 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Purpose
In virtual reality, avatar embodiment can spur perceptions and behaviours related the avatars’ characteristics. We tested whether embodying superhero-like avatars can change self-perceptions in people with chronic low back pain (CLBP).
Design
A non-blinded pilot randomized controlled trial.
Methods
Participants were randomly allocated to embody a superhero (VR-SH, n = 20) or a neutral, non-superhero (VR-Play, n = 10) avatar. Primary outcomes related to body image (e.g., self-perceived vulnerability) and pain intensity were assessed at baseline, during exposure, immediately after and at one-week follow-up. Fear of movement, strength and patient impression of change were also recorded.
Results
The VR-SH group reported gains in body image during (p < .001,=0.71) and immediately after (p < .001,
=0.66) VR, whereas the VR-Play group reported small gains during VR (p = .021,
=0.46) but not immediately after (p = .076,
=0.31). Pain, strength and fear of movement did not change and there were no sustained effects at follow-up (all ps > .05). A greater proportion of people in the VR-SH group reported at least minimal improvement at follow-up (7/20 vs. 1/10).
Conclusion
A VR-SH session produced temporary positive effects on body image. Future research may consider whether larger and sustained effects can be obtained with multisession exposures or explore combined interventions.
Physical confidence and bodily trust can be significantly enhanced in people with chronic back pain using virtual reality.
These positive body image effects may have implications for rehabilitation, such as in enhancing confidence with movement
Whether a multisession intervention might produce more robust effects and changes in pain is yet to be determined
Implications for rehabilitation
Introduction
Modern Virtual Reality (VR) enables a digital avatar to be synchronized with a user’s real body and viewed from the first person. This results in a sense of ownership and agency over the avatar, commonly termed “embodiment” [Citation1–3]. Studies support the idea that this kind of embodiment can evoke perceptions and behaviours that coincide with the avatar’s characteristics [Citation4]. For example, in one study (n = 60) participants who flew above a virtual city as a superhero subsequently displayed more helpful behaviours than those who flew in a helicopter – they were more likely to help the experimenter pick up the “accidentally” dropped stationary [Citation5]. In another study (n = 30) participants embodying an avatar of Albert Einstein, performed better in a problem solving task [Citation6]. This phenomenon has been coined the Proteus effect [Citation4] and is consistent with the apparently close relationship between mind and (perceived) body that underpins embodied cognition theory [Citation7].
Embodiment of a virtual avatar is possible, because brain-held representations of the body are continuously updated in line with multisensory and non-sensory information [Citation8]. While altered body perception can be experimentally induced, it may also be the basis of clinical disorders. For example, altered body perception has been associated with body dysmorphias [Citation9,Citation10], body integrity disorder [Citation11] and distorted phantom limbs [Citation12]. Interest has therefore grown in targeting misrepresentations of the body using VR and other sensory feedback techniques [Citation13]. For example, studies have shown that people with anorexia have more accurate body size estimations after embodying healthy-weight avatars [Citation14–17].
Pain persisting in the absence of pathology may be regarded as a condition of altered body perception [Citation8]. Beyond the pain itself, conscious impressions of the body referred to as body image may also be disrupted. Body image may include body-related attitudes, emotions and sensations, including pain. Indeed, negative body-related attitudes, such as reduced physical efficacy (i.e., low levels of perceived strength and skill [Citation18]) and impressions of the body as malfunctioning or at risk of (re)injury [Citation19,Citation20], are common findings in people with chronic low back pain (CLBP) [Citation18,Citation21]. Interestingly, some theories of pain are consistent with the idea that some aspects of body image may interact with pain itself. For example, pain is thought to relate to the implicit perception that the body is in danger [Citation19], therefore body image perceptions consistent with a vulnerable body may upregulate pain. As such, targeting vulnerability-related aspects of body image may also reduce pain.
In a recent case report, a patient with CLBP underwent a four-week VR Body Image Training (VR-BiT) intervention involving the embodiment of athletic avatars, with the goal of targeting negative self-perceptions and pain [Citation20]. Changes in self-perceptions were reported not only within sessions but appeared to lead to sustained changes following repeated sessions. This work built upon prior single-session case report data showing that a patient with LBP had reduced pain and increased perceived strength when viewing a video of their back manipulated to appear hyper-muscular [Citation22].
In order to move forward, it is important to know whether the apparent effects of VR observed in these prior case reports is unique, or whether other individuals with chronic pain may be similarly impacted. Indeed, should the effect be experienced more broadly, consideration of a clinical trial of VR-BiT may be warranted. This study aimed to explore the short-term effects of the core component of VR-BiT, the embodiment of superhero-like avatars, on people with CLBP. In particular, the effects of VR-superhero embodiment (VR-SH) relative to a control VR condition (VR-Play). We hypothesized that both groups would experience similar short-term changes in pain, because short-term analgesia would be primarily driven by a VR-based distraction effect that would be independent of group. However, we hypothesized that the VR-SH group would experience greater short-term improvements in body image dimensions such as perceptions of strength and vulnerability. Moreover, we hypothesized that secondary and exploratory outcomes such as fear of movement and muscle strength (force production), would also be enhanced by VR-SH relative to VR-Play. Finally, we hypothesized that a single session would not produce differential outcomes at one-week follow-up.
Materials and methods
Design
Twenty participants with CLBP underwent a single-session exposure to the virtual reality superhero condition (VR-SH), while a further 10 participants underwent exposure to a virtual reality play (VR-Play) control condition. Both conditions involved immersion within, and interaction with, a virtual world, but the nature of the virtual bodies and interactions were distinct. The VR-SH condition involved embodiment of athletic and superhero-like avatars, whereas the VR-Play involved embodiment of cartoon-like virtual hands. As VR is known to have analgesic effects [Citation23], the control exposure enabled us to examine the unique effects of the embodied avatars and related interactions. The study was approved by Queensland Health - Metro South Health (HREC/2019/QMS/53077) and Griffith University (2019/763) ethics committees. The protocol was registered with the Australian and New Zealand Clinical Trial Registry (ACTRN12619001776190; UTN: U1111-1240-1469). There were no significant deviations from the original protocol. However, we note that exploratory outcomes were not recorded in the published protocol. This RCT is reported following the CONSORT Statement [Citation24].
According to the VR-CORE guidelines for virtual reality in clinical research, a staged approach to investigation should be employed to prevent research waste [Citation25]. The first recommended step (VR1) is a human-centred design process, the second step (VR2) is early testing with a focus on factors such as initial indicators of clinical efficacy and feasibility, and the final step (VR3) are randomized trials comparing to control interventions. Since we were examining initial indications of potential efficacy, we considered this a VR2 study.
Participants
Participants were eligible if they were adults (>18 years of age) who had been referred to the Metro South Health Persistent Pain Management Service for the management of CLBP (duration at least six months), scored at least “moderate” on Question 7 (“How much bodily pain have you had during the past 4 weeks?”), and Question 8 (“During the past 4 weeks, how much did pain interfere with your normal work [including both work outside the home and housework]?”) of the SF-36 [Citation26], were able to read and understand the English language, had access to a computer, and were able to provide informed consent. Participants were excluded if they had a diagnosis of, or the presence of red flags, indicating serious spinal pathology (i.e., infection, tumour, recent fracture, significant structural deformity, such as unstable/unstabilized spondylolisthesis or progressive scoliosis, inflammatory disorder, and neuropathic radicular syndrome or cauda equina syndrome). They were also excluded if they had an inability to tolerate visual stimulation (e.g., susceptibility to migraines aggravated by light) or inability to tolerate the head mounted display (e.g., sensitivity to touch around the face and head). Recruitment and data collected occurred at the Metro South Health Persistent Pain Management Service in the period between 5 October 2020 and 1 April 2021.
As a single-session study, we did not aim to establish efficacy. Rather, we aimed to explore whether the short-term effect of VR-SH exposure seen in our early work [Citation20] was generalisable to a larger cohort, in order to explore the potential value of future research. Our early work [Citation20] and pilot work suggested that embodiment of superhero-like avatars was likely to produce very large and immediate effects on body image. Since samples of 10 per arm are sufficient and appropriate for exploratory studies where very large effect sizes are expected (Cohen’s ds ≥ 0.8) [Citation27], a sample size of 30 was targeted. An asymmetrical allocation ratio was designed to suit the needs of a parallel qualitative study focussed on participant experience of the VR-SH exposure, where we estimated that up to 20 participants would be required to reach saturation. While symmetrical groups would have been ideal, we also had to consider budget and time constraints.
Allocation and blinding
A concealed allocation approach was used, where participants were allocated to the VR-SH of VR-Play group with a 2:1 ratio. The random allocation sequence was generated using Microsoft excel by an experimenter not involved in data collection. The allocation of participants 1–30 were then recorded on dark, non-transparent cards and inserted into opaque envelopes that were numbered consecutively. The researcher facilitating the exposure was not blinded to group. While blinding of participants was not possible, they were “masked” to the existence of a second group. This assisted to prevent “information bias” that might arise from perceiving the lesser (or greater) of two interventions. The outcome measures were self-reported by the participants.
Equipment and software
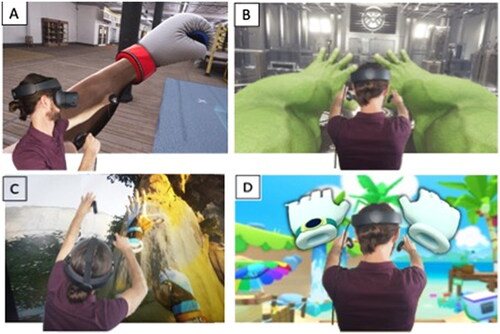
The VR was delivered via an Oculus Rift S head mounted display with connected Touch controllers (Oculus, Facebook Technologies, LCC, Menlo Park, USA) and a Windows computer (Alienware 17 R4, with NVIDIA GTX1080 GPU, Dell Technologies inc., Round Rox, Texas, USA). Four applications, all available on the Oculus store, were used. For VR-SH, the applications allowed the participant to embody a boxer (Creed: Rise to Glory), a superhero (The Avengers Powers Unite) and a rock climber (The Climb) (see ). For the VR-Play exposure, the application (Vacation Simulator) allowed embodiment of a cartoon-like character (). The hardware and software afforded six degrees of freedom for head and hand movement. Creed: Rise to Glory and The Avengers Powers Unite included full-body avatars, that were animated in response to head and hand tracking and “best guess” algorithms. This allowed dynamic full-body avatars without the need for full-body motion capture. This approach resulted in excellent synchronization of the avatar to the participants upper body. While the synchronization of the avatar to the lower body was to a lower degree, the interactions primarily involved the upper body, and the lower body was only visualized when standing still.
Figure 1. Visualization of the VR applications. Panel A: “Creed: Rise to Glory”; Panel B: “Avengers Powers Unite”; Panel C “The Climb”; Panel D “Vacation Simulator”.
Exposure details
To ensure participants understood the VR exposure, which may be a prerequisite to proper engagement with it, a short explainer video was shown. The videos also served to standardize information provision (See VR-SH: https://youtu.be/YnSs3SxwnYg and VR-Play: https://youtu.be/7UH9d6TdI_o). A more detailed explanation about pain was avoided, in order to focus the study on VR, rather than education.
VR-Superhero exposure
VR-SH involved embodiment of three characters: a muscular boxer, a super hero and a rock climber (). The Boxing Avatar: After facilitating embodiment of the avatar by encouraging participants to observe and move their body, participants were instructed to make “muscle poses” and perform “boxing actions”. Participants then further interacted with a virtual boxing bag. The Incredible Hulk Avatar: After facilitating embodiment of the avatar by encouraging participants to observe and move their body, participants were again instructed to make “muscle poses” and perform “boxing actions”. Participants were then led to do activities such as lifting and throwing “heavy” virtual objects and create “earth quakes” using the characters special powers. Rock Climbing Avatar: After facilitating embodiment of the avatar’s virtual hands by encouraging participants to observe and move their hands, participants were instructed to scale a virtual cliff by reaching, grasping, and pulling on hand-holds in the cliff face. Since this avatar did not include a full body, this activity was viewed as embodying the capability (more so than both the capability and physical structure) of the athletic avatar.
Patients opted to perform these tasks in standing or sitting, depending on their standing and sitting tolerance and personal preference. Where the activity was performed in sitting, the full-body avatars still appeared in standing. The experimenter facilitating the exposure was a physiotherapist with expertise in chronic pain and VR. The three experiences took approximately 6-min each, and were completed in a single session with 5-min intervals between embodiments. At the beginning of each experience the experimenter instructed on operation of the hand controls and facilitated avatar embodiment by encouraging the user to move and observe their virtual body.
VR-Play exposure
Participants in the VR-Play group engaged with an interactive 3 D environment, but without a physically enhanced virtual body. The single clinic-based session involved the application “Vacation Simulator”, for 18 min (in three blocks of 6 min, separated by 5-min intervals). Participants explored three scenarios: building a virtual sand castle, standing waste deep in the sea and playing at a virtual beach, and cooking a virtual barbecue at the beach.
Outcomes
Demographic and descriptive data
Prior to the experiment, a patient interview was conducted to gather demographic and clinical data (such as age, sex, duration of pain). The participant then completed a digital questionnaire (LimeSurvey online survey tool [Citation28]), to gather additional clinical and psychological data.
Primary outcomes: body image and pain intensity
Body image and pain intensity were assessed at baseline, during the exposure, immediately after the exposure, and at one-week follow-up. During and immediately after exposure assessments were considered the primary outcome timepoints, and the one-week follow-up assessments were considered a secondary timepoint. The body image assessment scales matched those used previously [Citation20] and assessed four dimensions of body image. For each body image scale, the participant was asked “Using the following scale, rate how your body feels (not how it might actually be)” using a 0-10 NRS. The four rating scales related to self-perceived strength, vulnerability, agility and confidence with activity. The four ratings were averaged to calculate the overall “body image score” used in analyses. Current pain and average pain over the past week were measured using a 11-point numerical pain rating scale (0: no pain; 10: worst imaginable pain). Numerical rating scales are comparable to other pain assessments (such as visual analogue scales) [Citation29] and was chosen as the method of choice as it was able to be administered verbally during VR exposure.
Secondary outcomes: embodiment, fear, force production, global change
To assess the strength of embodiment we used a modified version of the embodiment questionnaire designed to quantify body ownership during the rubber hand illusion [Citation1]. This questionnaire indexed the strength of illusory embodiment with a focus on user perceptions of agency and ownership over the avatars. Specifically, the questionnaire asked participants to rate their agreement with the following statements using a one to three agreement scale where, where 1 = disagree, 2 = somewhat agree, and 3 = strongly agree: During the task it felt as though: 1. when looking at the virtual body I was looking at my own body, 2. the virtual body was my body, 3. the virtual body was under my control, 4. the virtual body moved when I moved. The scale was administered verbally during each of the three avatar experiences. The score was then added across the four ratings, with a maximum score of 12. Scores were then converted to a percentage of the maximum. For descriptive analysis, scores were also calculated for the first two and second two ratings to index “ownership” and “agency” aspects of the embodiment experience respectively.
The short electronic version of the Photograph Series of Daily Activities (PHODA-SeV) scale [Citation30] was used to index perceived harmfulness of activity before and after the experience. This tool uses 40 pictures of tasks such as lifting, bending, turning, reaching and falling. Participants digitally drag-and-drop these pictures along a visual scale ranging from 0 (“not harmful at all”) to 100 (“extremely harmful”) according to their own situation. An average score is calculated across all pictures. A hand grip dynamometer (Lafayette, USA) was used to index peak force production in kilograms before, during, and after VR. Force production was assessed at baseline, and at 5-min in to each of the three 6-min experiences (and averaged across the three experiences in each condition), and immediately after VR.
While the exposure was only a single session, and not formulated as a clinical intervention, we nonetheless included a measure of self-reported clinical change. Overall perceived change was measured using the Patient Global Impression of Change scale (PGIC) [Citation31]. The PGIC is a seven-point scale with descriptors anchored to each point (1: Very much improved, 2: Much improved; 3: Minimally improved; 4: No change; 5: Minimally worse; 6: Much worse; 7: Very much worse). Typically, ratings of at least “Much improved” are considered to denote meaningful change [Citation31], however, these changes can typically be achieved over several rather than one treatment session. As such, we considered scores of 1 to 3 as meaningful improvements, and planned to contrast the numbers of participants reaching this criterion between conditions. PGIC was assessed at one-week follow-up using the digital (LimeSurvey) questionnaire.
Statistical analysis
Prior to analysis, data were checked for normality using the Shapiro–Wilk test, and the eyeball test and skewness and kurtosis. Additionally, Mauchly’s test of sphericity was used to see if the variances of the differences between all combinations of related groups were equal. Where the assumption of sphericity was violated during ANOVA tests, Greenhouse–Geisser corrected values were adopted.
The immediate and one-week follow-up effects on body image were analysed via Mixed design ANOVAs with one groups factor (Group with two levels: VR-SH vs. VR-Play) and one repeated-measure (Time with four levels: baseline, during, immediately after and one-week follow-up). Planned comparisons (LSD) were conducted for the primary timepoints (during and immediately after vs. baseline) and for the secondary timepoint (one-week follow-up vs. baseline). Current pain was compared within sessions, while average pain over the last week was compared between baseline and one-week follow-up. As such, within-session effects on the primary outcome “current pain” were assessed using a mixed design ANOVA (Group: VR-SH vs. VR-Play; Time: baseline, during and immediately after). Planned comparisons (LSD) were conducted for these primary timepoints (during and immediately after vs. baseline). One-week follow-up effects on “Average pain over the last week” were assessed using a mixed design ANOVA (Group: VR-SH vs. VR-Play; Time: baseline and one-week follow-up). Effect size was assessed with respect to absolute mean differences and partial eta squared (), interpreted according to Cohen’s guidelines (0.01: small, 0.059: medium and 0.138: large) [Citation32]. For all tests, alpha was set at p = .05. When comparing groups, we focussed on comparison of mean differences and effect size, rather than significance thresholds of test findings. The main reason for avoiding comparison on the basis of significance, was that the asymmetric group size resulted in greater statistical power for tests involving the VR-SH group.
Change in maximum force production was analysed via a mixed design ANOVA (Group: VR-SH vs. VR-Play; Time: baseline, during and immediately after). Change in perceived harmfulness of activity was assessed via a mixed design ANOVA (Group: VR-SH vs. VR-Play; Time: Baseline and Immediately after). To assess equivalence of the strength embodiment during VR between conditions, the four 0–10 ratings of the strength of the sense of ownership and agency over the avatar were converted a percentage score and subject to an independent samples t-test.
Results
All 30 participants completed the exposure. There was no missing data for the primary outcome timepoints. One participant from each group was lost to follow-up (one due to poor health, the other was unable to be contacted) and a last observation carried forward approach was used to preserve statistical power for the related secondary analyses. Participant descriptive data are detailed in . Independent t-tests confirmed that both groups experienced a similar degree of embodiment of the avatars in each condition (Mean(SD) VR-SH = 76(18)%, VR-Play = 73(22)%, t(28, 15.6) = 0.52, p = .61). The subscores of the embodiment scale were also similar (Ownership: VR-SH = 61(29)%, VR-Play = 57(34)%; Agency: VR-SH = 92(10)%, VR-Play = 88(14)%. Notably, it is typical for agency scores to be higher than ownership scores [Citation33].
Table 1. Descriptive data for both groups.
Body image
With respect to body image scores, there was a main effect of time (F(3, 83) = 18.83, p < .001, = 0.40 and an interaction between time and group (F(3, 84) = 3.03, p = .034,
= 0.10) (see , left panel). Pairwise contrasts within each group revealed that during and immediately after the exposure, body image scores were significantly different to baseline in the VR-SH group (p < .001,
= 0.71 and p < .001,
= 0.66, respectively). Scores at one-week follow-up were not different to baseline (p = .832,
=0.00). In the VR-Play condition, body image scores were improved during VR but not immediately after or at one-week follow-up (p = .021,
=0.46, p = .076,
=0.31 and p = .41,
=0.08, respectively).
Figure 2. Mean (95%CI) for the body image ratings (left panels) and pain ratings (right panels) at baseline, during VR, immediately after VR and at one-week follow-up for both interventions. For pain intensity rating data, grey triangles denote “average pain intensity over the last week” and black circles denote “current pain intensity”.
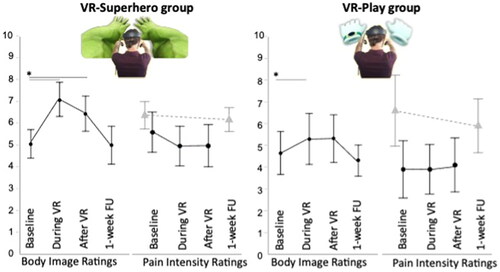
Pain intensity
For the within-session data, there was no effect of time (F(1.6, 44.81)=1.26, p < .29, =0.043 and no interaction between time and group (F(1.6, 44.81)=1.66, p = .13,
=0.074) (see , right panel). Greenhouse–Geisser corrected values are reported due to violation of the sphericity assumption. For the secondary one-week follow-up timepoint, there was also no effect of time F(1, 28)=3.07, p = .09,
=0.099) and no interaction with group (F(1, 28)=0.957, p = .34,
=0.033).
Force production
There was no effect of time (F(1.38, 38.73) = 0.15, p = .77, =0.005)) and no interaction with group (F(1.38, 38.73) = 0.14, p = .25,
= 0.048) with respect to maximum grip strength during VR or immediately after VR relative to baseline. Greenhouse–Geisser corrected values are given due to violation of the sphericity assumption.
Fear of movement
Due to technical issues with the PHODA-SeV, fear-of-movement data could only be included from 16 participants of the 30 participants. Nonetheless, we proceeded with the planned ANOVA and found no effect of time (F(1,14) = 1.38, p = .26, = 0.090) and no interaction with group (F(1, 14) = 2.62, p = .128,
= 0.158).
Global change
Of the 28 people who responded to follow-up, 8 reported being at least minimally improved and 1 reported being minimally worse. In the VR-SH group, 37% reported being at least minimally improved, 55% of people reported no change and 5% of people reported being minimally worse. In the VR-Play condition, 11% of people reported being at least minimally improved and 89% of people reported no change.
Discussion
We aimed to investigate the immediate and short-term effects of VR-SH on body image and pain intensity compared to a VR-Play control condition. Both groups had positive gains in perceptions of strength, vulnerability, agility and confidence with movement during VR. However, the effects were larger for VR-SH. No effects on body image were present by one-week follow-up and there were no changes in pain in either group. Embodying athletic avatars did not change real-world force production. Intriguingly, seven people in the VR-SH group (35%), reported at least minimal improvement at one-week follow-up, according to Patient Global Impression of Change scores, whereas only one-person in the VR-Play group (10%) reported this level of improvement. This study forms part of a larger body of work investigating the potential of whole-body illusions in altering the experience of the body in people with persistent pain [Citation22,Citation34,Citation35], including studies that involve athletically-enhanced avatars [Citation20,Citation22]. However, this is the only study to go beyond single-case analyses.
The VR-SH exposure, and the related VR-BiT intervention, utilizes strong and fit looking avatars because perceiving the body as vulnerable is proposed to be a mechanism underpinning chronic pain [Citation19]. That is, prominent perceptual models suggest that pain emerges from an inference of threat to body tissues, on the basis of stored and real-time sensory data [Citation19]. It follows that pain may reduce if we successfully counter perceptions of vulnerability. Our findings did not provide support for this hypothesis. However, it was nonetheless encouraging that although the exposure involved movement in a group with highly irritable symptoms, there was no overall increase in pain. Furthermore, analgesia during a single-session exposure does not rule out the possibility of pain reduction in response to a multisession intervention. Indeed, a prior single-case study of VR-SH did not report between-session gains in pain (or body image) until the third session [Citation20].
Future directions
In combination with earlier work [Citation20,Citation22] and findings from a qualitative evaluation of virtual reality embodiment experiences [Citation36], this current study lays the foundation for future work. In particular, this study has confirmed that experiencing immediate, short-term changes in body image through virtual reality is not a unique experience. Future studies may now consider, for example, exploring the effects of a multisession intervention. Another approach may be to investigate if the short-term changes in body image can be leveraged to augment the effects of other rehabilitation interventions. That is, since embodying superhero-like avatars induces short-term improvements in perceived strength and confidence with activity, such an exposure could be tested as a potential primer to improve engagement in other interventions involving physical activity. In this process, we also suggest consultation of guidelines designed to ensure scientific rigour in the development and evaluation of VR interventions [Citation25].
Limitations
This study has a number of key limitations. Firstly, it is important to recognize that studies of small sample size are inherently imprecise, debate about the relevance of significance testing continues [Citation37]. As such, although we chose to include statistical testing for primary and secondary outcomes, results should be viewed with due caution and as informative to further study rather than as conclusive. Furthermore, due to the asymmetrical group size, there was less statistical power for within-subjects statistical tests involving only the VR-Play group. As such, it is most appropriate, in the context of early investigations, to compare groups on the basis of apparent effect sizes rather than whether a statistically significant criterion was met.
As a single-session exposure, the study is unable to support or negate the potential effects of a multisession intervention. Moreover, the possibility remains that VR-SH exposures may have different effects if integrated with other cognitive, behavioural, or exercise-based approaches. A further limitation, is that although VR-SH and VR-Play were designed to be similar in the amount of physical movement involved (e.g., both involved limited, non-strenuous, non-loaded movement) we are unable to confirm their equivalence in regards to the amount of movement performed. Future studies could consider using motion capture or more controlled activities to tease out the independent effects of movement and embodiment. Although the reported strength of embodiment was similar among groups, there were some differences in the avatars beyond their athletic or non-athletic nature. Specifically, two out of three of the avatars in the VR-SH group included a whole-body avatar, whereas only hands were present in the VR-Play condition. However, observation of the data within the three VR-SH conditions, suggested that the effects on body image ratings were equally strong in the Rock Climbing Avatar condition (where only hands were present) compared with the other VR-SH conditions. We suggest therefore, that the physical capacity of the avatar may be as important as its physical (visually apparent) structure.
Somewhat surprisingly, the current study did not replicate the robust analgesic effect that VR typically produces [Citation23]. However, movement also tends to provoke chronic pain, yet no increase in pain was observed during the experiment either. As such, these effects may have simply offset one another, but a further non-VR control condition would have been required to confirm or negate this suggestion.
In studies that require explanation, it can be difficult to distinguish between the effects of this educational element, and the exposure itself. Indeed, in this case it was necessary to provide the two groups with different explanations, which may be responsible for some part of the between group differences observed. However, the body image ratings were taken prior to entering VR, but after the treatment explanation. As such, the immediate effects of the education would have been accounted for by the first ratings. Therefore, if the educational component was more potent in the VR-SH group, then this would actually diminish the apparent effect of the VR-SH exposure.
Conclusions
We aimed to explore the short-term effects of embodying superhero-like avatars on pain and body image in people with CLBP. Relative to VR without a superhero-like avatar, greater positive gains in perceptions of strength, vulnerability, agility and confidence with movement were observed during and immediate after VR. These single-session gains were extinguished by one-week follow-up and no significant changes in pain were found in either group. The immediate effects on body image, combined with the trends towards greater global change at one-week follow-up, supports further investigation of embodiment techniques, such as in a multisession intervention or as an adjunct to other rehabilitation strategies.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Botvinick M, Cohen J. Rubber hands ‘feel’ touch that eyes see. Nature. 1998;391(6669):756–756.
- Slater M, Spanlang B, Sanchez-Vives MV, et al. First person experience of body transfer in virtual reality. PLoS One. 2010;5(5):e10564.
- Serino S, Pedroli E, Keizer A, et al. Virtual reality body swapping: a tool for modifying the allocentric memory of the body. Cyberpsychol Behav Soc Netw. 2016;19(2):127–133.
- Slater M, Sanchez-Vives MV. Transcending the self in immersive virtual reality. Computer. 2014;47(7):24–30.
- Rosenberg RS, Baughman SL, Bailenson JN. Virtual superheroes: using superpowers in virtual reality to encourage prosocial behavior. PLoS One. 2013;8(1):e55003.
- Banakou D, Kishore S, Slater M. Virtually being Einstein results in an improvement in cognitive task performance and a decrease in age bias. Front Psychol. 2018;9:917.
- Costa MR, Kim SY, Biocca F. Embodiment and embodied cognition. in international conference on virtual, augmented and mixed reality. Springer; 2013. https://doi.org/10.1007/978-3-642-39405-8_37
- Moseley GL, Gallace A, Spence C. Bodily illusions in health and disease: physiological and clinical perspectives and the concept of a cortical ‘body matrix’. Neurosci Biobehav Rev. 2012;36(1):34–46.
- Gadsby S. Distorted body representations in anorexia nervosa. Conscious Cogn. 2017;51:17–33.
- Kaplan RA, Rossell SL, Enticott PG, et al. Own-body perception in body dysmorphic disorder. Cogn Neuropsychiatry. 2013;18(6):594–614.
- Giummarra MJ, Bradshaw JL, Nicholls MER, et al. Body integrity identity disorder: deranged body processing, right fronto-parietal dysfunction, and phenomenological experience of body incongruity. Neuropsychol Rev. 2011;21(4):320–333.
- Foell J, Bekrater-Bodmann R, Diers M, et al. Mirror therapy for phantom limb pain: brain changes and the role of body representation. Eur J Pain. 2014;18(5):729–739.
- Riva G, Wiederhold BK, Mantovani F. Neuroscience of virtual reality: from virtual exposure to embodied medicine. Cyberpsychol Behav Soc Netw. 2019;22(1):82–96.
- Keizer A, van Elburg A, Helms R, et al. A virtual reality full body illusion improves body image disturbance in anorexia nervosa. PLoS One. 2016;11(10):e0163921.
- Ziser K, Mölbert SC, Stuber F, et al. Effectiveness of body image directed interventions in patients with anorexia nervosa: a systematic review. Int J Eat Disord. 2018;51(10):1121–1127.
- Serino S, Polli N, Riva G. From avatars to body swapping: the use of virtual reality for assessing and treating body‐size distortion in individuals with anorexia. J Clin Psychol. 2019;75(2):313–322.
- Serino S, Chirico A, Pedroli E, et al. Two-phases innovative treatment for anorexia nervosa: the potential of virtual reality body-swap. Annu Rev Cyberther Telemed. 2017;15:111–115.
- Levenig CG, Kellmann M, Kleinert J, et al. Body image is more negative in patients with chronic low back pain than in patients with subacute low back pain and healthy controls. Scand J Pain. 2019;19(1):147–156.
- Tabor A, Thacker MA, Moseley GL, et al. Pain: a statistical account. PLoS Comput Biol. 2017;13(1):e1005142.
- Harvie DS, Rio E, Smith RT, et al. Virtual reality body image training for chronic low back pain: a single case report. Front Virtual Real. 2020;1:13.
- Crombez G, Eccleston C, Van Damme S, et al. Fear-avoidance model of chronic pain: the next generation. Clin J Pain. 2012;28(6):475–483.
- Nishigami T, Wand BM, Newport R, et al. Embodying the illusion of a strong, fit back in people with chronic low back pain. A pilot proof-of-concept study. Musculoskelet Sci Pract. 2019;39:178–183.
- Mallari B, Spaeth EK, Goh H, et al. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J Pain Res. 2019;12:2053–2085.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Trials. 2010;11(1):32–38.
- Birckhead B, Khalil C, Liu X, et al. Recommendations for methodology of virtual reality clinical trials in health care by an international working group: iterative study. JMIR Ment Health. 2019;6(1):e11973.
- Ware JE Jr, Sherbourne CD. The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Medical Care. 1992;30(6):473–483.
- Whitehead AL, Julious SA, Cooper CL, et al. Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat Methods Med Res. 2016;25(3):1057–1073.
- Schmitz C. LimeSurvey: an open source survey tool. Hamburg (Germany): LimeSurvey Project; 2012.
- Hjermstad MJ, Fayers PM, Haugen DF, et al. Studies comparing numerical rating scales, verbal rating scales, and visual analogue scales for assessment of pain intensity in adults: a systematic literature review. J Pain Symptom Manage. 2011;41(6):1073–1093.
- Leeuw M, Goossens MEJB, van Breukelen GJP, et al. Measuring perceived harmfulness of physical activities in patients with chronic low back pain: the photograph series of daily activities—short electronic version. J Pain. 2007;8(11):840–849.
- Fischer D. Capturing the patient’s view of change as a clinical outcome measure. JAMA. 1999;282(12):1157–1162.
- Cohen J. Statistical power analysis for the behaviour sciences. Hillsdale (NJ): Lawrence Erlbaum Associates; 1998.
- Waltemate T, Gall D, Roth D, et al. The impact of avatar personalization and immersion on virtual body ownership, presence, and emotional response. IEEE Trans Vis Comput Graph. 2018;24(4):1643–1652.
- Stanton TR, Gilpin HR, Edwards L, et al. Illusory resizing of the painful knee is analgesic in symptomatic knee osteoarthritis. PeerJ. 2018;6:e5206.
- Boesch E, Bellan V, Moseley GL, et al. The effect of bodily illusions on clinical pain: a systematic review and meta-analysis. Pain. 2016;157(3):516–529.
- Kelly J, Coppieters MW, Kluver J, et al. “It made you feel like you’ve still got it”: experiences of people with chronic low back pain undertaking a single session of body image training in virtual reality. Physiotherap Theory Pract. 2022, p. 1–11.
- Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res. 2011;45(5):626–629.
