Abstract
Purpose
Digital fabrication, like 3D printing, is a new opportunity for rehabilitation professionals to produce customized assistive devices. It allows for empowerment and collaboration in device procurement, but practical implementations are scarcely described. We describe the workflow, discuss feasibility and propose directions for future work.
Methods
We showcase a process of co-manufacturing a custom spoon handle together with two people with cerebral palsy. Our digital manufacturing process was centered around videoconferencing to remotely control the processes from design to final 3D printing. Device functionality and satisfaction were assessed using standard clinical questionnaires: the Individual Priority Problem Assessment Questionnaire (IPPA) and the Quebec User Satisfaction Assessment with Assistive Technology (QUEST 2.0).
Results
IPPA was instrumental in assessing user needs and device effectiveness. QUEST revealed where to focus future design efforts.
Conclusion
Involving people with disabilities in co-creation of assistive devices opens for new opportunities for healthcare providers that should be explored in depth using the described methodology. There may also be therapeutic benefits and we envisage specific actions to take in order to make it clinically viable.
IMPLICATIONS FOR REHABILITATION
Best practices for co-creation of assistive devices, cost and benefits should be investigated and documented further.
Standard questionnaires are useful for measuring effectiveness and satisfaction of co-created devices as well as for guiding design efforts.
Co-creation may be a valuable element in therapeutic interventions as an opportunity to unfold creativity.
Introduction
Caring for people with disabilities often involves the provision of appropriate assistive devices to maintain or improve their functional skills and autonomy. As every person with disabilities has unique needs, the provision may require more than simply prescribing a ready-made device [Citation1–3]. People with cerebral palsy, for example, may have difficulties in handling cutlery. This presents a special case for co-creating assistive devices as described in the following study.
Standard assistive device provision
Finding assistive devices that meet the personal needs of users is a challenging task [Citation4]. Clinicians may use reference databases, like EASTIN, to identify commercially available devices [Citation5]. However, mass-produced items designed for majority groups may not fit everyone and many assistive devices may be perceived as stigmatizing [Citation6]. Such device-user mismatch often leads to device abandonment [Citation7].
There is a two-way interaction in which an assistive device modifies the users motricity [Citation8,Citation9] and the users motor capacity may require modifications to or alternative versions of the assistive device [Citation9,Citation10]. Thus this may require an iterative process in which there is a mutual adaptation between device and user. Proposing the right device ‘tout de suite’ is sometimes difficult.
These problems can be solved by customizing devices and occupational therapists are trained in this as well [Citation11], but the standardization processes involved in commercializing devices can make customization difficult if not impossible. Sometimes therapists will engage in the creation of ad hoc solutions often using a participatory approach, helping their patients to modify their tools. This approach also respects the patient’s culture without requiring them to change habits or lifestyle [Citation12].
Creating personalized assistive devices
Enabling people to participate in daily living through meaningful activities is among the objectives of occupational therapy with a core assumption that such activities promote mental and physical well-being [Citation10]. Involving the patients in meaningful and useful creative activities has a beneficial therapeutic value [Citation13,Citation14]. Problem solving is a productive use of time that keeps the brain engaged (a preventive strategy to avoid cognitive decline). Being creative increases the sense of competence and self esteem and is a way of socializing through learning and sharing. Furthermore it may be an important outlet for self-expression [Citation13]. It follows that involving people with disabilities in co-creating personalized assistive devices may have therapeutic and functional advantages over providing off-the-shelf assistive devices.
Challenges to Co-creation
Co-creation may be viewed as a process that encompasses co-design (defining a solution) and co-production (manufacturing the device). Both involve the end-user and various people with different backgrounds in variable parts of the process [Citation15]. When people invest effort in customization and manufacturing, they create emotional bonds with the product [Citation16]. This can result in a sense of ownership of the assistive device and thereby an increased value for the user with respect to a commercial device, but it also poses challenges.
Firstly an appropriate solution must be invented or found. Not everyone is capable of inventing and it’s often a very time consuming process. Finding a solution requires that the inventor has shared a feasible solution and made it retrievable. It also requires people with the skills and abilities to replicate the device in an affordable manner. People with disabilities may not have such manual abilities and thus be excluded from auto-fabrication of the device.
An opportunity to solve these issues is the advent of digital fabrication, which has become simplified and available to the layman thanks to the “maker” movement. It holds the promise of solving some of the above problems. However, it is scarcely documented in scientific literature [Citation13,Citation14,Citation17].
Hands-free creation
Digital fabrication is a design and manufacturing process; computer aided design (CAD) is used to draw a three-dimensional (3D) model and computer controlled machinery creates the physical object. This allows for a repeatable hands-free production requiring minimal or no manual manipulation.
The models can be easily shared widely via the internet and there are several sites like Thingiverse containing 3D models ready for digital fabrication [Citation18]. Although Thingiverse with 2 million models is one of the largest repositories, it contains relatively few assistive devices. They are not classified in a way that makes them easy to find. Feasibility, functionality or user satisfaction of the solutions are scarcely described. Therefore, identifying suitable solutions requires knowledge and can be a daunting task for many clinicians and users [Citation13,Citation19].
An opportunity for inclusion
Participation in co-creation activities may be limited by mobility and logistic issues. The social distancing as recently caused by the COVID-19 pandemic caused an evolutionary leap in social life. Collaborative tools like Zoom ™ etc. became available for free and most people started using video conferencing software for work, study and social interactions. Telerehabilitation where clinicians interacted with their patients became routine [Citation20]. This presented the opportunity to meet online in different locations without the overhead of transportation; enabling a new workflow as described in this paper.
Cutlery adaptation
A wide variety of grips can be used for eating. A certain modification to a flatware may incur another type of grasping. This two way interaction may constrain the user to grip and move in a different way [Citation8,Citation9]. The question then becomes: do we want to change the users habits or do we want to maintain the users patterns and adapt the device to facilitate them?
The prevailing grip for many people when eating with a spoon/fork is the precision grip (the three finger clenched grip), . In cases where the adduction of the thumb is weak, an alternative grip, the palmar grip (or radial transverse palmar grip), may be used, . This is often the case for people having tetraplegia due to spinal cord injury [Citation11]. This incurs a different movement to pick up the food and bring it to the mouth than when using the clenched grip.
Figure 1. (A) The three finger clenched grip or transverse digital radial grip is commonly used by most people. (B) The transverse palmar grip (power grip) may be less suited for holding forks and spoons, but may be used as an alternative to the clenched grip. (C) Holding a spoon having a standard build-up handle thickening the shaft to facilitate clenching between thumb and index fingers. (D) Eating with a cuff-based device. The transverse palm grip is an option for people with impaired finger flexion strength e.g., resulting from cervical spinal cord injury.
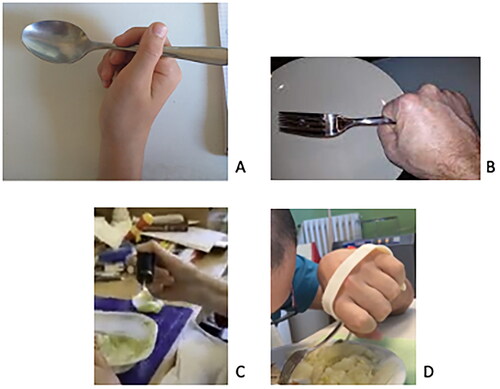
The cutlery section (ISO 15.09.13) of the EASTIN database (www.eastin.eu), holds over 500 commercial devices in which the majority for silverware handling are using one of two principles: modifying the cutlery itself to have a larger handle () and/or applying an interface element that 'attaches’ the cutlery to the hand. When the palmar grip (finger flexion) is weak as in quadriplegia, a strap around the dorsal side of the hand can provide a better grip. This is the principle of many 3D printed solutions () [Citation23].
However, as Western food culture uses the clenched grip, this grip may be preferred over the palmar grip as the latter has some implications; less control and risk of dipping your hand in soup when filling the spoon, just to name a few.
The need for best practice development
Co-creation of assistive devices with digital technologies offers new opportunities and we need to increase the knowledge within health care provision as to “best practice workflows” [Citation19]. Therefore the aim of this paper is to document a feasible workflow involving people with cerebral palsy in the co-creation process.
Methods
In a previous study an online platform for the creation of customized 3D printed assistive devices was tested by five people living in the residential nursing care department (RSD) of our rehabilitation center. They all were adults having cerebral palsy and consequently impairments of the upper limbs. The study is further described in reference [Citation23] and [Citation24]. One of the devices was a spoon or fork holder. Neither this device nor the standard alternatives proved effective or satisfactory for the users. Therefore we offered them an opportunity to engage in co-creating a custom device following an approach developed in previous research [Citation19]. The two participants in this study had a diagnosis of cerebral palsy as follows:
Participant 1. a 47 year old female with dysphagia and non-progressive congenital ataxia syndrome due to olive-ponto-cerebellar atrophy.
Participant 2. a 45 year old male with spastic tetraparesis and mild mental retardation.
All interactions with the participants were according to current clinical practice, rules and ethical code of conduct and reviewed by the local ethical commission.
Evaluations
The efficacy and satisfaction of assistive devices were evaluated using the Individual Prioritized Problem Assessment (IPPA) and the Quebec User Evaluation of Satisfaction with Assistive Technology (QUEST 2.0). The IPPA [Citation21] asks the user to list the most important problems that the device should solve, giving an importance and a difficulty to each on a scale of 1 (very little) to 5 (a lot). After using the device, the user re-evaluates the difficulty of each problem. The IPPA score is the change of the average product of importance and difficulty. The combination of being an individualized measure, the subjective nature of the tool and the collaborative nature of the problem identification means that validity and reliability is difficult to assess.
We used the QUEST 2.0 device subscale [Citation22] in which the participant is asked to score, from 1 (very little) to 5 (a lot), each of the eight satisfaction elements (Q1 - Dimensions, Q2 - Weight, Q3 - Adjustments, Q4 - Safety, Q5 - Durability, Q6 - Ease of use, Q7 - Comfort and Q8 - Effectiveness). The QUEST score is the average. An item with a score of less than 3 indicates an issue and should be commented on to explain the problem.
For both questionnaire scores in the range 4–5 is considered high and is a clear indication of satisfaction and relevance whereas IPPA scores below 1 suggests to check whether the assistive solution has proved ineffective or brought mixed advantages and disadvantages [Citation23].
The IPPA questionnaire is a two-step questionnaire where the evaluator has to refer to the issues set out in the first evaluation. In line with pandemic restrictions we wanted to reduce paper exchange and use an online form. Two-step form submissions are not supported by standard online forms providers like Google or Microsoft. For this reason, a dedicated website was created to collect the questionnaire (IPPA and QUEST) data via smartphone or tablet (source code available on demand from first author).
Observations and tools
Before designing ad-hoc solutions, major CAD repositories on the internet, like Thingiverse [Citation18], were searched, designers, students, maker communities and published works were consulted [Citation13,Citation14,Citation17,Citation19,Citation24–26]. No ready-to-make appropriate solutions were found.
We observed participants in their daily activities and living environment. Smartphone video clips of eating with and without assistive devices were used to share an understanding of movement patterns, grip types, possible solutions and ideas, between participants and facilitators.
We used a typical digital manufacturing method involving CAD for 3D modeling and 3D printing. Specifically, our workflow used the following toolchain: a CAD software service, a slicing program and a 3D printer and a video conferencing application as described in the following.
CAD
We selected a parametric solid modeling CAD solution as a free service for non-profit use. It basically works as follows: A two-dimensional (2D) projection is drawn, then it is transformed into a three-dimensional (3D) solid. Several solid objects can be combined to form a complex shaped model. Constraints can be added as parameters. A constraint can for example be a length, given as a variable, or it can be a rule or relation between entities.
Drawing a pencil, for example, requires you to draw the hexagonal shape of the pencil body, extruding it to a length given by a variable. Create a tip in a similar way and add it to the pencil body. Then the length of the pencil can be adjusted by changing the value of the variable.
We used Onshape ™ (www.onshape.com) which runs on a server in the cloud and is accessed via a standard internet browser. It allows real time collaboration where multiple users can access the same drawing and work on it at the same time. The design can be viewed on the user’s smartphone, tablet or computer by sharing the link (the URL) to the CAD internet site.
Slicing
The slicer, Cura ™ (www. ultimaker.com), is a program that converts CAD models into a code the 3D printer can understand and use to produce the object. Basically it is determining how the extrusion of the material will happen. This is where the compromise between quality and speed of the production process is established.
Printer
Our 3D printer, Ultimaker S5 ™ (www. ultimaker.com) was a commonly used desktop machine that uses fused deposition modeling, in which material is selectively melted and dispensed through a nozzle onto other layers or the build plate. Not all shapes and geometries can be created using this kind of fused filament fabrication. Some will require advanced skills and methods and the processing can become quite complex. The machine can be remote controlled over the internet and has a small built-in webcam.
Materials
There are many types of plastics available with polylactic acid (PLA) being the most common and easy to use. However, it tends to deform at dishwasher temperatures. A non-toxic alternative in the printer material range is thermoplastic polyurethane (TPU). Ultimaker TPU95 ™ is a smooth, dishwasher safe rubber-like material suitable for items that require skin contact, available in various colors. It is chemically resistant to alcohol and hand sanitizers. The latter was relevant as such agents were used extensively during the COVID-19 pandemic to disinfect objects and hands.
Video conferencing tool
We wanted to enable participants to remotely control all digital fabrication steps via a central computer; a computer running the necessary software and hosting the videoconference. Zoom™ (www.zoom.us) was the only free and commonly used video conferencing tool allowing such remote desktop control. It was also a tool that participants and facilitators had become accustomed to use for daily interactions during the pandemic.
Before the meeting, a browser was prepared with two windows, open side by side. A window showed the online CAD model. Another window exposed the slicer and printer control software. We used a smartphone with the camera facing the 3D printer, acting as a webcam, to show meeting attendees how the 3D printing process proceeded.
Co-creation workflow
Participants assistive needs
Two subjects from the previous project (see reference [Citation24]) were interested and able to participate in this ad-hoc co-creation process. They had been trying a 3D printed flatware holder and some commercial counterparts. The ‘facilitators’ driving the process were a research engineer and an occupational therapist.
The two participants had indicated the following problems (P) in the IPPA questionnaire along with the importance (I) and the difficulty (D):
First participant
P1. Improve the grip of the spoon (I = 3; D = 2)
P2. Improve performance in spoon-feeding at the end of a meal (I = 4; D = 4)
P3. Difficulty in bringing the spoon to the mouth (reaching the mouth precisely) (I = 5; D = 3)
P4. Difficulty in bringing the spoon to the mouth due to involuntary movements (I = 4; D = 3)
P5. Greater independence during the meal inside the structure (I = 5; D = 4)
P6. Greater independence during the meal outside the structure (I = 5; D = 4)
P7. Better self-esteem (independence, not getting dirty while eating) (I = 5; D = 4)
Second participant
P1. Difficulty in bringing the cutlery precisely to the mouth (I = 3; D = 4)
P2. Difficulty in taking the cutlery (I = 3; D = 4)
P3. Difficulty picking up food from the plate, especially with a spoon (I = 3; D = 4)
P4. Reduce the loss of food from the spoon (I = 5; D = 5)
P5. Greater independence during meals within the structure (I = 3; D = 5)
P6. Greater independence during meals outside the structure (I = 3; D = 5)
P7. Not Answered.
Model research and initial design proposal
We spent some weeks researching a suitable 3D printable model for the co-design process, using the requirements from the IPPA questionnaire. Most models were published in the STL format, which is non parametric and hence not very easy to modify by non-expert users.
Fundamental requirements were: the design should respond to the problems raised in the IPPA, be simple to produce on the 3D printer for the non-expert user; allowing the user to have a central role in the production process considering a limited manual ability. Furthermore the design should be:
* Fully user editable using a parametric and scalable design to fit hand size.
* Open source i.e., free to use and modify.
* 3D printable in a one-shot process (no separate slicing/printing of individual parts) and not requiring post-processing (removal of supports, etc.).
* Fitting generic cutlery, using skin friendly and dishwasher safe materials.
Not finding a suitable ready-to-use 3D printable solution for our participants meeting the above requirements, we decided to design an ad-hoc solution for the purpose of initiating a co-design process.
First iteration
In the first iteration we developed and tested a flexible, generic strap solution consisting of ovals, see . The cutlery could be held by intertwining the handle in the ovals.
Figure 2. (A) The first iteration consists of an elastic strap of ovals that can be hinged to adjust the tightness and a piece for fixing the cutlery. (B) Intermediate iterations knife, fork, spoon/teaspoon handles, and the strap solution. (C) The final build up handle for a spoon. (D) A participant using her self produced device.
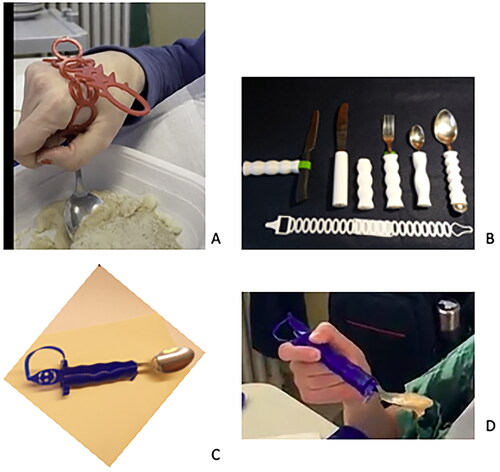
Our first participant tried 3 iterations of the strap with and without cutlery fasteners. We concluded that the palmar grip was not useful for spoon eating. Our participant did much better holding the spoon ‘normally’ using the clenched grip. So we decided to work on a custom ‘build up handle’ solution that the participant could try, some iterations are shown in .
We found TPU95 to be a soft and comfortable, but slippery material, in the sense that the friction between TPU and metal is low. We had trouble designing a method of attaching the spoon handle to the device that was easy for the participant to assemble while fixing the cutlery firmly. With an intermediate version we noticed that one participant was ‘biting’ when retracting the spoon, thus ending up detaching the handle from the spoon or losing the grip on the handle. To solve the latter, a “wavy” handle shape was applied to provide a better grip (ref. IPPA problems 1 and 2).
Spoon/fork holder
We settled for a two-part solution consisting of a handle in which a fork/spoon holder can be inserted (). The inner part could be folded allowing the spoon handle to be inserted in the two holes. When inserted into the handle the inner part locked onto the cutlery providing friction between the TPU part and the metal part. Standard hospital food service cutlery could be used so users did not need to carry dirty cutlery with them after eating thus partially solving IPPA problems number 5 and 6.
We wanted to make the device playful, as to distinguish itself from the stigmatizing “food device for the disabled” (see first participant IPPA problem 7). The handle has two “arms” for a better grip when disassembling the device and there are two “feet” at the inside of the device for the same reason, as well as a “head” that could be pulled during assembly. Since these features seemed to lend themselves to an anthropomorphic form, adding a “face” seemed obvious to give it an interesting aesthetic look. The two parts are connected by a band to avoid the separation of the parts during cleaning and transport. The model is publicly shared in Onshape ™ with the name 'Portaposata05' (https://cad.onshape.com/documents/aaa033610769cc0827ecb752/w/af6ffcb0ce38fc3151f7b425/e/365ae8e708fcad69efd6653a).
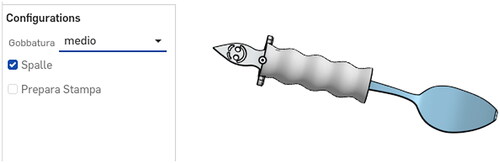
Co-creation process
With this model we engaged in the complete co-creation process where each participant was active in all stages of the workflow. The CAD was prepared with a graphical organization of parameters that the user could modify, see . Changes were rendered instantly. The descriptive variables were prepared in the language of the participants. A video conference call was organized between the remote computer in the 3D printing laboratory and a laptop in the RSD which the participant and the therapist used. The participant and facilitators were able to collectively edit the CAD model using the screen sharing and remote control facilities of the video conferencing software. The participant was instructed on how to modify the model according to personal preferences (shape selection, activation/deactivation of functions and insertion of the handle length). We explained how to export, slice and start the building process. Specifically, the participant downloaded the STL file on the remote machine, processed it with the slicing program and started the 3D printing process using the remote control. One of the video panels displayed the 3D printer building the object. The participants used mostly click, drag and drop actions; the first participant used a mouse and the second used a trackball. After the participant had launched the build process he/she could observe how the machine started 3D printing his/hers device, whereafter the machine was left unsupervised to complete the build process, which took 1–2 h. The only manual intervention required was to remove the object from the build plate and the therapist brought it to the participant. This workflow was used on both Windows and Linux operating systems.
Figure 3. An example from the cloud based CAD design with a configuration panel where the participant can modify features. 'Gobbatura’ is the 'undulation’ of the handle finger grooves and ‘Spalle’ is the ‘shoulders’ beneath the ‘head’. Selecting the ‘Prepara Stampa’ renders the part in the 3D printing position, ready to export it to the slicing software.
Results
Our first participant was able to eat both with a regular spoon and with her self-made device, but the latter gave her better control according to the IPPA questionnaire. The IPPA change score was 1.3 due to improvements in grip, independence, and improved self-esteem.
The QUEST score was 4.5 points meaning high satisfaction with the device [Citation23]. A helper could assemble the handle and return the spoon for cleaning after eating. The handle itself could also go in the dishwasher when needed. In the comments of QUEST and IPPA she indicated some details that she would like to correct in a further iteration. These problems were related to the way in which the spoon was positioned in the device and to some difficulties in assembling the device. As she commented: “The wavy version works well; the part near the spoon is a bit thick and often touches my nose. I'd like it tighter, maybe funnel-shaped. Assembly is too difficult. It’s not possible for me to insert/remove the cutlery and adjust its position”. Resolving these would require additional design efforts not available under this project.
The participant showed enthusiasm in using the self-made spoon handle and took it with her on vacation to use it outside of RSD facilities.
Our second participant produced a slightly modified version for a bent spoon. And with respect to our first participant, he perceived it as more functional with an IPPA change score of 6.6 points. In his case, a real priority was satisfied by the device he created. He was very satisfied with the device (QUEST score 4.4 points) and continued using the device in daly living.
Discussion
Digital manufacturing such as 3D printing opens up new possibilities in the healthcare sector. It may be an alternative way of assistive device provision that takes personal needs into account. Our two participants had less difficulty in their prioritized problems, scoring 1.3 and 6.6 on the IPPA scale, which means the devices were perceived as respectively moderately and highly effective. The QUEST scores, respectively 4.5 and 4.4, are to be considered high [Citation23]. Both participants were satisfied with their co-created devices which they continued to use after project end.
In the following we discuss some considerations for developing an efficient and meaningful co-creation workflow.
Language
An implicit aspect of co-creation is to break down barriers and focus on peer collaboration between people. Therefore, a person-centered language [Citation27] within a co-design framework is desirable. The word “patient” implies that one is ill or is being treated due to an injury or illness [Citation27,Citation28]. A hospital or rehabilitation setting traditionally uses doctor-patient roles, while the co-creation paradigm encourages a mindset and language in which participants are individuals with disabilities, people with special needs and facilitators are people with skills and experience, doctors, technicians etc. that promote and support co-creation activities.
Iterative adjustment to requirements
As discussed in the introduction, users may adapt to the device or the device may be adapted to the user. Eating styles, methods and habits are individual therefore device provision may become a trial and error process where new movement strategies and solutions can be explored. This is where co-design and co-production may have an advantage as the assistive device can be specifically made to meet not only needs but also to fit into existing movement habits. Solutions placing the cutlery in the palm (cuff and strap solutions) may be feasible in cases where the normal grip is not possible. One issue with this grip is that the user may have difficulty in filling liquid food into the bowl of the spoon without dipping the hand into the plate as well. Thickening the handle (build up handle) can facilitate spoon manipulation and therefore this device type may be preferable over the ‘strapping solutions’. The diameter of the handle may influence performance [Citation9]. Using digital fabrication in the co-creation process provided the possibility to optimize that through iterations in a timely manner.
Assessment of appropriateness
The IPPA questionnaire prompted participants into verbalizing problems in an open way which we found helpful for understanding what the participant really wanted to work on. Furthermore IPPA provided quantitative indication of the appropriateness of the co-created result.
The QUEST, on the other hand, provided standardized inputs to general aspects of the design in engineering and design oriented terms. As this prompted the user to pin down the usability and effectiveness issues that could influence the IPPA score, it gave a structured identification of issues and advantages of the design that prompted the participants to propose improvements.
However, it is likely that questionnaire based evaluations are biased by the emotional bonding that the participants may have created during the process[Citation16]. One may be inclined to say that something that has been self-made is better than a ready-made device and this raises a philosophical question: what is more important, objective efficiency or user satisfaction?
Co-creation toolchain model
A freely accessible online (cloud based) toolchain of collaborative software reduces the barrier caused by limited mobility and enables laymen to meet, plan, co-design and produce objects. Browser based software for meeting, remote control and CAD designing eliminates the overhead for installation and renders the toolchain independent of operating systems. This favors clinical practicality. It gives the flexibility to use the participant’s computer or any computer at hand to participate in the co-creation process; to share, inspect and comment on design ideas in a collaborative process.
The video meeting tool is critical as it should allow remote control (agonistic to safety concerns). Remote control is essential when some components in the toolchain, such as the slicing tool, are not cloud based and thus require installation on the computer that controls the 3D printer. It is implicit that the equipment has to be adequate with respect to internet speed and display size. The experience must be smooth and CAD details require a large and high resolution screen. Difficulties may have arisen if using slow connections and smaller tablet/smartphone screens and thus exclude people in remote or less technologically equipped regions.
CAD programs
Modeling in a parametric CAD program is currently not an intuitive process as it is radically different from normal drawing on paper or modeling physical objects. Learning how to use such programs and the basics of designing 3D printable objects may exclude many non-technically minded people. Most CAD programs, suitable for 3D printing, assume professional design skills having technically challenging user interfaces (e.g., Solidworks, Autocad etc.). Some free programs (e.g., Tinkercad, SketchUp, Freecad, OpenSCAD) may claim to be very easy to use, allowing even children to produce 3D models, but they may fall short of important features that our chosen CAD program had such as: creating solid (manifold) 3D printable objects, being parametric with instant rendering, allowing online collaboration and instant sharing, using graphical input methods (as opposed to text based input user interface) etc.
Online collaboration allowed participants in co-designing to connect from anywhere and view/modify the design; the design could instantly be shared publicly allowing other people to contribute without the need to send and receive design files. Instant rendering was useful for providing some dynamic simulations to help participants in understanding the design functionality.
We especially consider the possibility of letting the participant edit the design as important (otherwise it would not be co-creation). For example, our first build up version had two 'feet’, aimed to facilitate replacement of the cutlery. These appeared to be in the way when eating as they protruded into the dish. When making a second version, the participant removed these by suppressing that specific design feature in the parametric design with a mouse click, thus effectively becoming part taking in the design process.
A useful comparison and comprehensive list of CAD programs can be found on wikipedia [Citation29].
From design to co-design
Though there are platforms for sharing designs, these are not specifically built to provide the specific information that rehabilitation professionals and their patients may need [Citation13,Citation19]. One may find solutions apparently matching an unmet need, however before replicating a solution one may want to understand what resources (time, skills, materials and machinery) are required as well as how functional and satisfactory the solution is. This puts the co-creation team in a dilemma of having to decide whether to replicate, eventually with modifications or start a completely new design. The former may involve the risk of replicating an unvalidated solution. The latter requires significantly more resources as it is time consuming and requires product design skills. Our experiences confirm a need for the development of a dedicated innovation sharing platform of do-it-yourself solutions for co-creatable assistive devices [Citation17,Citation25,Citation30,Citation31]. We envisage that such a platform may include a validation system of the proposed solutions. This could be in the form of dedicated questionnaires such as IPPA and QUEST. It would ideally be a partnership between existing platforms for standardized products such as the Global Assistive Technology Information Network (EASTIN) [Citation5,Citation31]. Finally, as co-creation is essentially a button-up solution, the platform should be co-created with users as was the case for Wikipedia, which has demonstrated a model of crowd sharing leading to quality content [Citation32].
Issues in digital fabrication
Digital fabrication as a hands free, self-production method can enable people with disabilities like impaired dexterity to manufacture assistive devices by themselves. A popular and economical method is 3D printing using fused filament fabrication, but it is just one of many methods ranging from automated industrial factories to hobbyist-level laser cutting and even knitting machines [Citation33,Citation34]. Many alternatives to 3D printing should be explored.
Before printing an object the machine has to be prepared and filament has to be loaded. Other operations may be needed. Thus, though not requiring particular dexterity, it’s not a completely hands free process. Substantial knowledge about the method must be acquired to use the machine and get satisfactory results.
There are many factors that may cause the process to fail so some supervision of the process should be done, which adds to the time participants need to invest. It does take some time to prepare and produce the object typically from one to several hours. Our final devices took 1–2 h to manufacture using rough quality settings. The finest quality setting multiplies production time by 4–5 times. Promoters of 3D printing often claim that it’s inexpensive, but they only compare material prices [Citation14,Citation26]. Mass production methods produce items in minutes whereas 3D printing takes hours while still requiring experienced persons to set up and supervise. Hence it calls for a substantial amount of man-machine time to get one specialized result. Commercial build up handles are available from 5 €(foam tube style). Considering the time invested in co-creation (estimating at least 40 man-hours of net involvement) the total cost is a hundredfold more. A cost benefit analysis with respect to buying mass produced devices is therefore warranted, not only comparing material price but overall cost as a service including professional man-hours. However, it should also be considered that finding the right commercial device may involve time and cost of going through, acquiring and testing numerous commercial solutions.
Some geometric shapes are difficult to make on this type of machine (composite materials, protruding arches, unsupported elements, etc.), so other types of digital fabrication methods may be required to meet general demands for assistive devices.
However, digital manufacturing technology is developing rapidly and we expect many problems to be solved in the near future. Furthermore, there are many online services offering digital fabrication, so the process can be delegated from the participant to a professional. This leads to a question about how this opportunity would affect the clinical value of co-production.
When to start co-creating
The availability of resources, skills, experience with digital fabrication and the participants’ physical and cognitive abilities must be considered when deciding when and how they should be included actively in the design and production process. We had no prior experience involving adults with cerebral palsy in co-creation, neither found examples in literature. Therefore we designed solutions for the participant to try before actively involving them in the idea generation. Rendering the models sufficiently simple to allow the participants to alter the design was difficult. However, the participants understood the process and were able to control the computer via a mouse or trackball. Help was needed when it came to inserting numbers for parametric variables. Letting the users create the CAD models would probably not have been possible as CAD programs are still very technically challenging and require 3D design skills. Therefore, design preparation by a clinical-technical facilitator collaboration precedes including the user. It not only involves creating a technically feasible solution, but also translating it into a multidisciplinary ecosystem enabling all participants to contribute and finally produce the assistive device.
Therapy of Co-design
Social distancing during the pandemic had led to regression in the participants mood. We observed that the involvement in co-design research was welcomed by the participants. It was a functional means of social inclusion with empowering objectives. Activities were driven by curiosity, a wish to explore devices and methods eventually facilitating activities of daily living, but not so much a specific need for an assistive device. Participants became engaged in the evaluation, asked for improvements and suggested modifications. Particularly the possibility in the questionnaire of adding comments to the ratings appeared to give a sense of empowerment to the participants, besides being potentially useful for design iterations. This is an observation that should be investigated further.
Co-creation may be a functional and useful occasion for 'doing’ together as a therapeutic activity [Citation35]. It allows for a humanistic approach that extends beyond a mere functional need in order to develop holistic solutions that embody the emotional, social, and cultural aspects of users [Citation36]. The emotional impact and 'therapy of making’ could be subject to further investigation on a psychological level. We saw participants becoming more motivated for independent eating. Whether this was due to 'end of pandemic isolation’, the participation in this study or other factors can be questioned. It may be a practically useful activity in the 'toolbox’, from which the therapist can select ideas to inspire their patients with ways of promoting autonomy, well-being, and social participation.
We hypothesize a beneficial psychological effect for a patient to become both producer and consumer of the assistive device; a so-called prosumer [Citation37], a responsible and competent maker of self-created assistive device solutions. It may increase the level of acceptance, autonomy and motivation as well as giving a sense of being in charge of one’s condition. The idea of co-creation became viral in the department prompting other residents with disabilities to ask for specific solutions to their daily challenges.
Therefore a further study could investigate the psychological benefits of the co-creation as a meaningful and functional therapy.
Feasibility of a Co-creation paradigm
This provision model was feasible within an action research framework, because the technical part (3D printing etc) was fully taken care of by the research technician and evaluations could fit into the occupational therapist’s work plan. However, the time spent on co-designing must be accounted for and will affect the cost of assistive device provision service. In some context, the added time may not be compatible with existing public healthcare provision plans.
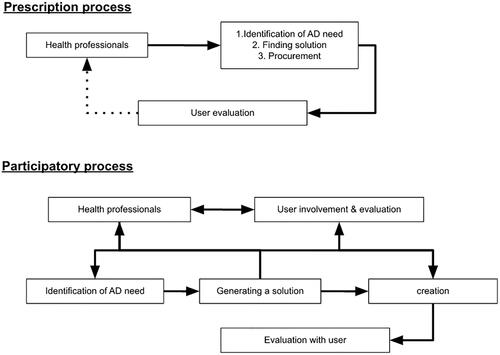
The paradigm for prescribing commercial assistive devices is usually a top-down process where the health care professional involves the client in deciding a standard solution. Digital fabrication holds a possibility to shift this paradigm towards a participatory interactive process where the user becomes involved in the identification of needs, design and eventually co-created the device, see .
Figure 4. Schematic illustration of models of assistive device provision interactions. The upper is the classic top-down approach where the user is a passive receiver. The lower is a step towards an interactive process where the user becomes involved in three phases and ends as a prosumer of the assistive device.
As this is still uncharted territory we need more research for an effective implementation in clinical practice.
Critical issues of the process
Cost effectiveness. Co-design requires a significant amount of time and qualified human resource investment
Timeliness. Solution and CAD model identification, need for research and development can take a considerable amount of time and be a bottleneck for co-creation.
Compliance. Many people may prefer an off-the shelf solution; they may be disinterested in the co-design, unable to participate or there may be economical obstacles.
Quality. Commercially mass produced certified devices have guaranteed quality, whereas newly designed devices will be of prototype quality.
Conclusion
Digital fabrication, as for example 3D printing, is a feasible opportunity for healthcare professionals to actively include their patients when providing assistive devices. In this study we involved adults with cerebral palsy in a process in which they succeeded in co-creating their personal assistive devices with substantial involvement of the staff of healthcare professionals.
A workflow, involving the user in co-creating assistive devices was developed and tested, but a number of steps have to be taken to facilitate its deployment in clinical practice:
We need to develop a reliable method for identifying validated, functional and feasible solutions for co-creation. For that we envisage a database aggregating feasible self-produced solutions which are evaluated using validated instruments like the IPPA and QUEST questionnaires.
There is a need to render elements of the digital manufacturing toolchain more user friendly. Specifically CAD programs are still for advanced users and 3D printing should become faster and more versatile.
Qualitative and quantitative research should generate evidence of clinical value and we propose systematic use of clinical questionnaires for assessment of efficiency and satisfaction of co-created devices. The therapeutic value of co-creation should be further explored and compared to alternative occupational therapy options.
Ethical approval
The research has been approved and conducted according to the local ethics committee requirements.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
Data available on request from the authors.
Additional information
Funding
References
- Edwards NI, Jones DA. Ownership and use of assistive devices amongst older people in the community. Age Ageing. 1998;27(4):463–468.
- Holt RC, Holt RJ. Gerotechnology: kitchen aids. Eur. Geriatr. Med., Vol. 2011;2(4):256–262.
- Kottow MH. Between caring and curing. Nurs. Philos. 2001;2(1):53–61.
- Scherer MJ, Craddock G. Matching person & technology (MPT) assessment process. Technol. Disabil. 2002;14(3):125–131.
- Andrich R. Towards a global information network: the European assistive technology information network and the world alliance of at information providers. In: Everyday Technology for Independence and Care. IOS Press, 2011. p. 190–197.
- Giesbrecht E. Application of the human activity assistive technology model for occupational therapy research. Aust Occup Ther J. 2013;60(4):230–240.
- Cruz D, Emmel MLG, Manzini MG, et al. Assistive technology accessibility and abandonment: challenges for occupational therapists. Open J Occup Ther. 2016;4(1):10.
- Roda-Sales A, Vergara M, Sancho-Bru JL, et al. Effect of assistive devices on hand and arm posture during activities of daily living. Appl Ergon. 2019;76:64–72.
- van Roon D, Steenbergen B. The use of ergonomic spoons by people with cerebral palsy: effects on food spilling and movement kinematics. Dev Med Child Neurol. 2006;48(11):888–891. Nov.
- Hammell KRW, Iwama MK. Well-being and occupational rights: an imperative for critical occupational therapy. Scand J Occup Ther. 2012;19(5):385–394.
- Bromley I. Tetraplegia and paraplegia: a guide for physiotherapists. New York: Churchill Livingstone Elsevier Health Sciences; 2006.
- Maia FB, Teixeira ER, Silva GV, et al. The use of assistive technology to promote care of the self and social inclusion in patients with sequels of leprosy. PLoS Negl Trop Dis. 2016;10(4):e0004644.
- Lunsford C, Grindle G, Salatin B, et al. Innovations with 3-Dimensional printing in physical medicine and rehabilitation: a review of the literature. Pm R. 2016;8(12):1201–1212.
- Schwartz JK, Fermin A, Fine K, et al. Methodology and feasibility of a 3D printed assistive technology intervention. Disabil Rehabil Assist Technol. 2020;15(2):141–147.
- Windasari N, Visita L, Of Economics F, et al. Universitas islam negeri – walisongo, Jl. Prof. Dr. Hamka, 3rd campus UIN walisongo, ngaliyan, semarang, Indonesia, “user engagement mechanisms of online Co-Design service: does user innovativeness matter? Asian Acad Manag J. 2019;24(1):59–82.
- Mugge R, Schoormans JPL, Schifferstein HNJ. Emotional bonding with personalised products. J Eng Des. 2009;20(5):467–476.
- Thorsen R, Bortot F, Caracciolo A. From patient to maker - a case study of co-designing an assistive device using 3D printing. Assist Technol. 2021;33(6):306–312.
- Thingiverse.com. Thingiverse - Digital Designs for Physical Objects. Accessed 2022. https://www.thingiverse.com/
- Buehler E, et al. Sharing is caring: assistive technology designs on thingiverse. Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems, Seoul, Republic of Korea. 2015. p. 525–534.
- Gonzales-Zamora JA, Alave J, De Lima-Corvino DF, et al. Videoconferences of infectious diseases: an educational tool that transcends borders. A useful tool also for the current COVID-19 pandemic. Infez. Med. 2020;28(2):135–138.
- Wessels R, et al. IPPA: individually prioritised problem assessment. Technol Disabil. 2002;14(3):141–145.
- Demers L, Weiss-Lambrou R, Ska B. The Quebec user evaluation of satisfaction with assistive technology (QUEST 2.0): an overview and recent progress. Technol Disabil. 2002;14(3):101–105.
- Salatino C, Pigini L, Andrich R. How to measure the impact of assistive technology solutions on the person’s quality of life? Proceedings of the 4th EAI International Conference on Smart Objects and Technologies for Social Good. Goodtechs 2018 – Bologna 28-30/11/2018 2018. p. 238–242.
- Grippos. Grippos. 2022. https://www.grippos.it/
- Aflatoony L, Lee SJ. Codea: a framework for Co-Designing assistive technologies with occupational therapists, industrial designers, and End-Users with mobility impairmentsin. Proceedings of the Design Society: DESIGN Conference, Cambridge University Press, 2020. p. 1843–1852.
- Hunzeker M, Ozelie R. A Cost-Effective analysis of 3D printing applications in occupational therapy practice. Open J Occup Ther. 2021;9(1):1–12.
- Crocker AF, Smith SN. Person-first language: are we practicing what we preach? J Multidiscip Healthc. 2019;12:125–129.
- Zhao J, Gao S, Wang J, et al. Differentiation between two healthcare concepts: person-centered and patient-centered care. J Nurs. 2016;2352:0132.
- Wikipedia. Computer-aided design. 2022. https://en.wikipedia.org/w/index.php?title=Computer-aided_design&oldid=1081445697
- Boral H, Gefen N. The PELE center: making tailored solutions for children with disabilities. In: Global perspectives on assistive technology., World Health Organization, Geneva, Switzerland, 22–23 August 2019. Volume 2. World Health Organization. 2019. p. 286–293.https://apps.who.int/iris/handle/10665/330372.
- Zahid A, Krumins V, De Witte L, et al. The development of innovation sharing platforms for low cost and do-it-yourself assistive technology in low and Middle-income countries. In: Global perspectives on assistive technology.; 2019. p. 359–376.
- Michelucci P, Dickinson JL. The power of crowds. Science. 2016;351(6268):32–33.
- Brooks L, Ta K-HN, Townsend AF, et al. I just love it’: avid knitters describe health and well-being through occupation. Can J Occup Ther. 2019;86(2):114–124.
- Fossdal F, Heldal R, Peek N. Interactive digital fabrication machine control directly within a CAD environment. In: Symposium on Computational Fabrication, Virtual Event USA, 2021. p. 1–15.
- Piergrossi JC. The function of ‘doing’ in the intermediate space: donald winnicott and occupational therapy. In: Psychoanalytic thinking in occupational therapy. West Sussex: John Wiley & Sons, Ltd; 2013. p. 57–67.
- Sarmiento Pelayo MP. Co-design: a Central approach to the inclusion of people with disabilities. Rev Fac Med. 2015;63(3Sup):149–154.
- Goodman C, Jimison H, Pavel M. Participatory design for home care technology. Presented at the Proceedings of the Second Joint 24th Annual Conference and the Annual Fall Meeting of the Biomedical Engineering Society. Engineering in Medicine and Biology, Houston, TX, USA vol. 3. 2002. p. 1873–1874.
