Abstract
Purpose
Patients in the chronic phase after stroke often lack the possibility to intensively train their upper limb function. Assistive devices can be a solution to training intensively at home. This qualitative study investigated stroke survivors’ experiences regarding training using the hoMEcare aRm rehabiLItatioN (MERLIN) system, an assistive device and telecare platform. We investigated patients’ perspectives regarding the home-based training with the MERLIN system, on the International Classification of Functioning, Disability and Health (ICF) domains and the facilitators and barriers of the MERLIN system.
Methods
Eleven patients in the chronic phase of stroke who completed the MERLIN trial took part in semi-structured interviews. Interviews were analysed using the framework method.
Results
Participants were in general positive about the device and the training. Several experienced positive effects on ICF body functions, such as joint range of motion and self-confidence. Some experienced improvements in activities, but not on participation level. Home training had advantages: flexibility in training time and duration and no need to travel. The major barriers were technical hard- and software issues and ergonomic complaints. A list of recommendations regarding assistive devices and home-based rehabilitation was created.
Conclusions
Homebased training using an assistive device was well received by stroke patients to train their upper limb function. Future device developers should take patients’ feedback into account to overcome the barriers related to the introduction of new assistive devices at home. Our recommendations may be the first step to implementing patients’ perspectives during the early stages of device development.
Training at home was a well-received and convenient solution to improve the upper limb function
Barriers regarding hard- and software and device ergonomics need to be addressed in future assistive devices
Recommendations are provided for more successful implementation of assistive devices and home-based telerehabilitation programs
Implications for rehabilitation
Introduction
Stroke can have a major impact on someone’s life. Multiple cognitive and physical problems are commonly seen in stroke patients, such as problems with concentrating, walking or using the upper limb. In rehabilitation centres most time is spent on improving walking, the upper limb is often undertreated [Citation1]. According to a qualitative study among stroke survivors, arm function seems to be neglected during the critical time window during rehabilitation [Citation1]. This imbalance may result in many patients having remaining problems using the arm or hand in daily life. After the first six months post-stroke, there are often minimal opportunities for further training [Citation2]. Other factors such as travel time, travel costs or lack of transportation towards the facility may also be a burden to continue training.
To pursue training on an intensive level, home programs can be a solution. By means of home training, patients can increase the amount of training time. Assistive devices are often used to provide training programs at home, such as electro-stimulation in combination with exercises, orthoses, joysticks or spring systems [Citation3–8]. These devices have the advantage of guiding and monitoring the patient's movements. The use of assistive devices makes it possible to train for more hours in comparison to supervised training [Citation9]. Another great advantage of assistive devices is enhanced engagement due to fun and challenging exercises. Home training can especially be useful during the chronic phase of stroke since patients are only reimbursed for a limited number of training sessions per year due to limited resources of the current healthcare system, as is e.g. the case in the Netherlands. It is generally known that much repetition is necessary to achieve functional recovery [Citation10]. Repeatedly performing the same movement can be demotivating and may lead to boredom. Stroke survivors emphasise that it is difficult to adhere to performing exercises daily if the training is not interesting [Citation1]. Gaming for rehabilitation purposes is therefore a useful addition to assistive devices in the patients’ homes.
The International Classification of Functioning, Disability and Health (ICF) is often used to investigate the effect of training on function, activity and participation levels [Citation11]. While qualitative studies often focus on the improvement of body functions [Citation12], less information is available on whether the training also has an impact on the patient’s activity or participation level. A qualitative approach can reveal the experiences and perspectives of the patients regarding changes in ICF levels, as also their opinions on the rehabilitation program and the feasibility of device usage at home. External and personal factors are often not taken into consideration and they are especially important when training at home.
This study investigates stroke survivors’ experiences with training their upper limb function at home with hoMEcare aRm rehabiLItatioN (MERLIN), an assistive device combined with a telecare platform and serious gaming [Citation13]. The aims of this study were to 1) investigate the experiences and perspectives of chronic stroke survivors on ICF levels (body functions, activities and participation) and ICF factors (external and personal) after using MERLIN to train the upper limb function at home; 2) describe the facilitators and barriers regarding upper limb training at home using MERLIN.
Materials and methods
A qualitative approach with individual semi-structured in-depth interviews was used. Methods and results were reported using the Consolidated Criteria for Reporting Qualitative Research criteria (COREQ) [Citation14].
Participants
Participants taking part in the current study were patients who were enrolled in the Dutch MERLIN trial [Citation13]. Inclusion criteria for the MERLIN trial were: aged over 18 years; the first incidence of stroke; between six months and three years post-stroke; unilateral paresis with a Fugl-Meyer Assessment-Upper Extremity score below 50 points, the ability to perform finger extension three times and some proximal voluntary movement capability in the arm; ability to speak and understand Dutch or English. For extensive in- and exclusion criteria, see [Citation13].
Participants were recruited through the Center for Rehabilitation of the University Medical Center Groningen (UMCG) and “Revalidatie Friesland” in the Netherlands. All 11 participants who completed the training in the MERLIN trial were invited via phone to participate in the interviews. A sample size of 10 is likely to be sufficient to obtain the most important and notable topics using semi-structured interviews [Citation15].
Ethics statement and informed consent
Prior to inclusion, written informed consent was obtained from all participants. The study was approved by the Medical Ethics Committee of the University Medical Center Groningen (METc UMCG 2019/189) and registered in the Dutch Trial Registry (NTR: NL7535). Participants were informed that the qualitative research was performed as part of the research education of the interviewers and they had no ulterior motives or conflicts of interest.
Intervention
The intervention consisted of training with an upper limb non-actuated robotic assistive device (ArmAssist) in the patient’s home setting, supported by a telecare platform (Antari Homecare platform, GMV) [Citation16,Citation17]. The combination of the ArmAssist and Antari Homecare platform formed the MERLIN system . The ArmAssist was used to train the upper limb function using serious games. The device did not contain motors and did not impose movement on the participant. The ArmAssist was coupled to the Antari Homecare platform, which provided a way to; 1) monitor and evaluate the treatment, 2) communicate between patient and therapist and 3) collect biomechanical training data [Citation17]. Multiple games were available to stimulate motivation and enjoyment. The intervention consisted of six weeks of training, with a minimum of three hours per week, divided into four to seven training sessions per week. There was a notable variation in total training time with a range between 5.5 and 32.8 h, evidently, not all participants achieved the desired training time per week. A significant and clinically relevant improvement in arm impairment and arm function was found after training with MERLIN for six weeks [Citation13]. Improvement in the impairment level was measured using the Fugl-Meyer Assessment – Upper Extremity and showed a significant improvement of 6.8 points between baseline and the end of the training period. The upper limb function, assessed using the Action Research Arm Test, improved significantly with 4.4 points between the start of the training and the end of the training. The Wolf Motor Function Test showed a significant improvement of 5.0 points between baseline and the end of the training. For more information regarding the quantitative results, we refer to Rozevink and colleagues [Citation13].
Figure 1. HoMEcare aRm rehabiLItatioN (MERLIN) device.

Interviewers and data coders
The first interviewer (AHS) was a female resident at the Department of Rehabilitation Medicine of the UMCG. AHS had experience in patient care, but no prior practice in qualitative interviewing. Therefore, pilot interviews were conducted and evaluated by experienced qualitative researchers CKvdS and JMH for fine-tuning the interview skills. The second interviewer (KAH, see acknowledgments) was a male master's student (Human Movement Sciences, University of Groningen), who also had no experience in qualitative interviewing. For optimal consistency, one pilot interview and three interviews of the study were conducted with both interviewers present. SGR was a Ph.D. student at the Department of Rehabilitation Medicine and conducted the coding together with AHS. SGR was not present at the interviews but was involved in the quantitative part of the MERLIN trial.
Assessments
Participants’ background information was obtained at inclusion. Interviews were conducted within three weeks after the cessation of the training. The first four interviews were conducted by the first author (AHS) face-to-face at the participant’s home. Of the remaining seven interviews (conducted by KAH), the last four were conducted by phone due to COVID-19 pandemic restrictions.
Interviews and data collection
The interview guide with semi-structured questions was based on several themes. Patients were asked about their experiences and perceptions regarding ICF levels of body functions, activities, participation and personal and environmental factors in relation to the intervention. Furthermore, patients’ opinions regarding the facilitators and barriers of the training system MERLIN, the telerehabilitation platform and the home-based rehabilitation were investigated.
Before the study started, pilot interviews were conducted with one patient in the subacute stage of stroke and one patient in the chronic stage of stroke, who did not participate in the study. Interviews were discussed by most authors (AHS, SGR, CKvdS and JMH). This resulted in some minor modifications in the interview guide regarding the formulation of questions and the order of the questions.
Prior to the interview, participants were informed about the purpose of the study and were encouraged to be as truthful as possible. The interview contained open-ended, non-directive questions and the participants were stimulated to elaborate or to raise other issues if they felt that was of importance. During two interviews, the partner of the participant was also present. The interviews were digitally recorded, and field notes were taken. Ad verbatim transcriptions of the interviews were sent to the participants for comments and corrections. No follow-up interview was conducted.
Data analysis
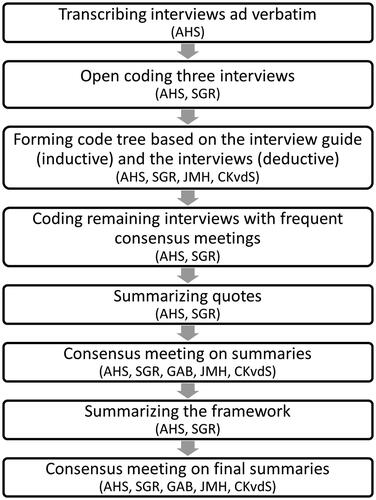
Data analysis took place according to the framework method [Citation18, Citation19]. All interviews were analysed using Atlas.ti software (Scientific Software Development GmbH, version 8.4.5 for Windows or Mac). The data analysis process consisted of eight phases as shown in the flow chart ().
Figure 2. Flow chart of the data analysis process.
Results
Twelve participants were included in the MERLIN trial (), but one patient had to terminate the study after three weeks due to discomfort with the assistive device and poor health. The remaining eleven participants were interviewed for the current study.
Table 1. Participant characteristics (n = 11).
The average duration (±standard deviation) of the interviews was 56 (±33) minutes. Physical interviews took longer (70 ± 33 min) compared to interviews over the phone (33 ± 10 min). In retrospect, data saturation was reached after the tenth interview. None of the participants provided feedback regarding the content of the interviews.
Body functions
Most participants experienced improvements in shoulder function, dexterity, elbow extension and wrist rotation. Participants reported the training had a positive influence on hand oedema. Negative effects of training were temporary muscle pain, pain complaints in the neck or arm due to a wrong posture or painful pressure points on the skin due to the device. Participants did not experience any effects on spasticity. Sensory disorders did not seem to affect participation in the training.
“Well, you have more control over the hand. That is one thing that is sure.” (P5)
Some participants found the training cognitively challenging and experienced an improvement in their memory during the games. The training did not influence their mood, although participants indicated that they felt more emotional after their stroke. When the training did not go according to plan, the participants responded emotionally. Other participants felt proud that they were able to do this training and that they experienced improvement. Two patients looked more positively towards themselves due to this proudness. Some participants felt courageous and self-confident because of the possibility of improvement in arm function. This did not apply to everyone, others did not experience any difference in self-confidence or courage. Due to their stroke, participants were limited in their daily energy and, in combination with the training program, this led to exhaustion in some cases. Stress was experienced in a few participants because MERLIN interfered with their daily routines. These patients felt relieved as soon as the program was finished.
“In the way that I improved somewhat. I am happy that I did it [the training], that I took this opportunity” (P4)
Activities and participation
Due to the MERLIN training, some participants were more triggered to use their arms during activities. Some participants took the opportunity to try new activities with their affected hands. Other participants did not notice a difference in their daily activities. No changes in participation level were noticed.
“Yes, easier. Just to name something. Putting away a cookie or coffee or, yes all kinds of daily activities, that are important. You notice you are getting better.” (P2)
“[…] that I more easily could press something between my arm [and body] to carry it home after grocery shopping.” (P9)
Personal factors
Participants acknowledged their limitations and tried to be as independent as possible. In general, they tended to be creative in finding solutions, but they asked for assistance if they needed it. Most participants were very motivated to improve their upper limb function during this trial, but also during previous rehabilitation therapy. They indicated that the drive to improve themselves made them less likely to cheat during the training. Participants mentioned that humour and perseverance were helpful character traits to improve as much as possible. A lack of intrinsic motivation in participants was considered a factor that increased strain on the relationship with the caregiver/partner.
“Yes, you accept that you can’t do as much as you did before. And besides you don’t have a choice, but you try to speed things up as much as you can, to keep improving.” (P2)
“I experienced that if it doesn’t work the first time and I focus really hard, than I succeed. That is just persevering.” (P3)
Environmental factors
The majority of the participants experienced mental support from their environment and enjoyed showing the device and serious games to family and friends. Most of the participants were able to carry out the training independently. Several participants needed assistance from a caregiver, for example, to position their arm in the device, for technical support and for motivation. Because of technical issues, most participants needed support from the investigators at some point during the intervention. With this support, the vast majority of the participants had no major set-backs during the training, even those who had little previous experience with handling computer systems.
“I couldn’t get into it [the device] myself. So then you already need help with that.” (P1)
Training system MERLIN
Facilitators
In general, participants were positive about the training. All participants stated that they would have continued the training if that would have been a possibility.
“It was a pity that it [the training] was over. I also asked if I could have him [MERLIN] for another few weeks, because it is an adequate tool.” (P2)
In comparison to training without an assistive device, participants found MERLIN more stimulating. Important factors for this opinion were the variation in games and the increasing difficulty of the games. Even participants who had experienced more trouble using the device said they would recommend this therapy to other patients. Participants agreed that the software was easy to understand.
Most participants were positive regarding the assistive device, they thought the device was not too complicated and user-friendly. While some participants had problems with the adjustability, others thought these were fine. Training using the device was fun and they thought it was an ingenious device.
“I said jokingly: are the occupational therapists now going on a strike because their job is gone? Well that won’t be the case, but just to say. Because it is a very pleasant device and it just works.” (P2)
The games were in general well perceived, but mixed responses regarding the variation were received. There was a limited variety of words or pictures in the games which were unsatisfying for a few participants. Some participants perceived this as useful because they could focus more on the movement. Other participants thought there was enough variation in the both easy and more difficult games. Games with a cognitive component were liked the most. It was appreciated that the games were simple and easy to understand. Participants without computer knowledge were also able to understand and play the games. Participants liked that they could score points in the game, that was a good stimulus to persevere.
“It were just, well I thought it were just normal fun games to play. Let’s say it this way, it were not the most intelligent games, but well.” (P9)
Barriers
Some aspects of the assistive device were not satisfactory according to the participants. The shape of the device was too big and too high. Some participants had trouble sitting in a correct ergonomic position. During the training, the hand sometimes slipped out of the orthosis that was attached to the device, which was perceived as frustrating. For some patients, it took a lot of time to position the arm and hand into the device. This was partly due to the hand grip which was often too large or too small and could not be adjusted properly to the participant’s hand size. This could result in painful pressure points on the hand.
“I thought it [the training device] was too high. The device itself. I always sat with my arm held up high and I thought that was very unpleasant. It also limited my [arm] function.” (P3)
For a few participants, MERLIN had some malfunctions: the game was blocked or the computer froze, and the participant could not continue the training. Sometimes the calibration was wrong which resulted in movements that were impossible to execute. Due to computational errors, the progression could not always be updated in the overview on the participant’s computer. Furthermore, there was a lot of wear on the device due to intensive use. Screws would fall out, wheels were hampered, and the rotation arc was affected by wear. Minor incidents were the charging pin that fell into the device and the placemat being damaged on one occasion. The Velcro straps to keep the arm in place were too short for some people.
“But because of the rotation, I had the same screw falling off all the time.” (P4)
Some games were not variable enough, which was perceived as annoying for some participants, because it led to too much repetition. Participants mentioned that they thought more games could be added for more variation. Some participants found the games with a cognitive component too challenging. The formulation of the instructions was not always clear, as such the participants did not know immediately what was expected from them. The small letters on the screen made the instruction even more difficult to read.
“You could play six games. But it was often one game one time, one game two times and one game three times. That would go on for the whole week. At some point you have seen it all.” (P1)
The feedback on the MERLIN device was used to create general recommendations for future rehabilitation assistive devices ().
Table 2. Important topics and recommendations regarding rehabilitation assistive devices.
Telerehabilitation platform
Facilitators and barriers
Via the telerehabilitation platform, it was possible for the investigators to monitor the training sessions and communicate with the participants. In general, the participants did not mind that someone was monitoring them. For some, the idea that the investigator received the data via the telerehabilitation platform was actually motivating. A few participants felt a psychological strain due to the monitoring of the researcher. Also, the intensity of the training interfered with their normal daily routine. Receiving information via chats through the chat function was considered convenient. Some participants found it inconvenient to use the chat function on the telerehabilitation platform to send messages back. They preferred calling or e-mailing the investigator with questions. The display was positioned too far away for convenient typing and was difficult to handle with one impaired arm.
“Well, I think it [a therapist monitoring the training] adds five to ten percent extra motivation. Yes it makes a difference.” (P1)
“But that [training too little] happened now and again. Then S. [investigator] would say, you haven’t trained much. Then I would feel guilty.” (P3)
Homebased training
Facilitators
Generally, the participants were positive about the home-based telerehabilitation program. The main benefits were the ability to be in control of their own training schedule and to be able to divide the training into shorter training sessions. Participants were enthusiastic about the flexibility to train whenever it was most feasible for them. If necessary, they were able to skip training and catch up at another moment. Also, it provided the opportunity to train spontaneously if they had no other obligations.
Furthermore, it was considered very time efficient since there was no travel time or wait time before therapy. The absence of travel was extra beneficial in case of long travel distances and when individuals were dependent on others for outdoor transport. Participants did not miss peer support during the home-based training. They were used to training individually during previously followed physiotherapy.
“It was a bit exhausting. And then I split it in half and then it was fine.” (P8)
“Yes because you can sit behind it [the training device] yourself. You don’t have to wait for anyone else.” (P5)
Barriers
At the beginning of the training period, participants had to get used to the hard- and software. A few participants experienced psychological pressure due to the physical presence of the system in their homes. Also, it was not always possible to receive direct assistance in case of technical issues. Furthermore, some needed assistance from their relatives to operate the system. Lastly, because there was no direct therapist supervision, it was tempting to cheat in the range of motion or to skip training, especially when participants were busy or had unexpected visitors. Also, training with the assistance of the partner appeared to be a source of frustration.
“But that [the flexibility] is also a danger. You tend, if an unexpected appointment pops up, to skip the training and that yeah. You need to have a backbone for that.” (P3)
Some participants or caregivers advised that the rehabilitation system should be placed in a rehabilitation centre and not at home, because it would be easier to overcome issues with the soft- and hardware, and could prevent friction between a participant and caregiver.
The feedback on homebased rehabilitation was used to create general recommendations for future home-based training programs ().
Table 3. Important topics and recommendations regarding home-based (tele)rehabilitation.
Discussion
The stroke survivors expressed a generally positive attitude towards home-based telerehabilitation with an assistive device for training the upper limb function. According to the participants, the training resulted in improvements in body function level, minor improvements in activity level and no improvements in participation level. From the data, facilitators and barriers regarding assistive devices and home rehabilitation were extracted. Important topics that should be taken into account when developing future devices and home training programs were summarised.
Experiences related to ICF levels
Participants experienced some improvement in arm- or hand function and self-confidence. However, this only translated to a small extent to experiencing improvements in activities but not participation. Most recovery in the upper limb function occurs in the first three to six months after the stroke [Citation20]. Although more recent evidence shows that improvement in upper limb function in the chronic phase after stroke is possible, the improvement is still limited [Citation2]. Furthermore, our participants have lived with one impaired arm for quite some time. The behaviour of learned non-use of the arm may be more difficult to overcome in the chronic stage after stroke [Citation21]. Therefore, an improvement in activities and participation may have been more difficult to be perceived by our patient group. Patients in the subacute phase of stroke may experience more improvement in ICF levels. The duration of the treatment, six weeks of at least three hours per week training, might also have been too short to induce changes in functionality.
Even though participants experienced limited improvement in activities and participation, several participants reported an increase in use of the affected arm. The forced use of the affected arm during the training may have resulted in increased awareness and therefore more use in daily life. The interviews were taken shortly after the termination of the training, it is therefore not known if this increased awareness continued to be a long-term effect.
Some participants experienced an increase in self-confidence, because of the challenges they overcame during the intervention and the improvement they independently achieved. This can be seen as an important by-product of the training and may be exploited more in future training programs. In contrast to what Cherry et al. found, no effect was reported on social participation and emotional well-being [Citation22], perhaps because included participants did not live in remote areas. Most of them still followed general fitness therapy or participated in social or cultural groups.
Experiences related to the assistive device
Participants generally enjoyed using the assistive device and playing the games. They found it easy to use and thought other stroke survivors could benefit from it too. In contrast to our expectations, the participants thought that also digitally illiterate stroke survivors would be capable to use the device after brief instructions. Future devices should however pay more attention to ergonomic factors, Neibling et al. described it as an important factor to improve the perseverance of training [Citation23]. Certain parts of the device should be adjustable to ensure an optimal fit for different sizes of arms, hands and the participants’ heights. The durability of the device and the well-functioning of the software appeared to be important, especially in a home-based setting because there are no experts present to instantly solve problems or malfunction of the device.
Experiences related to the telerehabilitation platform
The ability of the researcher to monitor the training sessions through the platform provided for some participants an extra stimulant to persevere in the training. Monitoring the training also provided the additional benefit of precise knowledge about progression in the past training sessions. Targeted questions regarding why the participant did not train or skipped a game on a certain day, may lead to valuable information of potential motivational or behavioural problems that complicate training. Remarkably, participants did not consider the monitoring an invasion of their privacy. However, there were also people who felt pressured because of the monitoring. In the future, agreements can be made with participants to decide on the training time and content and how often and in what way the therapist will provide feedback about goal achievement to tailor the training even more to the individuals’ needs. Besides the inconvenient chat function, participants had little to say about the telerehabilitation platform. Likely because most of the software was intended for the therapist and not visible to the participant.
Experiences related to homebased rehabilitation
In line with previous research regarding home-based rehabilitation, participants were positive about the convenience of training at home [Citation22]. They especially appreciated the sense of control over the timing, duration and difficulty of the training. On the other hand, some patients were unable to adhere to the training protocol. Intrinsic motivation was found to play an important role in success, in accordance with a recent review [Citation24]. It, therefore, seems that patients that have the high intrinsic motivation to train, are most eligible to profit from the freedom that is provided by home-based training. Some participants needed a lot of guidance and help from their relatives and might therefore gain more from training in a rehabilitation facility. In contrast to previous qualitative research [Citation12, Citation22], we found that in some cases the home-based training caused strain on the relationship with the partner. The researcher observed that this was mostly the case in participants with cognitive or motivational problems. Patients who have less intrinsic motivation or more cognitive problems may benefit more from extra guidance provided by physical therapy appointments or more intensive guidance through a telerehabilitation platform. Future research could investigate which other patient characteristics are of influence on home-based rehabilitation and could therefore be used as eligibility criteria.
Even though it may seem that this home-based therapy could replace a therapist, participants were missing intensive guidance during the first training sessions [Citation12]. Even when the participants became more comfortable with the device and software, they occasionally needed assistance with software and hardware problems. Furthermore, to ensure that the training remains challenging, the device had to be calibrated which required additional visits. This essential step is advised to be performed with or monitored by an experienced therapist [Citation25]. Using this type of training in addition to infrequent face-to-face therapy would be most beneficial. Furthermore, the cost-effectivity of the MERLIN treatment should be investigated. If it is possible to develop a sustainable device with low production costs, it could be an interesting cost-effective alternative to face-to-face training with a therapist.
Facilitators and barriers to persevere in training
For any home-based training, facilitators and barriers can be distinguished, which contribute to perseverance and successful implementation of the training. In a review by Neibling et al., the authors formed a conceptional framework with three stages that contribute to perseverance in technology-facilitated home-based upper limb practice, namely: 1) getting in the game; 2) sticking with it and 3) continuing or moving on [Citation23].
Stage 1) “Getting in the game” is described as the usability and acceptability of the technology. In accordance with the review, the participants in our study agreed that more attention should be paid to the ergonomics and robustness of the assistive device to improve its usability. In the review, it was stated that the usability of the device is increased with sufficient support from a therapist or relative. As we have reported, some relationships were not suitable for providing such support, since the training caused strain on the relationship. Another discrepancy was the opinion regarding telerehabilitation for elderly and digitally illiterate persons, which influences the acceptability of the device. While according to the review elderly and digitally illiterate would have problems using assistive devices, our participants did not agree with this and thought everybody would be able to use the MERLIN system.
Stage 2) “Sticking with it” is described as staying engaged and integrating practice into daily life. The lack of social interaction was considered a bottleneck for sticking with the therapy. However, our participants did not experience any lack of social interaction. For the participants in our study, the main challenge was to fit practice into daily life which is also considered an important factor for perseverance. The participants were able to determine when and how they wanted to train. Future studies may provide some better guidelines to enhance therapy compliance; let the participants choose their training moments and stick to a preplanned schedule.
Stage 3) “Continuing” with the training was in this case not possible due to the end of the trial. All participants in our study wanted to continue the training if that would have been a possibility. The optimal balance between training frequency and duration and adherence to the training schedule might be an interesting topic to investigate.
Strengths and limitations
This qualitative research showed stroke survivors’ experiences with home use of an assistive device in combination with a telerehabilitation platform. The interviews of 11 participants provided rich data, with a broad perspective. Interestingly, the total training time varied greatly among participants with a range between 5.5 and 32.8 h. This may have led to differences in the patients’ perspectives on the training. The training had a favourable effect on the upper limb function of the patients, this might have influenced their opinions and might have resulted in more positive feedback.
Unfortunately, we were unable to avoid a selection bias in our sample. Although we approached around 60 patients for the MERLIN trial [Citation13], probably only motivated patients responded to our invitation to participate. Therefore, the motivation among patients might have been higher compared to the general population of stroke survivors. Another limitation was that two different interviewers conducted the interviews, therefore there may have been some differences in the way questions were asked. To minimalize these differences, an interview guide was used, and the two interviewers performed the first few interviews together. Also, we were forced to conduct some interviews by phone due to the COVID-19 pandemic. According to the literature, this does not decrease the quality of the interviews [Citation26]. Because of cognitive problems or aphasia, some participants had difficulties expressing themselves. A relative was therefore present to support the participant during the interviews. Furthermore, the software was updated during the trial and as a consequence participants who were included later reported fewer software problems.
Recommendations/future research
Although most of the participants’ recommendations regarding home-based training of the upper limb with an assistive rehabilitation device have previously been reported in the literature, these findings do not seem to have been adopted by engineers sufficiently. Recurrent themes are: device ergonomics, hard- and software malfunction, degree of support from a relative and therapist and engagement [Citation12, Citation24, Citation25, Citation27–29]. Although the participants in this study enjoyed the current training, there is room for improvement. For future research, it is essential to learn why this valuable information does not reach the developers, or why the suggestions are not incorporated into the new devices and training programs. In our opinion, future (home-based) assistive devices should be developed in a co-creation process with the different stakeholders (e.g., patients, therapists and healthcare insurance) and should take into account all the lessons we have learned so far about the implementation of new medical devices in the home situation. Our results can contribute to several implementation issues and facilitate the usage of new assistive technology.
Conclusion
Homebased therapy to improve upper limb function in stroke survivors has promising advantages such as more training time, training at own pace and at preferred times. Participants experienced some improvement in their arm/hand function, which occasionally translated to an improvement in activities. The MERLIN system and telerehabilitation platform were well received by the participants, although there were some major points of improvement. A list of recommendations was provided to guide researchers and engineers for future assistive devices and training programs for home-based telerehabilitation. Co-creation between all stakeholders and developers seems the best way forward to overcome the current barriers in telerehabilitation training. Lessons learned from the implementation of assistive technology in the home situation should be taken into account when developing new devices.
Consent for publication
The picture of a man training was made for marketing purposes and is not a participant in the study.
Author contributions
AHS, SGR, JMH and CKvdS designed the study. AHS contributed to the interviews. AHS, SGR, JMH, GAB, CKvdS performed the data analysis. AHS, SGR, JMH, CKvdS, GAB contributed to writing the manuscript. All authors read and approved the final manuscript.
Acknowledgements
We thank all participants for their efforts in this study. We would like to thank K.A. Horstink (KAH) for his help in conducting the interviews. Special thanks to A. M. Boonstra for her critical thinking at the start of this study.
Disclosure statement
The authors declare that there is no conflict of interest.
Data availability statement
Data will be made available upon request via DataverseNL. To protect the privacy of the participants, it is not possible to fully anonymize the transcript of the interviews and therefore we publish the data with restricted access. The coding tree will be published with open access. DataverseNL: https://doi.org/10.34894/MBABRA.
Additional information
Funding
References
- Barker RN, Brauer SG. Upper limb recovery after stroke: the stroke survivors’ perspective. Disabil Rehabil. 2005;27(20):1213–1223.
- Teasell R, Mehta S, Pereira S, et al. Time to rethink long-term rehabilitation management of stroke patients. Top Stroke Rehabil. 2012;19(6):457–462.
- Kim GJ, Otr L, Rivera L, et al. Combined clinic-home approach for upper limb robotic therapy after stroke: a pilot study. Arch Phys Med Rehabil. 2015;96(12):2243–2248.
- Alon G, Sunnerhagen KS, Geurts ACHH, et al. A home-based, self-administered stimulation program to improve selected hand functions of chronic stroke. NRE. 2003;18(3):215–225.
- Nijenhuis SM, Prange GB, Amirabdollahian F, et al. Feasibility study into self-administered training at home using an arm and hand device with motivational gaming environment in chronic stroke training at home using an arm and hand. J Neuroeng Rehabil. 2015;12:1–12.
- Wittmann F, Held JP, Lambercy O, et al. Self-directed arm therapy at home after stroke with a sensor-based virtual reality training system. J Neuroeng Rehabil. 2016;13:1–10.
- Chen J, Nichols D, Brokaw EB, et al. Home-based therapy after stroke using the hand spring operated movement enhancer (HandSOME). IEEE Trans Neural Syst Rehabil Eng. 2017;25(12):2305–2312.
- Reinkensmeyer DJ, Pang CT, Nessler JA, et al. Web-based telerehabilitation for the upper extremity after stroke. IEEE Trans Neural Syst Rehabil Eng. 2002;10(2):102–108.
- Masiero S, Armani M, Ferlini G. Randomized trial of a robotic assistive device for the upper extremity during early inpatient stroke rehabilitation; 2014. https://doi.org/10.1177/1545968313513073.
- Kwakkel G, Kollen B, Lindeman E. Understanding the pattern of functional recovery after stroke: facts and theories. Restor Neurol Neurosci. 2004;22(3-5):281–299.
- World Health Organization. International classification of functioning, disability and health (ICF). 10th revis. Geneva: World Health Organization; 2011.
- Chen Y, Chen Y, Zheng K, et al. A qualitative study on user acceptance of a home-based stroke telerehabilitation system. Top Stroke Rehabil. 2020;27(2):81–92.
- Rozevink SG, van der Sluis CK, Garzo A, et al. hoMEcare aRm rehabiLItatioN (MERLIN): telerehabilitation using an unactuated device based on serious games improves the upper limb function in chronic stroke. J NeuroEngineering Rehabil. 2021;18(1):12.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357.
- Weller SC, Vickers B, Russell Bernard H, et al. Open-ended interview questions and saturation. PLOS One. 2018;13(6):e0198606–18.
- Proxima medical technology. ArmAssist. Website 2020. http://armassist.eu/.
- GMV. Antari Homecare n.d. https://www.gmv.com/en/Products/antari_ehealth_epidemiology_solutions/antari_home_care/.
- Friese S. Qualitative data analysis with ATLAS.ti. Londen, England: Sage; 2019.
- Gale NK, Heath G, Cameron E, et al. S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117–111.
- Kwakkel G, Van Peppen R, Wagenaar RC, et al. Effects of augmented exercise therapy time after stroke – a meta-analysis. Stroke. 2004;35(11):2529–2539.
- Taub E, Miller NE, Novack TA, et al. Technique to improve chronic motor deficit after stroke. Arch Phys Med Rehabil. 1993;74(4):347–354.
- Cherry COB, Chumbler NR, Richards K, et al. Expanding stroke telerehabilitation services to rural veterans: a qualitative study on patient experiences using the robotic stroke therapy delivery and monitoring system program. Disabil Rehabil Assist Technol. 2017;12(1):21–27.
- Neibling BA, Jackson SM, Hayward KS, et al. Perseverance with technology-facilitated home-based upper limb practice after stroke: a systematic mixed studies review. J Neuroeng Rehabil. 2021;18:1–26.
- Chen Y, Abel KT, Janecek JT, et al. Home-based technologies for stroke rehabilitation: a systematic review. Int J Med Inform. 2019;123:11–22.
- Linder SM, Reiss A, Buchanan S, et al. Incorporating robotic-assisted telerehabilitation in a home program to improve arm function following stroke: a case study. J Neurol Phys Ther. 2013;37:125–132.
- Novick G. Is there a bias against telephone interviews in qualitative research? Res Nurs Heal. 2008;31:391–398.
- Tyagi S, Lim DSY, Ho WHH, et al. Acceptance of tele-rehabilitation by stroke patients: perceived barriers and facilitators. Arch Phys Med Rehabil. 2018;99:2472–2477.e2.
- Niknejad N, Ismail W, Bahari M, et al. Understanding telerehabilitation technology to evaluate stakeholders’ adoption of telerehabilitation services: a systematic literature review and directions for further research. Arch Phys Med Rehabil. 2021;102:1390–1403.
- Jayasree-Krishnan V, Ghosh S, Palumbo A, et al. Developing a framework for designing and deploying technology-assisted rehabilitation after stroke: a qualitative study. Am J Phys Med Rehabil. 2021;100:774–779.
