connections to international agendas.
The two overarching themes are presented below.
Intersection of health, human rights and sustainable development
Statements did not only discuss AT and health. This theme expresses the connections made between the Resolution to improve access to AT and global health, human rights, and sustainable development issues and agendas. Extracts from Statements exemplifying this inter-play are presented in .
Table 6. Key Statements exemplifying the inter-play between health, human rights and sustainable development.
2. International collaboration and support within an international agenda framework
Statements acknowledged past and present collaboration and support, and offered or requested further international collaboration and support to improve access to assistive technology. The need for and advantages of international collaboration and support in areas including research, trade and policy were both implicit and explicit in many of the Statements as shown in .
Table 7. Key Statements relating to international collaboration – support required or on offer.
Discussion
The views of 122 member states and members of civil society were represented within the 41 statements, demonstrating a powerful coordination of players and readiness for global action. The Statements from Member States and non-state actors ultimately represented a clear common goal regarding access to assistive technology, in spite of differences in priority, in perspectives and in progress.
Most of the shared Statements resonated with the key components of the WHA Resolution 71.8, confirming the need for and the current and potential impact of AT; challenges in access; need for research and development; standards; procurement and supply, and the alignment with UHC. Analysis of the Statements (i) clearly depicted the convergence of the health, human rights as well as the sustainable development agenda’s, and (ii) highlighted the importance of international collaboration and support.
It is also important to note that key among the priorities is a move beyond the ‘product’ as evidenced by the Statement from HelpAge International:
HelpAge would however caution against too great [an] emphasis being put on the products themselves. The resolution and WHO’s work in this area, must remain person rather than product orientated, recognising diversity, including older age and rapidly changing personal needs. HelpAge welcomes the focus on function and ability in the discussion but cautions against the over-emphasis on mobility. Efforts related to AT must respond to a range of needs, and have at their hearts, the promotion of autonomy, dignity and independence. (HelpAge International)
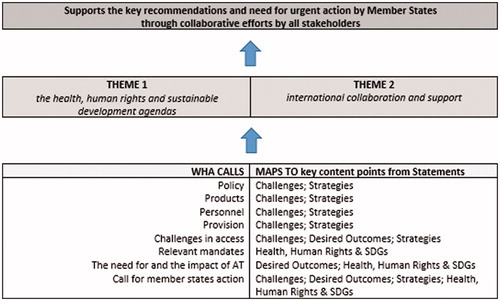
AT as a complex system is demonstrated through the interlinking and multiple challenges noted and solutions proposed. The intersections between international agendas were also evident across the subsidiary themes of challenges, desired outcomes and goals, as well as key strategies as depicted in .
In contrast to individualised views of AT usage, and resonating with a more systemic approach, the Statements analysed in this study focussed on community and population level change, viewing improved access to AT as an enabler of health, development, and human rights. It is also evident that improving access to AT requires inter-sectoral partnerships and knowledge sharing. To assure access to affordable, quality AT and to create sustainable change, will require the engagement and collaboration of all stakeholders, including those not present at the WHA, i.e., service users, carers, service providers, private sector, and health and other professionals. Real change requires empowering and enabling all stakeholders in a way that meaningfully interconnects and compliments their resources, interests and abilities.
AT is related to the political economy of international development cooperation; it is not simply a matter of demand and supply, and it necessitates an understanding that improving access to AT is beyond health professionals alone, requiring inter-sectoral partnership and systems thinking. The donor supporters of AT e.g., USAID, DFID and NORAD, need to be buttressed by other international donors, international and national corporates, and the stimulation of local demand and supply to sustain local provision. We must ensure that national governments, bilateral organisations, donors, and the private sector work conscientiously and deliberately together, to stimulate local demand and supply, and incrementally build the absorptive capacity of AT systems. This will allow sustainable services to be developed, which can genuinely meet the needs of their users.
Recommendations
The range of recommendations contained within the Statements by Member States and non-state actors provide a guide as to the multiple, concurrent and urgent actions required to progress access to AT globally.
A synthesis of these Statements suggests the following key actions are needed:
Including AT as an essential health product to be covered under UHC is one of the most effective ways of improving access.
An innovative and global response to deployment of AT through a reorientation, from isolated interventions to an integrated, sustainable and systemic approach;
Coordination of national and local policies and practices across multiple sectors to provide high quality and affordable assistive products and services that meet diverse and changing needs;
Consensus on the role of AT in global efforts in improving population health outcomes and strengthening health systems
Limitations
Limitations of this study relate to the sample and context from which it is drawn. In this case, nation states and non-state actors who attended, or were represented, at the WHA and who wished to publicly respond to the Resolution. We are aware that AT is also considered important in education, employment, social services, leisure and justice, among other areas. Thus people in those fields may have a different perspective on the relationship between AT and health from those expressed in the context of the WHA. Statements in response to resolutions commonly repeat or stress the content of a resolution. It is therefore difficult to draw any conclusions based on similarities between the resolution and the responses. To manage this limitation, we have not quantified the frequency of responses, but rather provided illustrative examples with a particular interest in those statements that went beyond the content of the resolution and reflected the particular perspectives that participants wished to draw attention to.
Conclusion
Many people live with disability and an unmet need for AT. Additionally, global trends towards ageing societies and the increasing prevalence of non-communicable diseases indicates growing demand from populations who require AT to fill the capability gap, between function and participation. Inclusion of AT as a pillar of affordable public health provision, will protect the world’s most vulnerable from catastrophic health expenditures, and provide renewed opportunities to those trapped in cycles of poverty to realise more productive, independent, and dignified lives. Together with the Resolution itself, Statements made at the 71st WHA highlight a sense of urgency in addressing this need. This paper demonstrates the perceived intersection of the health, human rights and the sustainable development agendas among those voices heard at the WHA; and the need for international collaboration and support on AT to complement other efforts seeking to tackle global inequalities.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Notes
References
- World Health Assembly. Resolution on improving access to assistive technology. 71st WHA; 2018.
- United Nations. Convention on the Rights of Persons with Disabilities; 2006. Available from: http://www.un.org/disabilities/convention/conventionfull.shtml.
- MacLachlan M, Scherer M. Systems thinking for assistive technology: a commentary on the GREAT summit. Disabil Rehabil Assist Technol. 2018;13(5):492–496.
- Khasnabis C, Mirza Z, MacLachlan M. Opening the GATE to inclusion for people with disabilities. Lancet. 2015;386(10010):2229–2230.
- Rimmer J, Chen M-D, Hsieh K. A conceptual model for identifying, preventing, and managing secondary conditions in people with disabilities. Phys Ther. 2011;91(12):1728–1739.
- World Health Organization. Towards access 2030. WHO Medicines and Health Products Programme Strategic Framework 2016–2030. 2017. Available from: https://www.who.int/medicines/publications/towards_access2030/en/
- Tebbutt E, Brodmann R, Borg J, et al. Assistive products and the Sustainable Development Goals (SDGs). Global Health. 2016;12(1):1–6.
- World Health Organization. World health report. Health Systems Financing. The path to universal coverage. 2010. Available from: https://www.who.int/whr/2010/en/
- United Nations. Disability and Development Report. 2019. Available from: https://issuu.com/unpublications/docs/2019_disability_report
- Borg J, Lindstrom A, Larsson S. Assistive technology in developing countries: national and international responsibilities to implement the Convention on the Rights of Persons with Disabilities. Lancet. 2009;374(9704):1863–1865.
- Borg J, Lindström A, Larsson S. Assistive technology in developing countries: a review from the perspective of the Convention on the Rights of Persons with Disabilities. Prosthet Orthot Int. 2011;35(1):20–29.
- Borg J, Östergren P-O. Users’ perspectives on the provision of assistive technologies in Bangladesh: awareness, providers, costs and barriers. Disabil Rehabil Assist Technol. 2015;10(4):301–308.
- World Health Organization. Priority assistive products list. Geneva: WHO; 2016.
- MacLachlan M, McVeigh J, Cooke M, et al. Intersections between systems thinking and market shaping for assistive technology: the SMART (Systems-Market for Assistive and Related Technologies) Thinking Matrix. IJERPH. 2018;15(12):2627.
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.