Abstract
Purpose
The purpose of the study was to investigate whether the sustained use of the "Hug," a "hugging" type robotic transfer support device, could increase the level of quality of care.
Methods
The effect of proficiency on using the device was examined in terms of time spent for transfer, ratio of transfers using the device, and range of targets. The results were compared between skilled care facilities that had used the device for >24 months and unskilled facilities.
Results
The time spent for transfer at the unskilled facility was 4.6 min (2nd week after introduction), was reduced to 3.0 min (5th week), and 1.5 min at the skilled facility. The usage ratio at the unskilled facility was 13% and 30% (2nd and 5th week, respectively), while it was 97% in the skilled facility. Further, we identified wider in the range of target care recipients in the skilled facility.
Conclusion
It takes time to master the use of Hug; however, its use was associated with many positive aspects, especially from the perspective of care recipients, e.g., better care, use of their own legs, and reduced time for transfers. These findings suggest that the widespread use of Hug would improve the quality of care.
Less physically burdened on the caregivers using Hug, they can afford to talk to the care recipients.
Using recipient’s own legs during transfers, it prevents leg muscle disuse.
As reduced time for transfers, recipients will have more opportunities to get out of bed.
IMPLICATIONS FOR REHABILITATION
Background
With the super-aging society and shortage of caregivers in recent years, it is necessary to reduce the burden on caregivers and improve the quality of long-term care. The introduction of nursing care-support devices using robotic technology is an effective way to solve this problem [Citation1]. Various long-term care robotic support devices have been developed and are beginning to become available on the market [Citation2]. For example, some exoskeleton type robots are using for care support, such as Hybrid Assistive Limb® (HAL®) assists a caregiver’s movements by sensing their muscle activities [Citation3], and the Muscle Suit provides assistance to a caregiver’s body such as when lifting/transferring a person or an object [Citation4].
In long-term care facilities in the United Kingdom, a floor-moving hoist has been introduced as a necessary device by the Health and Safety Executive [Citation5], and in the United States, the Occupational Safety and Health Administration has established guidelines for the use of lifting devices for occupational safety reasons [Citation6]. However, in Japan, the introduction of such devices has been delayed because there are no strict guidelines defining which situations they should be used in. According to a 2014 survey in Japan, only 14.7% of long-term care facilities had introduced floor-moving lifts or ceiling-mounted lifts, and only 20% of these facilities used them on a daily basis [Citation7]. Other reasons for their delayed introduction include the associated cost and complexity of applying for subsidies from the Japanese long-term care insurance system [Citation8]. In addition, it has been reported that nursing care worker training schools in Japan do not provide sufficient education on the use of nursing care assistive devices [Citation9]. Under these circumstances, it is necessary to conduct detailed research on the use of lift-type devices, how to identify care recipients who would benefit from their use, and the effects of these devices on care recipients and caregivers after their introduction.
In our previous research, we focussed on a robotic lifting device named “Hug” (, Hug T1-01; Fuji Corporation, Aichi, Japan). We reported that the heart rate of caregivers was decreased and communication with care recipients was increased during transfer-support using Hug in a facility that had been using the device for more than 24 months, i.e., a skilled facility [Citation10]. Hug is a battery-powered mechanical lifting device that inserts a soft robotic arm under each armpit of a care recipient, as shown in , from the front and lifts them in a “hugging” motion while they hold on to handles on the device [Citation11]. The constant use of Hug enabled caregivers to perform their tasks more efficiently and improved the quality of life (QOL) of care recipients due to increased verbal communication when using the device [Citation10]. However, the impact of Hug in a facility in which it was newly introduced was not investigated.
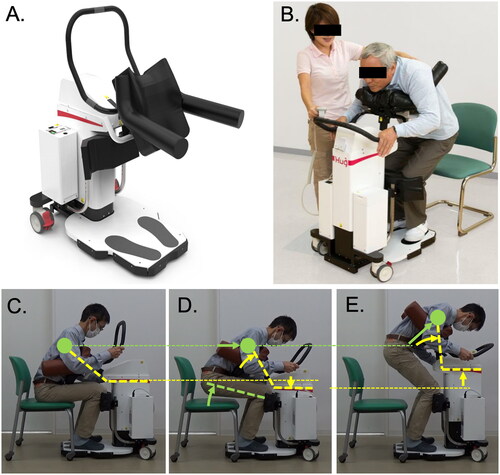
Figure 1. Photographs of the transfer support device “Hug” and its mechanism of action. Photographs of Hug (A) and an example of the use of Hug (B). After placing the care recipient in the correct position (C), pressing the “Stand up” button moves the centre of gravity of the care recipient’s chest (closed green circles) horizontally and also raises their buttocks (D). Next, the robotic arms rotate and the shaft rises further, causing the care recipient to stand up (E). The angle of the robotic arms is shown by yellow lines, the green lines show the movement of the care recipient, and the thin broken lines show the horizontal level. The images in A and B were kindly provided by Fuji Corporation with permission for use in publications.
Hypotheses and objectives
We considered that it would be difficult to detect the significant benefits of nursing care robots on caregivers’ work efficiency in the early stages of their introduction. However, as a result of the continuous use of care robots, their effect on reducing the burden on caregivers would become apparent as the level of proficiency in their care protocols increased. Therefore, in the present study, we compared a long-term care facility that had used Hug daily for >24 months with two facilities in which the device was newly introduced. We hypothesized that increased skill on Hug would result in the following outcomes: (1) a reduction in the time required to perform transfer assistance; (2) a reduction in the number of caregivers required to perform transfers; and (3) an expansion in the range of care recipients who would benefit from the use of Hug. The objective of this study was to show how this device affected care protocols in nursing homes by the level of proficiency. To show the difference in proficiency of using the device, we conducted an interventional study in three phases consisting of 3 weeks each to identify the changes in the proficiency levels of caregivers at an unskilled facility, differences between the skilled and unskilled facilities, and discussed how to select and assess target care recipients.
Methods
Mechanism and action of Hug
The movement mechanism and protocol of Hug usage are shown as the yellow drawings in ; the green drawings show the movement of the body of care recipient. The main shaft including the robot arms and thoracoabdominal support pad (the black pad between the two arms in ) can be moved up and down by simply pressing the “Plus/Minus” buttons to adjust height. The robot arms are inserted under the armpits of the care recipient, and by pressing the other “Stand up” button, the centre of gravity of the chest and abdomen is moved forward horizontally (). Note that it uses a two-axis motor that lowers the main shaft as the arm rotates, shifting the centre of gravity of the caregiver’s chest horizontally instead of vertically (closed green circles). As the chest moves horizontally, the buttocks rise up with the knees as the fulcrum (). The care recipient is “hugged” by the device and, as the robot arms rotate and the shaft rises further, starts to stand up (). They can then be moved to a suitable location, and by simply pressing the “Sit down” button, the protocol is reversed and the transfer is completed.
Study overview
The spread of Hug has generally been very slow in Japanese long-term care facilities, but some facilities are using this device frequently and sustainably. In other words, there are some reasons to prevent the use of robotic care devices. Therefore, we planned a study at the stage when caregivers are becoming familiar with the use of Hug to identify an efficient method to introduce this device into care facilities. We contacted facilities that had not used Hug as unskilled facilities, as well as skilled facilities that had been using Hug for >24 months on a daily basis, which were identified from the literature [Citation12,Citation13]. Due to our research budget and time limitations, three facilities (one skilled and two unskilled facilities) participated in this study. The study was carried out using a questionnaire and an observational time-motion study (details below). To assess the proficient use of Hug, as shown in Supplementary figure 1, the study period was set at 9 weeks (1 phase = 3 weeks; 3 phases), and the numbers of transfer and toileting assists were recorded for 1 week (in the middle of each phase). A time study was conducted by selecting a normal day on which no special events (e.g., ceremonies or seasonal parties) were held at the facilities during the middle week of each phase. The robot was introduced to the unskilled facilities in the second phase, and we observed the process of mastery. That is, the unskilled facilities did not use Hug during the first phase as the baseline. In the skilled facility, we collected results over the three phases in two measurement periods. In each measurement period, one skilled and one unskilled facility participated, respectively. The skilled facilities in Measurement Periods 1 and 2 were the same but these were independent units. Thus, in total, three facilities participated in this study.
Subjects
Measurement Period 1 (August–October 2019): Five full-time caregivers including certified care workers and care helpers and two care recipients in the unskilled facilities and four full-time caregivers and three care recipients in the skilled facility participated in the study. After the study purpose and observational procedures were explained, all participants signed informed consent forms (approved by the Ethics and Conflicts of Interest Committee of the National Centre for Geriatrics and Gerontology). If a participant could not sign the form, it was signed by a caregiver or family member. The capacity of the care units at all facilities was 18 people. In the skilled facility, one Hug was used for three care recipients (two males/one female, age 77 ± 13 years) in the unit; however, we introduced two Hugs to the unskilled facilities for the personal use of two care recipients (two females, age 85 ± 3 years).
Measurement Period 2 (November 2019–January 2020): Eight full-time caregivers and two care recipients in the unskilled facilities and seven caregivers and three care recipients in the skilled facility (a different unit to that assessed in Measurement Period 1) participated in the study. After explaining the study procedure, all participants signed informed consent forms as described above. The capacity of the care units at the unskilled facilities was 44 people and that at the skilled facility was 18 people. Similar to Measurement Period 1, in the skilled facility, one Hug was used for three care recipients (two males/one female, age 86 ± 6 years), and we introduced two Hug devices to the unskilled facilities for the personal use of two care recipients (two females, both aged >90 years). The results of Measurement Period 2 were used only for the identification of target cases.
The subject inclusion criterion was a person who could provide informed consent after receiving an explanation of the study. Care recipients were excluded from the study if they weighed 100 kg or more; however, there are no defined standards for the use of Hug by caregivers and care recipients. The numbers of subjects who were approached and consented (in parentheses) to participate in the study were as follows: Measurement Period 1: skilled facility unit 1, caregivers 5 (5) and care recipients 3 (3); unskilled facility, caregivers 4 (4) and care recipients 3 (2), and Measurement Period 2: skilled facility unit 2, caregivers 8 (8) and care recipients 3 (3); unskilled facility, caregivers 7 (7) and care recipients 3 (2). The caregivers only used Hug on the care recipients who had consented to participate in the study.
Japanese scale for representing the physical and cognitive levels of care recipients
In order to develop an assessment method that can be used as a guide for selecting users (care recipients) of this device, we collected information about the physical and cognitive levels of the care recipients using Hug. Although this scale is unique to Japan, the respective grades for disability and cognition are shown in Supplementary tables 1 and 2, respectively. These scales are not diagnostic tests, but rather indicate the level of independence in daily living. This scale is widespread in Japan because it allows professionals such as public health nurses, nurses, and care workers to make objective and rapid level judgments.
Observation protocol
To investigate the reduction in time for providing transfer assistance, a 1-min time study (hereafter referred to as the time study) was used. The time study was widely used to assess the workload, and a systematic review assessing the impact of patient transfers on nurse workload with time study was published [Citation14]. The time study was similar to an observational study that was reported previously as a time-motion study [Citation15], in which all caregivers were observed directly. In brief, a professional observer, following a caregiver throughout the daytime shift, analysed the tasks and recorded them using codes that were based on the code chart used in the Ministry of Health, Labour, and Welfare, Survey of Long-term Care in Japan [Citation16], which has been translated into English and is available as supplementary materials in our previous study of the proficiency of exoskeleton usage in nursing care facilities [Citation17]. Note that in the present study, care code 222: Transfer was subdivided into 22201: Verbal action for transfer, 22202: Actual assistance, and 22203: Watching after transfer in order to examine the transfer situations in more detail.
Care records
To investigate the reduction in the number of caregivers required to perform transfers, the caregivers were asked to fill out a separate form indicating the number of times they provided assistance with transfers and toileting care and the number of people involved during the middle week of each phase.
Assessment (target care recipient case)
To produce an assessment method to identify individuals who could benefit from the use of Hug, the sex, age, weight, and level of disability and cognition levels of the care recipients were recorded. We also assessed the activities of daily living (ADL) on a three-point scale (). Regarding disability and cognitive levels, we used a grade unique to Japan as explained above, and the classification is shown in Supplementary tables 1 and 2.
Table 1. Information about the target care recipients of Hug.
Questionnaire
The questionnaire for caregivers obtained information on their sex, caregiving history, qualifications, ranges of age, body height and weight as shown in Supplementary figure 3. They were also asked to rate on a four-point scale (Agree/Agree somewhat/Disagree somewhat/Disagree) whether using Hug daily reduced their physical and mental burden and increased their communication with the care recipient compared to when not using Hug. The questions were: (A) “Was physical burden reduced by the use of Hug?” (B) “Did you have sufficient mental capacity when performing transfers using Hug?” and (C) “Was communication with the care recipient increased by the use of Hug?” as shown in the questionnaire sheet 3-1. Prior to the introduction of Hug to the unskilled facilities, the questions were changed to (A) “Do you expect that the use of Hug will reduce physical burden?” (B) “Do you expect to have sufficient mental capacity when performing transfers using Hug?” and (C) “Do you expect that communication with the care recipient will be increased by the use of Hug?” as shown in Supplementary figure 4. We have usually used questionnaire similar to these in our study, but this is the first time we have presented the questionnaire sheet in English.
Important points when performing transfers using Hug
A series of important points for using Hug were identified in discussions with the caregivers and manufacturer’s technicians and also our experiences of its use in physiotherapy along with its mechanisms (Supplementary figure 2). It was a design concept of Hug that the centre of gravity of the chest and abdomen is moved forward in a horizontal direction, raising the hips with the knees as the fulcrum at the same time.
Treatment fidelity
We evaluated the treatment fidelity according to a previous study [Citation18]
Treatment design
Under an interventional study, we provided information about treatment design at a meeting with the manager of each nursing care facility. We asked the caregivers to use Hug as many times as possible in their daily nursing care schedule.
Training
When we introduced Hug to the unskilled facilities, we invited a trainer from the manufacturer to the facility who trained the manager and several caregivers to use Hug for 1 h, practicing with each other. Then, we asked the caregivers to consent to take part in the study. We asked the caregivers to show the Hug device to the care recipients and ask them if they would be willing to use it. On a separate day, we visited the facility to ask the care recipients to sign the consent document.
Delivery and receipt of treatment
To check the delivery and receipt of treatment in the intervention period, one member of our study group visited each facility once a week to assess transfer assistance using Hug.
Enactment of treatment skills
The improvement of skill using Hug appeared as a decreased number of caregivers and shorter time required for transfer assistance. These were recorded as quantitative results.
Results
Quantitative results (time study and care records) from Measurement Period 1
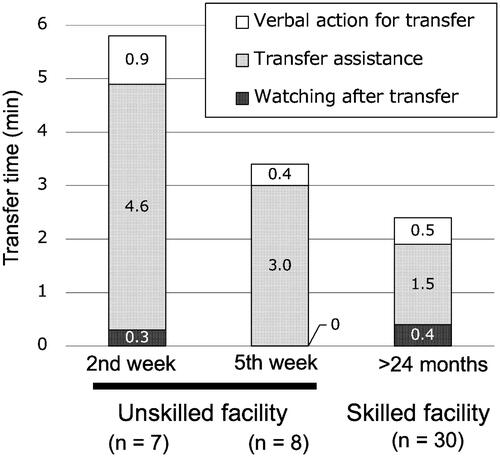
In order to investigate quantitatively the changes associated with proficiency when using Hug, the time required for transfers was measured by a time study (). As a result, the transfer time at the unskilled facility, which was 4.6 min on average (n = 7, standard deviation (SD) = 3.0) in the second week after its introduction, was reduced to 3.0 min on average (n = 8, SD = 2.1) in the fifth week. Conversely, transfer time was 1.5 min on average of Phase 3 (n = 30, SD = 1.1) at the skilled facility; therefore, we believe that it will be further reduced in the unskilled facility as proficiency with using Hug is increased. Regarding the time for preparing and cleaning the device, it took approximately 0.4 min to perform each in the skilled facility because the device was placed in a corridor. However, in the unskilled facility, much less time was spent on both because Hug was used on an individual basis. This is an unusual situation, but if these devices are installed for home care, it could be a merit.
Figure 2. Time involved in transfers using Hug during the development of proficiency after its introduction. The transfer time using Hug at the unskilled facility, which was 4.6 min on average in the second week after introduction, was reduced to 3.0 min on average in the fifth week after introduction. And the transfer time at the skilled facility was 1.5 min on average. The results were obtained from the time study performed in Measurement Period 1, as described in the Methods section.
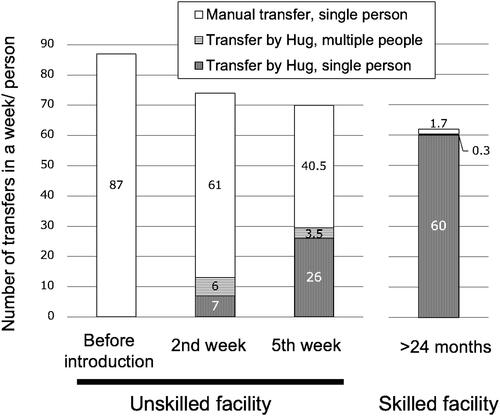
Next, the number of transfers per care recipient per week, in which the number of times Hug was used and/or involving multiple people, was counted (). In the unskilled facility, Hug was used 13 times in 1 week out of a total of 74 transfers/person. Moreover, six of these transfers were performed with multiple caregivers. The frequency of Hug use increased slowly, but even after 5 weeks of use, it did not reach 50% of transfers; however, the number of transfers with multiple assistance decreased significantly to 3.5 out of 29.5 transfers/person/week. In contrast, in the skilled facility, most transfers (60 out of 62) were performed using Hug. The results shown here were from phase 2 for 1 week, but similar results were obtained in the other phases.
Figure 3. Changes in the number of transfers with or without Hug before and after its introduction. The numbers in the unskilled facility were compared with that in the skilled facility. The frequency of Hug use in the unskilled facility increased slowly, even after 5 weeks of use, it did not reach 50% of transfers; however, the number of transfers with multiple assistance decreased significantly to 3.5 out of 29.5 transfers/person/week. In contrast, skilled facilities used Hug for most transfers. The results were obtained from Measurement Period 1.
Finally, one of the purposes of the time study was to survey the work content of the target units, but there was no change in the content or amount of work performed due to the introduction of Hug to the unskilled facility (data not shown).
Quantitative results (questionnaire) from Measurement Period 1
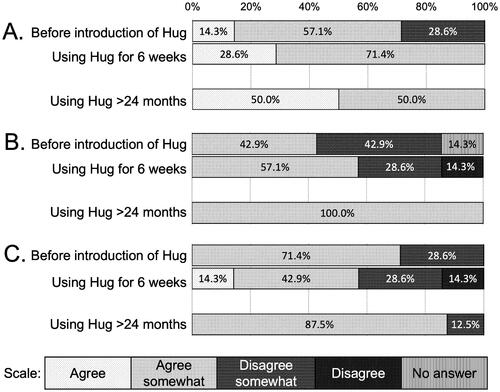
The effects of using Hug on the physical and mental burdens of caregivers were assessed using a questionnaire. As a result, all eight caregivers working in the skilled facility answered positively to the question “Was physical burden reduced by the use of Hug?” In the unskilled facilities, 61% of caregivers answered positively with Agree/Agree somewhat before its introduction, but this changed to 100% after using Hug for 6 weeks (). In the case of mental burden, all eight caregivers working in the skilled facility answered positively to the question “Did you have sufficient mental capacity when performing transfers using Hug?” In the unskilled facilities, 43% of caregivers answered positively to this question with Agree/Agree somewhat before the introduction of Hug, but this changed to 57% after using it for 6 weeks (). Additionally, in response to the question “Was communication with the care recipient increased by the use of Hug?” 88% of caregivers at the skilled facility gave a positive answer of “Agree somewhat,” and one caregiver (14%) in one of the unskilled facilities answered “agree” after using Hug for 6 weeks (). The questionnaire used in the measurement has been translated to English and is attached as Supplementary figures 3 & 4.
Figure 4. Results of the questionnaire before and after the introduction of Hug. Comparing the results at the unskilled facility (before introduction and using Hug for 6 weeks) and at the skilled facility (using Hug >24 months). Questions: (A) “Was physical burden reduced by the use of Hug?” (B) “Did you have sufficient mental capacity when performing transfers using Hug?” and (C) “Was communication with the care recipient increased by the use of Hug?” In the case before the introduction of Hug to the unskilled facilities, the questions were changed to A, “Do you expect that the use of Hug will reduce physical burden?” B, “Do you expect to have sufficient mental capacity when performing transfers using Hug?” and C, “Do you expect that communication with the care recipient will be increased by the use of Hug?” Questionnaire forms are attached as Supplementary figures 3 & 4.
Assessment of target cases for Hug from Measurement Periods 1 & 2
As shown in , regarding the level of disability (the criteria for the determination of the daily life independence level [bedridden level] of older adult subjects with disability are described in Supplementary table 1) of the 10 subjects who used Hug in this study, various grades were observed (A, B, and C), but three out of six people with grade B were almost bedridden. The levels of cognition (the criteria for the determination of the daily life independence level of older adult subjects with dementia are described in Supplementary table 2) were IIb and IIIa, indicating that Hug can be used for care recipients with a certain level of cognitive impairment. In the assessment in terms of weight, although the major weight class was 40–50 kg, five target subjects weighed >50 kg, who were used to assess the use of Hug for older adults who are relatively heavier than normal.
Regarding the ADL level of the care recipients, there were three who could not be raised into a sitting position on the bed; however, Hug could still be used for transfers with these individuals. Most recipients were able to maintain a sitting position, but were generally unable to stand upright and walk. The results were different for each individual regarding their ability to maintain a sitting position, to express the need for bowel or bladder evacuations, to perform postural changes, and to use the nurse call button (“Nurse call”).
Summary of the important points for using Hug
We have summarized the notable points for using Hug in Supplementary figure 2. The instructions in the user manual were summarized as red drawings. The most notable points for caregivers when using Hug for transfer assistance (shown as yellow circles) were that the device should be brought close to the care recipient until it is in contact with their knees (Supplementary figure 2B) and the main shaft should be moved down until the thoracoabdominal support pad lightly touches their thighs (Supplementary figure 2C) to ensure that the centre of gravity of the chest and abdomen is placed on the pad.
Discussion
Training for using Hug
In this study, we described the changes associated with increased proficiency in the use of Hug. Training is required for its efficient use, and it is important that the robot arms are inserted securely under the armpits of the care recipient and that their knees are firmly in contact with the knee pad of the device (). After that, when Hug is operated, the arms and chest of the care recipient sink automatically, and weight transfer is performed by the device. It supports the care recipient’s weight (as if they were being “hugged”) and then stands up. The caregivers in the skilled facility stated that it took at least 2 weeks to train new users before the device can be used safely to the target care recipients.
Benefit of proficiency on using Hug
Reduced time for transfers
From the quantitative results of the interventional study, the first point to note is the change in proficiency reflected by the time required to perform transfers using Hug (). In the skilled facility, it took an average of 2.4 min for a transfer due to the preparation and tidying up time required as Hug was stored outside of the care recipients’ private rooms. In most cases, a manual transfer (not using a device) takes less than 1 min, so it takes more than twice as long when using Hug. However, in a previous study, we reported that the number of vocal interactions between a caregiver and care recipient was increased by approximately 2.4 times with Hug compared to during manual transfers [Citation10]. In other words, even though it takes more time, Hug promotes communication between a caregiver and care recipient, which might lead to better care and increased QOL.
Reduced person involving the transfers
The second notable point is the change in proficiency according to the number of transfer assists performed using Hug. At 2 weeks after its introduction, Hug was not used efficiently, resulting in it being utilized in only 13 (17.6%) out of 74 transfers in the unskilled facility (). Moreover, six of these transfers required multiple caregivers, which means that the burden on the staff was clearly increased. In contrast, in the skilled facility, almost all transfer assists (97.2%, 60.3/62 transfers/person/week) were performed by a single person using Hug. As proficiency increases, Hug can be used comfortably in a short period of time, so the ratio of Hug use should be increased further in the unskilled facility.
Increased usage rate of hug for transfers
Due to the feature that Hug is hugging the care recipients, preparation time is short and it can be used easily and quickly. It reportedly takes an average of 5.5 min to perform a transfer from a bed to a chair when using an ordinary floor-type lift that requires a sling sheet [Citation19], but Hug can perform the same transfer in 2.4 min, i.e., less than half the time. According to a study examining the usage rate of ergonomic devices in Dutch facilities [Citation20], a lift was not used in 28% of transfers in nursing care facilities and in 57% of transfers in hospitals, where the use of an ergonomic device is required according to workplace guidelines. As for the reason for not using these devices, 89% of caregivers (nursing care facilities) and 93% of nurses (hospitals) said that they were not located close to the bed. In other words, if the device is easy to use and ready to use like Hug, the usage rate should be increased. As a limitation, the caregivers reported that if transfer assists were scheduled in the morning or after lunch, one Hug could only assist with transfers for 3–4 people during these busy hours.
Expanding the usage of Hug for bedridden people
The usefulness of this device is outstanding, except that the target of use is limited to bedridden individuals who can maintain a sitting position. Furthermore, by not using a sling sheet, this device can make full use of a care recipient’s own leg strength, which helps to maintain residual capacity. As the use of a muscle strength has been shown to improve health [Citation21], it may also prevent frailty and sarcopenia [Citation1].
Confirmation of the awareness of Hug’s usability
In the questionnaire, we asked caregivers about physical and mental burden and communication with the care recipient when using Hug (). As a result, the answers to all of these questions changed in a positive manner according to increased proficiency in using Hug. These changes over time suggested that the use of Hug had positive effects that were further enhanced by increased proficiency. The results show that the quality of care has improved for each proficiency level of using Hug in the nursing homes.
Notable points for using Hug
Taking time to become skilled with the use of Hug
Despite the beneficial effects associated with the introduction of Hug, there were also some notable points. The first point, as mentioned above, is that training is required before it can be used smoothly, and it takes at least 6 weeks of use to be effective. The use of a sling sheet with a normal lift can be mastered in a short period of time, but Hug is difficult to use because it does not support the care recipient from behind. When introducing Hug, it is necessary for the facility manager to secure a time and place for the caregiver to practice sufficiently. Supplementary figure 2 summarizes the important points when using Hug. Some of the steps of its use should be performed precisely and require the skill of caregivers for giving correct instructions. Two points identified in discussions with the caregivers and manufacturer’s technicians were related to the movement of the care recipient’s centre of gravity. Users at the unskilled facilities had not become proficient with these points even after 6 weeks of using Hug according to interviews. Additionally, these points can be explained clearly from the perspective of the mechanism of Hug. When standing up, Hug moves the centre of gravity of the care recipient’s chest and abdomen horizontally () using a robotic mechanism. This makes it easy and comfortable to raise the care recipient’s buttocks. Therefore, we conclude that ensuring that the care recipient’s body is lifted onto the support pad during transfers is the most important step when using Hug.
Expanding the applicable cases
The second notable point is that the range of applicable cases is narrow. For a completely bedridden care recipient, the transfer destination is a stretcher rather than a wheelchair, and Hug cannot be used if the patient is unable to maintain a sitting position. Therefore, we thought that it was necessary to characterize the target care recipients who would benefit from its introduction. By identifying applicable target persons using Japanese classification scales (criteria for older adults with disability, criteria for older adults with dementia, and activities of daily living, ADL), we identified the suitable target persons from the actual user information in . Additionally, in discussions with the staff at the skilled facility, we have compiled a target case proposal chart (). Regarding the average ADL level shown in , especially for “Sitting position” with an average score of 1.3, the ability to maintain a sitting position was the main factor for selection as a target. The average scores of 2.6 and 3.0 for “Standing up” and “Walking,” respectively, indicate the importance of care recipients being unable to perform these tasks when selecting target cases. Regarding “Standing (hold),” Hug may also be used for putting on and taking off underwear and changing diapers, so it was included in the ADL scale.
Table 2. Assessment correspondence chart for target care recipients.
How to select a target care recipient using
Overall, Hug can be introduced to a care recipient with disability grade B and for those with dementia grade IIIa or lower. In addition, if they can hold the handle of the device according to guidance, Hug can even be used for some care recipients with disability grade A2 and dementia grade IIIb or higher. Conversely, it is considered impossible or unnecessary to use Hug for a completely bedridden person or a person who can stand up stably. Additionally, we have studied the use of another transfer-support device for bedridden people that may be suitable in certain cases for improving QOL if Hug is not applicable [Citation22,Citation23].
Particular note as usable targets for transfers by Hug
Usable targets are those who can manage a sitting position, even if they are almost bedridden, such as disability grade B2 (). A target person of this grade should be transferred with multiple assistance or a floor-type lift device, but if Hug can be applied, the care recipient could be transferred with assistance from a single caregiver by using their own muscle strength. This may not only reduce the burden on the caregiver but also improve the QOL of the care recipient [Citation10]. Furthermore, an example of disability grade C (recipient ID2) in Measurement Period 1 in the skilled facility is shown in . According to the interview with the caregivers, the care recipient was almost bedridden, but he was able to hold on to Hug for a short period of time, and during that time, the caregivers were able to replace his bed pads. Similarly, in a case of disability grade A2, by using Hug after standing up, it was possible for the care recipient to maintain the same posture and have their clothes (trousers or underpants) changed. As changing clothes is also a difficult task in long-term care, it would be convenient to use Hug when performing toilet assistance. We have not mentioned toilet assistance so far, but Hug can be used to carry a care recipient a short distance to a toilet in a private room. However, as described in the instruction manual, this device is prohibited from being used for long-distance travel, such as moving from one room to another via a corridor.
Cost effectiveness
The third notable point is that it is difficult to show quantitatively the cost-effectiveness of introducing Hug. It has a higher introduction cost than an ordinary floor-type lift device, and we mentioned above that Hug can be applied to a limited range of care recipients. But efforts have been made to expand the scope of its application in the skilled facility as described in the former subsection. As a result, in the skilled facility, its operating rate was increased as one Hug was mainly used by three care recipients, and when the device was not being used, it was also used occasionally for another individual. Although there are some limitations, the effect on better care [Citation10] and the mental burden of caregivers () is apparent. We cannot evaluate these as costs, but we believe they are beneficial for management in nursing facilities.
Improved care protocols
After all, if a Hug will be installed and used proficiently at a unit in nursing home with 20 to 30 care recipients, one Hug can reduce the number of manual transfers for 3 to 4 care recipients by more than 180 times per week. This will be accomplished by proficient assessment of care recipient, optimal placement of one Hug to share, and decreasing the time for transfer by practice, resulting decreased physical burden of caregivers. The introduction of Hug should lead here, and exactly these would improve quality of care. Although it takes several months for maturing the care protocols, introducing Hug should be beneficial for long-term care facilities that have care recipients in a certain level of disability.
Comparison with similar devices
There are several devices that lifts target as “hugging” manner. A type is manual transfer support devices called “Sasaete” [Citation24] and “Ka-rukun” [Citation25]. Transferring with these devices is done with the power of the caregiver’s arms and legs. The other, "Ai-Ijo-kun," is electric and the recipients can be moved from bed to wheelchair by oneself using a remote control [Citation26]. The main difference between these devices and the Hug is that there is no horizontal shift of the centre of gravity, and the transfer is performed with a single centre of rotation. Above all, the demand for this type of device is increasing, and there is a possibility that it will spread to long-term care facilities by different protocols that compared to use the conventional sling sheet type equipment. Because when caregivers will master to use these devices, the transfers should be performed much faster than the conventional lifts.
Hug and the future
One of the most beneficial point of using Hug is its portability. In particular, ceiling lifts require reinforcement of the ceiling for installation, and ordinary lifts also have a large figure, so it is difficult to even carry them indoors. A transfer assist robot like Hug should be introduce to home care. As discussed in a literature [Citation27], the reality of the need for personal robots to lead independent living was becoming clear, and also in project [Citation28], a future in which multiple robots work together to support individual lives was proposed. Basic robots like Hug are also expected to help support individual lives by incorporating transfer assistance functions into personal robots.
New version of Hug
Finally, we would like to discuss the specifications of Hug. We used a T1-01 Hug in the present study, but this device has been updated to the T1-02 model [Citation29]. The main difference is the weight of the main body, 35 kg for T1-02 compared to 60 kg for T1-01. As the weight of the machine has been reduced, the usability and impact of the new model should be better in relation to the results reported here.
Limitations of the study
One of the limitations of the study is the relatively small number of participants, as the number of care recipients in this study was 6 in skilled facilities and 4 in unskilled facilities. This is due to the narrow range of care recipients to whom the Hug is applicable, and may require improvements, such as fall prevention, to expand the range. Another point of the limitation is that the study period at the newly introduced facility was 6 weeks after the introduction of Hug, which was a relatively short period of time. Therefore, there is little information on how long the time required for the transfer operation using the device can be sufficiently reduced.
Conclusion
We described the advantages and notable points of using the Hug, lift-type robotic device, for transfer assistance and how to select target care recipients. The proficient use of the device had many positive effects on the care protocols in nursing homes, especially from the perspective of care recipients, such as better care, improved QOL, and taking less time to perform transfers compared to a conventional lift. It takes more than several months for realizing improved quality of care but we consider it would be beneficial if Hug or similar lifting device is used widely in the near future. Along with the spread of such basic robots, it will be necessary in the future to spread personal robots that assist independent living by utilizing useful basic technologies.
Declarations
The study protocols have been reviewed and approved by the Ethics and Conflicts of Interest Committee of the National Centre for Geriatrics and Gerontology (acceptance nos. 1258 and 1293-2). All participants in these studies provided informed consent. All methods were carried out in accordance with relevant guidelines and regulations.
Clinical trials registry
The study was registered at UMIN Clinical Trials Registry [https://www.umin.ac.jp/ctr/] Nos. UMIN000039203 and UMIN000039204; registration date: January 21, 2020; interventional study; parallel, non-randomized, single blinded. All the participants of the study have given informed consent.
Author contributions
IK conceived the study. All authors designed the study. TY, KK, ST, NM, KA, and NI performed the study and data collection. TY analysed the data, prepared the figure, and KK and TY wrote the paper. All authors revised the manuscript.
Supplementary_Materials.pdf
Download PDF (561.3 KB)Acknowledgement
We thank the care staff and care recipients at Choju-no-Sato-Jushiyama (special nursing home for older adults), Flower-Search-Obu (paid nursing home for older adults), and Sawayaka-no-Oka (paid nursing home for older adults) for their cooperation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability and materials
The datasets analysed during the current study are not publicly available given that the research team has not completed its analysis, but are available from the corresponding author on reasonable request.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Kondo I. Frailty in an aging society and the applications of robots. Japanese J Comprehense Rehab Sci. 2019;10(0):47–49.
- Crume Y. Assistive Device Revolution for the Independence of Older Adults in Japan – Care Robots and Other Technology Innovations-Research Activities. 2018. International Longevity Center Japan. 2018. Available from: https://www.ilcjapan.org/studyE/index.html.
- Miura K, Kadone H, Abe T, et al. Successful use of the hybrid assistive limb for care support to reduce lumbar load in a simulated patient transfer. Asian Spine J. 2021;15(1):40–45.
- Muramatsu Y, Kobayashi H. Assessment of local muscle fatigue by NIRS - development and evaluation of muscle suit. Robomech J. 2014;(1):19.
- Health and Safety Executive, HSE [Internet]. Moving and handling equipment; [cited 2022 April 11]. Available from: https://www.hse.gov.uk/healthservices/moving-handling-equipment.htm.
- Occupational Safety and Health Administration, OSHA [Internet]. Guidelines for nursing homes: ergonomics for the prevention of musculoskeletal disorders. Publication 3182; 2003. Revised March 2009); [cited 2022 April 11]. Available from https://www.osha.gov/ergonomics
- Kakinuma T, Kakinuma T, Sekita Y. 介護老人福祉施設における人的資源運用のための高齢者雇用分析とリフト導入の効果と課題 [effects and issues of employment analysis of older adult and introduction of lifts for human resource management in nursing homes for long-term care]. Kousei-no-Shihyou. 2016;63:9–15.
- Nakamura S. Japan’s Welfare for the Elderly—Past, Present, and Future. Asia Health and Wellbeing Initiative. 2018; [cited 2022 April 11]. Available from: https://www.ahwin.org/japans-welfare-for-the-elderly-past-present-and-future/.
- Wakabayashi M, Taniguchi T. Factors interfering in the use of lifts at caretaking facilities: perspectives from education on using lifts at training institutions for certified care workers. Bulletin, Mimasaka University. 2019. p. 111–116.
- Yoshimi T, Kato K, Tsuchimoto S, et al. Increase of verbal communication by long-term use of transfer-support robots in nursing facilities. Geriatr Gerontol Int. 2021;21(2):276–277.
- Wright J. Tactile care, mechanical Hugs: Japanese caregivers and robotic lifting devices. Asian Anthropol. 2018;17(1):24–39.
- Ministry of Health, Labour and Welfare of Japan [Internet]. Report on research project to support the introduction of nursing care robots and demonstrate the effects of introduction. 2018. Japanese. Available from: https://www.mhlw.go.jp/file/06-Seisakujouhou-12300000-Roukenkyoku/1353.pdf.
- Bureau of Social Welfare and Public Health, Tokyo Metropolitan Government [Internet]. Robot nursing care device/welfare device utilization support model project, 2016–17. Japanese. Available from: https://www.fukushihoken.metro.tokyo.lg.jp/kourei/hoken/jisedaikaigo/robotmodel.html.
- Blay N, Duffield CM, Gallagher R, et al. A systematic review of time studies to assess the impact of patient transfers on nurse workload. Int J Nurs Pract. 2014;20(6):662–673.
- Qian S, Yu P, Hailey D, et al. Nursing staff work patterns in a residential aged care home: a time–motion study. Aust Health Rev. 2016;40(5):544–554.
- Ministry of Health, Labour and Welfare of Japan [Internet]. 高齢者介護実態調査ケアコード表 [Care code chart on the Survey of Long-term Care]. 2016. Japanese; [cited 2022 April 12]. Available from: https://www.mhlw.go.jp/shingi/2006/12/dl/s1206-7f.pdf.
- Kato K, Yoshimi T, Tsuchimoto S, et al. Identification of care tasks for the use of wearable transfer support robots – an observational study at nursing facilities using robots on a daily basis. BMC Health Serv Res. 2021;21(1):652.
- Borrelli B, Sepinwall D, Ernst D, et al. A new tool to assess treatment fidelity and evaluation of treatment fidelity across 10 years of health behavior research. J Consult Clin Psychol. 2005;73(5):852–860.
- Alamgir H, Li OW, Yu S, et al. Evaluation of ceiling lifts: transfer time, patient comfort and staff perceptions. Injury. 2009;40(9):987–992.
- Koppelaar E, Knibbe JJ, Miedema HS, et al. Individual and organisational determinants of use of ergonomic devices in healthcare. Occup Environ Med. 2011;68(9):659–665.
- Pratesi A, Tarantini F, Di Bari M. Skeletal muscle: an endocrine organ. Clin Cases Miner Bone Metab. 2013;10(1):11–14.
- Yoshimi T, Kato K, Aimoto K, et al. Utilization of transfer support equipment for meeting with family members in a nursing home during the COVID-19 pandemic: a case report. Geriatr Gerontol Int. 2021;21(8):741–742.
- Kato K, Yoshimi T, Aimoto K, et al. Reduction of multiple-caregiver assistance through the long-term use of a transfer support robot in a nursing facility. Assistive Technol. 2022;2022:1–8.
- Simple manual transfer lift “Sasaete ” [Internet]. Abilities Care Net Co., Ltd. Japanese; [cited 2022 April 12]. Available from: https://www.abilities.jp/fukushi_kaigo_kiki/fukusiyougu/idouyoulift/703100.
- loor-type manual transfer lift “Ka-rukun” [Internet]. Tekunoeido Kenkyuujo Co. Japanese; [cited 2022 April 12]. Available from: https://ka-rukun.com/products/.
- Simple electric transfer lift “Ai-Ijo-kun II” [Internet]. Daikei Co., Ltd. 2021. Japanese. Available from: https://www.youtube.com/watch?v=ImcrijfH0mI.
- Fiorini L, De Mul M, Fabbricotti I, et al. Assistive robots to improve the independent living of older persons: results from a needs study. Disabil Rehabil Assist Technol. 2021;16(1):92–102.
- Bevilacqua R, Felici E, Marcellini F, et al. Robot-era project: preliminary results on the system usability. In Marcus A, editor. Design, user experience, and usability: interactive experience design. Vol. 9188. Lecture notes in computer science. Cham: Springer International Publishing; 2015. pp 553–561.
- Mobility support robot “Hug T1” [Internet]. FUJI Corp. [cited 2022 April 12]. Available from: https://www.fuji.co.jp/en/about/hug/.
