Abstract
Purpose
To test the hypotheses that, after the delivery of manual wheelchairs following the WHO 8-step service-delivery process, wheelchair-related health and quality of life, wheelchair skills, wheelchair use, and poverty probability would improve; and that the number of wheelchair repairs required, adverse events, caregiver burden, and the level of assistance provided would decrease.
Methods
This was a longitudinal, prospective within-subject study including 247 manual wheelchair users, and 119 caregivers, in El Salvador who received a wheelchair following the WHO 8-step process as well as maintenance reminders. Outcome measurements were performed via structured questionnaires and dataloggers at the initial assessment, at wheelchair delivery, and at 3- and 6-month follow-up.
Results
Significant improvements in wheelchair-related health indicators (all with p < 0.004) and quality of life (p = 0.001), and a significant reduction in national and “extreme” poverty probability (p = 0.004 and p = 0.012) were observed by six months. Wheelchair use significantly decreased (p = 0.011 and p = 0.035) and wheelchair skills increased (p = 0.009). Caregiver burden did not change (p = 0.226) but the number of activities of daily living (ADLs) that required no assistance significantly increased (p = 0.001) by three months and those who required complete assistance decreased (p = 0.001). No changes were observed in wheelchair repairs (p = 0.967) and breakdowns over time with new wheelchairs.
Conclusions
Wheelchair service delivery using the WHO 8-step process on manual wheelchair users in El Salvador has positive effects on health and quality of life, wheelchair skills, caregiver assistance levels, and poverty. Further research is needed to determine the relative contributions of the intervention components.
IMPLICATIONS FOR REHABILITATION
Providing manual wheelchairs using the 8-step process of the WHO has benefits on health and quality of life, wheelchair skills, caregiver assistance levels, and poverty.
The WHO 8-steps service delivery process for manual wheelchairs can be used in less-resourced settings.
Introduction
The World Health Organization (WHO) defines an appropriate wheelchair as one that satisfies the user’s needs in terms of size and postural support, is appropriate to the user’s environment and allows him/her to carry out his/her daily activities of self-management and for social, educational, and economic participation [Citation1]. In addition, an appropriate wheelchair should be locally available along with the affordable means to maintain and repair it [Citation1]. Based on prospective modelling, having access to an appropriate wheelchair is believed to have a positive impact on the individual’s health, social inclusion, and lifetime earnings [Citation2].
Wheelchair users often face several challenges to access appropriate wheelchairs. Among these challenges are not only those imposed by personal factors such as health condition, diagnosis, life stage, and living conditions. Challenges are also imposed by the environments such as lack of wheelchair service delivery systems, policy and funding, lack of affordable, quality product options, procurement strategies, and shortage of competent workforce [Citation3]. Inappropriate, low-quality wheelchairs and poor service delivery processes have negative effects on users’ health, independence and wellbeing, participation, and access to basic human rights such as health, education, and employment [Citation3].
The WHO has developed Guidelines and training packages for the provision of manual wheelchairs in less-resourced settings [Citation1,Citation4,Citation5]. The Guidelines recommend eight steps in the wheelchair service delivery process: referral and appointment; assessment; prescription; product funding and ordering; product preparation; fitting; user training; and maintenance, repair, and follow-up [Citation1]. The WHO wheelchair service training packages (WHO WSTPs) were designed to provide service providers with the knowledge and skills required to deliver wheelchairs that meet the specific postural and environmental needs of the users [Citation4,Citation5].
However, relatively few research studies have been carried out to evaluate the outcomes and long-term impact of the WHO 8-step wheelchair service delivery process in low- and middle-income countries (LMIC) [Citation6–11]. An uncontrolled cohort study of 55 wheelchair users in Zimbabwe showed a significant increase in users’ satisfaction with product features and related services, as well as with function after experiencing the WHO 8-step wheelchair service delivery process [Citation6]. A wait-list controlled study in Indonesia found significant improvements in health/environmental quality of life (QOL) and satisfaction with a device in users who received a wheelchair as compared with those on the waitlist [Citation7]. A cross-sectional survey study evaluating the outcomes of wheelchair services in 420 users in Kenya and 432 in the Philippines, who had or had not received services along with their wheelchairs, found that select services, such as providing training and assessing the fit of the wheelchair while the user propelled it, more than doubled the users’ chances of performing three or more activities of daily living (ADL) independently and of using their wheelchairs daily [Citation8]. A qualitative analysis of 48 of the participants in the same study found that wheelchair users frequently receive ill-fitted products without formal training on how to use them and that maintenance and repair services are frequently unavailable [Citation9]. A secondary analysis of the combined data from Kenya and the Philippines revealed that a composite service score (total number of services provided) was significantly related to ‘daily wheelchair use’, ‘outdoor unassisted wheelchair use’, ‘high performance of ADLs’ and a composite outcome score (consisting of these 3 outcomes and the ‘absence of serious falls’) [Citation10]. And finally, a self-controlled pilot study of 12 wheelchair users in Mexico showed a significant increase in users’ satisfaction with products features and related services, as well as a 10.9% improvement in wheelchair skills capacity and performance after receiving a wheelchair and a cushion following the WHO 8-step process [Citation11].
Although the studies mentioned above document positive outcomes related to the WHO 8-step process, there is also evidence of positive outcomes due to alternative approaches [Citation12–14] even if not provided according to WHO guidelines. For instance, a survey administered to 188 recipients of a one-size, economical wheelchair provided with no services found increased independent function and fewer pressure injuries [Citation12]. Another study on 519 individuals receiving the same type of wheelchair without services found a reduction of sick and hospitalization days, as well as improved emotional health, time spent outside the home and independence to perform self-care activities [Citation13]. A subsequent study on 191 recipients of wheelchairs without services found that “self-directed” employment and income level gradually increased until becoming significant after 30-months [Citation14]. Grider et al. (2016) found that 261 recipients of donated wheelchairs (fitting to their sizes being the only service) increased their time dedicated to work, reduced their time spent on begging, and raised their incomes [Citation15].
The broad goal of the current study was to contribute to the body of evidence investigating the outcomes related to providing manual wheelchairs according to the WHO 8-step service delivery process in less-resourced settings. Our specific objectives were to test the hypotheses that, after the delivery of manual wheelchairs with the WHO 8-step wheelchair-service-delivery process, wheelchair-related health and quality of life, wheelchair skills, wheelchair use, and poverty probability would improve; and that the number of wheelchair repairs required, adverse events, caregiver burden and the level of assistance provided would decrease.
Methods
Ethical approval
Ethics approval was granted from the National Committee on Research Ethics for Health in El Salvador (CNEIS/2018/043) and the Institutional Review Board at the University of Pittsburgh (number PRO18010578). Written informed consent was obtained from all participants before implementing study procedures.
Setting
All procedures of the study were conducted at 11 different rehabilitation centres, that served as wheelchair-service-delivery centres, in El Salvador. Although these organizations had recurrent wheelchair donations and an established network for rehabilitation, they had limited existing capacity and resources to conduct appropriate wheelchair service [Citation16].
El Salvador is a LMIC in Central America with a population of about 6.4 million people, with Spanish as the official language. It has two weather seasons, dry (November to April) and wet (May to October). The last national health survey implemented in El Salvador reports that 7.1% of households in El Salvador had at least one member with functional difficulty to move around [Citation17] (i.e., about 465,000 people who may need a wheelchair). In El Salvador there are no wheelchair-service-delivery policies or programs. Users frequently obtain their wheelchairs from donations given to government organizations.
Although El Salvador has registered moderate poverty reduction, 22.8% of the population still live under the national poverty line, and its levels of economic growth continue to be low (average of 2.3% Gross Domestic Product in recent years) [Citation18]. Out-of-pocket expenditure (% of current health expenditure) in El Salvador was 28.4 in 2019 [Citation19]. Only 21.4% of women between 15 and 49 years have healthcare coverage, either from the public or private sector [Citation17].
Participants
A consecutive sampling method was used to select participants using the waitlists at the 11 rehabilitation centres. We recruited wheelchair users and their caregivers. Inclusion criteria for wheelchair users were being a person with a mobility limitation requiring a wheelchair as a primary means of personal mobility, waiting to receive a new wheelchair from any of the participating wheelchair service delivery centres, 18-years of age or older, had the cognitive and verbal abilities required to respond to the study questions or a proxy who could respond on his or her behalf, and had access to a cell phone. Wheelchair users who required postural support to sit upright were excluded. Inclusion criteria for caregivers were being a person assisting the wheelchair user with ADLs, 18-years of age or older, being the primary caregiver and willing to participate in the study.
Intervention
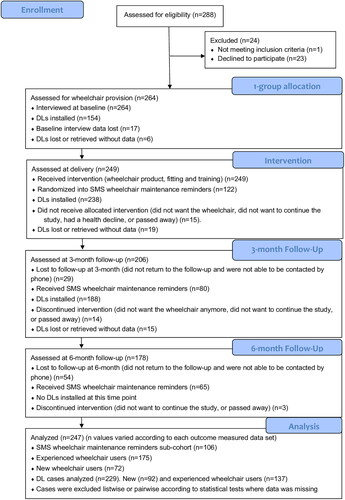
Following the initial assessment, all participants were placed on a waiting list until wheelchairs and services were available. All study participants were provided with a new wheelchair, donated by a faith-based organization, The Church of Jesus Christ of Latter-day Saints (LDS) [Citation20], a wheelchair cushion, and wheelchair services. The services were delivered by trained wheelchair service providers according to the WHO 8-step wheelchair service delivery process including assessment, fitting, and a 30-min individual or group training on seven wheelchair skills, device care, and pressure injury prevention techniques (see for a flow diagram of the progress through the phases of the study). The wheelchair skills taught during training consisted of two basic skills (pushing and turning), three intermediate skills (going up and down slight slopes and performing a partial wheelie), and two advanced skills (ascending and descending stairs with assistance). Additionally, wheelchair maintenance reminders were sent through a text message service (SMS) to a sub-cohort of 106 (43%) participants, selected through a block sampling technique, to explore the utility of the reminders to promote the care and appropriate working condition of the wheelchairs between those who had a wheelchair at the beginning of the study compared to those who did not. Wheelchair maintenance reminders were sent twice a week based on the recommendations of a Wheelchair Maintenance Training Program developed by the University of Pittsburgh [Citation21].
Figure 1. Study flow diagram.
Twenty-one wheelchair service providers of the 11 participating centres, all with a physiotherapy professional background and limited experience providing appropriate wheelchair services and products, were trained prior to the study in the basic and intermediate levels of the WHO WSTP and completed the International Society of Wheelchair Professionals (ISWP) Basic Knowledge Test [Citation22] to evaluate their knowledge of the 8-step process. For the 21 providers, the mean (SD) score on the Test was 70.8% (9.0). Fifteen providers (71%) met the 70% pass criterion. The wheelchair service providers had the greatest difficulty with the user fitting, product preparation, and user training test domains. Providers who did not pass the ISWP Test were offered additional training and studied the reference manual of the WHO Wheelchair Service Training Package – Basic Level.
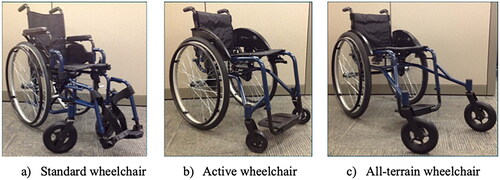
Wheelchair users were provided with one of three different wheelchair models according to the users’ needs and availability: standard, active, and all-terrain models (). The standard wheelchair was a cross-brace folding wheelchair with either solid or pneumatic rear tires (610 mm in diameter and 35 mm wide), available in six different seat widths (from 350 to 600 mm), with height-adjustable rear-wheel axles, and polyurethane front casters (200 mm in diameter and 50 mm wide). Active wheelchairs had a rigid frame, pneumatic rear tires (610 mm in diameter and 35 mm wide), backward-and-forward adjustable rear-wheel axles (with a 75 mm range), were available in five different seat widths (from 300 to 500 mm) and had polyurethane front casters (130 mm in diameter and 35 mm wide). All-terrain wheelchairs had a rigid frame, pneumatic rear tires (610 mm in diameter and 38 mm wide), backward-and-forward adjustable rear-wheel axles (with a 75 mm range), were available in three seat widths (from 400 to 500 mm) and had polyurethane front casters (200 mm in diameter and 50 mm wide). All wheelchair types had undergone standardized wheelchair testing methods (ISO 7176-8) intended to ensure durability for three to five years of use, including on rough terrains.
Figure 2. Study wheelchairs. From left to right: a) standard, b) active, and c) all-terrain wheelchairs.
In addition, all wheelchairs were provided with a basic contour cushion made of polyurethane foam. However, whenever a risk of pressure injury was identified for a study participant, wheelchair providers fabricated a pressure-relief cushion based on the WHO WSTP basic-level guidelines. Pressure-relief cushions were fabricated with 5-centimetrer firm polyurethane foam as the base and 5-centimeter soft polyurethane foam in the top layer. Additional information about the study wheelchairs can be found in the supporting information at the end of the manuscript.
Data collection
Data were collected between January and November 2019, by a group of eight data collectors from the University of El Salvador. Data collectors completed an online training course in research ethics from the Global Health Network [Citation23] and were also trained on-site to administer all study questionnaires and procedures during a 3-day workshop conducted by a staff member from United Cerebral Palsy Wheels for Humanity (UCPW; https://ucpwheels.org). All data collectors and the workshop trainer were native Spanish speakers. Following input from the training workshop, the translated questionnaires were finalized by the Spanish-speaker research staff at the University of Pittsburgh without formal back-translation and cross-cultural assessment.
Study participants were interviewed during the wheelchair assessment (about two months before wheelchair delivery), at the wheelchair delivery visit, and at 3- and 6-month follow-up visits after wheelchair delivery. Participants who were not able to attend a follow-up visit were interviewed by phone. Data were collected using the following structured questionnaires translated into Spanish () which included the same predetermined questions to all participants in the same order: ISWP Minimum Uniform Dataset (MUD) which included demographic, clinical and wheelchair-related questions [Citation24], Wheelchair Skills Test Questionnaire (WST-Q) [Citation25], Wheelchair Maintenance Training Questionnaire (WMT-Q) [Citation26], Breakdowns and Adverse Consequences Questionnaire (BAC-Q) [Citation27], Poverty Probability Index (PPI) for El Salvador [Citation28], WHO Quality of Life Questionnaire – Brief version (WHO QOL-BREF) [Citation29], and the MIT-Wheelchair-related Health Questionnaire [Citation30]. Some of these questionnaires include a standardized scoring system.
Table 1. Questionnaires administered by study visit and participant type.
Data loggers (DLs) were also used to objectively assess wheelchair use. DLs were battery-powered units that used 3-axis accelerometers and gyroscopes to sense the number of wheel rotations and the duration of each bout of motion [Citation31]. The DLs were attached to the spokes of the user’s wheelchair three times for two weeks each; at baseline (if they had a wheelchair), at delivery and at 3-month follow-up. After two weeks of data collection with the DLs, participants were visited at their homes, or other point near by their homes, to retrieve the DLs. The number of days of wheelchair use, average daily distance travelled, and average speed were calculated using a MATLAB (The MathWorks, Inc; Natick, Massachusetts) algorithm that combined the sensors’ data with wheel diameter.
Caregivers were interviewed using the Assistance with Activities of Daily Living Questionnaire [Citation32] assessing the amount of assistance provided with ADLs, and an abbreviated version of the Zarit Burden Interview (ZBI-12) [Citation33] questionnaire to measure caregiver burden. Both structured questionnaires were administered at baseline, at 3-month follow-up, and at 6-month follow-up (see ).
Responses to study questionnaires were entered using KoboToolbox app [Citation34], a tablet application that does not require the availability of an internet connection at the time of the interviews. All responses were answered and recorded in Spanish and converted to English using KoBoToolbox. All responses were reviewed for errors by native Spanish and English-speaking research staff. After data collection was completed, KoBoToolbox data were exported to a spreadsheet database.
Sample size
A sample size of 200 participants was estimated to detect a "small effect" (0.10) of a within-between interaction term with adequate power (0.8). This was assuming two groups (no wheelchair vs had a wheelchair previously), two time points (baseline and 3- or 6-moth follow-up), correlation between repeated measures = 0.5, and alpha = 0.05. So, this would allow us to detect differences in an outcome between the two types of wheelchair users, over time.
A total of 300 wheelchairs were donated by LDS for the study, so every effort was made to provide the totality of the wheelchairs followed the WHO 8-steps, which will in turn, account for the drop out of participants.
Data analysis
All data were analysed using descriptive statistics and graphics. For continuous, normally distributed variables, means and standard deviations (SD) are reported, whereas non-normally distributed variables are reported as medians and inter-quartile ranges (IQR). For categorical variables, frequency, and percentages (%) are reported. To detect significant changes in normally-distributed data within participants over time, repeated-measures ANOVA and paired t-tests were carried out. In cases where non-parametric data were analysed, Friedman’s Test and Wilcoxon signed-rank tests were used. To detect significant changes by wheelchair ownership at baseline or effect of SMS group where specified, independent t-tests were carried out if data were normally distributed, and their non-parametric counterpart, Mann-Whitney tests, in cases where data violated test assumptions. The significance level was set at p < 0.05. Only participants who continued using the study wheelchair provided by the end of the study were included in the analysis. All data was analysed using IBM SPSS Statistics for Windows, Version 21.
Clinical trial registration
The authors confirm that this study trial for this wheelchair intervention is registered in the ISRCTN clinical trials registry with the identification number: NCT04936087. This study was not registered before the enrollment of participants started because it did not meet the criteria for applicable clinical trials required by the United States of America federal law.
Results
Demographic and clinical data
Wheelchair users
A total of 264 wheelchair users were enrolled but, due to various reasons (including passing away, lack of transportation to commute to the study centre, lack of time for the study visits, no longer wanting the wheelchair, health decline or no wheelchair size available), only 178 persisted until the 6-month follow-up (). Eighty-one wheelchair users were lost to follow-up (32.6%).
The mean (SD) time between baseline and 6-month follow-up was 271 (14) days, including a two-month waiting time before wheelchair delivery. Some participants were harder to reach for follow-up interviews after they had received their new wheelchair and they were given an additional month to be contacted for the last follow-up questionnaire.
The demographic and clinical data are shown in . The study recruited more males than females. About half of the participants lived with their spouses or significant others. Of the participants, 65% had primary education level or less and 40% were employed. Predominant diagnoses were spinal cord injury and amputation.
Table 2. Demographic and clinical data.
Caregivers
One hundred and nineteen caregivers were recruited to participate in the study at baseline as not all wheelchair user participants needed assistance from a family member or caregiver. At the time of wheelchair delivery, 3- and 6-month follow-up visits, 112 (94%), 74 (62%), and 43 (36%) caregivers were interviewed, respectively. A variety of different family members or caregivers, in addition to those who had given informed consent to participate, took the wheelchair user participants to their appointments. shows the demographic data of caregivers.
Table 3. Demographic data at baseline for caregivers.
Wheelchair-related health
summarizes wheelchair-related health indicators collected over time. The frequency of reported pressure injuries, which included all study participants, was significantly higher at baseline compared to later assessments. In wheelchair users who had previously owned a wheelchair, falls during wheelchair transfers and wheelchair riding, back pain, and injuries in hands and upper extremities were significantly lower at the 6-month visit compared to baseline.
Table 4. Wheelchair-related health indicators over time, n (%).
Quality of life
The overall rates for quality of life, satisfaction with health, and the physical and environment health domains of the WHO QOL-BREF significantly increased from baseline to six months (see ).
Table 5. Mean (SD) quality of life scores by time as measured with WHO QOL-Bref (n = 164).
Participants who owned a wheelchair at baseline had higher quality of life and satisfaction with health at baseline than those who did not (p = 0.001 and p = 0.002, respectively.) Physical (p = 0.001), psychological (p = 0.002), and environmental health domains (p = 0.010) were also higher at baseline for the first group. At 6-month follow-up only satisfaction with health (p = 0.011), physical (p = 0.015) and psychological health (p = 0.024) remained significant higher for participants who owned a wheelchair at baseline.
Wheelchair skills
shows the WST-Q capacity scores by wheelchair ownership at baseline and by time. Those participants who owned a wheelchair at baseline had significant higher WST-Q capacity scores at three and six months than those who did not own a wheelchair at baseline. WST-Q capacity increased from baseline to both three and six months in the experienced user group. The magnitude of the improvement was less at six months than at three months for the same group
Table 6. Median (IQR) total percentage WST-Q capacity scores by time and by wheelchair ownership at baseline.
Similarly, users who had a wheelchair at baseline were able to perform a greater number of basic (p < 0.009) and intermediate level skills (p < 0.004) at three and six months than those who did not have a wheelchair at baseline. In terms of advanced skills, there were no significant differences (p > 0.100).
As baseline WST-Q capacity scores were not collected for users who did not have a wheelchair at baseline, it was not possible to know if the intervention resulted in any improvement for this cohort.
Wheelchair use
Significant differences were found in the daily distance and average speed by time. For experienced users, there was a significant reduction in daily distance travelled at delivery and three months compared to baseline; the daily average speeds at delivery and three months were also significantly lower than the speed at baseline. When analysing wheelchair use by wheelchair ownership group, no significant differences were found between those who owned a wheelchair previously compared to those who did not (p > 0.053 and p > 0.780, respectively). Refer to for additional details on wheelchair use measurements.
Table 7. Wheelchair use measurements by time, median (IQR).
Baseline datalogger measurements were only recorded for participants who owned a wheelchair at this time. Participants gave permission to attach a DL to their wheelchairs.
Wheelchair repairs and adverse events
shows the number (%) of participants who did repairs to their wheelchairs in the previous three months. The number of participants who did repairs in the previous three months at baseline and delivery were significantly higher than at 3- and 6-month follow-up visits. The number of wheelchair repairs in the previous three months decreased from one to seven and one to four with previously owned wheelchairs at baseline and delivery to one to three repairs with new wheelchairs at 3-month follow-up visit. No significant differences were found in the number of participants who did repairs between three and six months (p = 0.861). Additionally, no significant differences were found in adverse events (being stranded, injured, missed work or school, missed a medical appointment, or other) by time (p = 0.392). Not enough valid cases were available to analyse wheelchair repairs and adverse event by wheelchair ownership at baseline.
Table 8. Number (%) of participants who did wheelchair repairs and who experienced adverse events by time and by wheelchair ownership at baseline.
Effect of SMS maintenance remainders
In investigating the sub-cohort of study participants who were selected to receive maintenance reminders, no significant differences were found in age, gender, or medical diagnoses between these SMS participants and those who did not receive the reminders (p = 0.539, p = 0.417, and p = 0.745, respectively). No significant differences were found in the number of repairs in the previous three months at 3- (p = 0.967) and 6-month (p = 0.176) follow-up visits when comparing users by SMS group. Furthermore, no significant differences were found in the number of adverse events that were reported at 3- (p = 0.697) or 6-month (p = 0.898) follow-up visits by SMS group.
Caregiver burden and ADL assistance levels
summarizes the results of the Caregiver burden ZBI-12 scale and Checklist of Activities of Daily Living. Caregivers reported no difference in perceived caregiver burden over time compared to baseline measurements (p = 0.492). Similarly, no significant differences were found in employment status of the caregivers (p = 0.666), paid work of caregivers (p = 0.926), or hours of care provided per week (p = 0.618) over time. Caregiver’s social participation measured through the social domain using the abbreviated ZBI-12 showed no change over time (p = 0.953). There was a significant increase in the number of ADLs that required no assistance from assessment to 3-month follow-up, and a reduction in the number of ADLs that required complete assistance from baseline to 3- and 6-month follow-up visits.
Table 9. Burden of care indicators for caregivers over time, median (IQR).
Poverty probability
On average, the likelihood of living below the National and the USAID “Extreme” poverty lines was significantly reduced from baseline to six months after wheelchair delivery (see ). No significant differences were found for poverty probability by wheelchair ownership at baseline (p = 0.717 and p = 0.679).
Table 10. Mean (SD) poverty probabilities by time (n = 162).
Discussion
This study contributes to the body of evidence on outcomes related to providing wheelchairs according to the WHO 8-step process for manual wheelchair service delivery in less-resourced settings. Although the data suggest that receiving a wheelchair through the WHO 8-step process has a positive effect in wheelchair-related health, wheelchair skills, poverty probability, quality of life of wheelchair recipients, and in the level of assistance provided by caregivers for ADLs, caution should be taken as the loss to follow-up rate may pose a potential threat to this study’s validity. Study participant dropout may have been due to the duration of the study, the number of visits required to the study centres and/or the lack of transportation resources of study participants. No effects were observed in caregiver burden and wheelchair breakdowns, repairs, and adverse events. A significant reduction was noted in wheelchair use likely caused by environmental factors and lack of appropriate user training.
In this study, the provision of early advice on pressure relieving techniques and injury prevention, along with high-quality, reliable wheelchair products, that were matched to the users’ dimensions and environmental needs, may have reduced the incidence of pressure injuries, back pain, falls, and upper-extremity injuries and pain, which likely promoted the health, participation, economy, and overall wellbeing of wheelchair users. A pressure injury can take from six weeks to 12 months to completely heal depending on its severity and may cost up to 2,483 USD [Citation35]. Back pain has been regarded as a factor contributing to reduced participation of wheelchair users and device abandonment [Citation36,Citation37]. Products that are poor quality, old, in bad working conditions, not appropriate for the user’s environment, or in need of maintenance and repair put the user at additional risk of falls and injuries [Citation38–40].
The results on quality-of-life indicators in this study were similar to previous studies [Citation12–14]. This suggests that the delivery of wheelchairs may be only partially responsible for the health of the users and that people with disabilities face additional factors affecting their health, such as limited access to healthcare and rehabilitation services.
Having had a wheelchair in the past may have given a health advantage to participants in this group to the point that their satisfaction with health remained significantly higher compared to those who did not have one but who were eventually able to reach similar rates in quality of life after six months. The fact that wheelchair-related health improved may have also contributed to the overall increase in quality of life and satisfaction with health rates; especially among the most active wheelchair users in this study, who were significantly younger.
Wheelchair users in this study reported lower WST-Q scores compared to users from other studies (84% − 88%) living in countries with higher incomes, where healthcare and assistive technology systems are more established [Citation41,Citation42], and to users in Indonesia (71% and 78%) and Mexico (62% and 73%) [Citation7,Citation11]. The small improvements in wheelchair skills and low retention in this study may be presumably due to insufficient dose of training to ensure skill transfer, and lack of practice and expert advice, among other reasons. Service providers and institutions recruited for this study did not have sufficient experience and resources to conduct wheelchair skills training. Moreover, the WHO 8-step wheelchair service delivery process only includes seven wheelchair skills, and the WST-Q evaluated many more advanced skills that are not part of the WHO Basic WSTP. This can also be a reason why wheelchair users had higher scores in basic and intermediate skills and did not present an improvement in advanced skills. The Wheelchair Skills Program (WSP) (www.wheelchairskillsprogram.ca) provides training recommendations for which there has been supportive evidence in many studies, including 16 RCTs and two meta-analyses [Citation43,Citation44]. Including additional wheelchair skills training and expert-supervised practice to the skills already recommended in the WHO Basic WSTP, especially to new wheelchair users, their caregivers and service providers, is recommended.
With the delivery of a new wheelchair, wheelchair use was reduced. In El Salvador, the rainy season began when wheelchairs were being delivered and continued through six to seven months, which may be one of the reasons for wheelchair use reduction. Other reasons for the reduction in wheelchair use may be related with the age and health condition of the participants, the small improvement on wheelchair skills, and the adaptation time to the new wheelchair.
Daily distance travelled and speed by participants in this study were by far much lower than those of wheelchair users in countries with more accessible infrastructure, where distance has been reported to be more than two kilometres per day and average speed approximately 1.0 m/s [Citation45]. Wheelchair use is indicative of the users’ levels of social and occupational participation, the accessibility of their environment, and their wheelchair skills [Citation41,Citation45].
A reduction in the number of wheelchair breakdowns that required repair was as expected as the wheelchairs provided during the study were new and passed recommended quality-standards (ISO 7176-8). The lack of impact of using SMS maintenance reminders may be also explainable by the little need of maintenance of these wheelchairs. For future studies, the effect of maintenance reminders should be studied over a longer period as some studies suggest that about half of users needed at least one repair minimum in the prior six months of a wheelchair-related accident [Citation26,Citation46].
The results on caregiver burden and assistance provided to ADLs supports the evidence that provision of a wheelchair does not automatically make the user completely independent to move around or to perform ADLs [Citation47]. Besides environmental and resource constraints, personal attributes, such as aging and health status, and lack of appropriate training to both, the user and the caregiver, on how to effectively use the wheelchair and overcome obstacles found in different environments often hinders the capacity to achieve desired goals [Citation48,Citation49]. Furthermore, although a wheelchair may reduce some of the physical effort associated to mobilizing someone with functional difficulties, still some physical, mental and emotional demands exist for the caregiver as the user may still need help with repairing the wheelchair, assisting with transfers and non-accessible environments, anticipating wheelchair-related issues in activities outside the home, or dealing with unpredictable situations, etc. [Citation47,Citation50]. Caregiver support is provided across the continuum of care, and not just related to the wheelchair.
Previously published evidence indicates that households with a family member with a disability have a higher incidence and intensity of multidimensional poverty than those without a relative with a disability [Citation51]. The data for the participants in our study were consistent with this finding and wheelchair provision may have an important effect on this. A recent economic assessment found that investing in assistive technology, services included, increases the lifetime earning potential of the recipient with a 900% return of investment by accruing improved physical and mental health, educational, and employment skills outcomes [Citation2]. By using econometric-analysis methods, Grider et al. [Citation15] found that those who received a wheelchair were able to raise their income by 77.5% by increasing their time spent on working, which resulted in a 122% rate of return, and that beneficiaries must continue to have the wheelchairs for outcomes to be sustained. Whereas Shore (2008) found no changes in employment and education rates for users who had used their donated wheelchairs for more than six months [Citation12], changes in “self-directed” employment and sufficient income generation after 12 and 30 months of wheelchair use were observed [Citation13,Citation14]. The results of this study also suggest that having a wheelchair vs not having one, among other factors, is partially responsible for changing the households’ poverty probability.
Limitations
The exclusion of individuals who require postural support to sit upright is an important consideration. The findings of this study are not generalizable to a large portion of individuals who have a very significant need for a well-fitted wheelchair.
Although randomization of wheelchair users to a wheelchair intervention or a control group is not ethically possible, because the utilization of a wheelchair is an intervention for which there is growing research evidence, another study design (e.g., a waitlist-controlled study) could have been used. However, our study participants were recruited from waitlists and making half of them wait for more time was not advised by local service providers. Therefore, as a cohort study with pre- versus post-intervention comparisons, the improved outcomes may be attributed to other factors in addition to the WHO 8-step wheelchair service delivery process. Also in this study, heterogeneity (the two cohorts) blurred the findings somewhat versus separate studies of new and experienced users.
An a priori power analysis was not performed to estimate the sample size needed, instead the sample size estimate was based on sample sizes that proved to be adequate in similar previous studies as well as pragmatic considerations of the number of participants that could be enrolled in the study. Even though an attempt was made to include up to 300 study participants, many of them were unable to follow through the entire duration of the study for different causes. Lost to follow-up data was neither adjusted nor measured as the worst outcome. No additional data analysis was performed to further investigate how those lost to follow up differed in wheelchair and training received, health condition, and sociodemographic characteristics from the participants that remained in the study.
Future studies should try to prevent loss to follow-up with different strategies like making use of information technologies to perform follow-up interviews, providing individual accessible transportation to the study participants and their companions, and limiting the amount of time required as much as possible. Other options could be adjusting lost to follow- up data or deliberately measuring worse case scenarios.
As all participants underwent the same set of interview questions at four time points, fatigue and boredom could have occurred affecting the quality of the questions and individual answers, and the willingness of the participants to continue the study. Future studies should also limit the number of questions asked to reduce the study time spent in the study.
Statistical analysis was limited to comparisons of outcome measures over time and by wheelchair ownership groups and did not provide proof of the existent association between outcomes and the WHO’s recommendations as the wheelchair treatment effect could not be isolated. A secondary statistical analysis that employs regression analysis [Citation8] or matched models [Citation18] to estimate the impact of wheelchair products and services on socioeconomic, health, mobility, and quality of life outcomes is recommended. A subsequent analysis of the data of this study to explore any relationship between sociodemographic background and changes in outcomes is also recommended, as this was not performed at the time of data analysis.
Also, the SMS reminder group was limited by one-way SMS, so there was no way to determine whether the participant received or read the maintenance reminders. The limited time frame of the study, six months, may have biased our results because the impact of wheelchair service delivery may not have been realized until after the study concluded.
Some of the study variables may have not been defined well among participants and data collectors, and then, may have been misreported, such as what is considered to be a fall or a resolved pressure injury. Future studies should make sure that study participants, data collectors and researchers have the same understanding of study variables. Although data collectors reviewed all questionnaires for context-appropriateness, there was not a formal back-translation and cross-cultural assessment of the study questions.
Finally, the fact that a proportion of the wheelchair service providers did not pass the ISWP Basic Test and had limited experience and resources for wheelchair service delivery may have limited the quality and quantity of wheelchair services provided.
Future studies are needed to address the limitations discussed above. Also, more studies are needed evaluating the eight steps in the WHO process and the quality of their impact in order to make the case for appropriate wheelchair service delivery in less-resourced settings.
Conclusions
Wheelchair service delivery according to the WHO 8-step process may improve a variety of outcomes for wheelchair users including wheelchair-related health, wheelchair skills, quality of life, and decreased poverty probability as well as assistance level provided by caregivers for ADLs. More research on the benefits of providing wheelchairs following the WHO 8-step approach is needed. This research-based evidence is necessary to drive policy and wheelchair service delivery programs, especially in LMICs, toward more effective interventions that maximize health and social outcomes for wheelchair users.
Acknowledgments
The authors thank the personnel of Momentum Wheels for Humanity (formerly UCP Wheels for Humanity) and the University of Pittsburgh, the data collectors from the University of El Salvador, and the personnel of each service delivery centre in El Salvador. The authors declare that this manuscript is original, has not been published before and is not currently being considered for publication elsewhere.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All data files of this study are publicly available from the OPEN-ICPSR (Inter-university Consortium for Political and Social Research) database at https://doi.org/10.3886/E173201V1.
Additional information
Funding
Notes on contributors
Yasmin Garcia-Mendez
Yasmin Garcia-Mendez is the Technical Advisor of Momentum Wheels for Humanity. She earned her BS in Biomedical Engineering at the Universidad Iberoamericana in Mexico City and a MS in Rehabilitation Science at the University of Pittsburgh, PA, USA. Her research interests are in the areas of in assistive technology, public health, and regulation.
Megan D’Innocenzo
Megan D’Innocenzo earned her BS in Exercise Science from Slippery Rock University and her MS in Health, Physical Activity and Chronic Disease, with a concentration in statistics, from the University of Pittsburgh. Her research interests are in the areas of in rehabilitation technology, public health, and statistical analysis.
Jonathan Pearlman
Jonathan Pearlman is an Associate Professor and Chair of the Department of Rehabilitation Science and Technology. Pearlman earned his BS and MS in mechanical engineering at UC Berkeley and Cornell University, respectively. Pearlman completed his PhD work in Rehabilitation Science and Technology at the University of Pittsburgh in 2007, with an emphasis on assistive technology design and transfer to developing countries. His research interests are in the areas of participatory action design, assistive technology transfer methods, and new product development.
Stephanie Vásquez-Gabela
Stephanie Vásquez Gabela serves as Clinical and Research Manager at the University of Pittsburgh and as a Rehabilitation Engineer at the UPMC-Center for Assistive Technology. Stephanie holds a BS in Mechatronics Engineering and a MS in Rehabilitation Science & Technology. She is involved in projects on wheelchair testing and standards. She is interested in public policy for rehabilitation and access to Assistive Technology in low- and middle-income countries.
Perth Rosen
Perth Rosen is Senior Advisor to Momentum Wheels for Humanity and international development consultant. Rosen earned a degree in International Development from UC Boulder in 2000 and a Master in Advanced International Relations from the University of Queensland in 2008. She specializes in health security and health equity and between 2016-2022 led programming that increased access to rehabilitation and assistive technology in low-and-middle income countries.
Maria-Virginia Rodriguez-Funes
Maria-Virginia Rodriguez-Funes is the Quality Officer at the National Hospital Rosales in El Salvador. She was the Clinical Research Coordinator at the Faculty of Medicine in the University of El Salvador at the time of the study. She earned her MD at the Universidad Evangélica de El Salvador and a Master in Public Health at the Universidad Centroamericana José Simeón Cañas, El Salvador. She is a member of the Red Bioetica Latinoamericana UNESCO.
R. Lee Kirby
R. Lee Kirby received his MD degree from Dalhousie University in Halifax, Nova Scotia, Canada. His specialty training in Physical Medicine and Rehabilitation was carried out at the University of Washington in Seattle, Washington, USA, at Dalhousie University and at Stoke Mandeville Hospital in England. He is a Professor in the Division of Physical Medicine and Rehabilitation in the Department of Medicine at Dalhousie University with a cross-appointment in Community Health and Epidemiology. His primary research interest is the safety and performance of wheelchairs. He has held research grants from several national and international funding bodies. He has authored or co-authored 2 books and 175 papers in peer-reviewed journals. He heads the team that developed the Wheelchair Skills Program, a low-tech, high-impact training program that is relevant for both more- and less-resourced settings.
Anand Mhatre
Anand Mhatre is an Assistant Professor in the Department of Occupational Therapy at the Ohio State University. He has a PhD and post doctorate in Rehabilitation Science, a master’s degree in manufacturing systems engineering and a bachelor’s degree in mechanical engineering. Dr. Mhatre’s work focuses on technology development, standards development, user testing and technology transfer. He has taught undergraduate and graduate students product design in health science and engineering schools. He serves as an active member of the ISO committee for wheelchair standards and CLASP Product Advisory Council for global mobility aids procurement, among several other committees.
References
- World Health Organization. Guidelines on the provision of manual wheelchairs in less resourced settings. 2008. https://www.who.int/disabilities/publications/technology/English%20Wheelchair%20Guidelines%20(EN%20for%20the%20web).pdf
- ATScale. The case for investing in assistive technology. 2020. https://static1.squarespace.com/static/5b3f6ff1710699a7ebb64495/t/5fbf5c44eaf37e3b64932e6c/1606376534765/Case_for_Investing_in_AT_a11y.pdf
- Gowran RJ, Bray N, Goldberg M, et al. Understanding the global challenges to accessing appropriate wheelchairs: position paper. Int J Environ Res Public Health. 2021;18(7):3338. doi:10.3390/ijerph18073338.
- World Health Organization. Wheelchair service training package – basic level. Geneva: WHO; 2012. https://www.who.int/disabilities/technology/wheelchairpackage/en/
- World Health Organization. Wheelchair Service Training Package – Intermediate Level (WSTP-I). Geneva: WHO; 2013. https://www.who.int/disabilities/technology/wheelchairpackage/wstpintermediate/en/
- Visagie S, Mlambo T, van der Veen J, et al. Impact of structured wheelchair services on satisfaction and function of wheelchair users in Zimbabwe. Afr J Disabil. 2016;5(1):222.
- Toro ML, Eke C, Pearlman J. The impact of the world health organization 8-steps in wheelchair service provision in wheelchair users in a less resourced setting: a cohort study in Indonesia. BMC Health Serv Res. 2016;16(1):26. doi:10.1186/s12913-016-1268-y.
- Bazant ES, Himelfarb Hurwitz EJ, Onguti BN, et al. Wheelchair services and use outcomes: a cross-sectional survey in Kenya and the Philippines. Afr J Disabil. 2017;6:318. doi:10.4102/ajod.v6i0.468.
- Williams E, Hurwitz E, Obaga I, et al. Perspectives of basic wheelchair users on improving their access to wheelchair services in Kenya and Philippines: a qualitative study. BMC Int Health Hum Rights. 2017;17(1):22. doi:10.1186/s12914-017-0130-6.
- Kirby RL, Doucette SP. Relationships between wheelchair services received and wheelchair user outcomes in Less-Resourced settings: a Cross-Sectional survey in Kenya and the Philippines. Arch Phys Med Rehabil. 2019;100(9):1648–1654.e9. doi:10.1016/j.apmr.2019.02.002.
- Quiñones-Uriostegui I, Alessi-Montero A, Bueyes-Roiz V, et al. Wheelchair users’ satisfaction after provision using the WHO 8-step guidelines: a pilot study. J Spinal Cord Med. 2023;10:1–9. doi:10.1080/10790268.2023.2171627.
- Shore SL. Use of an economical wheelchair in India and Peru: impact on health and function. Med Sci Monit. 2008;14(12):PH71–9.
- Shore S, Juillerat S. The impact of a low cost wheelchair on the quality of life of the disabled in the developing world. Med Sci Monit. 2012;18(9):CR533–42. doi:10.12659/msm.883348.
- Shore S. The long-term impact of wheelchair delivery on the lives of people with disabilities in three countries of the world. Afr J Disabil. 2017;6:344. doi:10.4102/ajod.v6i0.344.
- Grider J, Wydick B. Wheels of fortune: the economic impacts of wheelchair provision in Ethiopia. J Dev Effect. 2016;8(1):44–66. doi:10.1080/19439342.2015.1064986.
- Sarin E. Accelerating core competencies for effective wheelchair service and support (ACCESS) project: evaluation of access project in five countries. Arlington, VA: JSI Research & Training Institute, Inc.; 2017. https://www.icpsr.umich.edu/web/ADDEP/studies/37156/publications
- Instituto Nacional de Salud de El Salvador. Encuesta Nacional de Salud: resultados principales. 2021. http://ins.salud.gob.sv/encuestas/
- The World Bank Group. The world bank in El Salvador. 2021. https://www.worldbank.org/en/country/elsalvador
- The World Bank Group. Out-of-pocket expenditure (% of current health expenditure) - El Salvador. 2019. https://data.worldbank.org/indicator/SH.XPD.OOPC.CH.ZS?locations=SV
- The Church of Jesus Christ of Latter-Day Saints. What we do: wheelchairs. 2021. https://www.latterdaysaintcharities.org/what-we-do/wheelchair
- University of Pittsburgh. Wheelchair maintenance training program. 2014. www.upmc-sci.pitt.edu/node/924
- International Society of Wheelchair Professionals. ISWP wheelchair service provision basic test. 2021. https://wheelchairnetwork.org/basic-knowledge-test/
- The Global Health Network. Global health training center: research ethics online training. 2021. https://globalhealthtrainingcentre.tghn.org/elearning/research-ethics/
- Toro-Hernández ML, Augustine N, Kankipati P, et al. Preliminary steps of the development of a minimum uniform dataset applicable to the international wheelchair sector. PLoS One. 2020;15(9):e0238851. doi:10.1371/journal.pone.0238851.
- Kirby RL, Smith C, Parker K, et al. The wheelchair skills program manual. Version 4.3 "low tech, high impact". 2016. www.wheelchairskillsprogram.ca/eng/manual.php
- Toro ML, Bird E, Oyster M, et al. Development of a wheelchair maintenance training programme and questionnaire for clinicians and wheelchair users. Disabil Rehabil Assist Technol. 2017;12(8):843–851. doi:10.1080/17483107.2016.1277792.
- Toro ML, Worobey L, Boninger ML, et al. Type and frequency of reported wheelchair repairs and related adverse consequences among people with spinal cord injury. Arch Phys Med Rehabil. 2016;97(10):1753–1760. doi:10.1016/j.apmr.2016.03.032.
- Schreiner M. Simple poverty scorecard® poverty-assessment tool El Salvador. 2017. http://www.simplepovertyscorecard.com/SLV_2014_ENG.pdf
- Development of the world health organization WHOQOL-BREF quality of life assessment. The WHOQOL group. Psychol Med. 1998;28(3):551–558. doi:10.1017/S0033291798006667.
- D'Innocenzo ME, Pearlman JL, Garcia-Mendez Y, et al. Exploratory investigation of the outcomes of wheelchair provision through two service models in Indonesia. PLoS One. 2021;16(6):e0228428. doi:10.1371/journal.pone.0228428.
- Gandhi A, Frey D, Sundar P, et al. Design of a cellular-enabled data-logging system for wheelchair use characterization. In: Procedings of the IEEE Global Humanitarian Technology Conference; 2017 October 19-22; San Diego, CA. p. 1–4. doi:10.1109/GHTC.2017.8239316.
- Drumm Boyd CL. Activities & instrumental activities of daily living - definitions, importance and assessments, paying for senior care. 2020. https://www.payingforseniorcare.com/activities-of-daily-living#Activities-of-Daily-Living-Checklist
- Bédard M, Molloy DW, Squire L, et al. The zarit burden interview: a new short version and screening version. Gerontologist. 2001;41(5):652–657. doi:10.1093/geront/41.5.652.
- Harvard Humanitarian Initiative. Kobotoolbox: data collection tools for challenging environments. 2021. https://www.kobotoolbox.org
- World Health Organization. Wheelchair service training package for managers and stakeholders. 2015 https://www.who.int/disabilities/technology/wheelchairpackage/wstpmanagers/en/
- Samuelsson K, Larsson H, Thyberg M, et al. Back pain and spinal Deformity-Common among wheelchair users with spinal cord injuries. Scand J Occup Ther. 1996;3(1):28–32. doi:10.3109/11038129609106679.
- Mukherjee G, Samanta A. Wheelchair charity: a useless benevolence in community-based rehabilitation. Disabil Rehabil. 2005;27(10):591–596. doi:10.1080/09638280400018387.
- Rice LA, Peters J, Sung J, et al. Perceptions of fall circumstances, recovery methods, and community participation in manual wheelchair users. Am J Phys Med Rehabil. 2019;98(8):649–656. doi:10.1097/PHM.0000000000001161.
- Rice LA, Sung J, Peters J, et al. Perceptions of fall circumstances, injuries and recovery techniques among power wheelchair users: a qualitative study. Clin Rehabil. 2018;32(7):985–993. doi:10.1177/0269215518768385.
- McClure LA, Boninger ML, Oyster ML, et al. Wheelchair repairs, breakdown, and adverse consequences for people with traumatic spinal cord injury. Arch Phys Med Rehabil. 2009;90(12):2034–2038. doi:10.1016/j.apmr.2009.07.020.
- Hosseini SM, Oyster ML, Kirby RL, et al. Manual wheelchair skills capacity predicts quality of life and community integration in persons with spinal cord injury. Arch Phys Med Rehabil. 2012;93(12):2237–2243. doi:10.1016/j.apmr.2012.05.021.
- Kirby RL, Worobey LA, Cowan R, et al. Wheelchair skills capacity and performance of manual wheelchair users with spinal cord injury. Arch Phys Med Rehabil. 2016;97(10):1761–1769. doi:10.1016/j.apmr.2016.05.015.
- Keeler L, Kirby RL, Parker K, et al. Effectiveness of the wheelchair skills training program: a systematic review and meta-analysis. Disabil Rehabil Assist Technol. 2019;14(4):391–409. doi:10.1080/17483107.2018.1456566.
- Tu CJ, Liu L, Wang W, et al. Effectiveness and safety of wheelchair skills training program in improving the wheelchair skills capacity: a systematic review. Clin Rehabil. 2017;31(12):1573–1582. doi:10.1177/0269215517712043.
- Tolerico ML, Ding D, Cooper RA, et al. Assessing mobility characteristics and activity levels of manual wheelchair users. J Rehabil Res Dev. 2007;44(4):561–571. doi:10.1682/jrrd.2006.02.0017.
- Hansen R, Tresse S, Gunnarsson RK. Fewer accidents and better maintenance with active wheelchair check-ups: a randomized controlled clinical trial. Clin Rehabil. 2004;18(6):631–639. doi:10.1191/0269215504cr777oa.
- Giesbrecht EM, Miller WC, Woodgate RL. Navigating uncharted territory: a qualitative study of the experience of transitioning to wheelchair use among older adults and their care providers. BMC Geriatr. 2015;15(1):91. doi:10.1186/s12877-015-0092-2.
- Mortenson WB, Miller WC. The wheelchair procurement porcess: perspectives of clients and prescribers. Can J Occup Ther. 2008;75(3):167–175. doi:10.1177/000841740807500308.
- Kraskowsky LH, Finlayson M. Factors affecting older adults’ use of adaptive equipment: review of the literature. Am J Occup Ther. 2001;55(3):303–310. doi:10.5014/ajot.55.3.303.
- Mortenson WB, Demers L, Fuhrer MJ, et al. How assistive technology use by individuals with disabilities impacts their caregivers: a systematic review of the research evidence. Am J Phys Med Rehabil. 2012;91(11):984–998. doi:10.1097/PHM.0b013e318269eceb.
- Pinilla-Roncancio M. The reality of disability: multidimensional poverty of people with disability and their families in latin america. Disabil Health J. 2018;11(3):398–404. doi:10.1016/j.dhjo.2017.12.007.
